Highlights
By July 25, Colombia had confirmed 240 795 cases of COVID-19 and 8269 deaths (case fatality rate of 3.4%).
All departments had reported cases, but 292 municipalities were apparently free of COVID-19 (26%) and 373 (33.2%) had seen limited transmission.
Specific mortality rates by department ranged from 0 in Vichada to 1278 in Amazonas, which was 7.8 times the national rate (incidence rate ratio (IRR) = 7.8, 95% confidence interval 6.4–9.5).
Using a conservative approach to assess the potential underestimation of cases, it was estimated that, by July 25, Colombia should have detected 1 328 175 cases instead of the actual 240 795 observed, an underestimation of 82%.
Keywords: SARS-Cov-2, COVID-19, Epidemiology, Colombia, Pandemic, Lockdown
Abstract
Background
Colombia detected its first coronavirus disease 2019 (COVID-19) case on March 2, 2020. From March 22 to April 25, it implemented a national lockdown that, apparently, allowed the country to keep a low incidence and mortality rate up to mid-May. Forced by the economic losses, the government then opened many commercial activities, which was followed by an increase in cases and deaths. This paper presents a critical analysis of the Colombian surveillance data in order to identify strengths and pitfalls of the control measures.
Methods
A descriptive analysis of PCR-confirmed cases between March and July 25 was performed. Data were described according to the level of measurement. Incidence and mortality rates of COVID-19 were estimated by age, sex, and geographical area. Sampling rates for suspected cases were estimated by geographical area, and the potential for case underestimation was assessed using sampling differences.
Results
By July 25, Colombia (population 50 372 424) had reported 240 745 cases and 8269 deaths (case fatality rate of 3.4%). A total of 1 370 271 samples had been analyzed (27 405 samples per million people), with a positivity rate of 17%. Sampling rates per million varied by region from 2664 to 158 681 per million, and consequently the incidence and mortality rates also varied. Due to geographical variations in surveillance capacity, Colombia may have overlooked up to 82% of the actual cases.
Conclusion
Colombia has a lower case and mortality incidence compared to other South American countries. This may be an effect of the lockdown, but may also be attributed, to some extent, to geographical differences in surveillance capacity. Indigenous populations with little health infrastructure have been hit the hardest.
Introduction
Coronavirus disease 2019 (COVID-19) is a new emerging infectious disease, and more than 17 million cases and more than 680 000 deaths had been reported worldwide by August 1, 2020 (World Health Organization, 2020b). It has been declared a pandemic by the World Health Organization (WHO) and has prompted lockdowns of over 2 months in most countries (World Health Organization, 2020a). The virus has the potential to transmit from symptomatic and asymptomatic individuals, which has made it difficult to control its spread around the globe.
Colombia identified its first imported case of COVID-19 on March 2, and by July 25 had reported 240 745 cases and 8269 deaths (Instituto Nacional de Salud, 2020a), which is a low incidence compared to other countries in Latin America (Pan American Health Organization, 2020). It has been postulated that this relatively mild behavior of the virus may be explained in part by the lockdown and by demographic features of the population, considering that 86.4% of the Colombian population are under 60 years of age (Departamento Administrativo Nacional de Estadística, 2018).
The mild impact of the COVID-19 pandemic in Colombia is unexpected, given that it is one of the most unequal countries in a very unequal region of the world, with a health system that, despite having high population insurance coverage (94.6%) (Ministerio de Salud y Protección Social, 2018), still struggles to provide good quality healthcare services. In addition, a large number of hospitals are currently underfunded, since financial resources flow from health insurance organizations (HIO) to hospitals through a cumbersome process in which the HIOs have the upper hand and can leverage multiple strategies in order to block payments after a service has been provided. Currently, HIOs are withholding more than US$ 3 billion from hospitals for individual health services provided from 2000 through 2019, a debt that doubled over the last 5 years (Asociación Colombiana de Hospitales y Clínicas, 2019).
Given the structural shortcomings of the Colombian health care system, the apparent good standing of the country during the COVID-19 pandemic is a positive but unexpected outcome. This article presents the results of a critical analysis of the epidemiological data from the pandemic in Colombia, 5 months after the report of the first case, and tries to explore the reasons behind the apparent success of Colombia in maintaining a low number of COVID-19 cases.
Methods
Study design
This is a descriptive analysis of PCR-confirmed COVID-19 cases that occurred in Colombia from March 2 to July 25, 2020. Epidemiological data are curated by the Colombian National Institute of Health (Instituto Nacional de Salud (INS) in Spanish). Daily updates of the epidemiological data can be found at https://www.ins.gov.co/Noticias/Paginas/Coronavirus.aspx (Instituto Nacional de Salud, 2020a). The INS is the head of the Colombian national surveillance system. It provides technical advice on public health surveillance to local healthcare institutions and coordinates the field investigation of cases and the confirmatory laboratory testing for COVID-19 cases.
Case definitions
Case and severity of disease definitions used for the surveillance of COVID-19 are provided by the INS and can be fully accessed at the following URL: http://www.ins.gov.co/Noticias/Coronavirus/Estrategia%20VSP%20COVID-19%2023072020.pdf. From March to June, RT-PCR was predominantly recommended for symptomatic cases with a history of travel or contact with travelers, despite the fact that local transmission replaced imported transmission starting in April. Only in July were testing criteria expanded to include symptomatic and asymptomatic suspected cases with or without risk factors.
Variables
The INS database contains the following information: (1) dates of symptom onset, sample taking, epidemiological reporting, laboratory diagnosis, recovery, and death; (2) age and sex; (3) city of residence; (4) severity of disease classified as asymptomatic, mild, moderate, and severe; (5) place where health care is provided stratified by hospital care, intensive care unit (ICU), or home care.
Analysis
Data were described according to the level of measurement. Proportions were used for nominal or ordinal variables, and means or medians were used for continuous variables. Incidence rates of confirmed COVID-19 cases were estimated by department (state) and for several municipalities stratified by age and sex. COVID-19 mortality rates were also estimated by department and for selected municipalities stratified by age and sex.
The capacity of the departmental surveillance systems was assessed using several indicators: (1) cumulated proportion of samples taken per million people by department; (2) mean number of positive contacts for every imported case; (3) average interval in days between the onset of symptoms and date of diagnosis; (4) average interval in days from the date when the case was detected to the date of diagnosis.
A conservative assessment of the potential underestimation of cases was done using the following approach: (1) the ratio of samples taken per million people by department and district was estimated and the geographical area with the highest ratio was identified. (2) That ratio was projected to the population of every department/district, in order to estimate the ‘potential number of samples’ that the surveillance system would have obtained if the same effort had been made for every geographical area. (3) The positivity ratio of samples by department was obtained by dividing the number of positive samples in a department/district by the total number of samples taken in that department. (4) A ‘potential number of cases’ by department was obtained by multiplying the ‘potential number of samples’ of a particular department by its positivity ratio (see Supplementary Material Table S1).
A visual analysis of how COVID-19 was disseminated around the country during the first month of transmission was performed by mapping departments and municipalities where local cases – not linked to imported transmission – were detected during March 2020. Also, these territories were aggregated into geographic regions to describe the differential trends in the number of cases (mild, moderate, severe) and deaths (Supplementary Material Figure S1).
All data were analyzed using Microsoft Excel, Epi Info 7.2, Stata 12 (Stata Corporation, College Station, TX, USA), and Python v3.6 (packages: Pandas, Geopandas, Matplotlib, and Seaborn).
Results
General characteristics of COVID-19 cases
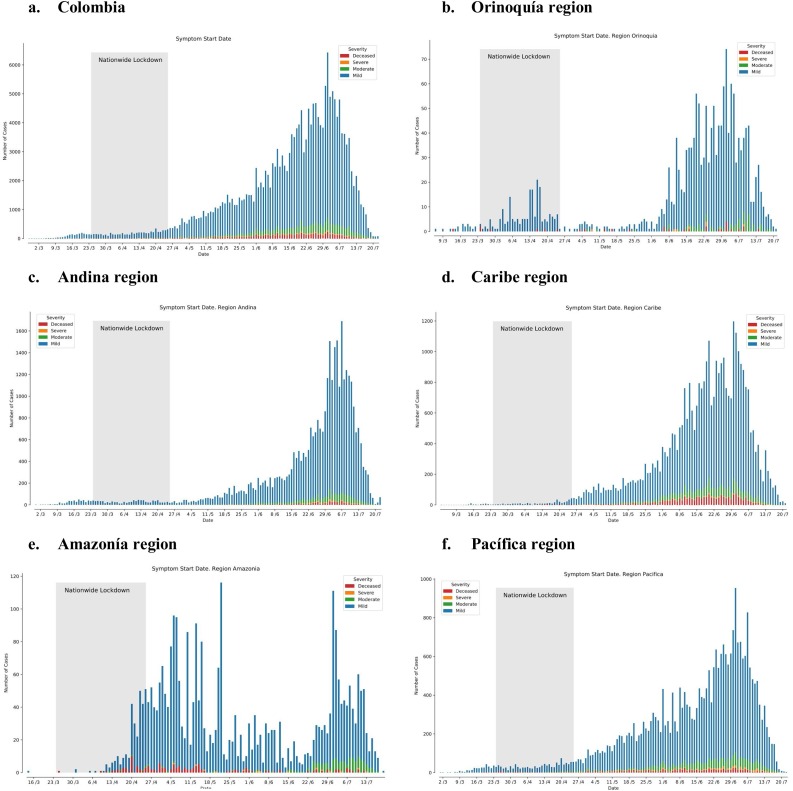
By July 25, Colombia had confirmed 240 795 cases of COVID-19 and 8269 deaths, with differential trends by geographic region (Figure 1). Males accounted for 53.6% of cases, while 72% of cases occurred in persons aged 0–49 years (Table 1 ). Most cases (90.1%) were asymptomatic or presented with mild clinical manifestations, 0.7% were in the ICU and 51.5% have recovered so far. The cumulated incidence of infection was 478 per 105 persons and the average incidence density was 97.6 cases per 105 person-months. The incidence rate was lower among persons <20 years of age (<50 cases per 105 person-months), and it increased to more than 100 cases per 105 person-months among adults >20 years of age. The case incidence was higher in males than in females (524 vs 434 cases per 105 persons, respectively) (Table 2 ).
Figure 1.
Numbers of deaths, cases, and recovered cases by date of onset of symptoms of COVID-19 in Colombia and its regions up to July 25, 2020.
Table 1.
Characteristics of the population with COVID-19; Colombia, July 25, 2020.
| Variable | N = 240 795 | % |
|---|---|---|
| Sex | ||
| Male | 128 979 | 53.6 |
| Female | 111 816 | 46.4 |
| Age (years) | ||
| 0–9 | 8971 | 3.7 |
| 10–19 | 15 546 | 6.5 |
| 20–29 | 52 848 | 21.9 |
| 30–39 | 56 989 | 23.7 |
| 40–49 | 39 251 | 16.3 |
| 50–59 | 31 585 | 13.1 |
| 60–69 | 19 051 | 7.9 |
| 70–79 | 10 182 | 4.2 |
| 80–89 | 6372 | 2.6 |
| Clinical presentations | ||
| Asymptomatic | 32 994 | 13.7 |
| Mild | 183 899 | 76.4 |
| Moderate | 13 626 | 5.7 |
| Severe | 1499 | 0.6 |
| Death | 8269 | 3.4 |
| NA | 508 | 0.2 |
| Healthcare type | ||
| Intensive care unit (ICU) | 1517 | 0.7 |
| Hospitalized | 12 613 | 5.4 |
| Home care | 98 241 | 42.2 |
| Recovered | 119 667 | 51.5 |
| NA | 488 | 0.2 |
| Case type | ||
| Imported | 969 | 0.4 |
| Related | 18 796 | 7.8 |
| In studya | 221 030 | 91.8 |
NA, not available.
Cases likely associated to local transmission, with no link to imported cases.
Table 2.
Incidence, mortality, and fatality in the population with COVID-19, according to age groups; Colombia, July 25, 2020.
| Age (years) | Population in 2020 | Person-months (4.9 months of follow-up) | Cases of COVID-19 | Deaths from COVID-19 | Cumulative incidence ×105 | Incidence density ×105 person-months | CFR (%) | Mortality rate per 105 persons |
|---|---|---|---|---|---|---|---|---|
| Total | ||||||||
| 0–9 | 7 863 825 | 38 532 743 | 8971 | 14 | 114 | 23.3 | 0.2% | 0.2 |
| 10–19 | 8 112 327 | 39 750 402 | 15 546 | 11 | 192 | 39.1 | 0.1% | 0.1 |
| 20–29 | 8 551 856 | 41 904 094 | 52 848 | 107 | 618 | 126.1 | 0.2% | 1.3 |
| 30–39 | 7 470 681 | 36 606 337 | 56 989 | 269 | 763 | 155.7 | 0.5% | 3.6 |
| 40–49 | 6 130 204 | 30 038 000 | 39 251 | 612 | 640 | 130.7 | 1.6% | 10.0 |
| 50–59 | 5 434 890 | 26 630 961 | 31 585 | 1181 | 581 | 118.6 | 3.7% | 21.7 |
| 60–69 | 3 795 322 | 18 597 078 | 19 051 | 1894 | 502 | 102.4 | 9.9% | 49.9 |
| 70–79 | 2 003 827 | 9 818 752 | 10 182 | 2081 | 508 | 103.7 | 20.4% | 103.9 |
| 80+ | 1 009 492 | 4 946 512 | 6372 | 2100 | 631 | 128.8 | 32.9% | 208.0 |
| Total | 50 372 424 | 246 824 878 | 240 795 | 8269 | 478 | 97.6 | 3.4% | 16.4 |
| Male | ||||||||
| 0–9 | 4 018 776 | 19 692 002 | 4523 | 9 | 113 | 23.0 | 0.2% | 0.2 |
| 10–19 | 4 132 721 | 20 250 333 | 8197 | 6 | 198 | 40.5 | 0.1% | 0.1 |
| 20–29 | 4 281 591 | 20 979 796 | 28 123 | 65 | 657 | 134.0 | 0.2% | 1.5 |
| 30–39 | 3 654 091 | 17 905 046 | 31 040 | 167 | 849 | 173.4 | 0.5% | 4.6 |
| 40–49 | 2 916 820 | 14 292 418 | 20 965 | 446 | 719 | 146.7 | 2.1% | 15.3 |
| 50–59 | 2 524 743 | 12 371 241 | 17 021 | 812 | 674 | 137.6 | 4.8% | 32.2 |
| 60–69 | 1 735 695 | 8 504 906 | 10 305 | 1213 | 594 | 121.2 | 11.8% | 69.9 |
| 70–79 | 897 276 | 4 396 652 | 5597 | 1328 | 624 | 127.3 | 23.7% | 148.0 |
| 80+ | 433 169 | 2 122 528 | 3208 | 1193 | 740 | 151.1 | 37.2% | 275 |
| Total | 24 594 882 | 120 514 922 | 128 979 | 5239 | 524 | 107.0 | 4.1% | 21.3 |
| Female | ||||||||
| 0–9 | 3 845 049 | 18 840 740 | 4448 | 5 | 116 | 23.6 | 0.1% | 0.1 |
| 10–19 | 3 979 606 | 19 500 069 | 7349 | 5 | 185 | 37.7 | 0.1% | 0.1 |
| 20–29 | 4 270 265 | 20 924 299 | 24 725 | 42 | 579 | 118.2 | 0.2% | 1.0 |
| 30–39 | 3 816 590 | 18 701 291 | 25 949 | 102 | 680 | 138.8 | 0.4% | 2.7 |
| 40–49 | 3 213 384 | 15 745 582 | 18 286 | 166 | 569 | 116.1 | 0.9% | 5.2 |
| 50–59 | 2 910 147 | 14 259 720 | 14 564 | 369 | 500 | 102.1 | 2.5% | 12.7 |
| 60–69 | 2 059 627 | 10 092 172 | 8746 | 681 | 425 | 86.7 | 7.8% | 33.1 |
| 70–79 | 1 106 551 | 5 422 100 | 4585 | 753 | 414 | 84.6 | 16.4% | 68.0 |
| 80+ | 576 323 | 2 823 983 | 3164 | 907 | 549 | 112.0 | 28.6% | 157.4 |
| Total | 25 777 542 | 126 309 956 | 111 816 | 3030 | 434 | 88.5 | 2.7% | 11.8 |
CFR, case fatality rate.
The case fatality rate (CFR) was 3.4% and the specific cumulated mortality rate was 16.4 per 105 persons. The CFR increased by age group, from less than 1% among younger people (0–39 years) to more than 30% among the oldest (80 years and older). The specific mortality rate also increased from less than 1 per 105 among younger people (<20 years old) to more than 200 per 105 people among the oldest (>80 years old). The CFR was higher among males compared to females (4.3% vs 2.4%, respectively) and the same trend was observed for the mortality rate (21.3 vs 11.8 cases per 105) (Table 2).
All departments had reported cases, but 292 municipalities were apparently free of COVID-19 (26%) and 373 (33.2%) had seen limited transmission. The incidence rate by department ranged from 1.8 to 3160 cases per 105 people, with the highest rate reported in Amazonas (seven times the average national rate), a southern region that shares borders with Brazil and Peru. Another four departments (Atlántico, Caquetá, Cesar, and Sucre) and four special districts (Bogotá DC, Barranquilla DE, Buenaventura DE, and Santa Marta DT) exceeded the national average rate (Table 3 ).
Table 3.
Distribution of cases and death rates by department; Colombia, July 25, 2020.
| Department | Population | Cases | Cumulative incidence ×105 | Deaths | Mortality rate ×106 | CFR (%) |
|---|---|---|---|---|---|---|
| Amazonas | 79 020 | 2497 | 3160.0 | 101 | 1278.2 | 4.0 |
| Antioquia | 6 677 930 | 23 035 | 344.9 | 321 | 48.1 | 1.4 |
| Arauca | 294 206 | 181 | 61.5 | 1 | 3.4 | 0.6 |
| Archipielago of San Andrés, Providencia and Santa Catalina | 63 692 | 33 | 51.8 | – | – | – |
| Atlántico | 1 447 878 | 20 485 | 1414.8 | 961 | 663.7 | 4.7 |
| Barranquilla DE | 1 274 250 | 27 088 | 2125.8 | 1399 | 1097.9 | 5.2 |
| Bogotá DC | 7 743 955 | 81 180 | 1048.3 | 2115 | 273.1 | 2.6 |
| Bolívar | 1 152 240 | 2028 | 176.0 | 93 | 80.7 | 4.6 |
| Boyacá | 1 242 731 | 759 | 61.1 | 25 | 20.1 | 3.3 |
| Buenaventura DE | 311 827 | 1998 | 640.7 | 131 | 420.1 | 6.6 |
| Córdoba | 1 828 947 | 651 | 63.9 | 9 | 8.8 | 1.4 |
| Caldas | 1 018 453 | 542 | 132.0 | 8 | 19.5 | 1.5 |
| Cartagena | 410 521 | 213 | 48.9 | 4 | 9.2 | 1.9 |
| Caquetá DT | 1 028 736 | 14 258 | 1 386 | 440 | 427.7 | 3.1 |
| Casanare | 435 195 | 1501 | 100.6 | 44 | 29.5 | 2.9 |
| Cauca | 1 491 937 | 2447 | 188.9 | 49 | 37.8 | 2.0 |
| Cesar | 1 295 387 | 2802 | 514.4 | 89 | 163.4 | 3.2 |
| Chocó | 544 764 | 3593 | 196.5 | 438 | 239.5 | 12.2 |
| Cundinamarca | 3 242 999 | 6928 | 213.6 | 161 | 49.6 | 2.3 |
| Guainía | 50 636 | 14 | 27.6 | 1 | 19.7 | 7.1 |
| Guaviare | 86 657 | 77 | 88.9 | – | 0.0 | 0.0 |
| Huila | 1 122 622 | 673 | 59.9 | 18 | 16.0 | 2.7 |
| La Guajira | 965 718 | 1757 | 181.9 | 103 | 106.7 | 5.9 |
| Magdalena | 888 414 | 1878 | 211.4 | 181 | 203.7 | 9.6 |
| Meta | 1 063 454 | 2256 | 212.1 | 27 | 25.4 | 1.2 |
| Nariño | 1 627 589 | 6610 | 406.1 | 197 | 121.0 | 3.0 |
| Norte de Santander | 1 620 318 | 1515 | 93.5 | 59 | 36.4 | 3.9 |
| Putumayo | 359 127 | 532 | 148.1 | 22 | 61.3 | 4.1 |
| Quindío | 555 401 | 245 | 44.1 | 6 | 10.8 | 2.4 |
| Risaralda | 961 055 | 1298 | 135.1 | 25 | 26.0 | 1.9 |
| Santa Marta DT | 538 612 | 3049 | 566.1 | 130 | 241.4 | 4.3 |
| Santander | 2 280 908 | 2564 | 112.4 | 64 | 28.1 | 2.5 |
| Sucre | 949 252 | 5119 | 539.3 | 327 | 344.5 | 6.4 |
| Tolima | 1 339 998 | 2049 | 152.9 | 38 | 28.4 | 1.9 |
| Valle del Cauca | 4 220 325 | 18 877 | 447.3 | 681 | 161.4 | 3.6 |
| Vaupés | 44 712 | 61 | 136.4 | 1 | 22.4 | 1.6 |
| Vichada | 112 958 | 2 | 1.8 | – | 0.0 | 0.0 |
CFR, case fatality rate.
Figure 1 shows the epidemic curve for the country and for the five main geographical areas. It suggests that widespread transmission started in June, after the lockdown was relaxed and gradual opening of commercial activities had started. By May 16, after 14 weeks of transmission, Colombia had reported 15 000 cases and 560 deaths, and by June 15, 5 weeks later, the number of cases had tripled (47 000 cases and 1545 deaths). Early peaks of transmission were detected in the Amazon, which started while the lockdown was still in place.
Specific mortality rates by department ranged from 0 in Vichada to 1278 in Amazonas, which had 7.8 times the national rate (Incidence Rate Ratio (IRR) = 7.8, 95% confidence interval (CI) 6.4–9.5). Eight additional areas (Atlántico, Barranquilla DE, Bogotá DC, Buenaventura DE, Caquetá, Chocó, Santa Marta DT, and Sucre) surpassed the national mortality rate (Table 3).
The average age increased with the severity of clinical presentation, being 37.5 years (standard deviation (SD) 17.6 years) for mild disease, 51.9 years (SD 20.5 years) for moderate disease, 54.6 years (SD 19.7 years) for severe clinical presentations, and 68.1 years (SD 16.5 years) for people who died. These differences persisted by geographical area (Table 4 ).
Table 4.
Average age (years) by COVID-19 severity by department; Colombia, July 25, 2020.
| Department | Deaths | Severe | Moderate | Mild | Total |
|---|---|---|---|---|---|
| Amazonas | 68.3 | 54.5 | 48.3 | 35.2 | 36.9 |
| Antioquia | 71.7 | 55.4 | 52.4 | 36.6 | 37.9 |
| Arauca | 42.0 | 19.5 | 36.6 | 28.1 | 28.4 |
| Archipielago of San Andrés, Providencia and Santa Catalina | – | – | – | 37.4 | 37.4 |
| Atlántico | 66.4 | 53.9 | 50.8 | 37.9 | 39.9 |
| Barranquilla DE | 68.0 | 57.3 | 53.8 | 38.5 | 40.7 |
| Bogotá DC | 68.8 | 54.2 | 52.9 | 37.4 | 40.1 |
| Bolívar | 69.3 | 50.0 | 49.6 | 37.2 | 39.7 |
| Boyacá | 69.4 | 59.0 | 50.8 | 38.7 | 41.2 |
| Buenaventura DE | 67.3 | 52.3 | 54.4 | 35.8 | 39.5 |
| Córdoba | 72.1 | 64.0 | 52.7 | 40.2 | 41.5 |
| Caldas | 71.0 | 42.3 | 47.7 | 34.7 | 36.6 |
| Caquetá | 67.4 | 57.6 | 51.5 | 37.6 | 39.1 |
| Cartagena DT | 62.0 | 61.0 | 43.8 | 36.2 | 37.6 |
| Casanare | 69.9 | 54.1 | 50.4 | 35.9 | 38.6 |
| Cauca | 66.2 | 46.1 | 39.2 | 35.2 | 36.2 |
| Cesar | 62.7 | 49.9 | 50.7 | 36.2 | 38.2 |
| Chocó | 67.1 | 53.0 | 50.1 | 39.7 | 44.7 |
| Cundinamarca | 65.0 | 55.2 | 53.1 | 36.7 | 38.8 |
| Guainía | 73.0 | – | – | 27.6 | 33.3 |
| Guaviare | – | – | 46.0 | 26.6 | 27.4 |
| Huila | 70.8 | 66.0 | 48.6 | 38.3 | 39.8 |
| La Guajira | 64.6 | 50.9 | 48.2 | 36.7 | 39.3 |
| Magdalena | 68.8 | 43.3 | 52.7 | 38.9 | 43.4 |
| Meta | 67.6 | 51.7 | 47.3 | 34.5 | 35.6 |
| Nariño | 65.8 | 48.9 | 47.2 | 36.9 | 38.6 |
| Norte de Santander | 64.5 | 48.6 | 52.3 | 38.2 | 40.9 |
| Putumayo | 60.0 | 31.6 | 44.2 | 36.5 | 38.7 |
| Quindío | 70.3 | – | 56.6 | 45.2 | 46.4 |
| Risaralda | 66.6 | 53.2 | 52.8 | 37.0 | 38.4 |
| Santa Marta DT | 66.4 | 49.6 | 48.0 | 37.5 | 39.6 |
| Santander | 68.2 | 62.5 | 53.1 | 36.9 | 39.6 |
| Sucre | 70.4 | 56.4 | 52.0 | 38.1 | 41.9 |
| Tolima | 67.1 | 62.8 | 61.9 | 36.1 | 37.6 |
| Valle del Cauca | 69.7 | 57.1 | 52.4 | 38.1 | 40.6 |
| Vaupés | 70.0 | – | – | 36.1 | 36.9 |
| Vichada | – | – | 78.0 | – | 78.0 |
| Total | 68.1 | 54.6 | 51.9 | 37.5 | 39.8 |
Selected surveillance characteristics
The Colombian surveillance system had taken 1 370 271 samples (27 203 samples per million people), but there was wide variability in the number of samples taken by department (range 2664 to 158 681/106). The positivity ratio (number of cases/number of samples) varied from 0.2% to 79.3%, with a national average of 17% (Supplementary Material Table S1).
It took a median of 11 days to confirm a case from the date of symptom onset (interquartile range (IQR) 2 days) and 5.6 days from the date of case detection by the health system (IQR 1.7 days). A median of 5 days passed from the beginning of symptoms to case detection (IQR 1.9 days) (Supplementary Material Table S2).
By July 25, 92% of Colombian cases were likely linked to local transmission, while imported cases and those related to imported cases represented 0.4% and 7.8%, respectively. Bogotá DC, Antioquia, and Valle del Cauca had most of the imported cases – 68% out of 969 imported cases – detected by surveillance across the country. There were 18 796 imported-related cases and most of them were identified in Bogotá DC (n = 5151), Antioquia (n = 2156), Valle del Cauca (n = 1806), and Meta (n = 1140). At the national level, one imported case was associated with 20 contact cases (related cases) (Supplementary Material Table S3).
Imported cases came from Europe (39%), other Latin American countries (29%), North America (26%), the Middle East (6%), Africa (0.4%), and Australia (0.1%). Spain and the USA were the individual countries from which most imported cases came (258 and 207 cases, respectively). No cases from China were detected.
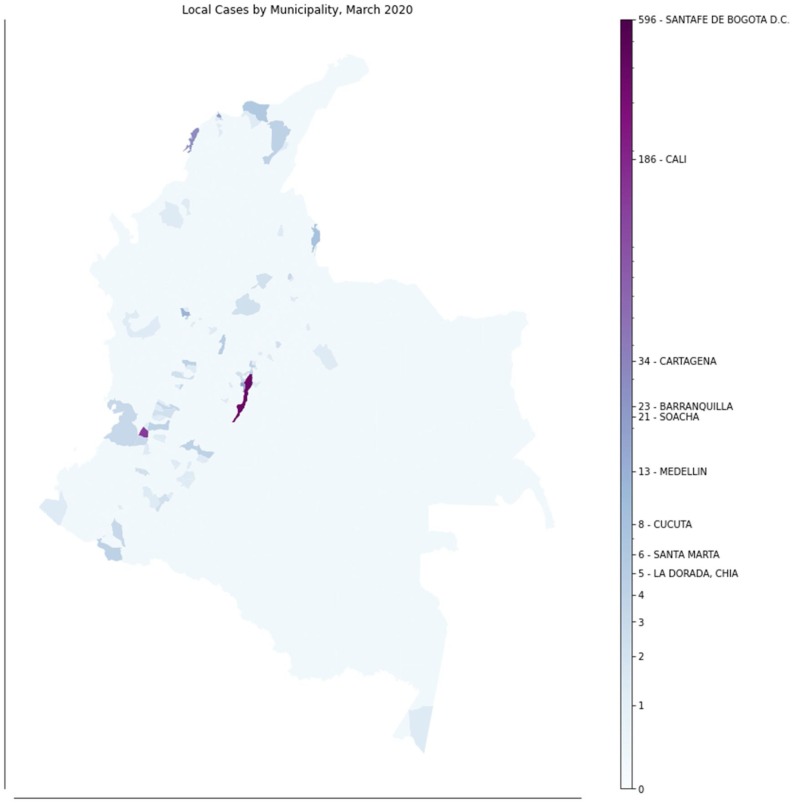
In March, local transmission (cases without a history of travel or contact with travelers) was identified in 14 different geographical areas covering the most populated departments. Only the Eastern area of the country did not report such cases at that time (Figure 2 ).
Figure 2.
Local cases of COVID-19 by municipality, March 2020.
Using a conservative approach to assess the potential underestimation of cases, it was estimated that, by July 25, Colombia should have detected 1 328 175 cases instead of the actual 240 795 observed, an underestimation of 82% (Supplementary Material Table S1).
Discussion
After approximately 140 days of COVID-19 transmission in Colombia, the numbers of cases and deaths were extremely low compared to projections. A mathematical model estimated that 21 237 000 cases and 212 000 deaths would occur in the first 100 days of the epidemic without interventions (Instituto Nacional de Salud, 2020b). However, only 0.3% of forecasted cases and 0.7% of forecasted deaths were reported after those first 100 days.
On comparison to other Latin American countries, Colombia had a lower incidence rate per 105 people (478/105), than Peru (1212/105), Panama (1507/105), Chile (1819/105), Brazil (1157/105), and Bolivia (636/105). Its mortality rate (17/105) was lower than Brazil (42/105), Chile (49/105), Panama (33.8/105), Mexico (33/105), and Ecuador (32.8/105). In addition, it had a higher rate of sampling than most Latin American countries except Chile, Panama, and Uruguay (Hasell et al., 2020).
One factor explaining Colombia’s seeming success in containing the pandemic is the enforcement of a strict lockdown early on. On March 18, 2020, the Colombian government released Decree 420 (Ministerio del Interior) closing schools and universities, cancelling almost all in-person work activities, stopping national and international land and air travel, cancelling all public and private gatherings (of more than six persons), and imposing self-isolation for people over 70 years of age, among other measures (Ministerio del Interior, República de Colombia, 2020a). These regulations were in place until the first week of May, when a reactivation of economic activities began (Ministerio del Interior. República de Colombia, 2020). In addition, Colombia, through the Colombian Association of Infectious Diseases (ACIN, the acronym in Spanish), promptly generated a consensus for the management of COVID-19 cases (Asociación Colombiana de Infectología and IETS, 2020; Marin et al., 2020), establishing criteria to manage cases at home, which may have contributed to decreasing the rate of nosocomial infections, an important source of transmission.
The decision in Colombia to implement an early lockdown contrasted with actions taken by other countries in the region. The governments of Brazil and Mexico ignored the potential threat of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and, as a result, they have been hit hard. However, other countries that implemented lockdowns (Chile and Peru) have also had higher rates of deaths and cases than Colombia, which may be explained by differences in the efficacy of the lockdown, differences in testing, and social and climatic conditions, some of which will need to be studied in the future (Villalobos et al., 2020, Perez-Brumer and Silva-Santisteban, 2020).
There is no experimental evidence on the effectiveness of social distancing measures, but modelling approaches consistently show that they are followed by a sharp decline in cases and deaths (Institute for Health Metrics and Evaluation (IHME), 2020, Kennedy et al., 2020). With our data, we may cite the low number of cases in the department of Cundinamarca as evidence of the success of the lockdown imposed in Bogotá DC, the country’s capital. Bogotá DC is surrounded by a myriad of Cundinamarca’s municipalities, containing around three million people, and there is continuous mobility of people from and to Bogotá DC. The lockdown stopped this mobility, and so far Cundinamarca has had an incidence rate approximately five times lower than Bogotá DC.
Two additional factors may have influenced the low incidence and mortality rates: weather and demographic profile. In Colombia, peaks of respiratory virus transmission and related mortality occur mostly during rainy seasons (Porras Ramírez et al., 2009, Cotes et al., 2012). However, since October 2019, the country has experienced an unusually longer dry season that has extended through June 2020 (El Tiempo, 2020). This year, the rainy season started late in June in most regions of the country, coinciding with the end of the lockdown. The potential role of both factors in the increase in cases and deaths observed after May has yet to be ascertained. In addition, Colombia has a relatively young population, which may have attenuated the SARS-CoV-2 impact on mortality (Amariles et al., 2020).
Underreporting and surveillance weaknesses may also have contributed to hide the real numbers of cases and deaths in Colombia. Colombia kept a conservative case definition (see Methods) for the first 2.5 months of transmission because of shortages in biological and laboratory supplies to perform PCR tests. While stringent criteria for sampling and testing may succeed in keeping demand at bay, they also contribute to the underestimation of cases.
Some surveillance indicators suggest that Colombia may have missed a substantial number of cases. First, the sampling ratio was found to differ widely by department. Results in Supplementary Material Table S1 suggest that if the sampling ratio in Amazonas had been reached by other departments, the number of cases would have increased eight-fold. Second, the ratio of COVID-19-positive contacts per imported case suggests that some departments were unable to track most imported cases. In three departments/districts with the highest incidence rates, the ratio of positive contacts to imported cases was four to 12 times the national average (19 to 1). Although super-spreaders of COVID-19 may exist, large ratios of positive contacts to imported cases suggest a lack of capacity to detect and track all imported cases (Pung et al., 2020).
Although the first imported case was detected on March 2, it is highly likely that transmission started in February or even in late January. The map in Figure 2 shows that there was simultaneous detection of local cases without known links to imported cases in several distant areas in March. One of the first cases reported symptoms on February 29, several days before the first imported case was detected. The role of undetected transmission during February in the subsequent pattern of disease spread is difficult to establish given the limitations in testing during March and April.
Colombia has increased its surveillance capacity. It jumped from taking less than 3000 samples/week in the first week to >600 000 in July (Supplementary Material Table S4). However, wide gaps between departments remain. The three largest cities have 60% (36/60) of the laboratories able to perform PCR testing, whereas 12 out of 33 departments have no such facilities. Public health officials must wait up to 15 days to confirm cases, which hampers their ability to detect and track contacts.
As reported by others, age is one of the strongest predictors of mortality (Cagnacci and Xholli, 2020; Immovilli et al., 2020). Patients who died were on average older (68 years) than those with mild cases (37 years). In Wuhan, the average age among those who died was 68 years (Chen et al., 2020). Wu et al. first reported that the CFR increases with age. However, the CFR in people aged 70 years and older was lower in Wuhan than in Colombia (14% vs 25%) (Wu and McGoogan, 2020).
Mortality in Colombia varied by geographic region and this may have been related to the availability of ICU beds and quality of care. Public discussions have centered around the number of ICUs with ventilators available in the country, and whether there will be enough to cope with the potential demand produced by COVID-19 (Amariles et al., 2020). Another caveat is the availability of healthcare workers. For example, the only hospital covering the Amazonas population (79 020 inhabitants) has five ICU beds with ventilators, but lacks personnel trained in critical care. The impact of these shortcomings is reflected in the high mortality rate observed there (approximately eight times the national average), surpassing even the mortality rates observed in Peru (21/105), Brazil (20/105), and Ecuador (23/105). Regional inequalities in the pandemic response capacity and their relationship to mortality in Colombia, mirror those described in China (Ji et al., 2020).
This analysis has limitations. We did not have access to clinical records of infected individuals. Therefore, it was not possible to assess the role of chronic underlying diseases in the mortality by COVID-19. The INS has published a list of the frequency of comorbidities in COVID-19 patients who have died, including hypertension (28%), diabetes (15%), chronic obstructive pulmonary disease (12%), obesity (8%), history of smoking (5%), and hypothyroidism (4%); 13% have had no underlying diseases. However, it is not possible to know how many concurrent diseases were present in each patient, or how they compare to individuals with milder presentations.
One strength of the present study is that it provides a critical overview of the potential explanations for the apparent success of Colombia in mitigating the effect of the pandemic. As well as discussing the effect of the preventive measures adopted by the government, we have discussed the role that weaknesses in the surveillance system, as well as sociodemographic and climatic factors, may have had in the unexpected positive results. This analysis provides a baseline for monitoring the impact that changes in containment strategy, such as relaxing lockdown measures on May 15, may have on COVID-19 transmission. It may also help to assess the impact of the ongoing improvements in laboratory capacity that Colombia is implementing.
Funding source
The authors received no financial support for this research.
Ethics approval and consent to participate
Ethical approval or individual consent was not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.08.017.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Amariles P., Granados J., Ceballos M., Montoya C.J. COVID-19 in Colombia endpoints. Are we different, like Europe? Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.013. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asociación Colombiana de Hospitales y Clínicas . 2019. Siguen aumentando deudas a hospitales y clínicas por prestación de servicios de salud, ya superan los $10 billones de pesos [Internet]https://achc.org.co/siguen-aumentando-deudas-a-hospitales-y-clinicas-por-prestacion-de-servicios-de-salud-ya-superan-los-10-billones-de-pesos/ [cited 2020 May 21]. Available from: [Google Scholar]
- Asociación Colombiana de Infectología, IETS Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-COV-2/COVID-19 en establecimientos de atención de la salud. Infectio. 2020;24(April (3)):1–153. [Google Scholar]
- Chen T., Wu D., Chen H., Yan W., Yang D., Chen G. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ. 2020:368. doi: 10.1136/bmj.m1091. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagnacci A., Xholli A. Age-related difference in the rate of coronavirus disease 2019 mortality in women versus men. Am J Obstet Gynecol. 2020;223(3):453–454. doi: 10.1016/j.ajog.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotes K., Moreno-Montoya J., Porras-Ramírez A., Rico-Mendoza A., de la Hoz-Restrepo F. Clinical characteristics of patients hospitalized with severe respiratory illness during influenza seasons in the cities of Bogota and Manizales, Colombia 2000-2006. Rev Salud Publica. 2012;14(1) doi: 10.1590/s0124-00642012000100011. [DOI] [PubMed] [Google Scholar]
- Departamento Administrativo Nacional de Estadística . 2018. Censo Nacional de Población y Vivienda.https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/censo-nacional-de-poblacion-y-vivenda-2018 [Internet]. 2018 [cited 2020 May 21]. Available from: [Google Scholar]
- Hasell J., Mathieu E., Beltekian D., Macdonald B., Giattino C., Ortiz-Ospina E. 2020. Coronavirus (COVID-19) Testing - Statistics and Research - Our World in Data. Web page; p. 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immovilli P., Morelli N., Antonucci E., Radaelli G., Barbera M., Guidetti D. COVID-19 mortality and ICU admission: the Italian experience. Crit Care. 2020;24(1):228. doi: 10.1186/s13054-020-02957-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME) 2020. COVID-19 Projections [Internet]https://covid19.healthdata.org/united-states-of-america Available from: [Google Scholar]
- Instituto Nacional de Salud . 2020. Coronavirus Colombia [Internet]https://www.ins.gov.co/Noticias/Paginas/Coronavirus.aspx [cited 2020 May 21]. Available from: [Google Scholar]
- Instituto Nacional de Salud . 2020. Modelo de transmisión de coronavirus COVID-19. Escenarios para Colombia [Internet] Available from: https://www.ins.gov.co/Direcciones/ONS/SiteAssets/Modelo COVID-19 Colombia INS_v5.pdf. [Google Scholar]
- Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Heal. 2020;8(4):e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy D.M., Zambrano G.J., Wang Y., Neto O.P. Modeling the effects of intervention strategies on COVID-19 transmission dynamics. J Clin Virol. 2020:104440. doi: 10.1016/j.jcv.2020.104440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin J.E.G., Castellanos J., Rodriguez-Morales A.J., Cardona-Ospina J.A., Duarte J.E.F., Mattar S. Ad-hoc group consensus recommendations on the evaluation and quality control of molecular and serological diagnostics tests for SARS CoV-2 human infection*. Infectio. 2020;24(May (3)) [Google Scholar]
- Ministerio de Salud y Protección Social . 2018. Comportamiento del aseguramiento [Internet]https://www.minsalud.gov.co/proteccionsocial/Regimensubsidiado/Paginas/coberturas-del-regimen-subsidiado.aspx [cited 2020 May 21]. Available from: [Google Scholar]
- Ministerio del Interior . 2020. República de Colombia. Decreto 457 de 2020 [Internet]https://id.presidencia.gov.co/Paginas/prensa/2020/Gobierno-Nacional-expide-Decreto-457-mediante-el-cual-imparten-instrucciones-para-cumplimiento-Aislamiento-Preventiv-200323.aspx [cited 2020 May 27]. Available from: [Google Scholar]
- Ministerio del Interior. República de Colombia . 2020. Decreto número 689 de 2020 [Internet]https://id.presidencia.gov.co/Paginas/prensa/2020/Gobierno-expide-decreto-sobre-ampliacion-del-Aislamiento-Preventivo-Obligatorio-hasta-el-31-de-mayo-200523.aspx Available from: [Google Scholar]
- Pan American Health Organization . 2020. Cumulative suspected and confirmed COVID-19 cases reported by countries and territories in the Americas [Internet]https://ais.paho.org/phip/viz/COVID19Table.asp [cited 2020 Aug 2]. Available from: [Google Scholar]
- Perez-Brumer A., Silva-Santisteban A. COVID-19 Policies can Perpetuate Violence Against Transgender Communities: Insights from Peru. Aids Behav. 2020;1:3. doi: 10.1007/s10461-020-02889-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porras Ramírez A., Rico Mendoza A., Moreno Montoya J., Cótes K., López J.D., Herrera D. Mortalidad asociada con las temporadas de mayor circulación de los virus de la influenza en Bogotá, Colombia, 1997-2005. Rev Panam Salud Pública. 2009;26:435–439. doi: 10.1590/s1020-49892009001100008. [DOI] [PubMed] [Google Scholar]
- Pung R., Chiew C.J., Young B.E., Chin S., Chen M.I.C., Clapham H.E. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395(March (10229)):1039–1046. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiempo El. 2020. “Lluvias en Colombia para junio y julio seguirán por debajo de lo normal”: Ideam - Medio Ambiente - Vida - ELTIEMPO.COM. Newspaper. [Google Scholar]
- Villalobos P., Browne J., Madero-Cabib I. It Is Not Just Mortality: a Call from Chile for Comprehensive COVID-19 Policy Responses among Older People | The Journals of Gerontology: Series B | Oxford Academic. J Gerontol. 2020:1–6. doi: 10.1093/geronb/gbaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Rolling updates on coronavirus disease (COVID-19) [Internet]https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [cited 2020 May 21]. Available from: [Google Scholar]
- World Health Organization . 2020. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]https://covid19.who.int/table [cited 2020 Jul 25]. Available from: [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. Feb. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.