Abstract
Background
The number of women entering the medical and healthcare workforce globally has increased in the past several decades. Women have many roles and positions in healthcare organizations, hospitals and healthcare education settings. Although there has been an increase in the number of women, female workers continue to face many workplace challenges. This scoping review aimed to explore the challenges female healthcare professionals face in the workforce.
Methods
A scoping review utilizing Arksey and O’Malley’s six-step framework was undertaken to identify and map available literature addressing challenges faced by female healthcare professionals in the workforce. The databases searched included Embase, EmCare, Medline, Cumulative Index of Nursing and Allied Health Literature (CINAHL) and Business Source Complete (BSC). Additional searches were performed using Google Scholar, Trove and grey literature.
Results
The initial search yielded 2455 publications (Medline n=369; EmCare n=276; Embase n=612; CINAHL n=1088; Business Source Complete n=109; mixed grey literature n=1). After removal of duplicates, 1782 citations remained. Abstract and title screening reduced the field to 36 publications, following which full-text reviews were conducted. Consensus was reached on 16 publications for final review. After analyzing the articles, three themes were identified: i) family responsibilities, ii) workplace environment and iii) stereotyping.
Conclusion
Findings confirm that female healthcare professionals face circumstances that may affect their family lives, as well as factors relating to the workplace environment and stereotypes. Implementing strategies such as reduced work hours, flexible timing and part-time work can support women in the workplace, which then enhances and supports gender equality in healthcare organizations.
Keywords: female, healthcare providers, family responsibilities, workplace, stereotype
Introduction
The number of women entering the medical and healthcare workforce globally has increased over the past several decades.1 In Australia, 79% of people employed in the healthcare and social assistance workforce are women,2 while in the United States (US) 78.4% of workers in the healthcare and social assistance workforce are women.3 Of note is that female healthcare professionals are distributed unequally across different clinical professions such as medicine, nursing and physiotherapy. For example, in the United Kingdom (UK) more than 89.4% of the nursing and midwifery workforce is female,4 and 93% of nurses in the US are female,5 while in Canada it is reported that 41% of physicians are female6 and just over one-third of Australian doctors are women.7
Women have many roles and positions in healthcare organizations, hospitals and healthcare education settings,8 such as doctors, nurses, midwives and administrators.9,10 For example, Petek et al11 reported that 65% of doctors in Slovenia were women and the ratio of male to female in general practice was 1:5, while in Latvia the percentage of female doctors was 74.3%.12 Treister-Goltzman and Peleg13 reported that females’ jobs in hospitals were located in all important areas, such as laboratories and radiological departments. However, figures from the UK National Health Service (NHS) showed that women held only 36% of senior positions in pharmacy departments (where 61% of pharmacists are female), which means gender equality has not been reached.14 Batchelor14 claimed that the importance of diversity in the workplace should facilitate all staff being able to balance their careers with their family life, regardless of gender.
Female healthcare workers globally continue to face many challenges in the workplace15 such as family duties, poor human resource policies and gender inequalities that hinder their professional growth.13,15–17 Work–family balance was highlighted as a significant barrier to career advancement in many countries. For example, Azeem and Akhtar18 reported that the perception of work interfering with family life was negatively related with work commitment (r= −.681, p=0.001) and job satisfaction (r= −.488, p=0.001) among Indian healthcare workers; for 46% of women their commitment to their job was impaired and for 24% job satisfaction was affected by work interfering with family life.
According to Desai et al19 and Hong Lu et al,20 women in health fields face challenges related to poor work environments, which include unequal pay, unsatisfactory working conditions, limited opportunities for career advancement, work-related stress and unfavorable policies that promote patriarchy. Moreover, Desai et al19 reported that women in the US earned less than their male counterparts despite having equal output, amount of work, academic qualifications and experience. Examples of this have been detailed by female nurses, who have reported dealing with unfriendly workplaces that present few opportunities to advance their careers, as well as experiencing work–family balance challenges that hinder career progress and affect their lifestyle causing stress and excessive tiredness.21–23 A systematic review of gender differences in surgical skills acquisition reported that gender-related differences were more pronounced among medical students.24 Future surgical curricula needed to consider tailoring personalized programs that accommodated more mentoring and one-on-one training for female physicians.24
To our knowledge, there is no recent comprehensive literature review undertaken to collectively explore challenges faced by female healthcare professionals around the world. Therefore, a scoping review was conducted to explore these challenges.
Methods
A scoping review is using manual search to identify and map available literature on a selected topic. In this scoping review, the researchers used the six methodological steps described by Arksey and O’Malley.25 The steps are: 1) identify the research question; 2) identify relevant studies; 3) select studies; 4) chart the data; 5) collate, summaries and report the results; and 6) consult experts. The scoping review approach systematically maps and reviews existing literature on a selected topic,26 including literature from peer-reviewed and non-peer reviewed literature or grey literature.
Identify the Research Question
The research question guiding the scoping review was: What challenges do female healthcare professionals face in the workforce?
Identify Relevant Studies
Five databases were used to search for relevant articles: Medline, EmCare, Embase, Cumulative Index of Nursing and Allied Health Literature (CINAHL), and Business Source Complete (BSC). Additionally, we searched the following websites: Google Scholar www.scholar.google.com, Trove www.trove.nla.gov.au and the grey literature website www.greylit.org. The search strategy used a list of MeSH terms and keywords and was verified by an expert librarian (Table 1). We limited our search strategy to English language studies. The searches resulted in 2455 records, which were exported to EndNote X8 for screening.
Table 1.
Search Strategy Including MeSH and Keywords
| MeSH: Challenges |
MeSH: Female |
MeSH: Healthcare professionals |
MeSH: Workforce |
|---|---|---|---|
| Keyword: barriers obstacles |
Keyword: women gender woman |
Keyword: healthcare professionals, allied health, nurs*, doctor*, physician*, paramedic*, physiotherapy*, occupational therapy*, psychiatrist, laboratories*, dentists* radiologist* |
Keyword: workplace career |
Note: *Truncation.
Study Selection
Articles were considered for inclusion if they met the following criteria: 1) quantitative, qualitative or mixed-method in design; 2) addressed challenges or obstacles faced by female healthcare professionals in the workforce in any healthcare-related discipline; 3) full-text peer-reviewed articles reported in English language.
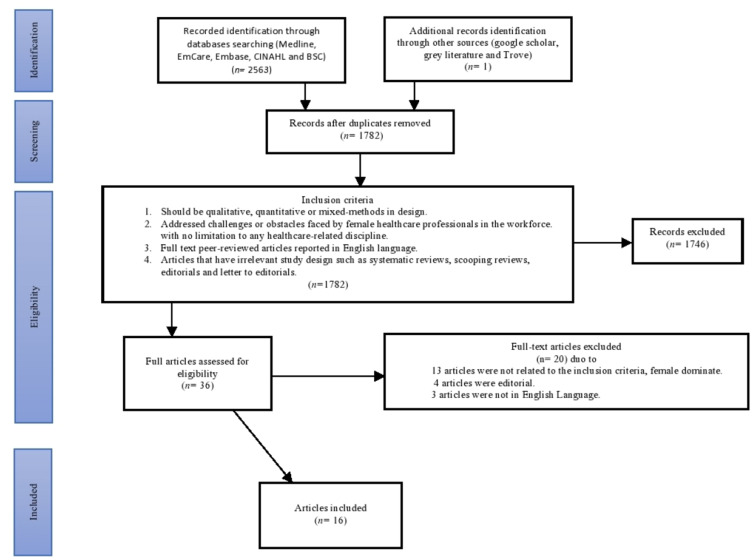
We excluded articles that had unsuitable study designs such as systematic reviews, scoping reviews, editorials and letters to the editor. The search yield from the databases was: Medline (n=369), EmCare (n=276), Embase (n=612), CINAHL (n=1088), BSC (n=109), and mixed grey literature (n=1). After the removal of all duplicates (n=673) and irrelevant studies and reviewing all relevant abstracts, the selection process was conducted at two levels: title and abstract review and full-text review. The titles and abstracts of selected studies were independently screened (AMA and EK) based on the inclusion criteria. In the second stage, the full text of potentially eligible studies (n=36) was assessed and inclusion confirmed by two authors (AMA and BW). The resulting 36 articles were reviewed again by both authors and further 20 articles were excluded following discussion surrounding the inclusion criteria. The remaining 16 articles were included in the scoping review. A PRISMA flowchart of article selection is presented in Figure 1.
Figure 1.
Flow chart of study selection.
Charting the Data
This stage of the Arksey and O’Malley framework allows data extraction from included studies for more descriptive data. A narrative review method was used to extract the data from each study. Narrative reviews summarize studies from which conclusions can be drawn into more holistic interpretations.27 The data included: author and year of publication, country the study was conducted in, area of the study, study design or type, sample size, and results and themes emerging from the study. After full-text review and synthesis of the 16 articles, three themes emerged: i) family responsibilities, ii) workplace environment and iii) stereotyping.
Collating, Summarizing and Reporting Results
The data extracted from the included studies are reported in Table 2. It presents data on the different findings, explaining workforce challenges facing women in healthcare. Key outcome data from each of the included studies are presented as well as some of the challenges and barriers that women face to be a member of the healthcare workforce. Family responsibilities, workplace environment and stereotyping were the themes extracted from the analysis.
Table 2.
Studies Selected for Inclusion
| No | Author/ year | Country | Discipline | Aim of the study | Study design and participants | Key outcomes | Theme |
|---|---|---|---|---|---|---|---|
| 1 | Sayres, M., et al.[33] (1986) |
UK | Medicine | To identify possible barriers to women physicians wishing to continue with medical careers. | Mixed methods: cross-sectional questionnaire (n=63) |
This study characterized the experience of pregnancy during residency at a group of Harvard-affiliated teaching hospitals and identified problems for both male and female residents that needed to be addressed. It is important that residency training programs reflect sensitivity to issues that are a natural and expected part of all our lives. | Family responsibilities |
| 2 | Barnett, R.C. & Garies, K.C.[34] (2000) |
USA | Medicine | To examine two hypotheses:
|
Mixed methods (in-depth interview and survey) 104 predominantly white, female, reduced-hours physicians in dual-earner couples with children. n=31 retested after 1-3 months |
Job-role quality was a significant predictor of life satisfaction, whereas the number of hours was not. In the reduced-hours, physicians experienced more rewards than concerns in their careers. |
Family responsibilities |
| 3 | Farahat, F.[32] (2009) | Egypt | Medicine | To explore challenges faced by Egyptian female physicians as they pursue their careers and find different ways of coping with these challenges. | Cross-sectional study (Questionnaire that included open and closed questions) 300 Egyptian female physicians. |
Challenges reported by physicians were either work or family related. Participating physicians dealt with challenges in different ways: deciding on a small family size (82.3%), recruitment of a babysitter/housekeeper (76.3%), and sharing in family income (62%). | Family responsibilities |
| 4 | Adisa, T.A., et al.[31] (2014) |
Nigeria | Medicine and nursing | To investigate challenges and realities of work–family balance among Nigerian female doctors and nurses in their efforts to balance work and family obligations. | Case study (interview) (n=131 female medical workers, comprising 60 female doctors and 71 female nurses) |
Multiple roles was very difficult for Nigerian female doctors and nurses. in Nigeria, the primary responsibility of Female doctors and nurses was to take care of her home and family while every other activity including her job was classified as a secondary role. |
Family responsibilities |
| 5 | Lane, N. & Piercy, N.[44] (2003) |
UK | Nursing | To identify organizational mindsets that militate against women’s career advancement. | Mixed methods Questionnaire (n=597) and “Three sets of 10–12 nurses were interviewed on a group basis, one group in each hospital. Also, seven nurse managers were interviewed individually at each of the three units”. |
Ethic of discrimination are maintained and perpetuated unequal outcomes for women in nursing. The results suggested that to attempt radical change would be to risk severe damage to the human infrastructure of the organization and hence its ability to effectively undertake its tasks. |
Workplace environment |
| 6 | Baker, S.R., et al.[56] (2006) |
USA | Radiology | To determine if the trend of women choosing radiology as a career differed from that for other medical specialties, and if there were differences on the basis of the gender of program directors or geographic location. | Descriptive study (186 female radiology residents) |
The percentage of women in this profession has remained remarkably constant at or slightly above 25%. Small but increasing numbers of women were found to be chairing academic radiology departments. |
Workplace environment |
| 7 | Mobilos S., et al.[37] (2008) |
Canada | Medicine | To examine experiences of women physicians with regard to the interplay between career and lifestyle choices and discover how women’s experiences had evolved during the previous three decades. | Phenomenological study using semi-structured interviews (12 female physicians) |
Three main challenges emerged: lifestyle and career choices, family planning and career trajectory, and seeking balance. All participants described the constant struggle they experienced to balance their personal and professional lives. |
Workplace environment |
| 8 | Nomura, K. & Gohchi, K.[39] (2012) |
Japan | Medicine | To investigate whether experiences and perceptions of gender-based career obstacles among women in Japan were associated with their working status. | Cross-sectional survey (1,513 female physicians) |
Being married and having children were significantly associated with part-time practice, indicating that domestic responsibilities still acted as strong obstacles that may discourage women physicians from working full-time. | Workplace environment |
| 9 | Nomura, K., et al.[57] (2015) |
Japan | Medicine | To investigate difficulties Japanese female doctors faced in continuing professional practice. | Cross-sectional survey (359 female doctors) |
Female doctors were struggled with long working hours due to a shortage of doctors in Japan. Poor working conditions with poor child support, and stereotypical views on gender roles are the main factors to reduced female doctors in Japan. |
Workplace environment |
| 10 | Price, K. & Clearihan, L.[7] (2015) |
Australia | Medicine | To explore female general practitioners’ (GPs’) perceptions of possible barriers to leadership and professional roles in the workforce. | Cross-sectional study (30 female general practitioners) |
Lack of energy and geographic location were key barriers for the participation of female GPs. Female GPs also often lacked self-confidence to speak up. Energy limitations and lack of self-confidence restricting women’s capacity to engage in leadership roles. |
Workplace environment |
| 11 | Phillips, J., et al.[41] (2016) |
USA | Medicine | To explore how physicians balance their professional and personal lives. | Phenomenological study using semi-structured interviews (25 female family physicians) | Female doctors had experienced challenges in balancing the demand of work with the needs of family life. Female rural physicians faced conflict between their professional demands and family lives. Women with young children and those new to rural practice described this as stressful. |
Workplace environment |
| 12 | Petek, D., et al.[11] (2016) | Slovenia | Medicine | To explore options and capabilities of women GP specialist trainees in coordinating their families and careers. | Phenomenological study using semi-structured interviews (10 female general practitioners) |
Specialist experienced high levels of stress at work due to the nature of profession, weaknesses in the healthcare system, personal traits, inexperience and interpersonal relations with colleagues and superiors. An additional burden was the needs of their families and/or children, housework and other obligations. | Workplace environment |
| 13 | Pfleiderer, B., et al.[42] (2018) |
European countries Italy, Germany, France, Norway, Poland, Lithuania, and Netherlands |
Medicine | To increase the number of women in academic medicine who can serve as mentors, role models and ambassadors of change and institutional change is of major importance. | Narrative review | Reducing recruitment barriers for women in all areas of healthcare, improving gender planning, flexible working schedules, fostering career progression, reducing gender imbalances and strengthening gender dimensions are all factors to improve female physicians’ experience of their career. | Workplace environment |
| 14 | Meghen, K., et al.[38] (2013) |
Ireland | Medicine | To capture female representation at all levels of medicine and to establish factors influencing career choice and progression. | Mixed methods study Interviews (25 female hospital specialists) Questionnaire (1,606 female specialist trainees) |
Findings indicated that females who completed specialist training were wary of pursuing either flexible training or part-time work options and experienced discrimination. Balancing motherhood and work commitments was the biggest challenge faced by female doctors with children and caused some to change career pathways. |
Workplace environment |
| 15 | Yamazaki, Y., et al.[48] (2011) |
Japan | Medicine | To explore challenges facing Japanese physician–mothers in efforts to identify solutions for their retention. | Cross-sectional study using questionnaire approach (249 female physicians) |
Challenges facing physician–mothers mainly comprised factors associated with Japanese society, family responsibilities and work environment. Japanese society, epitomized by traditional gender roles, was a powerful social barrier for female physicians who wished to continue working after they were married and had children. |
Stereotyping |
| 16 | Tlaiss, H.[49] (2013) |
Lebanon | Medicine and nursing | To explore barriers that hindered and enablers that fostered women’s career advancement in the healthcare sector. | Qualitative study, semi-structured, face-to-face, in-depth interviews (10 female healthcare managers) |
Discriminatory cultural values, gendered social roles and expectations in Middle Eastern societies, and illustrated their role as barriers hindering women’s career advancement. Spill-over effect of societal expectations and cultural gender stereotypes into the organizational realm, resulting in widely experienced attitudinal and structural organizational barriers. |
Stereotyping |
Consultation (Optional)
Two experts were contacted by email to provide any input to ensure there were no other studies missed. Neither expert suggested any additional literature.
Discussion
This scoping review explored the challenges faced by female healthcare professionals in the workforce. These will be discussed in three broad themes: challenges faced in balancing work and family responsibilities; challenges faced due to workplace issues such as lack of supportive policies and gender equality; and challenges faced in stereotyping of working women. All 16 reviewed articles mentioned these common challenges and confirmed that they were present and commonly experienced by female healthcare workers. Therefore, although the percentage of women joining the healthcare workforce has increased over recent years,28,29 female workers still face many impediments in their work lives that have a negative impact on their quality of life at work and at home.30
The scoping review clarifies that challenges are not mutually exclusive and often overlap. This may suggest that a lack of effective policies (workplace environment) often breeds stereotyping issues against working women and disrupts their work–life balance (family responsibilities). Although most of the studies were categorized under the theme of “workplace environment” and comparatively fewer studies categorized under “family responsibility” and “stereotyping”, they are all thematically interlinked.
Family Responsibilities
The four articles thematically listed under family responsibilities’ were undertaken in the UK, the US and Egypt in medicine and in Nigeria in medicine and nursing. These articles were tied with a singular idea that women health professionals struggle to balance their work and home, being torn between opposing expectations of their professions and family duties. For example, Adisa et al.31 conducted semi-structured interviews with Nigerian female doctors and nurses and identified how most (95%) acknowledged the negative impact of their profession on their family lives in a patriarchal society. Adisa et al31 described how Nigeria’s male-dominated society did not welcome the idea of women working professionally and, even if they did, that work should not come ahead of family priorities. The authors also noted that Nigerian women had to face domestic crises, family problems and social sanctions – such as humiliating behavior from relatives and family members – if they prioritized careers over familial duties. Another study by Farahat32 was conducted among female physicians in Egypt through self-administered questionnaires that used open and closed questions to identify challenges of work–life conflict. The cohort reported not being able to afford time to specialize in their medical careers because they had to maintain child-rearing and housekeeping duties.32
The challenges faced by female healthcare professionals in Nigeria and Egypt were primarily socio-cultural and in line with the stereotyping theme. Challenges faced by women in the UK and US were mostly related to stress in the workplace, including how medical institutions were under-prepared to meet the needs of pregnant physicians, sometimes even seeing program directors turning hostile towards their pregnant trainees.33
The Barnett and Gareis34 study of married female physicians with children (n=104) comprised an online survey using the 38-item reduced-hours job-role quality scale and face-to-face interviews. The main finding was that subjective reduced-hours job-role quality was a significant predictor of life satisfaction, whereas the number of hours worked per se was not. Another report indicated that women could tailor their workload and hours based on their needs; for example, in Australia, pregnant women can discuss the issue with their employers and find solutions to reduce their work hours while pregnant.35,36
Barnett and Gareis34 presented two hypotheses – the scarcity hypothesis and the enhancement hypothesis – to decide the level of overall fulfilment for women physicians. The scarcity hypothesis was based on longer working hours, meaning less family time and low life satisfaction, whereas the enhancement hypothesis balanced work and family, which suggests women gain rewards and life satisfaction.34 This study drew favor for the enhancement hypothesis, although many of the women opted for reduced work hours to resolve their work–family conflict. This could perhaps be explained by the fact that all respondents had employed spouses and the study was based in a progressive developed country.
Workplace Environment
The studies grouped under the workplace environment theme were undertaken in the UK, the US (two articles), Canada, Japan (two articles), Australia, Slovenia, Germany and Ireland, and addressed the healthcare professions of medicine, nursing and radiology. Some articles discussed long working hours and female physicians looking for flexible work hours or part-time work in different professions such as nursing and medicine.37–42 However, Lane & Piercy (2003) found that female nurses in the UK National Health Service faced major barriers in achieving fairness and equal opportunities in leadership because male managers deliberately behaved badly. For example, some managers disregarded female workers who spoke with them about unsatisfactory work that would lead to stressful environments in the workplace. Many leaders believed that women should not be allowed to progress into higher positions in their professions.43 The authors suggested that to attempt radical change would risk severe damage to the human infrastructure of the organization and hence its ability to effectively undertake its tasks.44
In addition to workplace issues, there are also issues related to stereotyping as identified in the scoping review themes. Gender stereotyping sometimes leads to self-silencing by female healthcare professionals, who are demotivated to even speak in meetings.7 Price and Clearihan7 attributed such self-silencing to lack of energy and confidence stemming from psychological repression in workplaces. Women are under-represented in leadership positions/roles in the healthcare system, including healthcare organizations.8,45,46 In Australia, where women now comprise more than one-third of the medical workforce, two factors may be restricting women’s capacities to engage in leadership roles: energy limitations and lack of self-confidence.7 This means that female professionals need to increase their motivation, which will increase their energy and confidence to speak up.47
The presence of obstacles, such as inappropriate working-hour schedules, prevents women from working and getting jobs,42 which could have a substantial negative effect on female motivation to work effectively.39 There are strategies that reduce this effect, such as reduced/flexible work hours to help achieve balance with personal roles and supportive relationships with spouses and parents. Both strategies facilitate women’s ability to be available to their patients and maintain clear boundaries between personal and professional space, providing adequate time for parenting, recreation and rest.41
Stereotyping
Two articles addressed the stereotyping theme, Yamazaki et al48 and Tlaiss,49 and were undertaken in Japan in the medical discipline and Lebanon in medical and nursing disciplines, respectively. Stereotyping does not exist in isolation and is embedded deeply within socio-cultural practices.50 While some societies and cultures, such as Japan and the Middle East, demonstrate greater conservatism in terms of female workforces,48,49 most western nations are open to the idea of women working.51
Tlaiss49 and Yamazaki et al48 studied obstacles that women faced in the Middle East and Japan. Tlaiss49 found that the healthcare sector in the Middle East would continue to under-represent women in the workplace due to cultural beliefs. For example, Saudi women believe that taking responsibility of kids and home while Saudi male taking care of income and expenses.52 In Japan, the cultural perspective on gender is influenced by society, family responsibility and work environment, which affects women’s careers because of their culture and political representation.48 For example, Japanese women faced unprofitable income due to the government tax policies and company, so they prefer to be at home and the husband providing salary and benefits.53 Both nations are driven by patriarchal, masculine values, whereby domestic responsibilities should be a woman’s foremost priority.54,55
Therefore, Tlaiss49 and Yamazaki et al48 reported that organizational barriers to female doctors were only an extension of larger socio-cultural expectations. To overcome these barriers, the researchers noted a need for external help (daycare, relatives, caregivers, etc.), although encouraging husbands to take on more responsibilities within the family was also helpful.48 Gender discrimination would never improve unless local government and authorities came forward and drove an instrumental effort to establish change and different expectation settings for women.49
Limitations and Future Research
Although the scoping review yielded 16 articles, there are several limitations that should be declared. First, some articles or references may have been missed due to using specific MeSH-terms/keywords. Additionally, we searched five of the most important databases in the healthcare field so some articles might have been missed. To address these limitations, we employed strategies such as manual searching, grey literature searches and expert advice to ensure key information was included in this review. Finally, we limited our search to include only studies conducted in English so this might have led to missing some relevant studies in other languages. More research is needed to further investigate the themes raised in this study. For example, a theoretical framework that integrates the themes of this study with a theory such as glass ceiling, gendered organizations theory and institutional theory can be researched in the future to help improve the status of female healthcare professionals in their workplace.
Conclusion
This scoping review aimed to describe the challenges faced by female healthcare professionals in the workplace. The 16 articles yielded information categorized under three broad thematic headings – family responsibilities, workplace environment and stereotyping. Although separated by theme, there was an apparent link across the themes and articles reviewed. For example, the workplace environment, such as inadequate support for women, led to work–life imbalance and affected family responsibilities, whereas stereotyping and discrimination led to stress, low productivity and low life satisfaction. Low life satisfaction affects all functions of an individual, personally and professionally. Therefore, implementing strategies such as reduced work hours, flexible timing and part-time work may contribute to highly motivated women in the workplace, which will, in turn, enhance and support gender equality across healthcare organizations.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Heron A More women than ever are in the workfore but progress has been glacial; 2016. Available from: https://theconversation.com/more-women-than-ever-are-in-the-workforce-but-progress-has-been-glacial-54893. Accessed February19, 2019.
- 2.Australian Bureau of Statistics. Gender indicators, Australia, Sep 2018; 2018. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4125.0~Sep%202018~Main%20Features~Economic%20Security~4. Accessed February17, 2019.
- 3.Bureau of labor statistics labor force statistics from the current population; 2019. Available from: https://www.bls.gov/cps/cpsaat18.htm. Accessed February20, 2019.
- 4.Punshon G, Maclaine K, Trevatt P, Radford M, Shanley O, Leary A. Nursing pay by gender distribution in the UK - does the Glass Escalator still exist? Int J Nurs Stud. 2019;93:21–29. doi: 10.1016/j.ijnurstu.2019.02.008 [DOI] [PubMed] [Google Scholar]
- 5.Barrett-Landau S, Henle S. Men in nursing: their influence in a female dominated career. J Leadersh Instr. 2014;13:10–13. [Google Scholar]
- 6.Canadian Institute for Health Information. A profile of physicians in Canada; 2017. Available from: https://www.cihi.ca/en/a-profile-of-physicians-in-canada-2017. Accessed February18, 2019.
- 7.Price K, Clearihan L Exploring female GPs’ perceptions about medical leadership; 2015. Available from: https://search-informit-com-au.ezproxy.lib.monash.edu.au/fullText;dn=213668411833510;res=IELHEA. Accessed February19, 2019. [PubMed]
- 8.Lantz PM. Gender and leadership in healthcare administration: 21st century progress and challenges. J Healthc Manag. 2008;53(5):292–301. doi: 10.1097/00115514-200809000-00004 [DOI] [PubMed] [Google Scholar]
- 9.EL-Sanabary N. The education and contribution of women health care professionals in Saudi Arabia: the case of nursing. Soc Sci Med J. 1993;37(11):1331–1343. doi: 10.1016/0277-9536(93)90163-X [DOI] [PubMed] [Google Scholar]
- 10.Schueller-Weidekamm C, Kautzky-Willer A. Challenges of work–life balance for women physicians/mothers working in leadership positions. Gend Med. 2012;9(4):244–250. doi: 10.1016/j.genm.2012.04.002 [DOI] [PubMed] [Google Scholar]
- 11.Petek D, Gajsek T, Petek Ster M. Work-family balance by women GP specialist trainees in Slovenia: a qualitative study. BMC Med Educ. 2016;16:31. doi: 10.1186/s12909-016-0551-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldman S. Female doctors by country, the statistics portal; 2018. Available from: https://www.statista.com/chart/14983/female-doctors-by-country/. Accessed February18, 2019.
- 13.Treister-Goltzman Y, Peleg R. Female physicians and the work-family conflict. Isr Med Assoc J 2016;18(5):261–266. [PubMed] [Google Scholar]
- 14.Batchelor H Women under represented in senior pharmacy and NHS roles the pharmaceutical journal; 2018. Available from: https://www.pharmaceutical-journal.com/news-and-analysis/news/women-underrepresented-in-senior-pharmacy-and-nhs-roles/20204515.article?firstPass=false. Accessed February17, 2019.
- 15.Al‐Riyami M, Fischer I, Lopez V. Nurses’ perceptions of the challenges related to the Omanization policy. Int Nurs Rev. 2015;62(4):462–469. doi: 10.1111/inr.12221 [DOI] [PubMed] [Google Scholar]
- 16.Alilu L, Zamanzadeh V, Fooladi MM, Valizadeh L, Habibzadeh H. Towards an understanding of clinical nurses challenges that leads intention to leave. Acta Paulista De Enfermagem. 2016;29(5):534–541. doi: 10.1590/1982-0194201600074 [DOI] [Google Scholar]
- 17.Sells JM, Sells CJ. Pediatrician and parent: a challenge for female physicians. Pediatrics. 1989;84(2):355–361. [PubMed] [Google Scholar]
- 18.Azeem SM, Akhtar N. The influence of work life balance and job satisfaction on organizational commitment of healthcare employees. Int J Hum Resour Stud. 2014;4(2):18. doi: 10.5296/ijhrs.v4i2.5667 [DOI] [Google Scholar]
- 19.Desai T, Ali S, Fang X, Thompson W, Jawa P, Vachharajani T. Equal work for unequal pay: the gender reimbursement gap for healthcare providers in the United States. Postgrad Med J. 2016;92(1092):571–575. doi: 10.1136/postgradmedj-2016-134094 [DOI] [PubMed] [Google Scholar]
- 20.Hong Lu K, Barriball L, Zhang X, While A. Job satisfaction among hospital nurses revisited: a systematic review. Int J Nurs Stud. 2011;49:1017–1038. doi: 10.1016/j.ijnurstu.2011.11.009 [DOI] [PubMed] [Google Scholar]
- 21.Mackusick C, Minick P. Why are nurses leaving? Findings from an initial qualitative study on nursing attrition. Medsurg Nurs. 2010;19(6):335–341. [PubMed] [Google Scholar]
- 22.Younas M, Rattani S. Harassment: a challenge at workplace. Imanagers J Nurs. 2014;4(1):35–39. doi: 10.26634/jnur.4.1.2630 [DOI] [Google Scholar]
- 23.Kerr HL, Armstrong LA, Cade JE. Barriers to becoming a female surgeon and the influence of female surgical role models. Postgrad Med J. 2016;92(1092):576–580. doi: 10.1136/postgradmedj-2015-133273 [DOI] [PubMed] [Google Scholar]
- 24.Ali A, Subhi Y, Ringsted C, Konge L. Gender differences in the acquisition of surgical skills: a systematic review. Surg Endosc. 2015;29(11):3065–3073. doi: 10.1007/s00464-015-4092-2 [DOI] [PubMed] [Google Scholar]
- 25.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 26.Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 28.Auerbach DI, Buerhaus PI, Staiger DO. Registered nurse supply grows faster than projected amid surge in new entrants ages 23–26. Health Aff. 2011;30(12):2286–2292. doi: 10.1377/hlthaff.2011.0588 [DOI] [PubMed] [Google Scholar]
- 29.Elston M women and medicine: the future; 2009. Available from: http://www.learning.ox.ac.uk/media/global/wwwadminoxacuk/localsites/oxfordlearninginstitute/documents/overview/women_and_medicine.pdf. Accessed February19, 2019.
- 30.Al-Asfour A, Tlaiss HA, Khan SA, Rajasekar J. Saudi women’s work challenges and barriers to career advancement. Career Dev Int. 2017;22(2):184–199. doi: 10.1108/CDI-11-2016-0200 [DOI] [Google Scholar]
- 31.Adisa TA, Mordi C, Mordi T. The challenges and realities of work-family balance among Nigerian female doctors and nurses. Economic Insights - Trends Challenges. 2014;66(3):23–37. [Google Scholar]
- 32.Farahat F. Challenges facing female physicians in Egypt. Arch Environ Occup Health. 2009;64(2):121–127. doi: 10.3200/AEOH.64.2.121-128 [DOI] [PubMed] [Google Scholar]
- 33.Sayres M, Wyshak G, Denterlein G, Apfel R, Shore E, Federman D. Pregnancy during residency. N Engl J Med. 1986;314(7):418–423. doi: 10.1056/NEJM198602133140705 [DOI] [PubMed] [Google Scholar]
- 34.Barnett RC, Gareis KC. Reduced-hours job-role quality and life satisfaction among married women physicians with children. Psychol Women Q. 2000;24(4):358–364. doi: 10.1111/j.1471-6402.2000.tb00218.x [DOI] [Google Scholar]
- 35.Victorian Equal Opportunity and Human Right Commission. Pregnancy and work: know your right and obligations. Victorian Equal Opportunity and Human Rights Commission; 2017. Available from: https://www.humanrightscommission.vic.gov.au. Accessed February21, 2019.
- 36.Australian Human Rights Commission. Pregnancy guidelines 2001. Australian Human Rights Commission; 2001. Available from: https://www.humanrights.gov.au/publications/pregnancy-fact-sheet. Accessed February19, 2019.
- 37.Mobilos S, Chan M, Brown JB. Women in medicine: the challenge of finding balance. Can Fam Physician. 2008;54(9):1285–6.e5. [PMC free article] [PubMed] [Google Scholar]
- 38.Meghen K, Sweeney C, Linehan C, O’Flynn S, Boylan G. Women in hospital medicine: facts, figures and personal experiences. Ir Med J. 2013;106(2):39–42. [PubMed] [Google Scholar]
- 39.Nomura K, Gohchi K. Impact of gender-based career obstacles on the working status of women physicians in Japan. Soc Sci Med. 2012;75(9):1612–1616. doi: 10.1016/j.socscimed.2012.07.014 [DOI] [PubMed] [Google Scholar]
- 40.Nomura K, Yamazaki Y, Gruppen L, Horie S, Takeuchi M, Illing J. The difficulty of professional continuation among female doctors in Japan: a qualitative study of alumnae of 13 medical schools in Japan. BMJ Open. 2015;5(3):(no pagination)(e005845). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Phillips J, Hustedde C, Bjorkman S, et al. Rural women family physicians: strategies for successful work-life balance. Ann Fam Med. 2016;14(3):244–251. doi: 10.1370/afm.1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pfleiderer B, Bortul M, Palmisano S, Rodde S, Hasebrook J. Improving female physician’s careers in academic medicine: chances and challenges. Best Pract Res Clin Anaesthesiol. 2018;32(1):15–23. [DOI] [PubMed] [Google Scholar]
- 43.Morley L. Lost leaders: women in the global academy. High Educ Res Dev. 2014;33(1):114–128. doi: 10.1080/07294360.2013.864611 [DOI] [Google Scholar]
- 44.Lane N, Piercy NF. The ethics of discrimination: organizational mindsets and female employment disadvantage. J Bus Ethics. 2003;44(4):313–325. doi: 10.1023/A:1023644602447 [DOI] [Google Scholar]
- 45.Weil PA, Mattis MC. To shatter the glass ceiling in healthcare management: who supports affirmative action and why? Health Serv Manage Res. 2003;16:224–233. doi: 10.1258/095148403322488928 [DOI] [PubMed] [Google Scholar]
- 46.Eiser BJ, Morahan P. Fixing the system: breaking the glass ceiling in health care. Leadership in Action. 2006;26(4):8–13. doi: 10.1002/lia.1171 [DOI] [Google Scholar]
- 47.Barsh J, Cranston S, Craske RA. Centered leadership: how talented women thrive. McKinsey Q. 2008;4:35–48. [Google Scholar]
- 48.Yamazaki Y, Kozono Y, Mori R, Marui E. Difficulties facing physician mothers in Japan. Tohoku J Exp Med. 2011;225(3):203–209. doi: 10.1620/tjem.225.203 [DOI] [PubMed] [Google Scholar]
- 49.Tlaiss HA. Women in healthcare: barriers and enablers from a developing country perspective. Int J Health Policy Manag. 2013;1(1):23–33. doi: 10.15171/ijhpm.2013.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hodges A Opportunities for women: challenging harmful social norms and gender stereotypes to unlock women’s potential; 2017. Available from: https://www.unilever.com/Images/unilever-opportunities-for-women_tcm244-500987_en.pdf. Accessed February25, 2019.
- 51.Kollmeyer C. Family structure, female employment, and national income inequality: a cross-national study of 16 western countries. Eur Sociol Rev. 2012;29(4):816–827. doi: 10.1093/esr/jcs060 [DOI] [Google Scholar]
- 52.Alotaibi F, Cutting R, Morgan J. A critical analysis of the literature in women’s leadership in Saudi Arabia. Int J Bus Adm Res. 2017;3(1):29. doi: 10.24178/ijbamr.2017.3.1.29 [DOI] [Google Scholar]
- 53.Okura Gagné N. Neoliberalism at work: corporate reforms, subjectivity, and post-Toyotist affect in Japan. Anthropol Theory. 2019;1463499618807294. [Google Scholar]
- 54.Metcalfe BD. Women, management and globalization in the Middle East. J Bus Ethics. 2008;83(1):85–100. doi: 10.1007/s10551-007-9654-3 [DOI] [Google Scholar]
- 55.Echabe AE. Role identities versus social identities: masculinity, femininity, instrumentality and communality. Asian J Soc Psychol. 2010;13(1):30–43. doi: 10.1111/j.1467-839X.2010.01298.x [DOI] [Google Scholar]
- 56.Baker SR, Barry M, Chaudhry H, Hubbi B. Women as radiologists: are there barriers to entry and advancement? J Am Coll Radiol. 2006;3(2):131–134. doi: 10.1016/j.jacr.2005.10.001 [DOI] [PubMed] [Google Scholar]
- 57.Nomura K, Yamazaki Y, Gruppen LD, Horie S, Takeuchi M, Illing J. The difficulty of professional continuation among female doctors in Japan: a qualitative study of alumnae of 13 medical schools in Japan. BMJ Open. 2015;5(3):e005845. doi: 10.1136/bmjopen-2014-005845 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Heron A More women than ever are in the workfore but progress has been glacial; 2016. Available from: https://theconversation.com/more-women-than-ever-are-in-the-workforce-but-progress-has-been-glacial-54893. Accessed February19, 2019.
- Australian Bureau of Statistics. Gender indicators, Australia, Sep 2018; 2018. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4125.0~Sep%202018~Main%20Features~Economic%20Security~4. Accessed February17, 2019.
- Bureau of labor statistics labor force statistics from the current population; 2019. Available from: https://www.bls.gov/cps/cpsaat18.htm. Accessed February20, 2019.
- Canadian Institute for Health Information. A profile of physicians in Canada; 2017. Available from: https://www.cihi.ca/en/a-profile-of-physicians-in-canada-2017. Accessed February18, 2019.
- Price K, Clearihan L Exploring female GPs’ perceptions about medical leadership; 2015. Available from: https://search-informit-com-au.ezproxy.lib.monash.edu.au/fullText;dn=213668411833510;res=IELHEA. Accessed February19, 2019. [PubMed]
- Feldman S. Female doctors by country, the statistics portal; 2018. Available from: https://www.statista.com/chart/14983/female-doctors-by-country/. Accessed February18, 2019.
- Batchelor H Women under represented in senior pharmacy and NHS roles the pharmaceutical journal; 2018. Available from: https://www.pharmaceutical-journal.com/news-and-analysis/news/women-underrepresented-in-senior-pharmacy-and-nhs-roles/20204515.article?firstPass=false. Accessed February17, 2019.
- Elston M women and medicine: the future; 2009. Available from: http://www.learning.ox.ac.uk/media/global/wwwadminoxacuk/localsites/oxfordlearninginstitute/documents/overview/women_and_medicine.pdf. Accessed February19, 2019.
- Victorian Equal Opportunity and Human Right Commission. Pregnancy and work: know your right and obligations. Victorian Equal Opportunity and Human Rights Commission; 2017. Available from: https://www.humanrightscommission.vic.gov.au. Accessed February21, 2019.
- Australian Human Rights Commission. Pregnancy guidelines 2001. Australian Human Rights Commission; 2001. Available from: https://www.humanrights.gov.au/publications/pregnancy-fact-sheet. Accessed February19, 2019.
- Hodges A Opportunities for women: challenging harmful social norms and gender stereotypes to unlock women’s potential; 2017. Available from: https://www.unilever.com/Images/unilever-opportunities-for-women_tcm244-500987_en.pdf. Accessed February25, 2019.