Dear Editor
Aerosol-generating procedures may expose physicians and nurses to pathogens causing respiratory infections.1 Although nebulizer administration may represent a less significant infection risk, close-range viral aerosol generation remains a considerable concern.2 Current guidance for the management of patients with COVID-19 infection suggests that a negative airflow room is preferred during aerosol nebulization treatment and that physicians and nurses should wear gowns, gloves, N95 respirators and eye protection.2 , 3 Medicated aerosols should be limited to strict indications, as alternative routes of administration may include breath-actuated nebulizers with exhalation filters or metered dose inhalers with valved holding chambers.3 However, the availability of negative airflow rooms or specific types of nebulizers could be scarce. Although a metered dose inhaler could have a lesser aerosol spreading effect, its use for patients with respiratory distress is generally limited. We therefore developed a novel, reusable mask for patients with respiratory infection that can prevent possible aerosol spread during nebulization treatment.
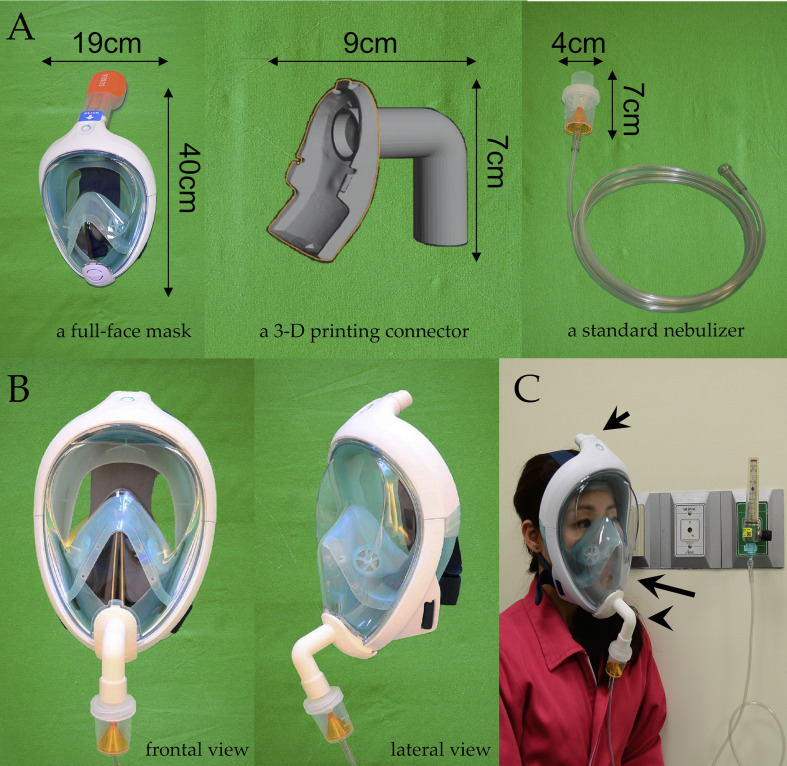
The novel nebulizer mask consists of three components, including a full-face mask, a 3-D printing connect, and a standard nebulizer (Fig. 1 A). We used a full-face mask (Decathlon® Surface Snorkeling Mask Easybreath) as the main mask body. We then removed the vent valve protector and reverted the membrane of the vent valve from outside to inside in the same hole, creating a one-way airflow system. Finally, we used 3-D printing to connect the new mask to a standard nebulizer. Fig. 1B demonstrates the frontal and lateral views of the assembled mask.
Figure 1.
The device consists of a full-face mask, a 3-D printing connect, and a standard nebulizer (Fig. 1A). Fig. 1B demonstrates the frontal and lateral views of the mask. The newly designed inlet (Fig. 1C, arrowhead) renders a shorter oxygen supply pathway. Nebulized medications are concentrated inside the mouth space of the mask (Fig. 1C, long arrow). The contaminated air is only allowed to pass out via the top orifice of the mask (Fig. 1C, short arrow).
We designed a new oxygen inlet (Fig. 1C, arrowhead) for nebulizer. The inlet renders a shorter oxygen supply pathway; thus, the medicine could be delivered into the pre-mouth area directly, though the aerosol delivery efficacy may require further validation. This novel mask allows nebulized medications to concentrate inside the mouth space of the mask (Fig. 1C, long arrow). The contaminated air that the patient breaths out is only allowed to pass out via the top orifice of the mask, which connects to a 3-D-printed adapter with a HEPA filter (Fig. 1C, short arrow).4 , 5 Previous studies showed the modified snorkel mask for medical use did not cause hypercapnia.4 , 7 The tightness and safety of the mask body with 3-D adaptors had been validated in previous studies.4 , 6 Thus, the mask can prevent the contaminated aerosol from spreading outside of the mask.
The nebulizer mask has several advantages. First, the mask is easy to wear. The silicone face border of the mask has a good face fit to prevent droplet or aerosol leakage and is comfortable for patients for prolonged use.
Second, the mask can relieve logistical burden during pandemics. The body of the mask can be reusable after adequate sterilization. The adaptors and connectors of the mask are replaceable as necessary. Since aerosols are contained during nebulization treatment, the risk of physicians and nurses being exposed to pathogens is decreased, which is especially important when personal protection equipment is insufficient. The mask and the connector are reusable after being sanitized with 70% ethyl alcohol or 0.5% sodium hypochlorite.7
Third, the mask is applicable for other medical needs. With proper adjustment and the utilization of connectors, the mask can be converted into an oxygen supply device. The seal of the mask can reduce the risk of respiratory infection when patients use high-flow oxygen, which can generate aerosols as well.
This newly designed nebulizer mask can provide a safer environment for physicians and nurses during nebulized therapy and other aerosol-generating treatments.
Funding and support
This study was supported by the Taiwan Ministry of Science and Technology (MOST 109-2327-B-006 -008).
Writing assistance
None.
Author contributions
Chih-Hao Lin and Chia-Lung Kao conceived the study. Chih-Hao Lin and Chia-Lung Kao drafted the manuscript. Chih-Hao Lin is the corresponding author who takes responsibility for the paper as a whole.
Declaration of competing interest
The authors report no conflicts of interest.
References
- 1.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PloS One. 2012;7(4):e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minnesota Department of Health . 2020. Aerosol-Generating Procedures and Patients with Suspected or Confirmed COVID-19.https://www.health.state.mn.us/diseases/coronavirus/hcp/aerosol.pdf Available at: [Google Scholar]
- 3.Amirav I., Michael T. Newhouse Transmission of coronavirus by nebulizer: a serious, underappreciated risk. CMAJ. Mar. 2020;192(13):E346. doi: 10.1503/cmaj.75066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greig P.R., Carvalho C., El-Boghdadly K., Ramessur S. Safety testing improvised COVID-19 personal protective equipment based on a modified full-face snorkel mask. Anaesthesia. 2020 Apr 10 doi: 10.1111/anae.15085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lisickis R. 2020. Italian Engineers Turn Snorkeling Masks into Life-Saving Ventilators.https://www.boredpanda.com/ventilator-scuba-masks-conversion-coronavirus/?utm_source=google&utm_medium=organic&utm_campaign=organic Available at: [Google Scholar]
- 6.Germonpre P., Van Rompaey D., Balestra C. Evaluation of protection level, respiratory safety, and practical aspects of commercially available snorkel masks as personal protection devices against aerosolized contaminants and SARS-CoV2. Int J Environ Res Publ Health. 2020;17(12):E4347. doi: 10.3390/ijerph17124347. Published 2020 Jun 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]