Abstract
Objective:
The purpose of this study was to determine the effectiveness of the Broselow tape in the evaluation of pediatric trauma patients.
Methods:
The trauma registry of a rural level I trauma center was examined. All pediatric trauma patients 16 years or younger were reviewed from 2002 to 2006, totaling 2358 patients. The Broselow tape measures to 146.5 cm. Patients whose height correlated with the tape and had their heights and weights in the medical record were included. The constant variable was the heights by which the estimated weights of the Broselow tape were compared with the actual weights of the patients.
Results:
A total of 657 patients matched this height and had both heights and weights in their record. Most children (349/657; 53.1%) fell outside the predicted weight range, and of these, 77.1% of the actual weights were greater than those predicted by the Broselow scale. This is observed across all age groups. In patients with heights less than 75 cm, two thirds of patients’ weights correlated with the Broselow estimated weight; however, those that deviated did so by 2 to 3 color intervals larger. This deviation was statistically significant in all groups.
Conclusions:
In our population, the Broselow tape is an ineffective tool to predict weight in more than 50% of pediatric trauma patients. This may lead to the underdosing of emergency medications and blood products.
Keywords: Broselow tape, length based tape, pediatric resuscitation, pediatric trauma
Dosing of drugs in the pediatric population is based largely on the weight of the patient. In the trauma setting, weighing patients on a scale is not feasible, and weight estimations are done under stressful conditions, resulting in an increased likelihood of dosing errors.1,2 Research has also shown weight estimations by physicians and nurses to be unreliable.3,4 There have been conflicting results as to a parent’s ability to estimate the weight of his/her child.3,5 The Broselow6 tape is one of the most widely used methods of length-based resuscitation tape (LBT) recommended by Pediatric Advanced Life Support and the Advanced Trauma Life Support to reduce medication errors during simulated pediatric emergencies.2
Nationwide, 36.6% of the general population is overweight, with a body mass index 25 to 30 kg/m2, and 26.6% is obese, with a body mass index greater than 30 kg/m2. This is a particular problem in West Virginia, where 36.9% of the population is overweight, and 31.9% is obese.7 In the United States, 12.5 million children are overweight in the United States—more than 17%. This prevalence has nearly tripled for adolescents in the past 2 decades.8
Recently, the accuracy of the Broselow tape has come into question, largely secondary to the growing problem of obesity in the pediatric population.9–12 Nieman et al9 found that the Broselow tape was accurate in predicting the correct weight only 55% to 60% of the time and is more likely to underestimate the correct dose of the drug to be given.
The goal of this study was to determine the degree of inaccuracy of the Broselow tape at estimating weight in a pediatric population at a rural level I trauma center.
METHODS
The study protocol was approved by the West Virginia University institutional review board with a waiver of consent. A review of the trauma registry of a university, rural level I trauma center was undertaken.
All pediatric trauma patients from 2002 to 2006 were evaluated. A total of 2359 records were identified. Patients excluded were those with incomplete data (n = 1455), of which 1398 patients had the height (in centimeters) and weight (in kilograms) recorded. Seven hundred forty-one patients had heights exceeded the tape and were excluded. Of these, 657 patients had heights within the parameters of the Broselow tape (<146.5 cm). Actual heights were plotted on the Broselow tape to determine the estimated weight and corresponding color zone. Patient’s actual weights were compared with the predicted weights from the Broselow pediatric emergency tape.
Each color zone of the Broselow tape, version 2007B, was measured with a measuring tape on a hard surface6 (Table 1). This was performed 3 separate times with a tape graduated in 1-mm increments.
TABLE 1.
Broselow Pediatric Emergency Tape (Product No. AE-4800)
| Color | Height, cm | Estimated Weight, kg |
|---|---|---|
| Gray | 46–60.5 | 3–5 |
| Pink | 60.5–67.5 | 6–7 |
| Red | 67.5–75 | 8–9 |
| Purple | 75–85 | 10–11 |
| Yellow | 85–98 | 12–14 |
| White | 98–110 | 15–18 |
| Blue | 110–122 | 19–23 |
| Orange | 122–133.5 | 24–29 |
| Green | 133.5–146.5 | 30–36 |
Determination of statistical significance was performed by analysis of variance.13 Post hoc comparison of individual concentration means with the control was completed using the Tukey-Kramer multiple comparisons test.14 All data are reported means and SDs. The data were analyzed using SigmaStat (SPSS Inc, Chicago, Ill) for Windows. Statistical significance was defined as P < 0.05.
RESULTS
In all, 657 patients were identified with heights less than 146.5 cm. Patient weights were correlated with predicted weights from the Broselow tape. Figure 1 plots each individual patient’s weight with relation to the Broselow ranges. Most (349/657; 53.1%) fell outside the predicted weight range. Figure 2 shows the correlation and noncorrelation of this patient population. Of these, 77.1% of the actual weights were greater than those predicted by the Broselow scale, and 22.9% (80/349) were less.
FIGURE 1.
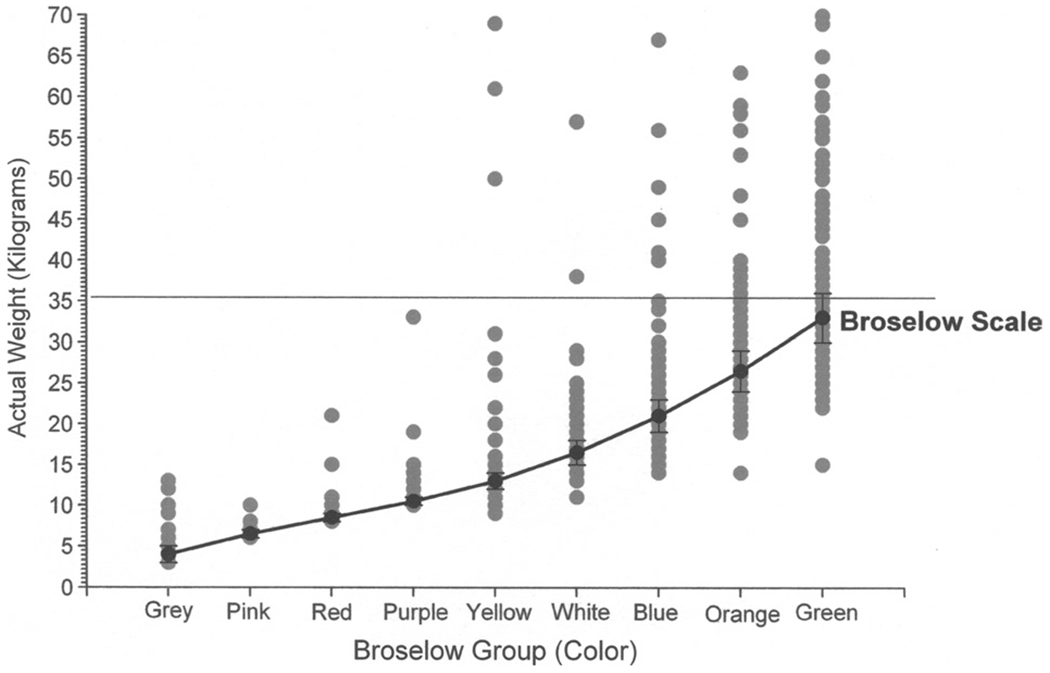
Scatter plot of individual weight correlation with Broselow ranges.
FIGURE 2.
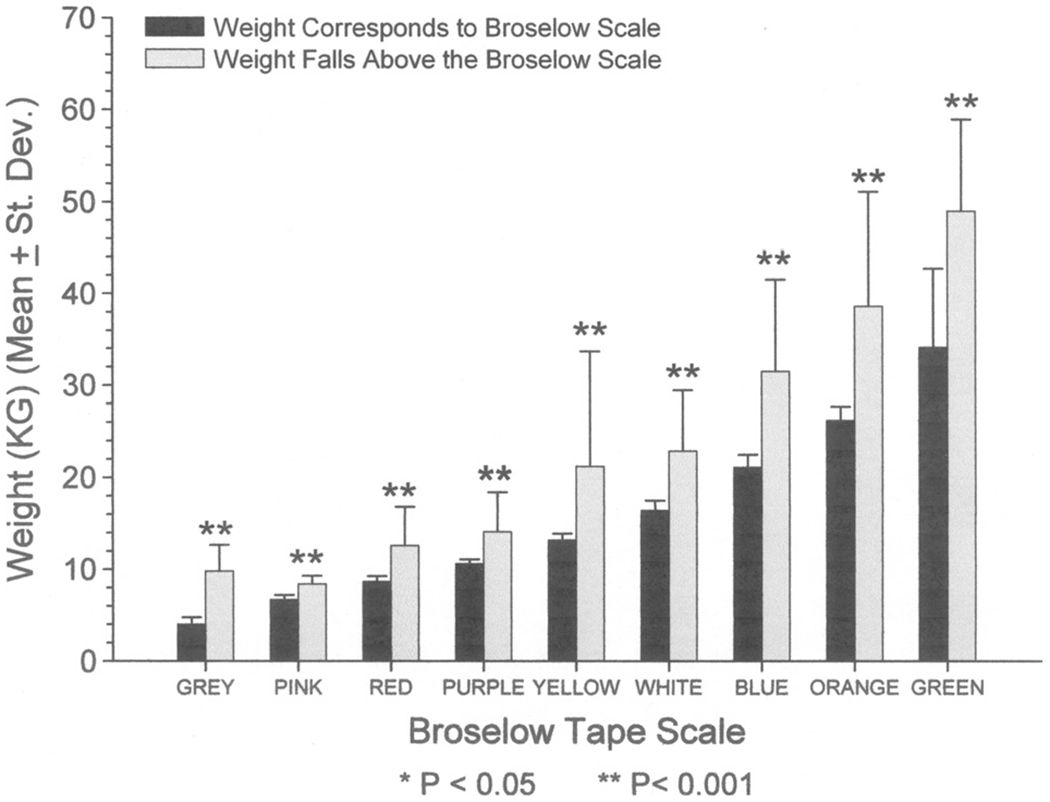
Correlation and noncorrelation of the patient population.
In the patient groups with heights greater than 75 cm (29.5 in, purple region), 46.0% of patient’s actual weight correlated with the Broselow estimated weight (Table 2). In these patients, those that deviated did so by just 1 color interval. In patients with heights less than 75 cm, two thirds of patients’ weights correlated with the Broselow estimated weight; however, those that deviated did so by 2 to 3 color intervals greater (Fig. 3). This deviation was statistically significant in all groups.
TABLE 2.
Evaluation of the Validity of Broselow Correlation in Trauma Patients
| Color | Estimated Weight (kg) | Patients With Correlating Weights, Mean (SD), n | Patients With Weight Above the Broselow, Mean (SD), n |
|---|---|---|---|
| Gray | 3–5 | 4.0 (0.76), 22 | 9.8 (2.86),† 7 |
| Pink | 6–7 | 6.73 (0.47), 11 | 8.4 (0.89),† 5 |
| Red | 8–9 | 8.65 (0.61), 17 | 12.6 (4.18),* 7 |
| Purple | 10–11 | 10.61 (0.50), 18 | 14.12 (4.26),† 25 |
| Yellow | 12–14 | 13.2 (0.70), 39 | 21.19 (12.5),† 37 |
| White | 15–18 | 16.41 (1.13), 44 | 22.88 (6.63),† 40 |
| Blue | 19–23 | 21.14 (1.35), 56 | 31.53 (9.96),† 34 |
| Orange | 24–29 | 26.2 (1.47), 41 | 38.6 (12.49),† 54 |
| Green | 30–36 | 34.08 (8.6), 60 | 49.0 (9.86),† 60 |
P < 0.01.
p ≤ 0.001.
FIGURE 3.
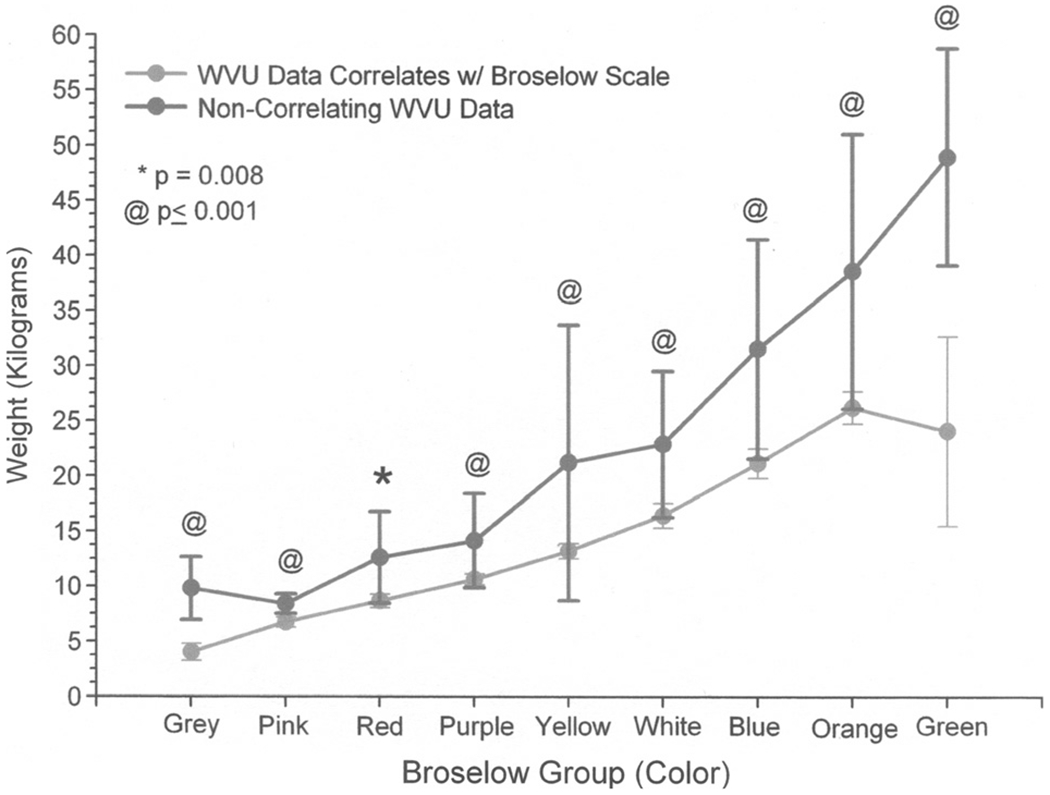
Noncorrelation patients and degree of deviation from Broselow scale.
DISCUSSION
The resuscitation of children requires an accurate and rapid measure of the child’s weight to provide doses of various drugs and fluid boluses. Care must be taken to provide a therapeutic drug dose, without overdosing or underdosing, placing the patient at risk of toxicity or ineffectiveness, respectively. Pediatric Advanced Life Support15 and Advanced Trauma Life Support16 provide national standardized recommendations for resuscitation and recommend the Broselow tape be used to estimate a child’s weight. This has recently come into question in the face of a growing obesity problem.
Our data indicate that the Broselow tape underestimates the weight of children. This underestimation is across all age groups. The best correlation is in the youngest and smallest of patients, but in this group, those children who deviated from the tape were overweight. As our patients age, their deviation from the predicted weight becomes more pronounced.
In our population, Broselow tape–guided resuscitations would potentially be compromised and prolonged secondary to underdosing. For example, most of our patients with body lengths falling into the red zone have actual weights that are far beyond the Broselow tape–predicted value of 5 to 8 kg. Dosing was underestimated in an overweight 3-year-old child from our sample population whose length placed her into the red region of the Broselow tape but placed her in the white region for weight at 15 kg (Table 3).
TABLE 3.
An Example Patient
| Drug | Dose Given Per Broselow Tape if in Red Region | Dose Given Per Broselow Tape if in White Region |
|---|---|---|
| Versed, mg | 2.5 | 5 |
| Propofol, mg | 25 | 50 |
| Atropine, mg | 0.17 | 0.33 |
| Epinephrine (1:10,000), mg | 0.085 | 0.17 |
| Fluid bolus, mL | 170 | 325 |
| Blood bolus, mL | 85 | 165 |
| First/second dose, J | 9/17 | 33/66 |
The first article to validate the Broselow tape in 1988 was that of a multicenter study.4 Recent studies have shown the Broselow tape to be an accurate predictor of weight in the youngest and smallest children.17–21 However, several studies have shown LBT to underestimate a child’s weight, particularly as age increases.22 A large study from Ohio looked at 7813 urban and suburban children.9 The weight of 55.3% of children was accurately predicted (within 10%) using the LBT but were 2.5 to 4.4 times more likely to underestimate drug dosages in 4 age categories and underdosed medications in nearly one third of all children. Medication dosages were accurately predicted in only 55% to 60% of cases.9
Recent National Health and Nutrition Examination Survey data show that the prevalence of overweight children aged 2 to 5 years currently is 13.9%, which increased from 5.0% in 1980. For children aged 6 to 11 years, the prevalence is 18.8%, which increased from 6.5% in 1980. For those aged 12 to 19 years, the prevalence is 17.4%, which increased from 5.0% in 1980. For obesity, 12.4% of children aged 2 to 5 years, 17.0% aged 6 to 11 years, and 17.6% aged 12 to 19 years are currently obese.23 Approximately 36.4% of children aged 10 to 17 years are overweight or obese, and 26.6% of low-income children aged 2 to 5 years in West Virginia are overweight or obese.7
Although numerous recent articles have questioned the accuracy of LBT, an argument can be made that many medications are distributed in lean body mass, and dosing should be based on ideal body weight as predicted by the Broselow tape and not actual weight. When goal-directed therapy is instituted, end points may be achieved less quickly.24–26 Early shock reversal is associated with decreased morbidity and mortality,27 and it might be inferred that systematic underdosing of medications and interventions may place these children at an increased risk of an adverse outcome.
A few authors have looked at adjuncts or alternatives for patients who are expected to be overweight. Yamamoto et al28 described using a body habitus model by which 5 or 6 body habitus icons supplemented length-based weight estimate tools for weight estimations. DuBois et al12 used the devised weight estimation method that correlated to actual weight but underestimates weights in the weight classes greater than 20 kg. A multidisciplinary approach to pediatric trauma care increases weight documentation and decreases adverse medical events.29 This is the current practice at our institution.
As with any study, our study had certain limitations. Within the period during which the trauma patients in this hospital series were admitted, the obesity prevalence among children in West Virginia was 13.9% to 18.8%, depending on age range.7 Although one can geographically define a hospital service area, it is not possible to determine precisely the pediatric population at risk, as hospital-based studies do not define populations in the same way that true population-based studies do. However, the strengths of our study lie in the fact that our cohort of children is largely racially homogeneous, rural, and obese.
In conclusion, the Broselow tape correlates poorly with weights seen in our setting. Use of the tape would result in underresuscitation across all weight categories, with the most significant deviation seen in the youngest patients, those falling into the gray, red, and pink intervals. Until the Broselow tape is updated to reflect the ongoing obesity epidemic, physicians are advised to remain cognizant of the potential for extreme underestimation and modify medication doses and fluid volumes accordingly. A consensus opinion is needed to guide providers of emergency pediatric care as to whether to treat ideal or actual body weight to avoid potential errors in resuscitation.
Footnotes
No financial support for funding to disclose.
REFERENCES
- 1.Kaushal R, Bates DW, Landrigan D, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16): 2114–2120. [DOI] [PubMed] [Google Scholar]
- 2.Shah AN, Frush K, Luo X, et al. Effect of an intervention standardization system on pediatric dosing and equipment size determination. Arch Pediatr Adolesc Med. 2003;157:229–236. [DOI] [PubMed] [Google Scholar]
- 3.Harris M, Patterson J, Morse J. Doctors, nurses, and parents are equally poor at estimating pediatric weights. Pediatr Emerg Care. 1999;15(1): 17–18. [DOI] [PubMed] [Google Scholar]
- 4.Lubitz DS, Seibel JS, Charmeides L, et al. A rapid method for estimating weight and resuscitation drug dosages from length in the pediatric age group. Ann Emerg Med. 1988;17(6):576–581. [DOI] [PubMed] [Google Scholar]
- 5.Krieser D, Nguyen K, Kerr D, et al. Parental weight estimation of their child’s weight is more accurate than other weight estimation methods for determining children’s weight in an emergency department? Emerg Med. 2007;24(11):756–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Broselow/Hinkle Pediatric Emergency System. Vital Signs, Inc; 1993. Patent R7331I-010494.
- 7.Centers for Disease Control Behavioral risk factor surveillance system 2008. Available at: http://apps.nccd.cdc.gov/BRFSS/list.asp?cat=OB&yr=2008&qkey=4409&state=All. Accessed December 3, 2009.
- 8.Childhood overweight and obesity prevention initiative. Available at: http://www.surgeongeneral.gov/obesityprevention/. Accessed December 3, 2009.
- 9.Nieman CT, Manacci CF, Super DM, et al. Use of the Broselow tape may result in the underresuscitation of children. Acad Emerg Med. 2006;13(10):1011–1019. [DOI] [PubMed] [Google Scholar]
- 10.Theron L, Adams A, Jansen K, et al. Emergency weight estimation in Pacific Island and Maori Children who are larger-for-age. Emerg Med Australas. 2005;17:238–243. [DOI] [PubMed] [Google Scholar]
- 11.Argall JA, Wright N, Mackway-Jones K, et al. A comparison of two commonly used methods of weight estimation. Arch Dis Child. 2003;88:789–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DuBois D, Baldwin S, King WD. Accuracy of weight estimation methods for children. Pediatr Emerg Care. 2007;23(4):227–230. [DOI] [PubMed] [Google Scholar]
- 13.Ludbrook J Multiple comparison procedures updated. Clin Exp Pharmacol Physiol. 1998;25:1032–1037. [DOI] [PubMed] [Google Scholar]
- 14.Dixon WJ, Massey FJ. Introduction to Statistical Analysis. 4th ed. New York: McGraw-Hill; 1983. [Google Scholar]
- 15.Pediatric Advanced Life Support Provider Manual. Elk Grove Village, Ill: American Academy of Pediatrics and Dallas, Tex: American Heart Association; 2006. ISBN 0-87493-527-X. [Google Scholar]
- 16.Advanced Trauma Life Support Student Course Manual. 8th ed. Chicago, Ill: American College of Surgeons; 2008. [Google Scholar]
- 17.Jang HY, Shin SD, Kwak YH. Can the Broselow tape be used to estimate weight and endotracheal tube size in Korean children? [published online ahead of print March 23, 2007] Acad Emerg Med. 2007;14(5): 489–491. [DOI] [PubMed] [Google Scholar]
- 18.Varghese A, Vasudevan VK, Lwein S, et al. Do the length-based (Broselow) tape, APLS, Argall and Nelson’s formulae accurately estimate weight of Indian children? Indian Pediatr. 2006;43:889–894. [PubMed] [Google Scholar]
- 19.Ramarajan N, Krishnamoorthi R, Strehlow M, et al. Internationalizing the Broselow tape: how reliable is weight estimation in Indian children. Acad Emerg Med. 2008;15(5):431–436. [DOI] [PubMed] [Google Scholar]
- 20.So TY, Farrington E, Absher RK. Evaluation of the accuracy of different methods used to estimate weights in the pediatric population. Pediatrics. 2009;123(6):e1045–e1051. [DOI] [PubMed] [Google Scholar]
- 21.Hofer CK, Ganter M, Tucci M, et al. How reliable is length-based determination of body weight and tracheal tube size in the pediatric age group? The Broselow tape reconsidered. Br J Anaesth. 2002;88(2): 283–285. [DOI] [PubMed] [Google Scholar]
- 22.Hashikawa A, Juhn Y, Homme J, et al. Does length-based resuscitation tape accurately place pediatric patients into appropriate color-coded zones? Pediatr Emerg Care. 2007;23(12):856–861. [DOI] [PubMed] [Google Scholar]
- 23.National Health and Nutrition Examination Survey. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/nhanes05_06.htm. Accessed December 3, 2009.
- 24.Carcillo JA, Davis AL, Zaritsky A. Role of early fluid resuscitation in pediatric septic shock. JAMA. 1991;266(9):1242–1245. [PubMed] [Google Scholar]
- 25.Han YY, Caricillo JA, Dragotta MA, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;112(4): 793–799. [DOI] [PubMed] [Google Scholar]
- 26.Oliveira CF, Nogueira de Sa FR, Oliveira DSF, et al. Time- and fluid-sensitive resuscitation for hemodynamic support of children in septic shock. Pediatr Emerg Care. 2008;24(12):810–815. [DOI] [PubMed] [Google Scholar]
- 27.Carcillo JA, Kuch BA, Han YY, et al. Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics. 2009;124(2):500–508. [DOI] [PubMed] [Google Scholar]
- 28.Yamamoto LG, Inaba AS, Young LL, et al. Improving length based weight estimates by adding a body habitus (obesity) icon. Am J Emerg Med. 2009;27(7):810–815. [DOI] [PubMed] [Google Scholar]
- 29.Kalina M, Tinkoff G, Gleason W, et al. A multidisciplinary approach to adverse drug events in pediatric trauma patients in an adult trauma center. Pediatr Emerg Care. 2009;25(7):444–446. [DOI] [PubMed] [Google Scholar]


