Abstract
Supplemental Digital Content is Available in the Text.
The coronavirus (COVID-19) pandemic continues to rapidly and dramatically transform the daily lives of patients and health care providers across the world. The number of new cases even at the time of this writing continues to grow. As individuals and as physicians, we have a responsibility to our patients and to society to “first, do no harm.” As such, neuro-ophthalmologists must balance their sacred oath to “treat the sick” against the need for social distancing to help “flatten the disease curve.” The American Academy of Ophthalmology (AAO), the American Academy of Neurology (AAN), the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and other public health organizations have actively updated recommendations and have suggested practices and protocols that may be of interest to practicing ophthalmologists. The AAO's early guidelines recommended that ophthalmologists defer any routine or nonurgent appointments in the clinic and postpone all elective surgical cases (see Supplemental Digital Content 1, Table E1, http://links.lww.com/WNO/A422). Thus, we have a responsibility to appropriately triage new and returning patients to ensure the safety of providers, patients, and the general public during and following this unprecedented pandemic. Neuro-ophthalmologists, however, often diagnose vision-threatening and potentially life-threatening disease, and delay in diagnosis or treatment can be devastating. Therefore, alternatives have been proposed to balance our competing interests of individual patient and provider safety from COVID-19 against the potential risk of undiagnosed or untreated neuro-ophthalmic disease.
Recent expansion of telehealth benefits for Medicare patients allows and encourages neuro-ophthalmologists to integrate telemedicine into practice (1). The North American Neuro-Ophthalmology Society (NANOS) has supported the use of telehealth in practice, and the reader is referred to the NANOS website for updates, resources, and webinars for the instruction of telemedicine skills for neuro-ophthalmologists.
Furthermore, there is no doubt that neuro-ophthalmologists are widely recognized as a scarce resource. According to a recent NANOS membership survey of US practicing physicians, there are 1.75 million people per 1.0 CFTE neuro-ophthalmologist, and only 187 total practicing CFTE in the nation (2). With an average wait time of 6 weeks, and with over 30% of survey respondents reporting over 3-month wait times, telemedicine is an intriguing alternative for patients from poorly represented regions of the country.
In this article, we present possible “best practices” for neuro-ophthalmologists to design and implement tele-neuro-ophthalmology during and following this national and international crisis. We review the previsit, intravisit, and postvisit steps in a practical manner that we hope will be of value to practicing neuro-ophthalmologists. We include sections on how to appropriately implement telemedicine and patient selection, focusing on different types of visits, determining eligible patients, and triaging patients. In addition, we outline the software and hardware requirements for the electronic medical record (EMR), including Epic and non-Epic platforms. We also describe the nuts and bolts of how to get started, including descriptions of the multiple useful applications and software available. As with any medical encounter, privacy regulations, billing, and coding can be significant hurdles to implementation, and we discuss each in detail. We hope that this article will be of use for neuro-ophthalmologists, comprehensive ophthalmologists, and general neurologists because we deal with effects and aftereffects of this COVID-19 pandemic. We believe that this current disruptive innovation will drive the future of telemedicine in neuro-ophthalmology.
IMPLEMENTATION AND PATIENT SELECTION
Choosing Telehealth Modalities
The terms “telehealth” and “telemedicine” are used interchangeably in this article because there is a significant interagency variation in and continual evolution of these concepts and associated technology modalities. Face-to-face telemedicine encounters between the provider and the patient are conducted through synchronous (live real-time) interaction through electronic audio and video platforms. Email or other time delayed methods (a.k.a. “asynchronous” or “store and forward”) address information electronically stored and used for patient communication, information gathering or dissemination, or provider-to-provider consultation (“E-consults”). Specific telemedicine terminology is detailed in Supplemental Digital Content 1 (see Table E2, http://links.lww.com/WNO/A422). Institutional consideration for telemedicine is described in Supplemental Digital Content 1 (see Table E3, http://links.lww.com/WNO/A422). Indications for each of the main modalities of telehealth delivery are described here (also, see Supplemental Digital Content 1, Table E4, http://links.lww.com/WNO/A422).
When to Consider a Video Visit
Video visit is optimal for those who desire a more personal connection to their provider and for external examinations. Although suboptimal compared with an in-person examination, especially for patients with suspected optic neuropathies with subjective vision changes, returning patients may still find comfort, counsel, and education from the clinician over video. In many cases, an in-person eye examination has already been performed elsewhere, and the neuro-ophthalmic virtual video visit is more of an informative review to discuss diagnostic findings, educate, and plan rather than to repeat the examination. Outside visual field testing, ocular imaging, and neuroimaging can still be presented visually to the patient in a virtual visit through screen-sharing. Video visits can also be particularly useful for visualizing an external lid, strabismus, or orbital problem (e.g., ophthalmoplegia, ptosis, or proptosis). The clinician can instruct the patient to demonstrate any neuro-ophthalmic signs over video platforms (e.g., ocular motility examination or even ice pack testing for myasthenia gravis). Synchronous video telemedicine is the best mimic of an in-person clinic visit, and it may have value in simply fostering uninterrupted time to consult one-on-one with the physician.
When to Consider Phone Visits
Phone visits may be used for the follow-up of a patient who has a known pathology with subjective outcome measures, such as ischemic cranial nerve palsy with accompanying diplopia, which is expected to recover over 6–12 weeks. If the diplopia is not recovered, the patient can then be brought into clinic or undergo further remote video visits to assess clinical progress. Phone visits also offer an opportunity for providers to adjust medications for patients with migraines or myasthenia gravis. In addition, a physician can use phone visits to triage visual symptoms with a normal dilated eye examination by another provider or discuss medication compliance and tolerance, neuroimaging findings, and laboratory test results.
When to Consider Email or Online Portal Communication
Established patients may decide to reach out through email or online (EMR) portal regarding their condition. This modality, because it is not real time, is best suited for communications that are not as time-sensitive (e.g., medication refills, test results, treatment plans, overall condition, or scheduling). Online portal communication can also aid in sharing photographs or videos (e.g., external examination findings, OCT, or visual fields) to aid in clinical evaluation. If there is a question or concern raised by the patient that may be better addressed in real time, a video or phone visit may then be undertaken.
When to Consider Provider-to-Provider Consultation (“E-consult”)
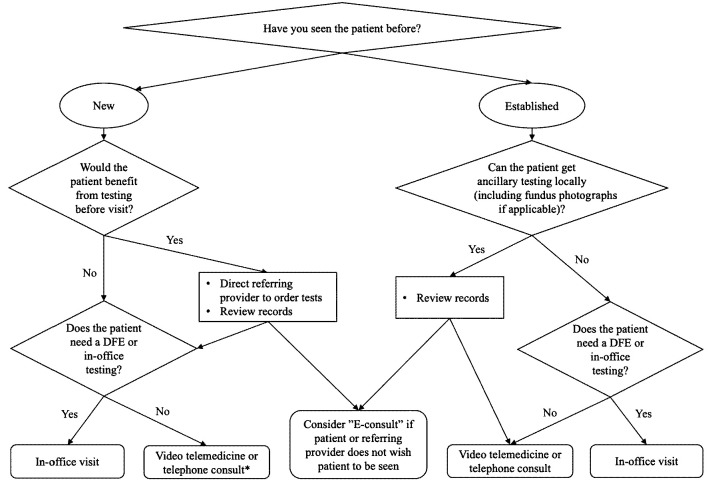
Neuro-ophthalmologists are often asked by other providers to provide consultations regarding the diagnosis or management of a patient but without the expectation of a clinic appointment (the so-called curbside consultation). This may be preferable for patients located in remote areas, who already have an engaged clinician. In an e-consult, the neuro-ophthalmologist would review clinical records and imaging, and then provide a written summary of impressions and recommendations to the referring provider. This option is ideal if the neuro-ophthalmologist determines that the patient requires related testing or medical care before an appointment or does not need their in-person examination (Fig. 1).
FIG. 1.
Choosing the appropriate type of telemedicine visit. *New telephone consults with patients are not typically a covered service. DFE, dilated fundus examination.
Selecting Appropriate Patients for Telemedicine Services
Selecting cases in neuro-ophthalmology that can be seen safely and effectively through telemedicine is a controversial discussion, but necessary given the COVID-19–related social distancing restrictions and need to maintain access to neuro-ophthalmic care. Particularly, as clinics recover from these restrictions, poor access to specialty care will be further limited, necessitating options for “work-arounds” to traditional clinic schedules. Some general guidelines for patient selection are summarized in Supplemental Digital Content 1 (see Table E5, http://links.lww.com/WNO/A422).
Triaging Neuro-Ophthalmology Patients Throughout the Crisis
In a national crisis such as the current COVID-19 pandemic, the normal triage techniques for appropriate patients may no longer apply in some cases. Before COVID-19, a telemedicine visit might follow an initial in-person visit: the patient could complete local visual field testing, fundus photographs, OCT, and/or MRI, and then review the results with the neuro-ophthalmologist over phone or video as the case history is discussed. In this setting, the neuro-ophthalmologist could use a majority of the information normally gleaned from an in-person examination. Nevertheless, this format may not be possible during a health crisis requiring social distancing in all clinical settings (i.e., no ancillary testing). Thus, what can be seen on videos and gleaned from history is perhaps all the information one may have to make a clinical workup or treatment decision.
For new referrals, the neuro-ophthalmologist may be forced to rely on the review of the patient's previous medical records and ancillary testing to determine whether the patient urgently needs to be seen in-person. Before COVID-19, the solution was generally “send them to the clinic” for the neuro-ophthalmologist to perform the initial evaluation before coordinating care; now, some coordination of care may need to precede the face-to-face evaluation. Just as general neurologists and ophthalmologists are trained to order laboratory testing in suspected giant cell arteritis before the patient may see a neuro-ophthalmologist, there are other situations in which a neuro-ophthalmologist may be able to direct referring providers in obtaining appropriate testing before an in-person evaluation. Telemedicine services such as the interprofessional consultation or live video telemedicine evaluation may allow the neuro-ophthalmologist to obtain sufficient data to make a reasonable recommendation on management, effectively reducing the risk of virus exposure by coordinating the patient's care more efficiently. The neuro-ophthalmologist may still elect to evaluate the patient in-person if necessary. The level of urgency dictates the type of visits available to the patient (e.g., in-person examination, video telemedicine visit, phone telemedicine visit, and interprofessional consultation) and the timeframe for management.
The decision as to whether to bring a patient into the clinic for evaluation should also take into account the potential for harm should the patient be exposed to and infected with COVID-19. For example, a 32-year-old healthy patient with a complaint suggesting a low likelihood of serious pathology might still be worth bringing in for evaluation to rule out such pathology, whereas an 82-year-old patient with diabetes who is at high risk of mortality from COVID-19 might be better served with an initial video visit.
Many subspecialties have provided general triage guidance for their providers (3). In neuro-ophthalmology, practice patterns vary greatly; thus, triage guidelines may vary between geographic regions, institutional capabilities, and individual patient situations. Although definitions of urgency will differ from provider to provider, telemedicine can be an effective tool for urgent triage and assessment, potentially moving a patient between categories of urgency more accurately. The specific modality choice is based on whether quick access to accurate history or seeing the external examination is paramount to determine next steps in care. Combining various modalities may improve efficacy: phone for triaging patient complaints and determining urgency, then an in-person appointment for assessment, and perhaps a follow-up visit by video once the video platform has been successfully established and the patient is clinically stable. The availability of ancillary testing will determine the ability to follow a patient remotely for optic nerve pathology, such as with idiopathic intracranial hypertension, which, in addition to history, requires a fundus view, a visual field, and arguably an OCT to determine clinical stability. In all these clinical situations, the physician may be able to use telemedicine tools to enhance their reach across practice settings, leading to potentially superior care, higher patient satisfaction, and, in the case of COVID-19, a safer environment for all.
SOFTWARE, HARDWARE, AND INTERNET REQUIREMENTS
Software
The choice of software and hardware for tele-neuro-ophthalmology is highly practice or institution dependent. If the institution already has a telemedicine platform that is integrated into the electronic health record (EMR), then the choice is clear and simple. Many institutions, however, may be overwhelmed with onboarding high volumes of providers to their integrated telemedicine platform. Recent changes in the policies and procedures of the Health and Human Services (HHS) Office for Civil Rights (OCR) have led to waiving of penalties for Health Insurance Portability and Accountability Act (HIPAA) violations against health care providers, assuming that they serve patients in good faith. This change allows telemedicine providers to communicate using everyday communication technologies and has permitted for the use of third-party platform applications during the COVID-19 nationwide public health emergency (4). There are many third-party platform applications available; however, we are highlighting one representative technology in this monograph (doxy.me) (5). Doxy.me is free, is HIPAA compliant, and includes a business associate agreement (BAA) that is easy to use for both provider and patient.
Other free platforms, however, include Zoom, Cisco Webex, Skype, and Apple FaceTime, but depending on the version that is selected, clinicians should be aware of issues regarding cost, security, and patient privacy. For example, the free version of Zoom automatically ends the call at 40 minutes if there are more than 3 participants on the call. For full service, one would need to purchase Zoom Pro or Zoom for Healthcare. Clinicians should also consider choosing a platform that is HIPAA compliant (e.g., FaceTime and Skype are not compliant) to avoid compliance issues and/or penalties after the pandemic emergency has ended when the exemptions may be reversed. The Texas Medical Association has also compiled a list of third-party vendors, which includes features and pricing information (see Supplemental Digital Content 1, Table E6, http://links.lww.com/WNO/A422) (5).
For the purpose of educating residents or fellows, there is an advantage to platforms that allow more than 2 participants, such as Zoom, so that the resident may join on the visit, with the patient's permission, as part of their resident education. Understanding the setup and needs of one's practice will dictate the best type of third-party telemedicine platform. For example, if one already has an existing EHR and does not want to invest in a telemedicine platform that requires integration with that EHR, obtaining a platform that is independent for a low monthly fee may make most financial sense (e.g., doxy.me and Zoom for Healthcare). If one seeks full integration of appointment scheduling, EHR, telemedicine visits, electronic medication orders, and patient portal communication, other platforms (e.g., AmWell, NextGen, and Zipnosis) offer more comprehensive services. Hardware requirements and some general guidelines for the setup are included in Supplemental Digital Content 2 (see Data E1, http://links.lww.com/WNO/A423). The authors are not endorsing any specific vendor, the accuracy, or timeliness of this compilation.
TELEMEDICINE USING EPIC AND NON-EPIC PLATFORMS
Connecting With the Patient: Implementation of Technology for Telehealth Neuro-Ophthalmology Visits
The mechanism used for establishing a video connection with the patient to perform a virtual visit will depend on whether your institution or practice uses Epic and whether telehealth platforms have been formalized and embedded into the Epic system.
Before initiation of a telemedicine visit, patient consent is required and must be documented. As a result, you should obtain and document patient consent in the chart before every telemedicine visit. Below is sample language that you can use:
“This is a telemedicine visit that was performed with the originating site at [INSERT PATIENT LOCATION] and the distant site at [INSERT PROVIDER LOCATION]. Verbal consent to participate in video visit was obtained. This visit occurred during the Coronavirus (COVID-19) Public Health Emergency. I discussed with the patient the nature of our telemedicine visits and its inherent limitations, that: I would evaluate the patient and recommend diagnostics and treatments based on my assessment. Our sessions are not being recorded and that personal health information is protected. Our team would provide follow-up care in person if/when the patient needs it.”
Virtual Visits Through Epic in a Formalized and Embedded System
Differences in Epic functionality and appearance may vary across medical centers and practices; thus, what follows serves as an example of how the system appears and functions at a single institution. A prerequisite for provision of virtual visits in Epic is setting up Epic on either an iPhone or iPad. Although Epic can be set up on Android phones, in this institution's example, Android phones cannot currently be used for virtual visits. The Epic application for iPhone use is called Haiku (see Supplemental Digital Content 3, Figure E1, http://links.lww.com/WNO/A411) and for iPad use is called Canto. The process of obtaining Haiku on the iPhone or Canto on the iPad, in this example, involves first downloading an application in the App Store called “Intelligent Hub” that allows installation of a program called “AirWatch.” This allows for remote management of work-related applications and is often the mechanism by which work email is obtained on a smartphone. Therefore, it may already exist on your phone if you receive your work email on your phone. Once installed, the Haiku or Canto application must be set up in Settings to allow for notifications. For those at academic medical centers, the information technology department is typically available to assist.
Once Haiku or Canto exists on your iPhone or iPad, respectively, virtual visits may occur using that device. When administrative staff schedule a patient for a virtual visit, these virtual visits are noted on the clinic schedule as a “Video Visit” type, and a video camera symbol can be seen on the schedule on Haiku, Canto, or the typical PC Epic schedule (see Supplemental Digital Contents 4 and 5, Figure E2A and E2B, http://links.lww.com/WNO/A412, and http://links.lww.com/WNO/A413). This visit type can occur within an existing face-to-face clinic schedule or on a day consisting of virtual visits alone. An example of such an embedded schedule is the following: a new face-to-face patient at 9 am, an established patient virtual video visit at 10 am, an established face-to-face patient at 10:30 am, etc. The video visit duration will be set on your schedule for the duration that you set for new and established visits, but as in a face-to-face visit, the duration of the visit just holds the spot on the schedule. Once the video visit is started, the video call does not automatically disconnect at any point. You will terminate the call only when the visit is completed.
The prerequisite for the patient to have a virtual visit through Epic is for them to have an active online portal account. At the time of scheduling, the patient is instructed to sign on for the visit 15 minutes before the visit time, so that they are ready and waiting in the virtual “waiting room” when the appointment time arrives. When the patient is connected, the video icon on the Epic schedule turns green on both desktop Epic and Haiku/Canto (see Supplemental Digital Content 6, Figure E2C, http://links.lww.com/WNO/A414), and a push notification appears on the iPhone or iPad that the physician will use for the video visit (see Supplemental Digital Content 7, Figure E3A, http://links.lww.com/WNO/A425). Reminder push notifications are sent at specific intervals until the physician connects with the patient. When ready to connect with the patient for the visit, the physician may either connect to the patient directly from Haiku/Canto or log onto desktop Epic as usual on either a desktop PC or laptop and click on the patient's visit on the schedule to open the chart. If logging onto desktop PC first, a “Handoff to Haiku/Canto” button will be present in the upper left corner (see Supplemental Digital Content 8, Figure E3B, http://links.lww.com/WNO/A415). Pushing this button will activate the iPhone/iPad, allow for Haiku/Canto log on, and connection to the patient through the “Join Video Call” button in iPhone/iPad (see Supplemental Digital Content 9, Figure E3C, http://links.lww.com/WNO/A416). The video visit proceeds on the iPhone/iPad, and documentation is completed on desktop Epic.
Virtual Visits Through a Third-Party App
Supplemental Digital Content 10 (Data E2, http://links.lww.com/WNO/A424) includes specific tips on using these applications. Depending on the third-party platform, a consent form may not be available or integrated into the workflow.
Doxy.me
Go to https://doxy.me/sign-up on your phone, tablet, or computer. Complete all fields and click sign up (see Supplemental Digital Content 11, Figure E4, http://links.lww.com/WNO/A417). Under account settings, you may select the tab “BAA” to generate a BAA if applicable. You can also select the checkbox “I don't need a BAA.” The telemedicine visit with your patient through doxy.me will work irrespective of your choice regarding a BAA.
You will then be logged into your dashboard, and you will be provided a room name link, doxy.me/(the room name you have selected), which will need to be provided to your patients so that they can connect with you at the time of their scheduled appointment (see Supplemental Digital Content 12, Figure E5, http://links.lww.com/WNO/A418). The patient does not need to download any software or create an account within doxy.me. Their sessions are anonymous, and none of their information is stored. They only need to enter your room link into their web browser, type their name, and select “check in” (see Supplemental Digital Content 13, Figure E6, http://links.lww.com/WNO/A419).
Before the appointment time, you can run a Pre-call Test (see Supplemental Digital Content 14, Figure E7, http://links.lww.com/WNO/A420) whereby doxy.me will run diagnostics on your device, including video and audio quality and stability. When the patient arrives into the virtual waiting room, you will see their image in the upper left corner under the “patient queue.” From your mobile device or tablet, you will see a red circle in the upper left corner when a patient is waiting to see you. You can click on the red dot area and, when ready, click the patient's name to start the video. If you are on a computer, click “start call.” Then, select “video call” to begin the visit. Always allow the use of your camera and microphone. When the video begins, the patient will be on the large screen and the provider will be on the smaller screen. If you hit “pause the video,” you will send the patient back into the “waiting room.” Once your visit is complete, you can hang up the call with the red telephone icon.
Applications for Home Testing
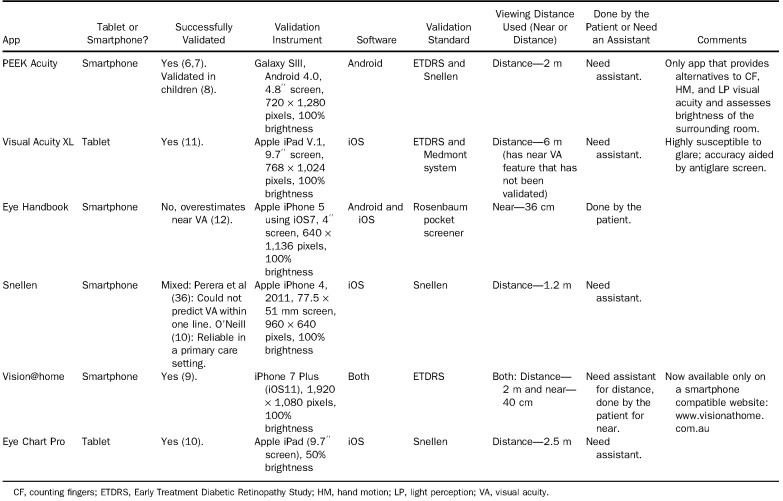
A challenge that many providers identify with telemedicine and remote evaluations is the physical examination and other objective data collection. Although remote physical and ocular examinations are not as useful as those in-person, there are a number of technological outlets to simplify and optimize home testing through telemedicine. Multiple smartphone and tablet applications have been validated for remote visual acuity testing. Patients with Android Galaxy phones and someone to help, as the phone is held 2 m away, can use “PEEK Acuity,” a free app validated for distance testing (6,7) and use in children (8). Patients who have Apple iPhone 7 Plus or who do not have an assistant available can use “Vision@home,” an online test validated for both near (40 cm) and distance (2 m, assistant needed) visual acuities that is accessible free on their phone browser at www.visionathome.com.au (9). For Apple iPad tablet users, “Eye Chart Pro” is a free app validated for distance vision (2.5 m, assistant needed) (10) on the iPad and available but not validated on the iPhone. “Visual Acuity XL” has also been validated for distance vision (held at 6 m) using the iPad (11), although its accuracy is highly susceptible to glare and it costs $75. Notably, the commonly used app “Eye Handbook,” available for Apple iPad and Android users, has a near card test that may overestimate near VA (12). Refer to Table 1 for a review of the findings of each visual acuity application validation study.
TABLE 1.
Visual acuity testing with smartphone and tablet review
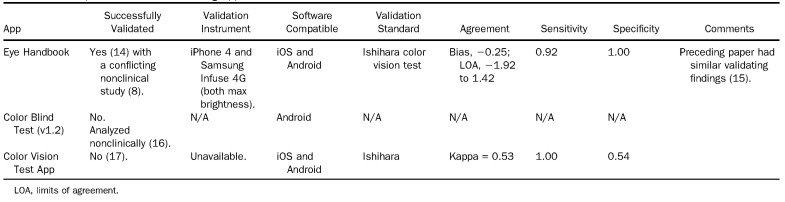
Smartphone applications exist for color vision testing, although options are more limited and are hampered by variation in tablet display manufacturing parameters (13). The most promising is contained within the “Eye Handbook” app, which is available free for both Apple iPhone and Android users. The app was validated against the Ishihara color vision test in 2 clinical studies (14,15), although a nonclinical study using image analysis found it likely underestimates color vision loss severity in patients with normal contrast sensitivity (CS) and does not contain as many specially designed plates as Ishihara for differentiation of R-G deficiency from total color blindness (8). Other less promising apps include “Color Blind Test” (16) and “Color Vision Test” (17). Refer to Table 2 for color validation studies. At the moment, these apps can only approximate a color perception test and detailed color testing needs to be performed in-person.
TABLE 2.
Smartphone color vision testing application review
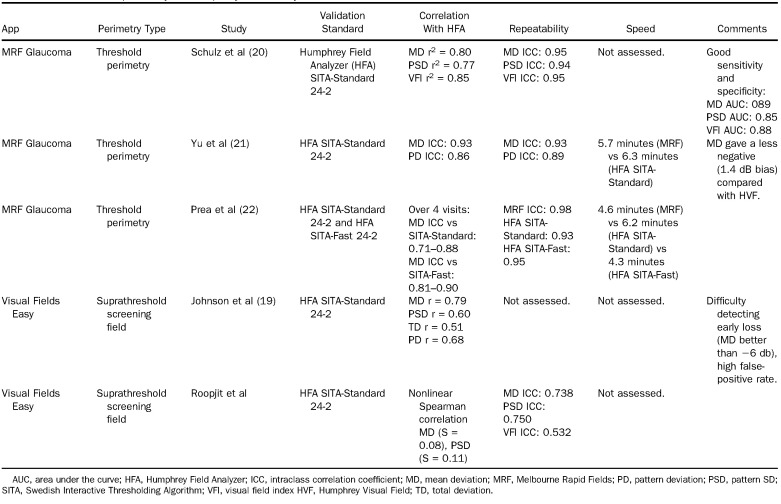
Regarding perimetry, 2 apps “MRF Glaucoma Lite” and “MRF Neuro Lite” provide reliable Apple iPad–based threshold perimetry, and “eyesimplify.com” uses the same technology in a computer browser form. MRF Glaucoma Lite tests the central 30° horizontally and 20° vertically by implementing a radial testing grid and changing the location of the fixation point held approximately 33 cm away (18). Stimuli have an operating range of 0 dB–30 dB and increase in size with eccentricity from Goldmann size III to IV with a background luminance of 5 cd/m2 (15.71 asb). Unexpectedly, altering ambient lighting and viewing distance (between 25 cm and 75 cm) did not affect the threshold in a small group of testing subjects (18). All MRF measurements were highly correlated with those of the 24-2 Humphrey Field Analyzer (HFA) across multiple investigations (19–22), showing reliability and reproducibility over multiple visits (20–22), strong sensitivity and specificity (20), and faster testing speed than the HFA SITA-Standard (comparable with the HFA SITA-Fast) (21,22). Notably, the proportion of fixation losses is found to be higher and more variable than the HFA (22,23). The most recent MRF technology has been licensed to “eyesimplify.com” and released for beta testing in a home computer browser version found at the aforementioned website. This version allows testing of either the 24-2 or the 10-2 visual field and may shortly be accessible on iPad or Android. “Visual Fields Easy,” the predecessor to the MRF programs, is another free iPad application; it does suprathreshold screening visual fields of the central 60° horizontally and 48° vertically at a background luminance of 10 cd/m2 (31.5 asb) of the iPad with size V Goldmann equivalent stimulus at 16 dB intensity. Johnson et al found that “Visual Fields Easy” detected most visual defects with moderate to advanced loss as seen on SITA-standard testing but had difficulty identifying loss of less than 6 dB (19,24). Unfortunately, to our knowledge, no validated perimetry testing applications exist for patients with Android, although patients without Apple iPads have access to “eyesimplify.com” on a home computer browser. Tablet-based perimetry has the potential to cut detection of rapid visual loss in glaucoma from 2.5 years to 0.9 years with more frequent testing (25), bring access to necessary visual field testing to bed-bound hospital patients (26), and transform remote and home testing (23). Refer to Table 3 for findings of the studies validating tablet-based perimetry against the HFA.
TABLE 3.
Tablet-based perimetry vs Humphrey Field Analyzer review
CS offers an additional means of assessment of optic nerve and macular function and has been shown to correlate with optic nerve thickness following optic neuritis. CS may be tested remotely, using VCStest.com, which uses gray and white grids of varying degrees of contrast and size and provides a comprehensive report or with the CS letter chart available on the Eye Handbook app. The reliability of CS is particularly sensitive to screen brightness, so online assessments should be interpreted as screening tests rather than definitive measurements of contrast function.
PRIVACY, REGULATION, BILLING, AND CODING
Institutional Support
National and institutional regulations should be considered to avoid privacy and legal infringements. Many larger institutions have dedicated telemedicine implementation staff who can support the roll-out of telemedicine services. For those in smaller groups or in private practice, there may be less bureaucracy, but national and state regulations still exist. It may be necessary to consult a health care policy lawyer before embarking on a new patient communication platform. During the COVID-19 pandemic, many of the previous barriers in implementing telemedicine have been suspended, but they will likely resume after the resolution of this crisis.
Privacy and Security
Conceptually, technological privacy and security refer to how the user (doctor–patient), the company providing the platform (e.g., Zoom and Google), and everyone else on the internet (external parties) relate to each other (see Supplemental Digital Content 15, Figure E8, http://links.lww.com/WNO/A421). Security is the term used to describe a company's ability to protect the consumer from external parties' access of unauthorized data. Privacy refers to the company's user-allowed rights to access, store, and share user data (27). One might think of security as “putting locks on the door” and privacy as “putting curtains on the windows.”
In the context of health care, security sets the standards for ensuring that only those who should have access to personal health information will actually have access. Privacy has additional stipulations. The 1996 Health Insurance Portability and Accountability Act (HIPAA) requires “appropriate safeguards to protect the privacy of personal health information, and sets limits and conditions on the uses and disclosures that may be made of such information without patient authorization” (28). Translating this to telemedicine, the HIPAA requires the visit be as secure and confidential as an in-person appointment and is achieved through the following elements:
The patient must consent to use of telemedicine technology to conduct a health care visit (and its associated billing).
The interaction should be made on a secure provider-to-patient platform with encrypted data exchange.
Video or audio should not be recorded or discoverable (one could imagine that recordings or screenshots with express patient written consent for treatment purposes could be allowable).
Each institution may have their own platforms with associated training modules and signed contracts required for use; for example, the VA Health Care System uses the secure “VA Video Connect,” or VVC platform, with dedicated talent management system prerequisite training and telework agreements (29). According to recent advice from the Office of Civil Rights (OCR) at the Department of Health and Human Services (HHS), covered health care providers subject to the HIPAA regulations can use any non–public-facing remote communication product that is available to communicate with patients during the COVID-19 nationwide public health emergency. In other words, the OCR is currently exercising its discretion not to audit telemedicine encounters for HIPAA violations, allowing providers to avoid penalties for noncompliance with the HIPAA rules, when the “good faith” provision of telehealth is used (30).
Despite the relaxation of HIPAA enforcement, clinicians should be careful to select communication platforms with “lockable rooms” to protect patient–doctor privacy in this unique clinical care format. Definitions of security and privacy vary between technology companies; carefully reading the service agreements is critical for ensuring that the platform is appropriate for telemedicine use. Companies that offer “HIPAA-compliant” services require a BAA, which is a legal contract between the company offering the platform and the company using the service (such as a hospital, clinic, or physician practice) in which both parties agree to maintain HIPAA-compliant storage and transmission of patient data. Because some companies offer both “secure” services that are not HIPAA-compliant and separate HIPAA-compliant services, it is important to select the appropriate option to avoid encounters that do not maintain patient privacy.
Medical Malpractice Liability
It is important to ensure that telemedicine services are covered by malpractice insurance. Although many carriers may have implicit or explicit clauses, there may be limitations on the amount of telemedicine that can be performed or whether the telemedicine services can be performed over state lines. Other malpractice insurance companies may require a separate policy for telemedicine services.
Medical Licensure
In the United States, medical licenses are typically limited to specific states; separate licenses are required to practice in multiple states, with some exceptions allowed within certain institutions. Some states required providers performing telemedicine services to hold separate medical licenses. COVID-19 emergency provisions temporarily suspended these limitations, allowing physicians or other health care professionals to provide medical care in any state as long as they hold a valid equivalent license with a state (31). These provisions also deemed credentialing requirements at hospitals or other health care facilities nonenforceable during the crisis.
Billing and Coding
One of the previous barriers to the utilization of telemedicine in neuro-ophthalmology has been reimbursement for services. Before the COVID-19 pandemic, insurers (e.g., Medicare, Medicaid, or private insurance in the United States) placed severe restrictions on telemedicine use, with many forms of telemedicine not being reimbursable at all (32). Because of the increased need for telemedicine since the outbreak of COVID-19 to limit in-person patient encounters to urgent/emergent problems, the CMS expanded its reimbursement of the existing telemedicine codes,1 encouraged private insurers to do the same, added reimbursement of telephone evaluation/management codes (99441–99443), and, in some cases, announced nonenforcement of certain rules, such as the established patient requirement for G2010, G2012, and 99421–99423 codes (4) and HIPAA requirements for live video telemedicine evaluations (33). Examination requirements for billing of real-time video telemedicine (99201–99215) was also changed to allow billing based on time alone or medical decision making alone, and eye examination codes (92002 and 92012) were later made available for video telemedicine encounters (34). Although many of these policy changes are limited to the duration of the current emergency declaration, the expansion of reimbursement of these services has accelerated the adoption and implementation of telemedicine services across all specialties. The CMS has updated and clarified their coding guidelines at least once per week since March 7, 2020; as such, the guidelines provided in this document are rapidly evolving.
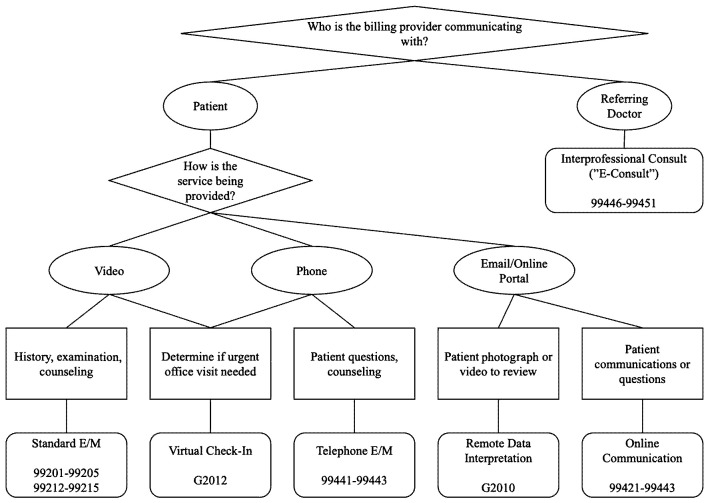
The AAO and AAN have released coding guidelines for the billing of telemedicine-related codes during the COVID-19 emergency (34,35). There are essentially 6 specific categories of telemedicine services as follows:
Live, real-time video consults with patients;
“Virtual check-in” evaluations with established patients for new problems;
Evaluation of patient-sent photographs or videos (remote data interpretation);
Interprofessional consultation (“E-consult”);
Online patient communications (e.g., online portals and secure email);
Telephone evaluation and management.
Choosing the correct code depends on the type of communication (Fig. 2), whether it satisfies the CMS requirements (see Supplemental Digital Content 16, Table E7, http://links.lww.com/WNO/A422), and time spent (see Supplemental Digital Content 17, Tables E8–E10, http://links.lww.com/WNO/A422). Additional resources for neuro-ophthalmologists can be found at https://www.nanosweb.org/telemedicine.
FIG. 2.
Coding for telemedicine services.
CONCLUSION
The unprecedented COVID-19 pandemic has created challenge, hardship, and disruption to the lives and practice of medicine including neuro-ophthalmology. The full effects of the crisis remain to be seen, and there will be long-term implications and downstream consequences for neuro-ophthalmology. Disruption, however, sometimes brings innovation and speeds adoption, and we believe that the development, refinement, and implementation of tele-neuro-ophthalmology have been forced to accelerate in response to the unexpected spike in demand created by social distancing requirements. The new development and implementation of telemedicine is instrumental at a time like this to provide adequate care to all patients while also trying to “flatten the curve.” While selecting patients and implementing telehealth into our daily practice, we must consider all institutional rules and regulations to avoid privacy and legal infringements, as well as consider different modalities and formats of providing care. It is important to consider the AAO guidelines to determine how to appropriately triage patients. There are a number of technological requirements including software, hardware, and Internet for the process to be optimized. One of the many challenges of telemedicine is the objective examination of the patient virtually—although limited, there are multiple good options, including visual fields and color vision testing, for objectifying important measures to help assess a patient remotely. In addition, we outline how to appropriately bill and code for these virtual visits, as the mechanics differ invariably from in-person appointments.
The COVID-19 pandemic has been a transformative disruption both to society and to the practice of medicine. Although telemedicine existed before the COVID-19 pandemic, the rate of adoption, innovation, and implementation as a solution to social distancing has been dramatic, and the use of telemedicine in our neuro-ophthalmic practices likely will continue long after the pandemic ends.
Footnotes
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jneuro-ophthalmology.com).
The information provided in this manuscript, to the best of our knowledge, was the most up-to-date available content, recommendations, and guidelines at the time of writing. The authors wish to emphasize that our manuscript represents recommendations and not prescriptions for tele-neuro-ophthalmology, and the information contained herein should not be construed as a “standard of care.” The views and opinions contained in our work represent the individual authors' opinions and do not necessarily represent the views of individual academic institutions, other medical or public health organizations, or the United States government.
REFERENCES
- 1.President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak. Centers for Medicare and Medicaid Services. 2020. Available at: https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak. Accessed March 30, 2020. [Google Scholar]
- 2.Subramanian P, Moster M, DeBusk A. North American Neuro-Ophthalmology Society Advocacy Committee—2019 CFTE Survey. Presented at the: NANOS Annual Meeting 2020; March 7, 2020; Amelia Island, FL. Available at: https://www.nanosweb.org/i4a/pages/index.cfm?pageID=3839&activateFull=true. Accessed April 4, 2020. [Google Scholar]
- 3.Skalet A, Allen R, Shields C, Wilson MW, Mruthyunjaya P, Gombos DS. Considerations for the Management and Triage of Ocular Oncology Cases during the COVID-19 Pandemic. American Association of Ophthalmic Oncologists and Pathologists; Available at: http://www.aaoop.org/wp-content/uploads/2020/03/AAOOP-COVID19-Oncology-Considerations-UPDATED.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medicare Telehealth Frequently Asked Questions (FAQs). Centers for Medicare and Medicaid Services. 2020. Available at: https://www.cms.gov/files/document/medicare-telehealth-frequently-asked-questions-faqs-31720.pdf. [Google Scholar]
- 5.Telemedicine Vendor Options. Texas Medical Association—Health Information Technology. Available at: https://www.texmed.org/uploadedFiles/Current/2016_Practice_Help/Health_Information_Technology/Telemedicine/Telemedicine%20Vendor%20Options.pdf. [Google Scholar]
- 6.Bastawrous A, Rono HK, Livingstone IAT, Weiss HA, Jordan S, Kuper H, Burton MJ. Development and validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmol. 2015;133:930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brady CJ, Eghrari AO, Labrique AB. Smartphone-based visual acuity measurement for screening and clinical assessment. JAMA. 2015;314:2682–2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao L, Stinnett SS, Prakalapakorn SG. Visual acuity assessment and vision screening using a novel smartphone application. J Pediatr. 2019;213:203–210.e1. [DOI] [PubMed] [Google Scholar]
- 9.Han X, Scheetz J, Keel S, Liao C, Liu C, Jiang Y, Müller A, Meng W, He W. Development and validation of a smartphone-based visual acuity test (vision at home). Transl Vis Sci Technol. 2019;8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Neill S, McAndrew DJ. The validity of visual acuity assessment using mobile technology devices in the primary care setting. Aust Fam Physician. 2016;45:212–215. [PubMed] [Google Scholar]
- 11.Black JM, Jacobs RJ, Phillips G, Chen L, Tan E, Tran A, Thompson B. An assessment of the iPad as a testing platform for distance visual acuity in adults. BMJ Open. 2013;3:e002730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tofigh S, Shortridge E, Elkeeb A, Godley BF. Effectiveness of a smartphone application for testing near visual acuity. Eye. 2015;29:1464–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dolores de Fez MJL, García-Domene MC, Caballero MT, Camps VJ. Can applications designed to evaluate visual function Be used in different iPads? Optom Vis Sci. 2018;99:1054–1063. [DOI] [PubMed] [Google Scholar]
- 14.Ozgur OK, Emborgo TS, Vieyra MB, Huselid RF, Banik R. Validity and acceptance of color vision testing on smartphones. J Neuroophthalmol. 2018;38:13–16. [DOI] [PubMed] [Google Scholar]
- 15.Shah AA, Pasadhika S, Kim J, Wang M. Pseudoisochromatic color vision testing on an iPhone. Invest Ophthalmol Vis Sci. 2012;53:6399. [Google Scholar]
- 16.Dain SJ, Almerdef A. Colorimetric evaluation of iPhone apps for colour vision tests based on the Ishihara test. Clin Exp Optom. 2016;99:264–273. [DOI] [PubMed] [Google Scholar]
- 17.Sorkin N, Rosenblatt A, Cohen E, Ohana O, Stolovitch C, Dotan G. Comparison of Ishihara booklet with color vision smartphone applications. Optom Vis Sci. 2016;93:667–672. [DOI] [PubMed] [Google Scholar]
- 18.Vingrys AJ, Healey JK, Liew S. Validation of a tablet as a tangent perimeter. Transl Vis Sci Technol. 2016;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson CA, Thapa S, George Kong YX, Robin AL. Performance of an iPad application to detect moderate and advanced visual field loss in Nepal. Am J Ophthalmol. 2017;182:147–154. [DOI] [PubMed] [Google Scholar]
- 20.Schulz AM, Graham EC, You YY, Klistorner A, Graham SL. Performance of iPad-based threshold perimetry in glaucoma and controls. Clin Exp Ophthalmol. 2018;46:346–355. [DOI] [PubMed] [Google Scholar]
- 21.Kong YXG, He M, Crowston JG, Vingrys AJ. A comparison of perimetric results from a tablet perimeter and Humphrey field analyzer in glaucoma patients. Transl Vis Sci Technol. 2016;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prea SM, Kong YXG, Mehta A, He M, Crowston JG, Gupta V, Martin KR, Vingrys AJ. Six-month longitudinal comparison of a portable tablet perimeter with the Humphrey field analyzer. Am J Ophthalmol. 2018;190:9–16. [DOI] [PubMed] [Google Scholar]
- 23.Kong YXG. Visual field testing in the era of portable consumer technology. Clin Exp Ophthalmol. 2018;46:325–326. [DOI] [PubMed] [Google Scholar]
- 24.Sahi RK, Ichhpujani P, Thakur S, Kumar S. Has the tablet perimetry arrived? Visual fields Easy app versus Humphrey field analyser in glaucoma patients. J Clin Exp Ophthalmol. 2017;8:4(Suppl). doi: 10.4172/2155-9570-C1-067. [DOI] [Google Scholar]
- 25.Anderson AJ, Bedggood PA, George Kong YX, Martin KR, Vingrys AJ. Can home monitoring allow earlier detection of rapid visual field progression in glaucoma? Ophthalmology. 2017;124:1735–1742. [DOI] [PubMed] [Google Scholar]
- 26.Nesaratnam N, Thomas PBM, Kirollos R, Vingrys AJ, Kong GYX, Martin KR. Tablets at the bedside—iPad-based visual field test used in the diagnosis of Intrasellar Haemangiopericytoma: a case report. BMC Ophthalmol. 2017;17:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heckman MR. The Difference Between Data Security and Privacy. United States Cybersecurity Magazine. 2017. Available at: https://www.uscybersecurity.net/csmag/data-security-privacy/. Accessed April 7, 2020. [Google Scholar]
- 28.The HIPAA Privacy Rule. U.S. Department of Health & Human Services. Available at: https://www.hhs.gov/hipaa/for-professionals/privacy/index.html. Accessed April 4, 2020. [Google Scholar]
- 29.Veterans Affairs Mobile Website. U.S. Department of Veterans Affairs. Available at: https://www.mobile.va.gov/. Accessed April 4, 2020. [Google Scholar]
- 30.Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. U.S. Department of Health & Human Services; 2020. Available at: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Accessed April 4, 2020. [Google Scholar]
- 31.Alex M, Azar II. Waiver or Modification of Requirements Under Section 1135 of the Social Security Act. U.S. Department of Health & Human Services; 2020. Available at: https://www.phe.gov/emergency/news/healthactions/section1135/Pages/covid19-13March20.aspx. Accessed April 4, 2020. [Google Scholar]
- 32.David ER. National Consortium of Telehealth Resource Centers (NCTRC) Webinar: Telemedicine: How to Do it Right! YouTube. 2019. Available at: https://www.youtube.com/watch?v=IpF9gW9OZQQ. Accessed March 30, 2020. [Google Scholar]
- 33.Medicare Telemedicine Health Care Provider Fact Sheet. Centers for Medicare and Medicaid Services. 2017. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed March 30, 2020. [Google Scholar]
- 34.Coding for Phone Calls, Internet and Telehealth Consultations. American Academy of Ophthalmology. 2020. Available at: https://www.aao.org/practice-management/news-detail/coding-phone-calls-internet-telehealth-consult. Accessed March 30, 2020. [Google Scholar]
- 35.Telemedicine and COVID-19 Implementation Guide. American Academy of Neurology. 2020. Available at: https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist--administrators/telemedicine-and-remote-care/20-telemedicine-and-covid19-v103.pdf. Accessed March 30, 2020. [Google Scholar]
- 36.Perera C, Chakrabarti R, Islam FMA, Crowston J. The Eye Phone Study: reliability and accuracy of assessing Snellen visual acuity using smartphone technology. Eye (Lond). 2015;29:888–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.James C, Holland GN, Yeh S. Important Coronavirus Updates for Ophthalmologists. American Academy of Ophthalmology. 2020. Available at: https://www.aao.org/headline/alert-important-coronavirus-context. Accessed March 30, 2020. [Google Scholar]
- 38.Ko MW. Telemedicine 20/20 in 2020: How Far Have We Come, where Are We Headed and How Is it Relevant to Neuro-Ophthalmology? (Slide Presentation). North American Neuro-Ophthalmology Society 2020 Annual Meeting. Neuro-Ophthamology Virtual Library. University of Utah. Available at: https://collections.lib.utah.edu/details?id=1534065. Accessed April 1, 2020. [Google Scholar]
- 39.Lai KE. Telemedicine: Does it Pay to Play? Billing, Coding, Reimbursement (Slides). North American Neuro-Ophthalmology Society 2020 Annual Meeting. Neuro-Ophthamology Virtual Library. University of Utah. Available at: https://collections.lib.utah.edu/details?id=1534201. Accessed April 1, 2020. [Google Scholar]
- 40.Speedtest. Speedtest—the Global Broadband Speed Test. Available at: https://www.speedtest.net/. Accessed March 30, 2020. [Google Scholar]