Abstract
Background:
The alpha angle is the most often used measure to classify cam morphology. There is currently no agreement on which alpha angle threshold value to use.
Purpose:
To systematically investigate the different alpha angle threshold values used for defining cam morphology in studies aiming to identify this threshold and to determine whether data are consistent enough to suggest an alpha angle threshold to classify cam morphology.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
The Embase, Medline (Ovid), Web of Science, Cochrane Central, and Google Scholar databases were searched from database inception to February 28, 2019. Studies aiming at identifying an alpha angle threshold to classify cam morphology were eligible for inclusion.
Results:
We included 4 case-control studies, 10 cohort studies, and 1 finite-element study from 2437 identified publications. Studies (n = 3) using receiver operating characteristic (ROC) curve analysis to distinguish asymptomatic people from patients with femoroacetabular impingement syndrome consistently observed alpha angle thresholds between 57° and 60°. A 60° threshold was also found to best discriminate between hips with and without cam morphology in a large cohort study based on a bimodal distribution of the alpha angle. Studies (n = 8) using the upper limit of the 95% reference interval as threshold proposed a wide overall threshold range between 58° and 93°. When stratified by sex, thresholds between 63° and 93° in male patients and between 58° and 94° in female patients were reported.
Conclusion:
Based on the available evidence, mostly based on studies using ROC curve analysis, an alpha angle threshold of ≥60° is currently the most appropriate to classify cam morphology. Further research is required to fully validate this threshold.
Keywords: femoroacetabular impingement syndrome, cam morphology, hip, alpha angle, diagnosis
Femoroacetabular impingement syndrome (FAIS) is a motion-related disorder of the hip caused by a premature contact between the proximal femur and acetabulum.17,43 FAIS can be diagnosed by the presence of hip pain, a clinical sign suggestive of FAIS during hip examination, and imaging findings. Imaging findings include the presence of cam morphology, which is an asphericity of the femoral head. This extra bone formation is often located in the anterolateral head-neck junction and in most cases develops during skeletal growth.2,4,39,50
The presence of cam morphology is a common imaging finding. The prevalence in the general population is roughly 15%-25% in male patients and 5%-15% in female patients.16,18,41 The significance of cam morphology in isolation, without the presence of symptoms and clinical signs, is unknown. Although its presence is associated with limited range of motion6,22,34 and the future development of osteoarthritis (OA),3,35,37,42,47,49 the association with hip pain is conflicting.24,48
Cam morphology can be quantified by various means. Measures that have been described include the head-neck ratio,29 triangular index,15 beta angle,8 and the alpha angle.38 To date, the alpha angle is the measure most often used to quantify cam morphology, and it has been used in various imaging modalities and views. The alpha angle, always measured in a 2-dimensional (2D) plane, quantifies the sphericity of the femoral head-neck junction on a location depending on the radiographic view. For example, on an anteroposterior (AP) view, the alpha angle quantifies the lateral head-neck junction, whereas on a frog-leg lateral or Dunn view, the alpha angle quantifies the anterolateral head-neck junction. The advantage of 3-dimensional (3D) imaging is that the alpha angle can be measured at multiple locations around the head-neck junction. Some analyze the alpha angle as a continuous variable,37 whereas others35 use threshold values to binary classify the presence and absence of cam morphology. As the alpha angle per definition is a 2D measurement, it might be applied to all imaging modalities such as radiographs and 3D planes. However, the reported alpha angle threshold values to identify or diagnose cam morphology have been inconsistent. Threshold values used range from 50° to 83°.13,15,38,40
Because of the inconsistencies in alpha angle threshold values prevalence data and associations between cam morphology and hip pain or pathology are difficult to interpret. Nötzli et al38 first described the alpha angle and suggested a 55° threshold, although a 50° threshold has frequently been used by others.18,21,23,24,27 By an advanced understanding of cam morphology prevalence and its association with pathology, some authors2–4,35,42,50 have suggested a higher alpha angle threshold to classify cam morphology. A recent scoping review30 suggested that a threshold around 60° would be more appropriate to classify cam morphology. In a recent consensus statement on FAIS and on the classification of hip-related pain, the authors acknowledged importance of the use of a consistent alpha angle threshold.17 Particularly for research purposes, future studies are warranted to study a homogenous population and to classify the presence of cam morphology consistently. However, no exact alpha angle threshold value could be advised because of the lack of a systematic synthesis of this data.17
Therefore, the aims of this systematic review were to (1) appraise studies investigating alpha angle threshold values for cam morphology and (2) determine whether data are consistent enough to suggest an alpha angle threshold to classify cam morphology.
Methods
Protocol and Registration
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed during the search and reporting phase.46 This review was registered in PROSPERO after a pilot search and before the updated search and extraction of the data. Protocol details can be accessed via the online PROSPERO database (registration No. CRD42019126021).
Identification and Selection of the Literature
The study protocol, with a PICO (patient-intervention-comparison-outcome) framework and eligibility criteria for the reports, was composed before the search was performed. We included (1) studies aiming at identifying an alpha angle threshold value based on imaging (eg, radiographs, magnetic resonance imaging [MRI], computed tomography [CT], or ultrasound) to distinguish between hips with and without cam morphology. We considered (2) all types of methodology to identify a threshold value, including, for example, reference intervals and confidence intervals based on the alpha angle distribution, receiver operating characteristic (ROC) curve analyses or associations between alpha angle thresholds, and certain outcomes. For studies using ROC curve analyses or association studies, we included the ones that explained threshold values in relation to symptoms, range of motion, intra-articular hip pathology (labral tears/chondropathy), hip OA, and/or total hip replacement (THR). (3) Studies that primarily investigated the association between cam morphology and symptoms, intra-articular hip pathology, hip OA, and/or THR and used predefined threshold values to quantify cam morphology were only included when they studied ≥3 alpha angle threshold values. The exclusion criteria were (1) studies including a group of patients with hip diseases such as dysplasia, Perthes, and slipped capital femoral epiphysis; (2) animal studies; (3) studies using 1 or 2 predefined alpha angle thresholds for cam morphology to study the association with hip symptoms, intra-articular hip pathology, hip OA, and/or THR; and (4) systematic reviews, meta-analyses, case series with fewer than 10 participants, and congress abstracts. No restrictions for publication language or publication period were used.
Literature Search Strategy and Information Sources
A sensitive literature search strategy was conducted for several online databases, with the assistance of a medical librarian. The following databases were searched from inception until February 28, 2019 (date last searched): Embase.com, Medline (Ovid), Web of Science Core Collections, Cochrane Library Central Registry of Trials (Wiley), and Google Scholar. The searches combined terms for hip with alpha angle. The complete search strategy for each database can be found in the Appendix.
Selection of Studies
The titles, abstracts, and full texts of all studies found using our search strategy were scored independently by 2 different raters (P.K., R.A.) to determine whether they met the inclusion criteria, resulting in an equal judgment between the raters. Disagreements were resolved by a consensus meeting. A third reviewer (M.R.) was involved for determination of full-text inclusion regarding 1 article because of failure to achieve consensus between the 2 main reviewers. Reference screening of included articles was also performed. The interrater reliability for final inclusion after full-text screening was 1.00 (100% agreement).
Data Extraction
The data extraction was performed by the 2 reviewers. Data that could answer the primary question were extracted, such as alpha angle thresholds for cam morphology (including alpha angle upper limits, 95% CI, etc) and the imaging modality used. The 2 reviewers extracted the data independently, with disagreements resolved through a consensus meeting.
Risk of Bias (Quality) Assessment
The risk of bias of the included studies was scored by the Cochrane Risk of Bias Tool (2.0)19 for randomized controlled trials (RCTs), the MINORS (Methodological Index for Non-Randomized Studies) scale44 for non-RCTs, and the Newcastle-Ottawa Scale (NOS)51 for case-control and cohort studies, as described in the PROSPERO protocol. Ultimately, only case-control and cohort studies were included in this systematic review, meaning that only the NOS assessment was performed. This tool focuses on 3 areas: the selection of groups, comparability of groups, and ascertainment of outcome. This tool results in a total score from 0 to 9, with 9 indicating the highest study quality. The 2 reviewers independently performed the risk of bias assessment, and discrepancies between the reviewers were resolved by a consensus meeting. The interrater reliability for the NOS score was 0.93 (95% CI, 0.81-0.98).
Synthesis of the Data
A meta-analysis was not performed because of significant methodological and clinical heterogeneity among included studies. Heterogeneity was primarily found in participant characteristics, imaging technique, exposures and outcomes, study designs, and risk of bias per study.
Results
Selection of Studies
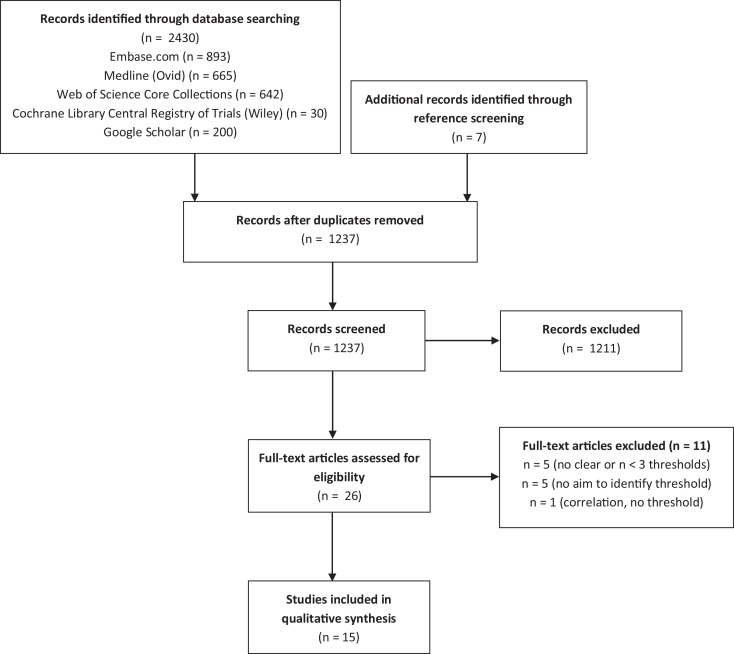
We identified 2437 titles after the initial review, of which 15 studies qualified for inclusion in the quality assessment and analysis (Figure 1).
Figure 1.
Flow diagram of the selection process, following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 guidelines.
Characteristics of the Included Studies
In this systematic review, 4 case-control studies,7,11,31,45 10 cohort studies,5,9,12–15,25,26,32,40 and 1 finite-element study28 were included. All the findings are summarized in Tables 1 and 2.
Table 1.
Case-Control Studiesa
| Authors, Year | Study Design | Cases | Controls | Imaging Modality Used? | Symptoms, Intra-Articular Pathology, OA, THR? | Methodology for Determining Threshold | Suggested Threshold Value | Confounders | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases (Hips) | Mean Age (Measure of Variation) | Sex (%, Male/Female) | (A)symptomatic | N (Hips) | Mean Age (Measure of Variation) | Sex (%, Male/Female) | (A)symptomatic | Type | Plane | ||||||
| Barrientos, 20167 | Case-control | 38 (38) | 36.1 ± 11.8 | 55/45 | Symptomatic | 101 (202) | 36.8 ± 14.4 | 41/59 | Asymptomatic | CT | Oblique axial, anterolateral 1:30-o’clock | Cases: symptomatic FAI, undergoing hip arthroscopy controls: asymptomatic | ROC | 57° | No differences in sex or age |
| Espie, 201411 | Case-control | 75 (96) | 38 (95% CI, 36-40) |
77/23 | Both | 50 (100) | 36.2 (95% CI, 34-38.4) |
54/46 | Asymptomatic | Radiograph | Frog-leg lateral | Cases: (a)symptomatic FAI controls: asymptomatic | 95% reference interval | Male: 63° Female: 58° (total: 60°) | No significant difference in age and height |
| Mascarenhas, 201831 | Case-control | 176 (176) | 35.6 ± 9 | 50/50 | Symptomatic | 372 (372) | 33.9 ± 8 | 50/50 | Asymptomatic | MRI | 360° clockwise, radial (NFS) | Cases: symptomatic FAI undergoing hip surgery Controls: asymptomatic |
ROC | 58°-60° | Weight, age, sex matched |
| Sutter, 201245 | Case-control | 53 (NFS) | 35.6 (range, 20-50) |
62/38 | Symptomatic | 53 (NFS) | 34.5 (range, 23-50) |
58/42 | Asymptomatic | MRI | Transverse-oblique: AI, anterior, AS, superior, PS | Cases: symptomatic FAI with cam morphology. Controls: asymptomatic | ROC | 60° | Age and sex matched |
aAI, anteroinferior; AS, anterosuperior; CT, computed tomography; FAI, femoroacetabular impingement; MRI, magnetic resonance imaging; NFS, not further specified; OA, osteoarthritis; PS, posterosuperior; ROC, receiver operating characteristic; THR, total hip replacement.
Table 2.
Cohort Studies (and 1 Finite-Element Study)a
| Authors, Year | Study Design | Cohort Characteristics | Imaging Modality Used? | Symptoms, Intra-Articular Pathology, OA, THR? | Methodology of Determining Threshold Value | Suggested Threshold Value | Confounders | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases (Hips) | Mean Age (Measure of Variation) | Sex (%, Male/Female) | (A)symptomatic | Type | Plane | ||||||
| Agricola, 20145 | Prospective cohort | 1457 (2879) | CHECK: mean 55.9 (range, 45-65) Chingford: mean 54.2 (range, 44-67) | CHECK: 20/80 Chingford: 0/100 |
Both | Radiograph | AP/coronal | Pathological cam: end-stage OA within 5-19 years (n = 105) versus no end-stage OA (n = 2774) | Cam morphology: based on bimodal alpha angle distribution, pathological cam morphology: ROC | cam: 60° pathological cam: 78° |
Separate male and female, uni/bilateral, no correction for age |
| Bouma, 20149 | Cross-sectional cohort | 83 (155) | N/A | NFS | Asymptomatic | Radiograph | Cross-table lateral | 95% reference interval | 66° (anatomic method) 58° (3-point method) |
No significant difference in alpha angle in male/female | |
| Fischer, 201812 | Cross-sectional cohort | 3226 (NFS) | 53 ± 14 (range, 21-90) | 49/51 | NFS | MRI (whole body) | AP/coronal | 95% reference interval | 71° | Significant association between age, weight, waist, BMI, height, and alpha angle | |
| Fraitzl, 201313 | Retrospective cohort | 339 (339) | Male: 47 ± 17, female: 55 ± 19 | 50/50 | NFS | Radiograph | AP/coronal and FLL | 95% reference interval | Male (AP/FLL): 70°/70° Female (AP/FLL): 61°/66° |
No correlation between age and alpha angle | |
| Golfam, 201714 | Cross-sectional cohort | 197 (394) | 29.4 (range, 21.4-50.6) | 44/56 | Asymptomatic | MRI | Oblique axial, radial, 1:30-o’clock | 95% reference interval | Axial: 63° Radial: 66° |
Insignificant relation between age and alpha angle, significant relation between sex and alpha angle | |
| Gosvig, 200715 | Cross-sectional cohort | 2803 (NFS) | NFS | 38/62 | NFS | Radiograph | AP/coronal | cam morphology: mean ± 1SD Pathological cam morphology: mean ± 2SD |
Male: 69° (borderline), 83° (pathological) Female: 51° (borderline), 57° (pathological) |
Specified for sex | |
| Laborie, 201425 | Cross-sectional cohort | 2005 (FLL: 3996, AP: 4004) | 18.6 (95% CI, 17.2-20.1) | 42/58 | NFS | Radiograph | AP/coronal (weightbearing) and FLL | 97.5% percentile | Male (AP/FLL): 93°/68° Female (AP/FLL): 94°/56° | Specified for sex and side | |
| Lepage-Saucier, 201426 | Cross-sectional cohort | 94 (188) | 49 ± 16.6 | 52/48 | Asymptomatic | CT | Oblique axial (90°) and double oblique (45°) | 95% reference interval | Male (45°/90°): 93°/68° Female (45°/90°): 84°/69° |
Specified for sex and side | |
| Liu, 201728 | Experimental finite-element study | 1 (1) multiple modeled hips | 35 | 0/100 | NFS | CT | AP/coronal | Peak acetabulum pressure: 60° = 6.295, 70° = 7.291, 80° = 10.620, 90° = 11.460 |
Peak pressure forces between various threshold values and motions | 80° | N/A |
| Mascarenhas, 201832 | Cross-sectional cohort | 590 (1111) | 33 ± 8 | 46/54 | Asymptomatic | CT | Pelvis: 9 positions around head-neck | 95% reference interval | 65°-70° for 12.00/3.00-o’clock 60° for 1- to 1.30-o’clock | Age, side, limb dominance, and sex | |
| Pollard, 201040 | Cross-sectional cohort | 83 (166) | 46 (range, 22-69) | 47/53 | Asymptomatic | Radiograph | Cross-table lateral | 95% reference interval | 62° | No significant difference between sex | |
aAP, anteroposterior; BMI, body mass index; CHECK, Cohort Hip & Cohort Knee; CT, computed tomography; FLL, frog-leg lateral; MRI, magnetic resonance imaging; N/A, not available; NFS, not further specified; OA, osteoarthritis; ROC, receiver operating characteristic; THR, total hip replacement.
Population Characteristics
The sample size of the studies ranged from 128 to 322612 (median, 197), with the number of hips ranging between 128 and 400425 (median, 339). The mean age of all study populations ranged from 18.625 to 55.95 years (median, 38). In 4 studies,7,11,26,45 more male than female participants were included; in 8 studies,5,12,14,15,25,28,32,40 more women than men were included; in 1 study,9 participant sex was not specified; and in 2 studies,13,31 the sex distribution was equal. Of the 4 case-control studies, 37,31,45 included patients with FAIS, while 1 study11 defined patients with hip pain as cases without specifying whether they fulfilled the FAIS criteria. All control participants were asymptomatic. In the 10 cohort studies, 5 studies9,14,26,32,40 specifically described their population as asymptomatic, 1 study5 had both symptomatic and asymptomatic participants, and the remaining 4 studies12,13,15,25 did not further specify this. The finite-element study28 also did not specify this.
Risk of Bias Within Studies
After inclusion, the interrater reliability for NOS scores suggested a moderate agreement (κ = 0.69). According to the results of the NOS tool and the predefined criteria, 9 studies (3 case-control11,31,45 and 6 cohort5,12,15,25,26,32) scored 5 points or higher (Table 3).
Table 3.
The Newcastle-Ottawa Scale Scores per Studya
| Authors, Year | Study Design | NOS Score | ||
|---|---|---|---|---|
| Selection | Comparability | Outcome | ||
| Agricola, 20145 | Prospective cohort |



|

|



|
| Barrientos, 20167 | Case-control |



|

|
|
| Bouma, 20149 | Cross-sectional cohort |


|

|
|
| Espie, 201411 | Case-control |




|


|

|
| Fischer, 201812 | Cross-sectional cohort |



|


|

|
| Fraitzl, 201313 | Retrospective cohort |


|

|
|
| Golfam, 201714 | Cross-sectional cohort |



|

|
|
| Gosvig, 200715 | Cross-sectional cohort |



|

|

|
| Laborie, 201425 | Cross-sectional cohort |



|


|

|
| Lepage-Saucier, 201426 | Cross-sectional cohort |


|


|

|
| Liu, 201728 | Experimental finite-element study |

|

|
|
| Mascarenhas, 201831 | Case-control |



|


|



|
| Mascarenhas, 201832 | Cross-sectional cohort |



|


|

|
| Pollard, 201040 | Cross-sectional cohort |



|

|
|
| Sutter, 201245 | Case-control |



|


|


|
aThe NOS score is a total score of 3 different domains: “selection” (maximum 4 stars), “comparability” (maximum 2 stars) and “outcome” (maximum 3 stars), with a maximum score of 9. Both cohort and case-control studies are presented. A blank cell indicates the lowest score (0 stars). NOS, Newcastle-Ottawa Scale.
Results of Individual Studies
Imaging Modality
Various imaging modalities were utilized in the 15 studies, including radiographs,5,9,11,13,15,25,40 CT,7,26,28,32 and MRI.12,14,31,45 Radiographic views included the AP,5,13,15,25 cross-table lateral,9,40 and frog-leg lateral.11,13,25 CTs were performed in several planes, such as an oblique axial plane,7,26 of which 1 was reconstructed,7 double-oblique plane,26 coronal plane,28 and alpha angle measured at 9 different positions around the femoral head-neck junction.32 The MRIs were performed in an oblique axial plane and radial view (1 study14), a coronal plane (1 study12), and a transverse-oblique plane parallel to the femoral neck axis (1 study45); 1 study31 did not specify the plane.
Symptoms, Intra-articular Pathology, OA, and THR
Six studies5,7,11,28,31,45 reported symptoms, intra-articular pathology, hip OA, and/or THR. One study5 showed that an alpha angle of 78° gave the maximum area under the ROC curve, which was 0.69 (95% CI, 0.62-0.75), for end-stage OA. A second study28 investigated the alpha angle in relation to peak pressure in the acetabulum and showed that if the alpha angle increased, the peak pressure increased as well. All 4 case-control studies, of which 3 used the ROC,7,31,45 reported their diagnostic alpha angle threshold for their patients with FAIS as compared with their asymptomatic controls.
Method of Determining Alpha Angle Threshold
Several methods of determining the alpha angle threshold were used in the studies. In 89,11–14,26,32,40 of the 15 studies, the 95% reference interval was used. This was measured as the mean ± 1.96 SD, and the upper limit was chosen as the threshold. In 1 study,25 the 97.5% percentile was used, and in 1 study15 the mean ± 1SD for cam morphology and the mean ± 2SD for pathological cam were used. In 4 studies,5,7,31,45 ROC curve analysis was used to assess the alpha angle threshold, which best distinguished the presence and absence of FAIS7,31,45 or end-stage OA.5 One study5 based their cam morphology threshold on the bimodal distribution of the alpha angle. The finite-element study28 measured peak contract pressure on the acetabular cartilage between various thresholds and motions.
Alpha Angle Threshold
Measurement Methods
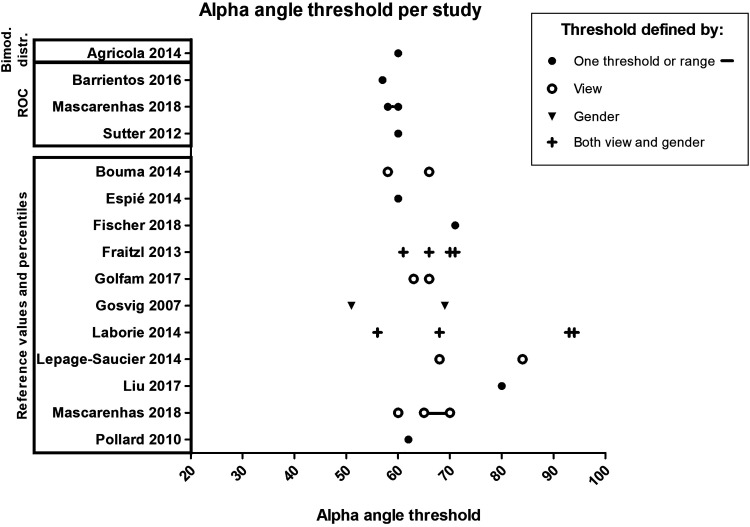
Four studies5,7,31,45 reported an alpha angle threshold for cam morphology by ROC curve analysis or by using the bimodal distribution. Three of these studies7,31,45 studied FAIS versus asymptomatic participants and suggested that alpha angle thresholds ranged between 57° and 60°. The 8 studies9,11–14,26,32,40 that reported alpha angle threshold values by using the 95% reference interval reported a range from 58° to 93°. In the 3 remaining studies, the study15 reporting the mean ± 1SD for cam morphology determined a suggested alpha angle threshold of 51° and 69° for female and male patients, respectively, and the study25 reporting the 97.5% percentile determined a suggested threshold for frog-leg lateral and AP views between 56° and 94° for female patients and 68° and 93° for male patients. The finite-element study28 suggested a threshold of 80° (Figure 2).
Figure 2.
The alpha angle thresholds summarized across all included studies. ROC, receiver operating characteristic.
Sex-Based Differences
Six studies,11–13,15,25,26 all using the 95% reference interval, mean ± 1SD or 2SD, or the 97.5th percentile, suggested different thresholds for male and female patients, with alpha angle thresholds ranging from 63° to 93° in men and 58° to 94° in women.
Discussion
We found 15 studies aimed at determining an alpha angle threshold to distinguish between hips with and without cam morphology. Most studies proposed an alpha angle threshold based on the upper limit of the 95% reference interval, and 3 studies7,31,45 were based on ROC curve analyses as 1 study5 was based on a bimodal distribution. Although a definite threshold value remains subjective, we suggest to report a threshold value of ≥60° to classify cam morphology based on the currently available literature.
Most studies (12 of 15) used the upper limit of the 95% reference interval or comparable methods such as the +1SD, +2SD, or 97.5% percentile as the cutoff value to define the presence of cam morphology. While reference values in an asymptomatic population might give an indication, it might for several reasons not be the optimal approach for quantifying cam morphology. The assumption that only the upper 2.5% of an asymptomatic population has cam morphology is probably incorrect, given the high prevalence of this abnormality in the asymptomatic population.33 Cam morphology might be more prevalent in male than in female patients, resulting in higher mean alpha angles in men than in women when a given population is being studied.20,21,27,40 Higher prevalence of mixed-type morphology is also observed in male compared with female patients.10,36 However, this does not imply that the alpha angle threshold should automatically be lower in female than in male patients, something that was proposed by 3 studies13,15,25 included in this systematic review. This is one of the reasons for the wide range of proposed alpha angle threshold values—between 51° and 94°—in studies using this methodology.
One study5 used the distribution of the alpha angle to propose a threshold value. This study combined data of 2 large cohorts that both independently showed a bimodal distribution of the alpha angle. Combining these alpha angle data resulted in a non–sex specific threshold of 60° to discriminate between hips with and without cam morphology. Interestingly, a bimodal distribution naturally shows a distinction between normal and abnormal alpha angles and is therefore optimal to determine cutoff values. Three studies7,31,45 used ROC analysis to distinguish asymptomatic people from patients with FAIS, which is clinically a much more relevant method, as cam morphology can be highly prevalent in asymptomatic people. These studies showed consistent threshold values ranging between 57° and 60°.
Utilizing a consistent alpha angle threshold and imaging modality to classify cam morphology is important to study etiology, compare prevalence numbers, and study associations with concurrent pathology. Based on the above-mentioned current literature arguments, we feel that an alpha angle threshold of ≥60° to quantify cam morphology would currently be the most appropriate value. This threshold was also found to be most appropriate by a recent scoping review.30 However, we also acknowledge that it remains subjective as to where to draw the threshold line. There might also be reasons for not dichotomizing the alpha angle and studying it as a continuous variable, for example in prognostic studies. Further research is required to determine this.
It is important to note that the ≥60° threshold is proposed as a classification criterion for cam morphology, which is different from a diagnostic criterion. Classification criteria intend to create a relatively homogeneous well-defined cohort for clinical research and do not intend to capture the more heterogeneous population of FAIS patients.1 In order to use cam morphology for the clinical diagnosis of FAIS, more anatomic variables should be considered, such as the femoral torsion, neck-shaft angle, and acetabular morphology, as well as clinical findings and patient symptoms. We therefore do not suggest using this threshold value in isolation for clinical decision making. It should be kept in mind that, although studies7,31,45 using ROC curve analysis generally showed that a 60° threshold could best distinguish patients with FAIS from asymptomatic people, there was still an overlap of these groups around the 60° threshold.
A wide range of imaging modalities and views were used in the included studies. For the purpose of the current systematic review, we described all outcomes of suggested alpha angle threshold values irrespective of the imaging modality or view used. Owing to study heterogeneity, it was not possible to pool studies based on the imaging modality or view used. Most studies used AP radiographs or 3D imaging reformatted as an AP view/coronal plane. Studies using ROC analyses, on which we mostly based our conclusions, also used different planes such as the coronal, oblique axial, clockwise radial (2-o’clock), and transverse-oblique planes. In these studies, a threshold of ≥60° was suggested utilizing these planes as well. Thus, despite heterogeneity in modalities and views, the studies concluded the same thresholds to distinguish between hips with and without cam morphology. Still, radiographs (2D view) are limited by the fact that positional differences can limit reproducibility, and only certain locations of the head-neck junction—depending on the type of view—can be studied, which might result in underestimation of cam morphology. Most included studies that used 3D imaging also reduced the analysis to 2 or 3 planes, thereby also suffering from potential cam morphology underestimation. Only the 2 studies by Mascarenhas et al31,32 used radial formatted reconstructions around the femoral head-neck junction and measured the alpha angle on multiple locations around the femoral neck. One of these studies,32 using the 95% reference interval to determine an alpha angle threshold value, suggested a 60° threshold for the 1- to 1:30-o’clock position and 65° and 70° for the 12-o’clock and 3-o’clock positions, respectively. Future studies should evaluate whether the suggested threshold of ≥60° is applicable for all imaging modalities and/or views before diagnostic criteria can be introduced.
Limitations
There are limitations related to the included studies, which need to be addressed. First, although some large studies with up to 3226 participants were included, 9 of the 15 studies had less than 200 participants. There were also studies with a high risk of bias. Most studies (11 of 15) scored high (at least 3 of 4 points) on the NOS item “selection,” as we considered most participants representative of people that can have cam morphology. However, only 2 studies scored 3 (of 3) points on the item “outcome.” As mentioned before, there was large heterogeneity in multiple factors, such as age, imaging modality and view used, sex, and the methodology used to study threshold values.
Conclusion
Based on the available literature on alpha angle threshold values, we suggest reporting a non–sex specific threshold of ≥60° to classify cam morphology.
APPENDIX
Search Strategy
EMBASE
(`hip disease'/exp OR `hip'/exp OR `hip arthroscopy'/de OR `hip radiography'/de OR `cam type femoroacetabular impingement'/de OR (femoroacetabul* OR femor*-acetabular* OR femoracetabul* OR cam OR hip OR hips OR cox OR coxae):ab, ti) AND ('alpha angle'/de OR `notzli alpha angle'/de OR `dunn 45 alpha angle'/de OR `dunn 90 alpha angle'/de OR `alpha angle measurement'/de OR `alpha angle threshold value'/de OR `alpha angle of femur'/de OR `reverse alpha angle'/de OR (((alpha OR a OR dunn OR notzli) NEAR/3 (angle* OR degree*))):ab, ti)
MEDLINE Ovid
(Hip Injuries/ OR exp Hip/ OR (femoroacetabul* OR femor*-acetabular* OR femoracetabul* OR cam OR hip OR hips OR cox OR coxae).ab, ti.) AND ((((alpha OR dunn OR notzli) NEAR/3 (angle* OR degree*))).ab, ti.)
Web of Science
TS=(((femoroacetabul* OR (femor* next acetabular*) OR femoracetabul* OR cam OR hip OR hips OR cox ORcoxae)) AND ((((alpha OR a OR dunn OR notzli) NEAR/2 (angle* OR degree*)))))
Cochrane CENTRAL
((femoroacetabul* OR (femor* next acetabular*) OR femoracetabul* OR cam OR hip OR hips OR cox OR coxae):ab, ti) AND ((((alpha OR a OR dunn OR notzli) NEAR/3 (angle* OR degree*))):ab, ti)
Google Scholar
femoroacetabulal|“femoral|femoroacetabular”|femoracetabular|“cam impingement|deformity|morphology|lesion|type”|hip|hips|cox|coxae "alpha|a|dunn|notzli angle| angles|degree|degrees"|“angle alpha”
Footnotes
Final revision submitted March 8, 2020; accepted March 15, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Aggarwal R, Ringold S, Khanna D, et al. Distinctions between diagnostic and classification criteria? Arthritis Care Res (Hoboken). 2015;67(7):891–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Agricola R, Bessems JH, Ginai AZ, et al. The development of cam-type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40(5):1099–1106. [DOI] [PubMed] [Google Scholar]
- 3. Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–923. [DOI] [PubMed] [Google Scholar]
- 4. Agricola R, Heijboer MP, Ginai AZ, et al. A cam deformity is gradually acquired during skeletal maturation in adolescent and young male soccer players: a prospective study with minimum 2-year follow-up. Am J Sports Med. 2014;42(4):798–806. [DOI] [PubMed] [Google Scholar]
- 5. Agricola R, Waarsing JH, Thomas GE, et al. Cam impingement: defining the presence of a cam deformity by the alpha angle: data from the CHECK cohort and Chingford cohort. Osteoarthritis Cartilage. 2014;22(2):218–225. [DOI] [PubMed] [Google Scholar]
- 6. Audenaert EA, Peeters I, Vigneron L, Baelde N, Pattyn C. Hip morphological characteristics and range of internal rotation in femoroacetabular impingement. Am J Sports Med. 2012;40(6):1329–1336. [DOI] [PubMed] [Google Scholar]
- 7. Barrientos C, Barahona M, Diaz J, Branes J, Chaparro F, Hinzpeter J. Is there a pathological alpha angle for hip impingement? A diagnostic test study. J Hip Preserv Surg. 2016;3(3):223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Beaule PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23(6):1286–1292. [DOI] [PubMed] [Google Scholar]
- 9. Bouma H, Slot NJ, Toogood P, Pollard T, van Kampen P, Hogervorst T. Where is the neck? Alpha angle measurement revisited. Acta Orthop. 2014;85(2):147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. [DOI] [PubMed] [Google Scholar]
- 11. Espie A, Chaput B, Murgier J, Bayle-Iniguez X, Elia F, Chiron P. 45° -45° -30° frog-leg radiograph for diagnosing cam-type anterior femoroacetabular impingement: reproducibility and thresholds. Orthop Traumatol Surg Res. 2014;100(8):843–848. [DOI] [PubMed] [Google Scholar]
- 12. Fischer CS, Kuhn JP, Ittermann T, et al. What are the reference values and associated factors for center-edge angle and alpha angle? A population-based study. Clin Orthop Relat Res. 2018;476(11):2249–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fraitzl CR, Kappe T, Pennekamp F, Reichel H, Billich C. Femoral head-neck offset measurements in 339 subjects: distribution and implications for femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1212–1217. [DOI] [PubMed] [Google Scholar]
- 14. Golfam M, Di Primio LA, Beaule PE, Hack K, Schweitzer ME. Alpha angle measurements in healthy adult volunteers vary depending on the MRI plane acquisition used. Am J Sports Med. 2017;45(3):620–626. [DOI] [PubMed] [Google Scholar]
- 15. Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89(10):1309–1316. [DOI] [PubMed] [Google Scholar]
- 16. Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92(5):1162–1169. [DOI] [PubMed] [Google Scholar]
- 17. Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–1176. [DOI] [PubMed] [Google Scholar]
- 18. Hack K, Di Primio G, Rakhra K, Beaule PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444. [DOI] [PubMed] [Google Scholar]
- 19. Higgins JPT, Sterne JAC, Savovic J, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database of Systematic Reviews. 2016;10(suppl 1):29–31. [Google Scholar]
- 20. Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93(10):1303–1307. [DOI] [PubMed] [Google Scholar]
- 21. Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93(19): 1842–1852. [DOI] [PubMed] [Google Scholar]
- 22. Kapron AL, Anderson AE, Peters CL, et al. Hip internal rotation is correlated to radiographic findings of cam femoroacetabular impingement in collegiate football players. Arthroscopy. 2012;28(11):1661–1670. [DOI] [PubMed] [Google Scholar]
- 23. Kapron AL, Peters CL, Aoki SK, et al. The prevalence of radiographic findings of structural hip deformities in female collegiate athletes. Am J Sports Med. 2015;43(6):1324–1330. [DOI] [PubMed] [Google Scholar]
- 24. Khanna V, Caragianis A, Diprimio G, Rakhra K, Beaule PE. Incidence of hip pain in a prospective cohort of asymptomatic volunteers: is the cam deformity a risk factor for hip pain? Am J Sports Med. 2014;42(4):793–797. [DOI] [PubMed] [Google Scholar]
- 25. Laborie LB, Lehmann TG, Engesaeter IO, Sera F, Engesaeter LB, Rosendahl K. The alpha angle in cam-type femoroacetabular impingement: new reference intervals based on 2038 healthy young adults. Bone Joint J. 2014;96(4):449–454. [DOI] [PubMed] [Google Scholar]
- 26. Lepage-Saucier M, Thiery C, Larbi A, Lecouvet FE, Vande Berg BC, Omoumi P. Femoroacetabular impingement: normal values of the quantitative morphometric parameters in asymptomatic hips. Eur Radiol. 2014;24(7):1707–1714. [DOI] [PubMed] [Google Scholar]
- 27. Leunig M, Juni P, Werlen S, et al. Prevalence of cam and pincer-type deformities on hip MRI in an asymptomatic young Swiss female population: a cross-sectional study. Osteoarthritis Cartilage. 2013;21(4):544–550. [DOI] [PubMed] [Google Scholar]
- 28. Liu Q, Wang W, Thoreson AR, Zhao C, Zhu W, Dou P. Finite element prediction of contact pressures in cam-type femoroacetabular impingement with varied alpha angles. Comput Methods Biomech Biomed Engin. 2017;20(3):294–301. [DOI] [PubMed] [Google Scholar]
- 29. Lohan DG, Seeger LL, Motamedi K, Hame S, Sayre J. Cam-type femoral-acetabular impingement: is the alpha angle the best MR arthrography has to offer? Skeletal Radiol. 2009;38(9):855–862. [DOI] [PubMed] [Google Scholar]
- 30. Mascarenhas VV, Ayeni OR, Egund N, et al. Imaging methodology for hip preservation: techniques, parameters, and thresholds. Semin Musculoskelet Radiol. 2019;23(3):197–226. [DOI] [PubMed] [Google Scholar]
- 31. Mascarenhas VV, Rego P, Dantas P, et al. Can we discriminate symptomatic hip patients from asymptomatic volunteers based on anatomic predictors? A 3-dimensional magnetic resonance study on cam, pincer, and spinopelvic parameters. Am J Sports Med. 2018;46(13):3097–3110. [DOI] [PubMed] [Google Scholar]
- 32. Mascarenhas VV, Rego P, Dantas P, et al. Hip shape is symmetric, non-dependent on limb dominance and gender-specific: implications for femoroacetabular impingement. A 3D CT analysis in asymptomatic subjects. Eur Radiol. 2018;28(4):1609–1624. [DOI] [PubMed] [Google Scholar]
- 33. Mascarenhas VV, Rego P, Dantas P, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: a systematic review. Eur J Radiol. 2016;85(1):73–95. [DOI] [PubMed] [Google Scholar]
- 34. Mosler AB, Agricola R, Thorborg K, et al. Is bony hip morphology associated with range of motion and strength in asymptomatic male soccer players? J Orthop Sports Phys Ther. 2018;48(4):250–259. [DOI] [PubMed] [Google Scholar]
- 35. Nelson AE, Stiller JL, Shi XA, et al. Measures of hip morphology are related to development of worsening radiographic hip osteoarthritis over 6 to 13 year follow-up: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage. 2016;24(3):443–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nepple JJ, Riggs CN, Ross JR, Clohisy JC. Clinical presentation and disease characteristics of femoroacetabular impingement are sex-dependent. J Bone Joint Surg Am. 2014;96(20):1683–1689. [DOI] [PubMed] [Google Scholar]
- 37. Nicholls AS, Kiran A, Pollard TC, et al. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: a nested case-control study. Arthritis Rheum. 2011;63(11):3392–3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. [DOI] [PubMed] [Google Scholar]
- 39. Palmer A, Fernquest S, Gimpel M, et al. Physical activity during adolescence and the development of cam morphology: a cross-sectional cohort study of 210 individuals. Br J Sports Med. 2018;52(9):601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pollard TC, Villar RN, Norton MR, et al. Femoroacetabular impingement and classification of the cam deformity: the reference interval in normal hips. Acta Orthop. 2010;81(1):134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reichenbach S, Juni P, Werlen S, et al. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken). 2010;62(9):1319–1327. [DOI] [PubMed] [Google Scholar]
- 42. Saberi Hosnijeh F, Zuiderwijk ME, Versteeg M, et al. Cam deformity and acetabular dysplasia as risk factors for hip osteoarthritis. Arthritis Rheumatol. 2017;69(1):86–93. [DOI] [PubMed] [Google Scholar]
- 43. Sankar WN, Nevitt M, Parvizi J, Felson DT, Agricola R, Leunig M. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2013;21 (suppl 1): S7–S15. [DOI] [PubMed] [Google Scholar]
- 44. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 45. Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW. How useful is the alpha angle for discriminating between symptomatic patients with cam-type femoroacetabular impingement and asymptomatic volunteers? Radiology. 2012;264(2):514–521. [DOI] [PubMed] [Google Scholar]
- 46. Swartz MK. The PRISMA statement: a guideline for systematic reviews and meta-analyses. J Pediatr Health Care. 2011;25(1):1–2. [DOI] [PubMed] [Google Scholar]
- 47. Thomas GE, Palmer AJ, Batra RN, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthritis Cartilage. 2014;22(10):1504–1510. [DOI] [PubMed] [Google Scholar]
- 48. van Klij P, Ginai AZ, Heijboer MP, Verhaar JAN, Waarsing JH, Agricola R. The relationship between cam morphology and hip and groin symptoms and signs in young male football players. Scand J Med Sci Sports. 2020;30(7):1221–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. van Klij P, Heerey J, Waarsing JH, Agricola R. The prevalence of cam and pincer morphology and its association with development of hip osteoarthritis. J Orthop Sports Phys Ther. 2018;48(4):230–238. [DOI] [PubMed] [Google Scholar]
- 50. van Klij P, Heijboer MP, Ginai AZ, Verhaar JAN, Waarsing JH, Agricola R. Cam morphology in young male football players mostly develops before proximal femoral growth plate closure: a prospective study with 5-year follow-up. Br J Sports Med. 2019;53(9):532–538. [DOI] [PubMed] [Google Scholar]
- 51. Wells GS, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed November 11, 2018 http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp