Abstract
Background
Up to one third of oncologists experience burnout. The objective was to determine correlates of work related stress in gynecologic oncologists (GOs)
Methods
Using an online tool, we surveyed 273 members of the International Gynecologic Cancer (IGCS) Society (60% from North America) to examine demographic, psychological and spiritual correlates of work related stress (WRS) and burnout. Measures of death anxiety (DA) and locus of control (LOC) were also administered.
Results
WRS did not correlate with religion, religiosity, race, or gender, but did correlate with DA (r = 0.23, p = 0.0006). WRS also was also associated younger age (p = 0.01) and fewer years out of training (p= 0.0286), higher scores on LOC Chance (r = 0.18, p = 0.007), higher scores on Powerful Other (r = 0.30, p < 0.0001), and lower scores on LOC Internality (r = −0.30, p < 0.0001).
Conclusion
Responses from younger and less experienced GOs, correlate with higher WRS scores especially if their LOC is weighted toward chance and powerful others. Responses of GO’s with these two characteristics also correlate with higher DA scores and reports of difficulty talking about death.
Keywords: work related strain, gynecologic oncologist, death anxiety, locus of control
Introduction
Individuals choose oncology as a profession for many reasons including intellectual challenge, personal satisfaction, and perhaps a feeling of sacred vocation. [1] Despite these desirable career traits, oncologists, experience high levels of emotional stress that can lead to burnout. [2, 3] Between 30–50% of medical oncologists are at risk for burnout; rates for surgical oncologists are as high as 28% and are more common among younger and female surgeons. [4] For surgeons, burnout may result from multiple stressors including challenges with office politics, economic pressure, time spent at the job, new technical challenges in the operating room, medical-legal issues, and lack of positive feedback. [1] In oncology, burnout can further be exacerbated by tragic patient scenarios and over empathizing, counter transference, and feelings of failure as the patient loses her battle with cancer, essentially compassion fatigue. [5] Further, this type of burnout may be a form of subconscious anxiety buffering, a type of “Terror Management”. [6]
Predictions for increased rates of cancer incidence over the next 20 years are well documented with notable shortages expected in the number of needed oncology specialists. [7] In addition, financial burdens are increasingly worrisome for both patients and physicians; loss of health care insurance , decreased reimbursement levels, and pressure to see more patients within tight time constraints add to all this. If increasing WRS negatively impacts physician’s ability to be compassionate and empathetic towards patients, there might be both direct and indirect consequences including decreased levels of patient satisfaction, decreased quality of care, and significant detriments to the physician’s career and QOL.
Gynecologic oncologists may be at increased risk for the aforementioned stressors. First, the number of practicing gynecologic oncologists is relatively small, with only 43 training programs in the country and 47 physicians graduating on an annual basis. Second, the gynecologic oncologist is trained to manage not only the surgical aspect of the cancer treatment but also the chemotherapy. Depending upon the scope of their practice, gynecologic oncologists may need to remain current on surgical advances including robotic techniques as well as the newest therapeutic agents. Additionally, the diagnosis of a gynecologic cancer often leads to treatments that might affect women’s view of themselves, namely sexuality and fertility and the “usual cancer threats” such as mortality, sense of self, sense of meaning in life, or spirituality, symptoms of which may require supportive interventions from GOs.
In an effort to explore the emotional / psychological state of gynecologic oncologists and how this might affect clinical encounters, we surveyed members of the International Gynecologic Cancer Society (IGCS), regarding their spiritual beliefs, their tendency towards a locus of control of internal, chance, or powerful other (LOC), work related strain levels (WRS), and death anxiety (DA). The objective was to compare physician demographics and a variety of psychological and spiritual surveys, to assess correlations between beliefs, LOC, and WRS. The initial phase of this research has been published. [8]
Methods
We sent an anonymous survey to 1,972 members of the IGCS and SGO via SurveyMonkey, an online survey management tool. Participants received surveys via email twice, approximately one month apart, with an introductory letter assuring that all information would be kept confidential. Participants were informed that completion of the survey implied consent. This study was approved by The University of Texas MD Anderson Cancer Center (Houston, Texas) institutional review board. Surveys were numerically coded prior to being sent. Investigators involved in data base management and statistical analyses did not have access to identities of study participants. Demographic information collected included age, gender, sex, ethnicity, specialty, practice setting, years of experience, and country of practice.
Religious Affiliation
Respondents were asked their religious affiliation. For the purpose of this analysis, responses were classified as Catholic/Episcopalian, Protestant, Eastern Orthodox, Jewish, Eastern (Hindu, Buddhist, or Sikh), Islam (Muslim or Sufi), no religion (agnostic, atheist, or none).
Spirituality vs Religiosity
Physicians were asked to categorize themselves as i) religious and spiritual; ii) spiritual but not religious; iii) religious but not spiritual; iv) neither spiritual nor or religious; or v) secular/humanist.
Intrinsic Religiosity Survey
Intrinsic religiosity represents the extent to which someone embraces his or her religion as the “master motive” that gives meaning and guidance to his or her life. We used Hoge’s Intrinsic Religiosity Scale (IRS), a 10-item scale that assesses religious beliefs or experiences and is scored from 1 to 5, where higher scores reflect higher religiosity. The scale has high internal reliability and demonstrated validity. [9]
Organizational/Non Organizational Religiosity
Organizational religiosity can be measured by the frequency with which one attends religious services. Non-organizational religiosity refers to the importance of religious beliefs in a person’s daily life. The Duke University Religion Index (DUREL) was used to determine respondents’ organizational religious behavior. Answers are measured on a scale of 1-5, where higher scores indicate higher religiosity. [10]
Locus of Control Scale (LOC)
This 9 item validated questionnaire is a modification of the 24-item scale by Levenson. This scale measures the extent to which people believe in internal control, chance and the powerful other. A higher LOC score suggests the less perceived occurrence of chance events and dependence on powerful others, and increased perceived internal control. [11, 12], [13]
Templer's Death Anxiety Scale (DAS)
The Death Anxiety Scale has 15 true/false questions that measure death fear/anxiety. Higher scores suggest higher death anxiety. Test- retest reliability is 0.83 and the scale has an internal consistency coefficient of 0.76. [14]
Work-Related Strain Inventory (WRSI)
This 18-item survey is designed to measure perceptions of strain in occupational settings. It has a high internal consistency reliability and correlates with the Maslach Burnout Inventory. Higher score indicates higher work related stress. [15]
Statistical Analysis
The Kruskall-Wallis test was used to determine whether responses on scales differed by religious affiliation. A pairwise comparison methods adjusting for multiple tests were used to determine which religious affiliations were significantly different; Tukey-style pairwise comparisons were made to determine differences. [16] We tested for subgroup differences using the Mann-Whitney test; pairwise comparison methods adjusted for multiple comparisons. Two-sided tests were used for all comparisons; a p-value less than 0.05 was considered statistically significant except when examining pair wise comparisons. Bonferonni adjustments were made so that the overall statistical significance after performing multiple tests was 0.05%.
Results
Demographics
Two hundred seventy-three of 1972 physicians responded (14%). Table 1 shows respondents’ demographic characteristics. More than 75% were gynecologic oncologists (performing both surgery and administering chemotherapy). Approximately 75% practiced in an academic setting.
Table 1.
Demographics (N=273)
| Characteristic | N (%) | 2010 SGO Survey [29] |
|---|---|---|
| Age (years) | Avg. 47.6 | 47 yrs (51 yrs 2005) |
| 20–30 | 4 (1.47) | |
| 31–40 | 76 (27.84) | |
| 41–50 | 87 (31.87) | |
| 51–60 | 78 (28.57) | |
| 61–70 | 20 (7.33) | |
| >70 | 8 (2.93) | |
| Sex | ||
| Male | 180 (65.93) | 67% |
| Female | 93 (34.07) | 33% (20% 2005) |
| Ethnicity | ||
| Asian | 55 (20.15) | 11% |
| Black, non-Hispanic | 5 (1.83) | 3% |
| Hispanic | 13 (4.76) | 5% |
| White, non-Hispanic | 182 (66.67) | 83% |
| Middle Eastern | 14 (5.13) | N/A |
| Other | 4 (1.47) | 1% |
| Years of Experience | ||
| 0–5 | 74 (27.11) | 25% (15% 2005) |
| 6–10 | 43 (15.75) | |
| 11–20 | 65 (23.81) | |
| >20 | 91 (33.33) | |
| Practice Location | ||
| United States | 136 (49.82) | |
| Canada | 25 (9.16) | |
| Europe | 44 (16.12) | |
| Asia | 42 (15.38) | |
| Africa | 5 (1.83) | |
| Australia/New Zealand | 7 (2.56) | |
| Central America, South America, Caribbean, and Mexico | 11 (4.03) | |
| Unknown | 3 (1.10) | |
| Affiliation | ||
| Christian | 149 (54.58) | |
| Jewish | 20 (7.33) | |
| None | 46 (16.85) | |
| Eastern | 47 (17.22) | |
| Other | 11 (4.03) | |
Work Related Strain Inventory
Increased WRSI scores did not correlate with religious affiliation (p = 0.67), spiritual self categorization, organizational religiosity, non-organizational religiosity, race or gender. WRSI scores, however, were associated with age (p = 0.01) and years out of training (0.03) so that younger physicians and those most recently out of training reported more stress. WRS did not vary by Country but Middle Eastern GOs trended toward the highest WRS. (Table 2)
Table 2.
Summary Statistics of Inventory Scores (note, N varies due to some with incomplete data)
| Scale | N | Mean (SD) | Median | Min -Max |
|---|---|---|---|---|
| Work-Related Strain Inventory | 221 | 37.52 (6.42) | 37 | 22 – 53 |
| Duke Religion Index - Organizational Dimension | 228 | 3.19 (1.63) | 3 | 1 – 6 |
| Duke Religion Index - Non-Organizational Dimension | 228 | 2.69 (1.82) | 2 | 1 – 6 |
| Duke Religion Index - Intrinsic Religiosity | 228 | 8.64 (3.76) | 9 | 3 – 15 |
| Intrinsic Religiosity Scale | 222 | 27.56 (10.62) | 26 | 10 – 50 |
| Templer Death Anxiety Scale | 224 | 6.01 (2.77) | 6 | 0 – 14 |
| Locus of Control - Chance | 222 | 4.82 (3.81) | 5 | 0 – 17 |
| Locus of Control - Internality | 222 | 13.9 (3.53) | 15 | 0 – 18 |
| Locus of Control - Power of Others | 222 | 3.02 (3.61) | 2 | 0 – 18 |
Locus of Control Scale
Regardless of scores on spiritual measures, physicians had high internal LOC scores (mean of 13.9 on 18 pt scale: SD 3–5, Table 2). LOC did not correlate with age, race, gender, or years out of training. Physicians scored low on powerful others LOC (3.0 +/− 3.6) and chance LOC (4.8 +/− 3.8) Neither internal LOC nor powerful other LOC scores differed by religious affiliation, although there was an association with chance LOC (p = 0.01). A pairwise examination revealed that chance LOC differed between those of Jewish faith (7.38 +/− 3.48) and Protestant faith (3.64 +/− 3.17) (p = 0.0003); such that Jewish respondents tended to have higher chance LOC than Protestant responders.
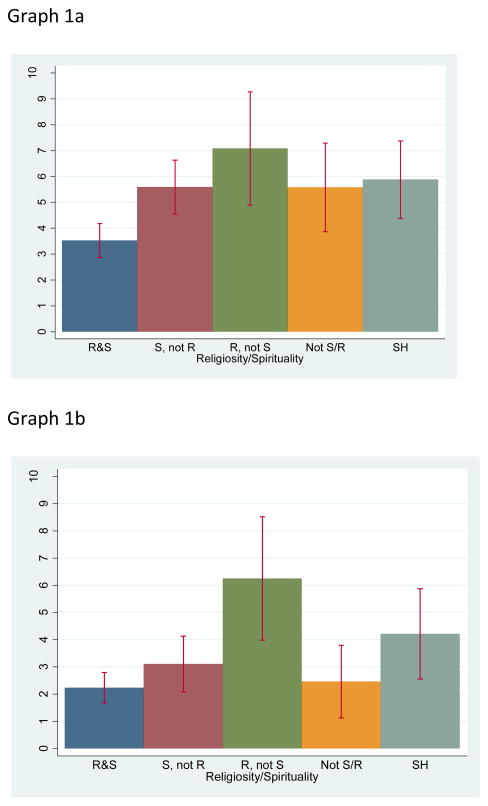
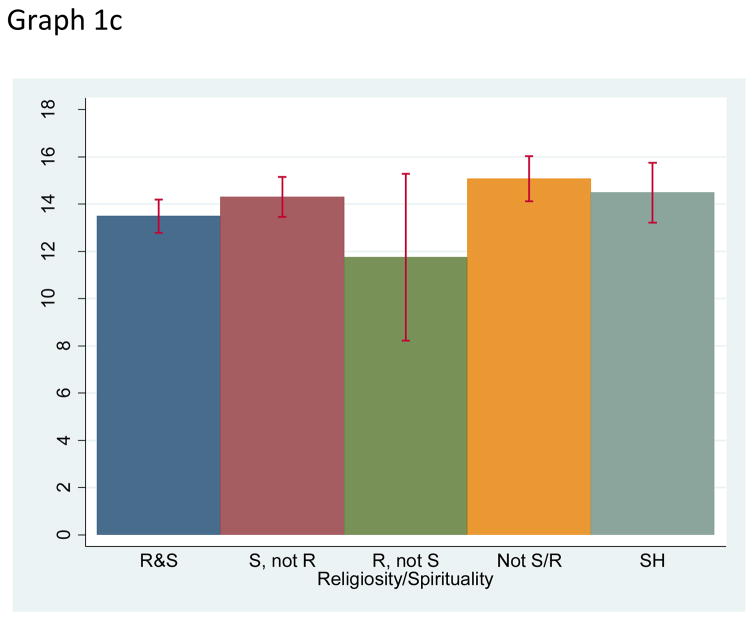
Chance and powerful other LOC also correlated with spiritual self categorization (p = 0.0004 and p = 0.005, respectively), but LOC internality only trended towards statistical significance (p = 0.08), (Graph 1 a, b, c). Those who identified themselves as both religious and spiritual scored lower on chance LOC than those who indicated they were spiritual but not religious (p = 0.0008), those who were religious but not spiritual (p = 0.0009), and secular/humanists (p = 0.002). On the powerful others LOC subscale, physicians who were religious but not spiritual scored higher than those who were religious and spiritual (p = 0.0002) and higher than those who indicated they were neither religious nor spiritual (p = 0.002). Although differences in powerful others LOC and internal LOC scores were found by country (p = 0.04 and p = 0.01, respectively), after adjusting for multiple comparisons, none of the pairwise differences between countries were found to be significant.
Comparison of WRS with LOC
WRSI scores correlated with LOC subscale scores (Table 3). There was a positive correlation with chance LOC (r = 0.18, p = 0.01) and powerful others LOC (r = 0.30, p < 0.0001). There was a negative correlation with internal LOC scores (r = −0.30, p < 0.0001). This indicates that those who experience more WRS have a higher outside LOC (powerful others or chance), while those who experience less stress have a high internal LOC.
Table 3.
Inventory Score Correlations
| WRSI | Duke Religion Index | Intrinsic Religiosity Scale | Death Anxiety | LOC - Chance | LOC - Internality | LOC - Powerful Others | |
|---|---|---|---|---|---|---|---|
| WRSI | 1 | ||||||
| Duke Religion Index | 0.08 | 1 | |||||
| Intrinsic Religiosity Scale | 0.05 | 0.87** | 1 | ||||
| Death Anxiety | 0.23* | −0.01 | 0.01 | 1 | |||
| LOC - Chance | 0.18* | −0.20* | −0.24* | 0.23* | 1 | ||
| LOC - Internality | − 0.30* * | −0.31** | −0.28** | −0.14^ | −0.14^ | 1 | |
| LOC - Powerful Others | 0.30** | -0.01 | −0.03 | 0.24* | 0.57** | −0.26** | 1 |
0.01 <= p < 0.05
0.0001 <= p < .01
p < 0.0001
WRSI also correlated with response to the statement “Telling a patient that they are going to die is difficult for me”. Those that agreed had the highest WRSI scores (r = −0.19, p = 0.006), indicating the highest WRS. This statement also correlated with religious affiliation (p = 0.02), with Protestants tending to agree with this statement more than Hindus, Buddhists, or Sikhs (p = 0.0002). Response to this statement did not correlate with spiritual self-categorization. Those that agreed with the statement had highest DA (p = 0.0002); whereas, those who disagreed and strongly disagreed had the lowest WRSI scores (p = 0.001).
Templers Death Anxiety (TDA)
There was no increase in DA as measured by the TDA by religious affiliation (p = 0.07) or spiritual self categorization, race, gender, or years out of training, but TDA did correlate with age (p = 0.01). Those that agreed with the statement “Telling a patient that they are going to die is difficult for me” also had the highest DA (p = 0.0006). WRSI scores correlated with the Death Anxiety Scale (r = 0.23, p = 0.0006), (Table 2).
Religiosity
The organizational index of the DUREL showed a correlation with both a chance LOC (r = 0.19; p = 0.006) and internal LOC (r = 0.17, p = 0.01) scores, but not powerful others LOC scores (r = 0.06, p = 0.38). Likewise, the non-organizational dimension was correlated with chance LOC (r = 0.22, p = 0.0010) and internal LOC (r = 0.16, p = 0.02), but not powerful others LOC (r = 0.05, p = 0.48). Finally, intrinsic religiosity was correlated with chance LOC (r = 0.20, p = 0.003) and internal LOC (r = 0.31, p < 0.0001), but not with a powerful others LOC (r = 0.01, p = 0.87). This suggests that lower religiosity is associated with a higher chance LOC and higher internal LOC control. Intrinsic religiosity (HOGE) did not correlate with WRSI (r = 0.05, p = 0.44). Intrinsic religiosity correlated with chance LOC (r = −0.24, p = 0.0004) and internal LOC (r = −0.28, p < 0.0001) but not with powerful others LOC suggesting that lower intrinsic religiosity is both associated with higher chance and internal LOC (Table 3).
Discussion
“Although physicians are not gods, they are required to deal with the drama that encompasses theology, human comedy, and tragedy.” [17] Oncologists grapple with an element of psychological stress that relates to the suffering their patients experience. Curing patients, relating to patients, providing symptom control, and the satisfaction associated with knowing they have done their best are important to oncologists. [18] When these things are not possible, burnout and compassion fatigue may ensue. Some have suggested that there is an inverse relationship between age and burnout; and further, that dealing with suffering and death was, in general, less stressful than issues of work overload and work place conflict. [4] The reason for less stress in “experienced” practitioners could be multifactorial and include reasons such as less academic and career stress, no young children at home, and may possibly be related to “lessons learned” (professional experience). [19] In this respect, it may be possible to decrease the incidence of burnout in younger physicians by improvement in the mentoring process as well as open discussions at work to discuss stressful experiences (i.e. professional debriefing). [4]
Dealing with mortality, meaning, and stress is difficult to do on a daily basis. It is known that many patients utilize religious/spiritual beliefs to cope. [20] Our previous research demonstrated that GOs may utilize religious spiritual beliefs to provide self comfort during daily stresses.[8] If one assumes the definition of spirituality is contiguous with “meaning in life” then it is easy to see how career concerns particularly in the field of oncology could translate from a source of physician well being and an opportunity for existential growth to existential anguish, in the words of Victor Frankl, the triad of pain, guilt and death. [21] Recently, physicians have been inclined to write memoirs, such as “My Own Medicine: A Doctor’s Life as a Patient” by Geoffrey Kurland [22] and “The Light Within” by Ramondetta and Sills. [23] Such works may be viewed as the modern day physician’s version of Frankl’s, Man’s Search for Meaning.[21] The continuous exposure to the reality of human mortality may result in an emotional reaction (conscious or unconscious) to the reminder that many of life’s events are not within a person’s control. Measuring the degree to which this “death anxiety” may affect physicians at their job is difficult due to the multidimensional nature of death anxiety. In this vein, studies examining the Terror Management theory/Mortality salience hypothesis suggests that if a cultural worldview (possibly religious in nature) and self-esteem provide protection from the fear of death, then reminding people of their own mortality will increase the need to value one’s own cultural worldview (and become more bound to the “rightness” of their faith) and self-esteem. [24] Thus, dedication to beliefs and self-esteem may insulate from fear of death. [24] In our study, religious affiliation did not, but age and perhaps other unmeasured beliefs/situations relating to human mortality did, correlate with DA and WRS.
The mutually satisfying doctor-patient relationship is important for many oncologists and communication skills are increasingly recognized for their importance in this arena. [25] Communication skills are important in order to effectively explore the patient’s feelings, distribute information, and to provide adequate compassionate support. The physician’s LOC has been explored as a possible contributor to communication effectiveness. [26] The concept of LOC refers to “belief regarding the extent to which life outcomes are controlled by and individual’s actions (internal control) or by external forces such as luck, fate, or other individuals (external control).” [12], [26] Prior studies have suggested that physicians with more internal LOC experienced less burnout than those with external LOC. They hypothesized that more internally oriented oncologists might feel less need to communicate openly as they feel more in control of doctor-patient relationships (e.g. more paternalistic?). The physicians in our study demonstrated a high level of internal control and a low level of belief in powerful others or chance. Interestingly, participants who had a higher internal LOC experienced less WRS than those with a lower internal LOC and conversely, those who had a higher external LOC experienced more WRS than those with a lower external LOC. This raises the question of whether a high internal LOC is necessary for low WRS for a gynecologic oncologist. Teaching communication skills and recognizing cultural differences as well as expanding time for self reflection and the engagement of a team approach (modeled by palliative care teams) may assist in these endeavors especially in the field of gynecologic oncology.[27],[28]
However, if having an external LOC improves communication skills and perhaps leads to more satisfactory patient care but may lead to increased work related stress- this is a very complicated situation. High internal LOC may be a buffering factor, effectively blocking deep patient input and assessments through avoidance in the form of not asking the patient their opinion.[26] This ultimately may decrease physician stress by making a medical decision a lot less complicated. More research should focus on how to help extrinsic LOC physicians avoid burnout as they practice the true art of medicine. And further to evaluate if improved communication skills and more honest self-reflection with mentors and colleagues regarding oncologic WRS and the human limits of medicine might reduce oncologist incidence of burnout. [8],[28]
There are many opportunities for personal growth as well as roads that lead to burnout or compassion fatigue with each patient encounter. [5] In order to combat this risk of psychological harm to physicians (which leads to impaired ability to provide quality care for patients), it is important to recognize skills and coping strategies to help protect them and to avoid these pitfalls. One question that could be explored is whether or not some fostering of existentialism, self reflection or addressing death anxiety might help physicians become more productive and empathetic to their patients, their families and themselves. [5]
Although this is an important topic, this study has significant limitations. We surveyed 1972 members of the SGO and IGCS. Our total response rate was 14% which was not unexpected for a detailed and unfunded physician survey. Therefore, the responses may not represent the opinions of most GOs; furthermore, associations may be under emphasized due to a lack of statistical power. The results should be interpreted with caution and are not necessarily applicable to all members of the SGO and IGCS. As with the nature of this type of inquiry, the respondents may represent a select group of members with the possibility of a response bias. It is unclear if non-responding members were uninterested, too busy, or possibly undervalue self-care. Although the percent of responders was low, the demographics of the respondent sample were not very different than that reported for all of SGO members in the 2010 SGO survey (Table 1). That said, we believe this study is important and should be revised and re-attempted with compensation.
How one's LOC relates to Work Related Strain and Death Anxiety is intriguing. Questions remain as to whether self-reflection and enhanced communication skills would improve the ability for physicians to relate to patients whose LOC is more oriented toward chance and powerful others. Based upon prior studies relating to this subject, research exploring the value of Self reflection and honest mentoring may be an important intervention to reduce work related strain, improve the quality and effectiveness of EOL discussions, and finally expand the potential for existential growth for both the patient and the physician.
Graph 1.
a, b, c: Spiritual Self Categorization and Locus of Control Subscales
Research Highlights.
Increased internal locus of control correlates with decreased work related stress.
Work related stress correlated with personal death anxiety.
Religiosity, race and gender do not correlate with work related stress.
Acknowledgments
This research is supported in part by the National Institutes of Health through M. D. Anderson's Cancer Center Support Grant CA016672
Footnotes
This study was presented in part in abstracts only: Ramondetta LM, Johnson AJ, Urbauer DL, Achanta LM, Thaker PH, Kavanagh JJ, Koenig HG, Sun CC. Religion and Spiritual Beliefs in Gynecologic Oncologist. IGCS 2008 12th Biennial Meeting, International Gynecologic Cancer Society, 10/2008.
Ramondetta LM, Johnson AJ, Sun CC, Achanta L, Kavanagh J, Koenig H. A Survey on the Role of Religion and Spirituality in Gynecologic Oncologist. MASCC/ISOO 2008 International Symposium, 6/2008.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shanafelt T. A career in surgical oncology: finding meaning, balance, and personal satisfaction. Ann Surg Oncol. 2008;15:400–6. doi: 10.1245/s10434-007-9725-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shanafelt TD. Enhancing meaning in work: a prescription for preventing physician burnout and promoting patient-centered care. Jama. 2009;302:1338–40. doi: 10.1001/jama.2009.1385. [DOI] [PubMed] [Google Scholar]
- 3.Kash KM, Holland JC, Breitbart W, Berenson S, Dougherty J, Ouellette-Kobasa S, Lesko L. Stress and burnout in oncology. Oncology (Williston Park) 2000;14:1621–33. discussion 1633–4, 1636–7. [PubMed] [Google Scholar]
- 4.Kuerer HM, Breslin T, Shanafelt TD, Baile WF, Crawford W, Balch CM. Road map for maintaining career satisfaction and balance in surgical oncology. J Am Coll Surg. 2008;207:435–42. doi: 10.1016/j.jamcollsurg.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 5.Kearney MKWR, Vachon ML, et al. Self-care of Physicians Caring for Patients at the End of Life: "Being Connected . . A Key to my Survival". JAMA. 2009;301:1155–1164. doi: 10.1001/jama.2009.352. [DOI] [PubMed] [Google Scholar]
- 6.Arndt J, Cook A, Goldenberg JL, Cox CR. Cancer and the threat of death: the cognitive dynamics of death-thought suppression and its impact on behavioral health intentions. J Pers Soc Psychol. 2007;92:12–29. doi: 10.1037/0022-3514.92.1.12. [DOI] [PubMed] [Google Scholar]
- 7.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–49. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 8.Ramondetta LM, Brown A, Richardson G, Urbauer D, Thaker PH, Koenig HG, Gano JB, Sun C. Religious and Spiritual Beliefs of Gynecologic Oncologists May Influence Medical Decision Making. Int J of Gynecol Cancer. 2011;21:573–581. doi: 10.1097/IGC.0b013e31820ba507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoge DR. A Validated intrinsic religious motivation scale. J for Sci Study of Religion. 1972;11:369–376. [Google Scholar]
- 10.Koenig HG, Cohen HJ, George LK, Hays JC, Larson DB, Blazer DG. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med. 1997;27:233–50. doi: 10.2190/40NF-Q9Y2-0GG7-4WH6. [DOI] [PubMed] [Google Scholar]
- 11.Levenson H. Differentiating among internality, powerful others, and chance. In: Lefcourt H, editor. Research with the Locus of Control Construct. New York: Academic Press; 1981. pp. 15–63. [Google Scholar]
- 12.Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966;80:1–28. [PubMed] [Google Scholar]
- 13.Sapp SG, Harrod WJ. Reliability and validity of a brief version of Levenson's locus of control scale. Psychol Rep. 1993;72:539–550. [Google Scholar]
- 14.Robinson P, Wood K. Fear of death and physical illness: a personal construct approach. Washington: Hempshire Publishing Company; 1984. [DOI] [PubMed] [Google Scholar]
- 15.Revicki DA, May HJ, Whitley TW. Reliability and validity of the Work-Related Strain Inventory among health professionals. Behav Med. 1991;17:111–20. doi: 10.1080/08964289.1991.9937554. [DOI] [PubMed] [Google Scholar]
- 16.Zar J. Biostatistical Analysis. 4. Prentice Hall; 1999. [Google Scholar]
- 17.Ramondetta LM, Sills D. Spirituality in gynecological oncology: a review. Int J Gynecol Cancer. 2004;14:183–201. doi: 10.1111/j.1048-891X.2004.014233.x. [DOI] [PubMed] [Google Scholar]
- 18.Ramirez A, Graham J, Richards M, et al. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347:724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 19.Peisah C, Latil E, Wilhelm K, Williams B. Secrets to psychological success: Why older doctors might have lower psychological distress and burnout than younger doctors. Aging & Mental Health. 2009;13:300–307. doi: 10.1080/13607860802459831. [DOI] [PubMed] [Google Scholar]
- 20.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–82. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 21.Frankl V. Man's search for meaning: An introduction to logotherapy. Beacon Press; 2006. [Google Scholar]
- 22.Kurland G. My own medicine: a doctor's life as a patient. New York: Times Books; 2002. [Google Scholar]
- 23.Ramondetta L, Sills D. The light within: The extraordinary friendship of a doctor and patient brought together by cancer. New York: William Morrow; 2008. p. 250. [Google Scholar]
- 24.Harmon-Jones E, Simon L, Greenberg J, Pszczynski T, Solomon S, McGregor H. Terror management theory and self-esteem: evidence that increased self-esteem reduces mortality salience effects. J Pers Soc Psychol. 1997;72:24–36. doi: 10.1037//0022-3514.72.1.24. [DOI] [PubMed] [Google Scholar]
- 25.Camps C, Escobar Y, Esteban E, Almenarez J, Moreno J, Galvez Herrer M, Arranz P, Sanchez P. Professional burnout among Spanish medical oncologists. Clin Transl Oncol. 2009;11:86–90. doi: 10.1007/s12094-009-0319-9. [DOI] [PubMed] [Google Scholar]
- 26.Libert Y, Janne P, Razavi D, Merckaert I, Scalliet P, Delvaux N, Etienne AM, Conradt S, Klastersky J, Boniver J, Reynaert C. Impact of medical specialists' locus of control on communication skills in oncological interviews. British Journal of Cancer. 2003;88:502–9. doi: 10.1038/sj.bjc.6600797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Penderell A, Brazil K. The spirit of palliative practice: A qualitative inquiry into the spiritual journey of palliative care physicians. Palliative and Supportive Care. 2010;8:415–420. doi: 10.1017/S1478951510000271. [DOI] [PubMed] [Google Scholar]
- 28.Wang P, Gao F. Mindful communication to address burnout, empathy, and attitudes. JAMA. 2010;303:330–331. doi: 10.1001/jama.2010.17. [DOI] [PubMed] [Google Scholar]
- 29.SGO, Society of Gynecologic Oncologists. State of the Subspecialty Survey. 2010. Gynecologic Oncology 2010; pp. 1–96. [Google Scholar]