Abstract
Background:
According to the American Association of Periodontology, subepithelial connective tissue graft (SCTG) is one the most reliable surgical technique available for the treatment of gingival recession (GR) with Miller's Class I defect. However, due to its various disadvantages, alternate grafts such as acellular dermal matrix (ADM) grafts have been introduced for recession coverage. The present study compares the clinical outcome of these two grafts in treating Miller's Class I GR.
Materials and Methods:
All the 15 patients participated in the study who had totally 30 bilateral Miller's Class I GR were divided randomly into SCTG group and ADM group each containing 15 defects. In the SCTG group, coronally advanced flap (CAF) with SCTG was performed, and in ADM group, CAF with ADM was done. Clinical parameters were measured on the day of surgery (baseline) and after 6 months. Data collected were statistically analyzed using paired and unpaired t-tests.
Results:
The analysis of the data collected at the baseline and 6 months later showed that there were no statistically significant differences in the recorded clinical parameters such as probing pocket depth, clinical attachment loss, and GR depth. ADM group showed a better color match than the SCTG group, while SCTG group achieved more keratinized tissue width than ADM group.
Conclusion:
From the outcome of the current study, we can conclude that ADM is an efficient substitute for SCTG for treating Miller's Class I GR. However, additional studies with greater number of samples and lengthier follow-up periods are necessary to validate the present inference.
Keywords: Acellular dermal matrix, acellular dermal transplant tissue, decellularized dermal scaffold, gingival recession, subepithelial connective tissue graft
INTRODUCTION
Gingival recession (GR) can be defined “as the migration of the gingiva to a point apical to the cemento-enamel junction (CEJ).”[1] The prevention of formation of root caries and noncaries cervical lesions along with tooth hypersensitivity and esthetic concern are the crucial reasons to deem surgical options for the treatment of GR.[2,3] An array of surgical methods have been offered over the years for GR coverage; among them, coronally advanced flap (CAF) with subepithelial connective tissue graft (SCTG) is considered as the gold standard because of its high predictability.[3,4,5,6] Regrettably, SCTG-based techniques come with its own constraints like a second surgical site leading to the postoperative discomfort.[7,8] Hence, an intense search for an alternate material which can successfully replace SCTG began. Acellular dermal matrix (ADM) graft is one such material, which was originally introduced in medicine to handle the third-degree burns.[9] ADM has been tried as an alternate graft material for SCTG to treat GR.[10,11] Even though a recent systematic analysis by Gallagher and Matthews on ADM and SCTG for recession coverage has concluded that both the treatment modalities have no clinical difference, the evidence was weak-to-moderate only.[12] Another recent systematic review from the Cochrane Database of Systematic Reviews by Chambrone et al. have also came to the same conclusion about ADM as an alternative to SCTG with weak evidence.[6] Even when esthetic concern is one of the major complications of GR, only a very few studies have compared the esthetic outcome between ADM and SCTG procedures.[13,14] Hence, the objective of the current study was to clinically evaluate the functional and esthetic efficacy of ADM over SCTG in treating Miller's Class I recession.
MATERIALS AND METHODS
Study population
The study was organized from 2013 to 2016 in the department of periodontics and was approved by the ethical committee of the institute. The present study was a randomized split-mouth clinical study which comprised 15 systemically healthy patients (8 males and 7 females) with an age range of 23–42 years (mean ± standard deviation: 29.67 ± 3.26 years) who had thirty Miller's Class I recession bilaterally. Among these thirty GRs, 15 were chosen randomly by a coin toss and allocated as the test group and the contralateral sides were assigned to the control group. If multiple recessions were treated, only the tooth with most recession depth was measured. The inclusion criteria were (1) patients with age range 18–50 years having bilateral Miller's Class I recession,[15] (2) identifiable CEJ, (3) nonsmokers, (4) no medical contraindications for periodontal surgery, and (5) not under any medication known to interfere with periodontal health or healing. The exclusion criteria were (1) other classes of Miller's recession, (2) recession defects combined with caries/restorations or noncaries cervical lesion, and (3) teeth with pulp pathology. Radiographs were taken to evaluate the interdental bone level.
Presurgical procedures
Phase I therapy consisting of a thorough scaling and root planning was completed first. Custom-made acrylic stents were constructed to make sure that probe position and angulations were reproducible.[16] Periodontal health of the participants in the study was monitored by the recording plaque index (PI),[17] gingival index (GI),[18] and retention index (RI)[19] throughout the study.
Recording of periodontal parameters
Gingival recession depth (GRD), probing pocket depth (PPD), clinical attachment level (CAL), and apicocoronal width of keratinized tissue (KTW) were measured at the baseline at the day of the surgery and 6 months after the surgery using the University of North Carolina (UNC) 15 probe and acrylic stent. Color matching (CM) with adjacent tissue was recorded using the Visual Analog Scale which was scored from 0 to 10 where 0 means poor CM and 10 represents the excellent CM.[20] All the values at the baseline and after 6 months were recorded by the same examiner who was blinded from the surgical procedure.
Surgical procedures
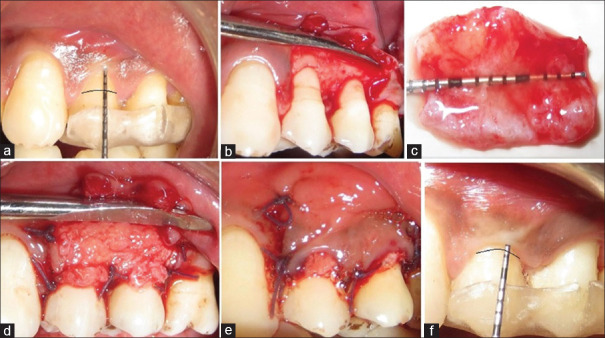
All the surgical procedures were performed by the same periodontal surgeon. Fifteen patients with 30 bilateral recessions who participated in the study were divided randomly by a coin toss into ADM group and SCTG group, each group containing 15 defects. In the SCTG group, CAF with SCTG was performed, and in ADM group, CAF with ADM was done. The surgical steps followed in both the groups were same for the recipient site. At the recipient site, the tooth with GR was anesthetized using local anesthesia and an intrasulcular incision was placed on the facial aspect till the proximal CEJ. At the level of the proximal CEJ, two horizontal incisions were placed in such a way that the gingival papillae of the adjacent teeth were not disturbed. From this point, two vertical incisions, slightly divergent, were placed which extended beyond the mucogingival junction (MGJ) [Figure 1]. Up to the MGJ, a full-thickness mucoperiosteal flap was reflected using a periosteal elevator. Beyond the MGJ, a split-thickness flap was extended using a no. 15 b Bard Parker (BP) blade which releases the tension and facilitates the coronal advancement of the reflected flap. The epithelium on the adjacent papillae was de-epithelialized.
Figure 1.

Intrasulcular incision was placed on the buccal surface with two horizontal incisions at the level of the cementoenamel junction without involving the adjacent teeth gingival papilla and two slightly divergent vertical incisions on either side of the involved tooth
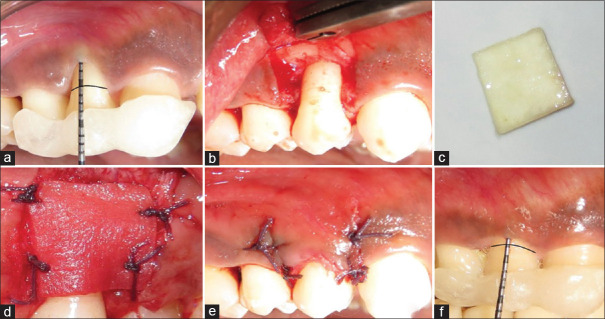
The exposed root surfaces were planed and flattened if convexities were present. Root conditioning with 24% ethylenediaminetetraacetic acid for 3 min was done followed by abundant saline irrigation. In the SCTG group, the SCTGs harvested from the palate were placed in the prepared recipient site and held in a position with 4-0 polyglactin 910 sutures [Figure 2]. In the ADM group, ADM was trimmed with respect to the recipient site and rehydrated according to the manufacturer's recommendation and stabilized in the recession site with the above-mentioned suture material [Figure 3]. Fully rehydrated ADM has two distinctive sides, a basement membrane side and connective tissue side. The basement membrane side is rough and does not absorb blood and the connective tissue side is smooth and readily absorbs blood. Identifying the sides are important because the material becomes more predictable if the basement membrane side is placed toward the flap and the connective tissue side is placed toward the root surface.[13] In both the cases, the previously reflected flap was coronally advanced to cover the entire GR and the secured graft without any tension and the sutures were placed to secure the flap.
Figure 2.
Subepithelial connective tissue graft group. (a) Preoperative view Miller's Class I recession on teeth #12 and #13. (b) Flap is reflected. (c) Harvested connective tissue. (d) The connective tissue was trimmed to the shape of the recipient site and sutured in place. (e) The overlying flap was placed coronally to cover the graft and sutured. (f) 6-month postoperative view of the treated site
Figure 3.
Acellular dermal matrix group. (a) Preoperative view Miller's Class I recession on tooth #5. (b) Flap is reflected. (c) Acellular dermal matrix graft after rehydration. (d) Acellular dermal matrix graft is trimmed to the shape of the recipient bed and secured with sutures in place. (e) The overlying flap was coronally placed and sutured to cover the graft completely. (f) 6-month postoperative view of the treated site
Postsurgical care
The noneugenol dressing was used to protect the surgical area. Standard postoperative instructions and medications were given. The patients were recalled every month for maintenance therapy, and after 6 months, all the above-mentioned periodontal parameters were rerecorded and evaluated with the baseline parameters.
Statistical analysis
The recorded parameters were statistically analyzed using paired t-test to compare intragroup P values and unpaired t-test to compare intergroup P values. P < 0.05 was considered statistically significant.
RESULTS
All the 15 patients who participated in the current study completed the study and none of the cases reported any adverse reaction. No statistically significant difference was found in the mean values of PI, GI, and RI which were recorded at the baseline and 6 months later in both the groups. This shows that the periodontal health of both the groups (SCTG group and ADM group) was similar at the baseline and was maintained throughout the study [Table 1]. There was no difference in all the clinical parameters (GRD, KTW, PPD, and CAL) that were measured at the baseline in both the groups because the defects in both the groups were similar sized. After 6 months, both the groups showed a significant reduction in the GRD and PPD and increase in the CAL and KTW [Table 2]. The intergroup data which were collected after 6 months were statistically analyzed, which showed that there was no statistically significant difference in the reduction of GRD and PPD and increase in CAL [Table 3]. The SCTG group showed a significant increase in the KTW when compared with that of the ADM group. On the other hand, the ADM group obtained a better CM with the adjacent gingival tissue than the SCTG group [Table 4].
Table 1.
Mean values±standard deviation of plaque index, gingival index, and retention index at the baseline and 6-month follow-up
| Plaque index | Gingival index | Retention index | ||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | Baseline | 6 months | Baseline | 6 months | |
| Mean±SD | 0.50±0.03 | 0.50±0.04 | 0.38±0.03 | 0.37±0.05 | 0.49±0.03 | 0.49±0.04 |
| P | 0.5 (NS) | 0.4 (NS) | 0.44 (NS) | |||
P<0.05 was considered as statistically significant. NS – No significant difference; SD – Standard deviation; P – Probability value
Table 2.
Mean values±standard deviation of clinical parameters at the baseline and 6-month follow-up
| Parameter | Subepithelial connective tissue graft | Acellular dermal matrix | Between-group difference† (P) | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline (mm) | 6 months (mm) | Difference* (P) | Baseline (mm) | 6 months (mm) | Difference* (P) | Baseline | 6 months | |
| GRD | 2.36±0.15 | 0.73±0.14 | S (0.0001) | 2.54±0.20 | 1.27±0.19 | S (0.00001) | NS (0.24) | NS (0.21) |
| KTW | 3.63±0.24 | 5.10±0.25 | S (0.0001) | 4.10±0.31 | 5.00±0.30 | S (0.00001) | NS (0.13) | S (0.002) |
| PPD | 2.00±0.23 | 1.36±0.15 | S (0.016) | 2.27±0.14 | 1.36±0.15 | S (0.0001) | NS (0.16) | NS (0.57) |
| CAL | 4.54±0.28 | 2.00±0.63 | S (0.00001) | 4.82±0.26 | 2.54±0.28 | S (0.00001) | NS (0.24) | NS (0.57) |
*Intragroup analysis – paired t-test, †Between-group analysis – Unpaired t-test. P<0.05 was considered as statistically significant. GRD – Gingival recession depth; KTW – Width of keratinized tissue; PPD – Probing pocket depth; CAL – Clinical attachment level; mm – Millimeter; S – Significant difference; NS – No significant difference; P – Probability value
Table 3.
Mean changes±standard deviation of clinical parameters between the baseline and 6-month follow-up within the experimental groups
| Group | Parameter (mm) | |||
|---|---|---|---|---|
| GRD | KTW | PPD | CAL | |
| Subepithelial connective tissue graft | 1.64±0.80 | 1.45±0.52 | 0.64±1.02 | 2.55±1.37 |
| Acellular dermal matrix | 1.27±0.47 | 0.91±0.16 | 0.91±0.70 | 2.28±0.79 |
| Difference* (P) | NS (0.21) | S (0.002) | NS (0.57) | NS (0.57) |
P<0.05 was considered as statistically significant, *Between-group analysis – Unpaired t-test. GRD – Gingival recession depth; KTW – Width of keratinized tissue; PPD – Probing pocket depth; CAL – Clinical attachment level; mm – Millimeter; S – Significant difference; NS – No significant difference; P – Probability value
Table 4.
Mean values±standard deviation of visual analog scale at 6-month follow-up
| Group | VAS |
|---|---|
| Subepithelial connective tissue graft | 6.00±0.23 |
| Acellular dermal matrix | 6.91±0.21 |
| Difference* (P) | S (0.004) |
*Between-group analysis – Unpaired t-test, P<0.05 was considered as statistically significant. VAS – Visual Analog Scale; S – Significant difference; P – Probability value
DISCUSSION
In the current clinical study, the functional and esthetic results of ADM and SCTG which is contemplated as the gold standard in recession coverage procedure of Miller's Class I defects were evaluated.[4,6] ADM and SCTG groups were able to create a statistically significant progress in all the clinical parameters which were recorded 6 months later when compared with clinical parameters which were noted at the baseline. The mean values of the GI, PI, and RI between the groups showed no significant difference throughout the study which coincide with the observation by Paolantonio et al. and Moslemi et al.[21,22] The reason for this observation might be because of the fact that all the participating patients were kept on a strict recall maintenance therapy and the importance of following a proper home care was also reinforced in every visit throughout the study period.
Intergroup analysis after 6 months showed that there was no statistically significant difference in clinical parameters such as PPD and GRD reduction and increase in CAL. Earlier reports by Paolantonio et al. and others also stated similar findings.[21,23,24] SCTG group exhibited a substantial increase in the KTW when matched with that of the AMD group after 6 months. These findings concur well with the previous reports by Harris, Paolantonio et al., Tal et al., and Hirsch et al.[21,24,25,26]
In contrast to the present findings, Novaes et al. and Barros et al. demonstrated that ADM was superior to SCTG in increasing the KTW.[23,27] Both the studies mentioned above used Schiller's iodine solution to stain the gingival tissue to determine the KTW instead of visual observation using UNC 15 periodontal probe and acrylic stents like the current study. Interestingly, studies by Joly et al. and Schlee and Esposito who used the UNC 15 probe and visual inspection method, respectively, stated that there was no statistically substantial increase in the KTW, which can be explained by the fact that the former used a different surgical technique and the latter used a different ADM material.[14,28] Another study by Barros et al. found no significant difference between the ADM group and SCTG group in every clinical parameter that was recorded which may be because they used an extended flap technique instead of a conventional technique which was followed in the current study.[29] A recent meta-analysis by Gallagher and Matthews has reported that ADM has a small but statistically significant higher KTW when compared with SCTG. The difference reported was < 1 mm which was not significant clinically.[12]
An important goal of the current study was to explore the CM between the treated and adjacent nontreated parts of the gingiva in both the groups, as esthetic concern was a significant complication of GR which brings the patients to a dental clinic and only a handful of studies have investigated this condition previously.[12] Our observation showed that ADM gave a better color match than the SCTG which coincides with the previous observations.[13,14] This may be because of the fact that the ADM graft is a nonvital graft which only provides a scaffold for ingrowth of native cells from the recipient site while healing, whereas the SCTG graft is a vital graft with live palatal connective tissue cells which determines the local keratinization hence can affect the color match.[14]
Limitations
The main limitations of the current study were that the sample size was less and short follow-up period. Due to the ethical concern, histopathological examinations of the treated sites were not performed, which could have helped us to understand the healing of the ADM and explained about the better CM of sites treated with ADM over SCTG. Patient-centerd outcomes were not included in the study.
CONCLUSION
Keeping in mind about the limits of this study, we can conclude that important clinical parameters like recession coverage and gain in the CAL obtained by the ADM group were equivalent to that obtained by the SCTG group. However, SCTG was capable of achieving a significantly greater increase in KTW, while ADM was capable of achieving a better CM than SCTG. Considering the overall clinical outcome both functionally and esthetically, patient compliance, and operator's convenience, ADM may be a suitable substitute for the SCTG in treating of Miller's Class I recession. However, further studies with larger sample size, long-term follow-up, and histological examination of the healing of the graft are needed to confirm these findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.American Association of Periodontology, 2019. Glossary of Periodontal Terms. [Last accessed on 2019 Aug 08]. Available from: https://members.perio.org/libraries/glossary/entry?GlossaryKey=543e026d-993d-44c1-b183-3b746f410ebc and tab=groupdetails> .
- 2.Chan HL, Chun YH, MacEachern M, Oates TW. Does gingival recession require surgical treatment? Dent Clin North Am. 2015;59:981–96. doi: 10.1016/j.cden.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: A systematic review from the AAP regeneration workshop. J Periodontol. 2015;86:S8–51. doi: 10.1902/jop.2015.130674. [DOI] [PubMed] [Google Scholar]
- 4.Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of miller Class I and II recession-type defects? J Dent. 2008;36:659–71. doi: 10.1016/j.jdent.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 5.Buti J, Baccini M, Nieri M, La Marca M, Pini-Prato GP. Bayesian network meta-analysis of root coverage procedures: Ranking efficacy and identification of best treatment. J Clin Periodontol. 2013;40:372–86. doi: 10.1111/jcpe.12028. [DOI] [PubMed] [Google Scholar]
- 6.Chambrone L, Salinas Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, et al. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev. 2018;10:CD007161. doi: 10.1002/14651858.CD007161.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang HL, Bunyaratavej P, Labadle M, Shyr Y, MacNeil RL. Comparison of two clinical techniques for treatment of gingival recession. J Periodontol. 2001;72:1301–11. doi: 10.1902/jop.2001.72.10.1301. [DOI] [PubMed] [Google Scholar]
- 8.McGuire MK, Nunn M. Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue. Part 1: Comparison of clinical parameters. J Periodontol. 2003;74:1110–25. doi: 10.1902/jop.2003.74.8.1110. [DOI] [PubMed] [Google Scholar]
- 9.Wainwright DJ. Use of an acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. Burns. 1995;21:243–8. doi: 10.1016/0305-4179(95)93866-i. [DOI] [PubMed] [Google Scholar]
- 10.Harris RJ. Root coverage with a connective tissue with partial thickness double pedicle graft and an acellular dermal matrix graft: A clinical and histological evaluation of a case report. J Periodontol. 1998;69:1305–11. doi: 10.1902/jop.1998.69.11.1305. [DOI] [PubMed] [Google Scholar]
- 11.Tal H. Subgingival acellular dermal matrix allograft for the treatment of gingival recession: A case report. J Periodontol. 1999;70:1118–24. doi: 10.1902/jop.1999.70.9.1118. [DOI] [PubMed] [Google Scholar]
- 12.Gallagher SI, Matthews DC. Acellular dermal matrix and subepithelial connective tissue grafts for root coverage: A systematic review. J Indian Soc Periodontol. 2017;21:439–48. doi: 10.4103/jisp.jisp_222_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aichelmann-Reidy ME, Yukna RA, Evans GH, Nasr HF, Mayer ET. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. J Periodontol. 2001;72:998–1005. doi: 10.1902/jop.2001.72.8.998. [DOI] [PubMed] [Google Scholar]
- 14.Joly JC, Carvalho AM, da Silva RC, Ciotti DL, Cury PR. Root coverage in isolated gingival recessions using autograft versus allograft: A pilot study. J Periodontol. 2007;78:1017–22. doi: 10.1902/jop.2007.060428. [DOI] [PubMed] [Google Scholar]
- 15.Miller PD., Jr A classification of marginal tissue recession. Int J Periodontics Restor Dent. 1985;5:8–13. [PubMed] [Google Scholar]
- 16.Badersten A, Nilvéus R, Egelberg J. Reproducibility of probing attachment level measurements. J Clin Periodontol. 1984;11:475–85. doi: 10.1111/j.1600-051x.1984.tb01347.x. [DOI] [PubMed] [Google Scholar]
- 17.Silness J, Loe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 18.Loe H, Silness J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 19.Björby A, Löe H. The relative significance of different local factors in the initiation and development of periodontal inflammation. Scand. Symp. Periodontology 1966. 1967;1:70–81. Abstr. No. 20. J Periodontal Res. [Google Scholar]
- 20.Shanmugam M, Sivakumar V, Anitha V, Sivakumar B. Clinical evaluation of alloderm for root coverage and colour match. J Indian Soc Periodontol. 2012;16:218–23. doi: 10.4103/0972-124X.99265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paolantonio M, Dolci M, Esposito P, D’Archivio D, Lisanti L, Di Luccio A, et al. Subpedicle acellular dermal matrix graft and autogenous connective tissue graft in the treatment of gingival recessions: A comparative 1-year clinical study. J Periodontol. 2002;73:1299–307. doi: 10.1902/jop.2002.73.11.1299. [DOI] [PubMed] [Google Scholar]
- 22.Moslemi N, Mousavi Jazi M, Haghighati F, Morovati SP, Jamali R. Acellular dermal matrix allograft versus subepithelial connective tissue graft in treatment of gingival recessions: A 5-year randomized clinical study. J Clin Periodontol. 2011;38:1122–9. doi: 10.1111/j.1600-051X.2011.01789.x. [DOI] [PubMed] [Google Scholar]
- 23.Novaes AB, Jr, Grisi DC, Molina GO, Souza SL, Taba M, Jr, Grisi MF. Comparative 6-month clinical study of a subepithelial connective tissue graft and acellular dermal matrix graft for the treatment of gingival recession. J Periodontol. 2001;72:1477–84. doi: 10.1902/jop.2001.72.11.1477. [DOI] [PubMed] [Google Scholar]
- 24.Tal H, Moses O, Zohar R, Meir H, Nemcovsky C. Root coverage of advanced gingival recession: A comparative study between acellular dermal matrix allograft and subepithelial connective tissue grafts. J Periodontol. 2002;73:1405–11. doi: 10.1902/jop.2002.73.12.1405. [DOI] [PubMed] [Google Scholar]
- 25.Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: Results of 107 recession defects in 50 consecutively treated patients. Int J Periodontics Restor Dent. 2000;20:51–9. [PubMed] [Google Scholar]
- 26.Hirsch A, Goldstein M, Goultschin J, Boyan BD, Schwartz Z. A 2-year follow-up of root coverage using sub-pedicle acellular dermal matrix allografts and subepithelial connective tissue autografts. J Periodontol. 2005;76:1323–8. doi: 10.1902/jop.2005.76.8.1323. [DOI] [PubMed] [Google Scholar]
- 27.Barros RR, Novaes AB, Grisi MF, Souza SL, Taba MJ, Palioto DB. A 6-month comparative clinical study of a conventional and a new surgical approach for root coverage with acellular dermal matrix. J Periodontol. 2004;75:1350–6. doi: 10.1902/jop.2004.75.10.1350. [DOI] [PubMed] [Google Scholar]
- 28.Schlee M, Esposito M. Human dermis graft versus autogenous connective tissue grafts for thickening soft tissue and covering multiple gingival recessions: 6-month results from a preference clinical trial. Eur J Oral Implantol. 2011;4:119–25. [PubMed] [Google Scholar]
- 29.Barros RR, Macedo GO, de Queiroz AC, Novaes AB., Jr A modified surgical flap for root coverage in association with grafting materials. J Esthet Restor Dent. 2015;27:84–91. doi: 10.1111/jerd.12122. [DOI] [PubMed] [Google Scholar]