Seven coronaviruses (CoVs) have been identified in the etiology of human infections, among which, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), SARS-CoV, and Middle East respiratory syndrome coronavirus (MERS-CoV) are highly pathogenic human coronaviruses (HPH-CoVs), whereas HCoV-229E, HCoV-OC43, HCoV-NL63, and HCoV-HKU1 belong to low pathogenic human coronaviruses (LPH-CoVs). SARS-CoV, MERS-CoV, and SARS-CoV-2 were first zoonotically transmitted to humans in 2002, 2012, and 2019, respectively, and are known to cause significant lower respiratory syndrome and severe pneumonia in humans [1]. Compared with MERS-CoV, SARS-CoV-2 is more closely related to SARS-CoV, since they both recognize angiotensin-converting enzyme 2 (ACE2) as the receptor for viral entry into the host cells [1]. Different from HPH-CoVs, the LPH-CoVs, including HCoV-229E, HCoV-OC43, HCoV-NL63, and HCoV-HKU1, exhibit a worldwide distribution, causing common cold in humans with mild upper respiratory tract infections [1].
Recently (in this issue), Ma et al. pointed out that LPH-CoV-specific antibodies (Abs) with crossreactivity against SARS-CoV-2 may have a more important impact on the global COVID-19 pandemic than HPH-CoV-specific Abs through the greater number of individuals with previous LPH-CoV infection [2]. Thus, they argue for the necessity of investigating the potential effect of LPH-CoV-specific Abs in humans on SARS-CoV-2 infection. We agree, since such study may, indeed, provide guidelines for the rational use of intravenous immunoglobulin (IVIG) and COVID-19 convalescent sera for treatment of SARS-CoV-2 infection.
HPH-CoV-Specific Abs with Crossreactivity against SARS-CoV-2
Abs against SARS-CoV have been identified with crossreactivity against SARS-CoV-2. These Abs can recognize the receptor-binding domain (RBD) in the S1 subunit of spike (S) protein of SARS-CoV-2. For example, monoclonal antibodies (mAbs), such as 18F3, 7B11, S309, and 47D11, recognize epitopes on the RBD of SARS-CoV-2 and neutralize SARS-CoV-2 infection; other mAbs, including S303, crossreact with SARS-CoV-2 RBD, but they do not neutralize its infectivity [3., 4., 5.]. A few SARS-CoV S2-specific Abs, such as mAb 1A9, have even demonstrated crossreactivity with SARS-CoV-2 [6]. However, we still need to address a clinically vital question, that is, whether SARS-CoV-specific Abs can enhance SARS-CoV-2 infection. At this time, no crossreactivity between Abs against SARS-CoV-2 and MERS-CoV has been identified, partially because of low sequence homology between their S proteins and different receptors that they recognize.
LPH-CoV-Specific Abs with Crossreactivity against SARS-CoV-2
Pre-existing Abs to LPH-CoVs with crossreactivity against SARS-CoV-2 proteins have been identified [7,8]. Patient serum IgG Abs against LPH-CoV S proteins, particularly the conserved S2 subunit, are crossreactive with SARS-CoV-2, but those targeting the S1 subunit, particularly the RBD, are mostly strain-specific with less crossreactivity against SARS-CoV-2 [8]. Still, while LPH-CoV-specific Abs with crossreactivity against SARS-CoV-2 may have beneficial effects (e.g., neutralizing SARS-CoV-2 infection), we again raise the key question of whether they might also have harmful effects (e.g., enhancing SARS-CoV-2 infection).
Potential Benefits of Pre-existing LPH-CoV-Specific Abs on SARS-CoV-2 Infection
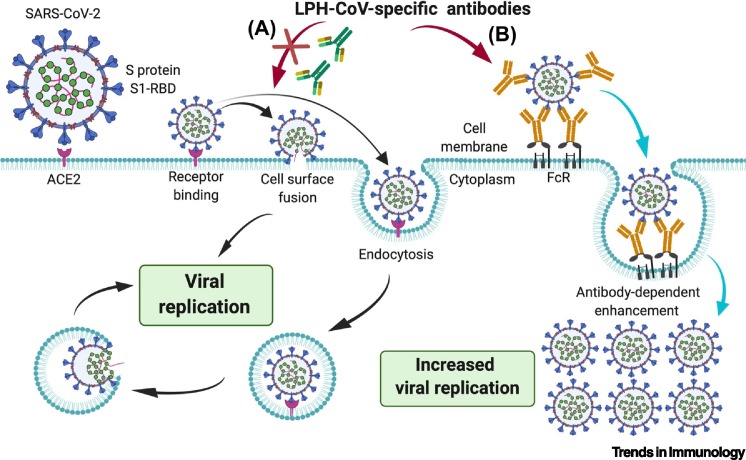
As mentioned earlier, the pre-existing LPH-CoV-specific Abs with crossreactivity against SARS-CoV-2 could effectively crossneutralize SARS-CoV-2 infection [8]. It appears that most of these LPH-CoV-specific Abs do not bind to the S1-RBD in SARS-CoV-2 S protein [8], which is responsible for binding of virions with the ACE2 receptor on the host cells [1]; instead, they mainly interact with the SARS-CoV-2 S2 region [8], which mediates the fusion between virions and target cell membranes (Figure 1 ) [9]. Therefore, future studies should investigate the underlying mechanism(s) by which LPH-CoV-specific Abs crossneutralize SARS-CoV-2 infection.
Figure 1.
Potential Effects of Low Pathogenic Human Coronavirus (LPH-CoV)-Specific Antibodies (Abs) on Infectivity of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).
SARS-CoV-2 first binds to a cellular receptor, such as angiotensin-converting enzyme 2 (ACE2), on the target cells through its receptor-binding domain (RBD) in the S1 subunit of the spike (S) protein, which triggers the conformational change of the S2 subunit, resulting in virus–cell membrane fusion and viral entry into to the target cells for replication. (A) LPH-CoV-specific Abs may bind to S1 (in some cases) or S2 of SARS-CoV-2 S protein to block receptor binding or inhibit membrane fusion and entry into the target cells. (B) LPH-CoV-specific Abs with no, or low-titer, neutralizing activity against SARS-CoV-2 may also enter the host cells by binding to Fc receptor (FcR) on the cell membrane, resulting in antibody-dependent enhancement (ADE) effect on SARS-CoV-2 infection. This figure was created using BioRender (https://biorender.com/).
Potential Harmful Effects of Pre-existing LPH-CoV-Specific Abs on SARS-CoV-2 Infection
CoV nonneutralizing Abs, or even some neutralizing Abs at low neutralizing titers, may cause harmful effects. For example, some SARS-CoV S-specific neutralizing Abs could enhance SARS-CoV infection in an Fc receptor (FcR)-dependent, ACE2-independent manner [10]. Indeed, co-infection of SARS-CoV-2 and LPH-CoVs, such as HCoV-HKU1, were found in some patients positive for SARS-CoV-2 [7]. Such a phenomenon calls for efforts to establish if LPH-CoV-specific Abs with low, or no, neutralizing activity can actually cause an antibody-dependent enhancement (ADE) effect, in which Abs may enhance, rather than neutralize, SARS-CoV-2 infection, or other mechanisms (Figure 1).
Overall, in addition to Abs specific for highly pathogenic SARS-CoV with crossreactivity or crossneutralizing activity against SARS-CoV-2, LPH-CoV-specific Abs may also have neutralizing effects on SARS-CoV-2 infection. Of relevance, however, they might enhance infectivity. In such cases, clarification of their effects is essential before attempting to design any Ab-based therapy against SARS-CoV-2, such as IVIG or COVID-19 convalescent sera, for clinical use in the treatment of COVID-19 [11,12]. Put simply, on the one hand, if pre-existing Abs in healthy individuals previously infected with an LPH-CoV (e.g., HCoV-OC43, HCoV-229E, HCoV-NL63, or HCoV-HKU1) exhibit potent crossneutralizing activity against SARS-CoV-2, then their sera or plasma may be collected for treatment of COVID-19 patients. On the other hand, if these Abs show an ADE effect, then the IVIG and COVID-19 convalescent sera containing these Abs should obviously be excluded from clinical use in treating SARS-CoV-2 infection. Therefore, testing LPH-CoV-specific Abs with ADE effects on SARS-CoV-2 infection in the IVIG and COVID-19 convalescent sera would establish a crucial benchmark before their use is allowed in clinics.
Acknowledgments
This study was supported by National Institutes of Health (NIH) grants R01AI157975, R01AI137472, and R01AI139092.
References
- 1.Wang N. Subunit vaccines against emerging pathogenic human coronaviruses. Front. Microbiol. 2020;11:298. doi: 10.3389/fmicb.2020.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma Z. Does cross-neutralization of SARS-CoV-2 only relate to high pathogenic coronaviruses. Trends Immunol. 2020;41 doi: 10.1016/j.it.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tai W. Identification of SARS-CoV RBD-targeting monoclonal antibodies with cross-reactive or neutralizing activity against SARS-CoV-2. Antivir. Res. 2020;179:104820. doi: 10.1016/j.antiviral.2020.104820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinto D. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature. 2020;583:290–295. doi: 10.1038/s41586-020-2349-y. [DOI] [PubMed] [Google Scholar]
- 5.Wang C. A human monoclonal antibody blocking SARS-CoV-2 infection. Nat. Commun. 2020;11:2251. doi: 10.1038/s41467-020-16256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng Z. Monoclonal antibodies for the S2 subunit of spike of SARS-CoV cross-react with the newly-emerged SARS-CoV-2. Euro Surveill. 2020;25:2000291. doi: 10.2807/1560-7917.ES.2020.25.28.2000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin D. Co-infections of SARS-CoV-2 with multiple common respiratory pathogens in infected patients. Sci. China Life Sci. 2020;63:606–609. doi: 10.1007/s11427-020-1668-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng K. Pre-existing and de novo humoral immunity to SARS-CoV-2 in humans. bioRxiv. 2020 doi: 10.1101/2020.05.14.095414. Published online May 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xia S. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res. 2020;30:343–355. doi: 10.1038/s41422-020-0305-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jaume M. SARS CoV subunit vaccine: antibody-mediated neutralisation and enhancement. Hong Kong Med. J. 2012;18:31–36. [PubMed] [Google Scholar]
- 11.Xie Y. Effect of regular intravenous immunoglobulin therapy on prognosis of severe pneumonia in patients with COVID-19. J. Infect. 2020;81:318–356. doi: 10.1016/j.jinf.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casadevall A., Pirofski L.A. The convalescent sera option for containing COVID-19. J. Clin. Invest. 2020;130:1545–1548. doi: 10.1172/JCI138003. [DOI] [PMC free article] [PubMed] [Google Scholar]