Heart failure (HF) is a leading cause of morbidity, mortality, and use of health care resources. The coronavirus-2019 (COVID-19) pandemic presents novel challenges at the patient level as dyspnea is a cardinal symptom of both conditions. The unprecedented challenges to health care systems have led to implementation of rapid ambulatory telehealth services. The consequences of COVID-19 and associated public health regulatory changes may adversely impact patients with HF due to patient avoidance of medical care (1). The secondary impact of the COVID-19 lockdown on the incidence and acuity of HF hospitalizations has not been studied.
We sought to compare the number of HF hospitalizations, patient characteristics on presentation, and key HF quality metrics across the COVID-19 and non-COVID-19 eras. Key metrics assessed included inpatient mortality, length of stay, and use of guideline-directed medical therapy. Cases were identified after comprehensive review of records of all patients hospitalized under the cardiology and internal medicine teams. HF in the COVID-19 era has been defined as the first 30-day period from the beginning of lockdown in Australia (March 16, 2020 to April 14, 2020). This period coincided with the peak of the COVID-19 epidemic curve in Australia. These data were compared to historic data at our hospital from the VCOR-HF (Victorian Cardiac Outcomes Registry-HF), which was collected prospectively over a 30-day period each year from 2014 to 2017. The methodology and results of the VCOR-HF project were described previously (2). This registry was coordinated by the independent Center of Cardiovascular Research and Education in Therapeutics at Monash University (Clayton, Victoria, Australia) with periodic quality control audits that demonstrated a data accuracy of 97% (2). Data from 2018 to 2019 had not been collated by the registry at the time of the study and was excluded. Data were collected at Austin Health, a major quaternary hospital with a catchment population of 1.14 million people.
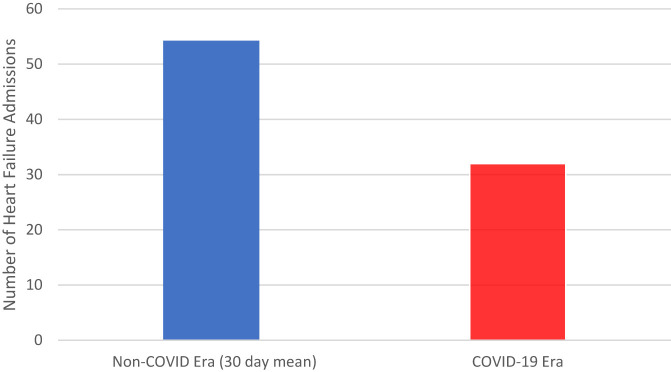
Overall, 249 patients were included in the study analysis. There were 32 HF hospitalizations in the COVID-19 era, which represents a 41% reduction from our historical monthly mean of 54 hospitalizations (range, 44% to 74%; p < 0.001) (Figure 1 ). Baseline clinical characteristics and burden of chronic disease were similar across the COVID-19 and non-COVID era. The proportion of patients with HF diagnosis with reduced ejection fraction did not vary. Infection remained the most common precipitant for acute HF in both the COVID and non-COVID eras (Table 1 ). Of note, 31% of HF hospitalizations in the COVID era were managed initially in a COVID-19 medical unit due to a high index of suspicion for infection with severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). Among these patients, there were no confirmed cases of SARS-CoV-2.
Figure 1.
Heart Failure Hospitalizations in the COVID-19 Era Compared to a 30-Day Mean Sampled From 2013 to 2017
Data show the number of heart failure hospitalizations in the COVID-19 era (March 16, 2020 to April 14, 2020) compared to a historical 30-day mean sampled from 2013 to 2017.
Table 1.
Baseline Characteristics, Presentation Details, and Clinical Outcomes
| Overall (N = 249) | COVID-19 Era (n = 32) | Non-COVID-19 Era (n = 217) | p Value | |
|---|---|---|---|---|
| Age, yrs | 79.9 ± 11 | 80.2 ± 14 | 79.8 ± 11 | 0.85 |
| Males | 217 (50) | 14 (44) | 113 (52) | 0.18 |
| Charlson comorbidity index | 7.5 ± 2.2 | 7.7 ± 1.7 | 7.5 ± 2.0 | 0.52 |
| Diabetes | 115 (46) | 18 (56) | 97 (45) | 0.70 |
| Hypertension | 197 (79) | 23 (72) | 174 (80) | 0.28 |
| Stroke | 55 (22) | 5 (16) | 50 (23) | 0.39 |
| CIED | 50 (20) | 8 (25) | 42 (19) | 0.45 |
| Chronic kidney disease | 172 (69) | 18 (56) | 154 (71) | 0.09 |
| Dementia | 26 (10) | 2 (6.3) | 24 (11) | 0.35 |
| Active malignancy | 23 (9.2) | 4 (13) | 19 (9.0) | 0.18 |
| COPD | 76 (31) | 5 (16) | 71 (33) | 0.05 |
| Cause of heart failure | ||||
| Ischemia | 68 (27) | 9 (28) | 59 (27) | 0.88 |
| Hypertension | 24 (9.5) | 4 (13.0) | 19 (8.8) | 0.37 |
| Valvular heart disease | 16 (6.5) | 2 (6.5) | 11 (5.1) | 0.69 |
| Ejection fraction, % | 0.25 | |||
| ≥50 | 113 (45.0) | 16 (51.0) | 96 (44.2) | |
| 45-49 | 28 (11.0) | 2 (6.3) | 28 (12.0) | |
| 35-44 | 52 (21) | 5 (16) | 48 (22) | |
| ≤35 | 56 (23) | 9 (29) | 45 (21) | |
| Presentation characteristics | ||||
| Systolic BP, mm Hg | 137 ± 26 | 144 ± 29 | 136 ± 26 | 0.06 |
| Diastolic BP, mm Hg | 75 ± 15 | 77 ± 12 | 74 ± 16 | 0.26 |
| Admission under cardiology | 80 (32) | 7 (22) | 75 (34) | 0.09 |
| NYHA functional class on admission | 0.009 | |||
| II | 71 (29) | 1 (3) | 70 (32) | |
| III | 120 (48) | 21 (66) | 99 (46) | |
| IV | 58 (23) | 10 (31) | 48 (22) | |
| III/IV | 178 (71) | 31 (97) | 147(68) | 0.01 |
| Precipitant for decompensation | ||||
| Ischemia | 26 (10.0) | 2 (6.5) | 24 (11.0) | 0.36 |
| Medication nonadherence | 20 (8.0) | 6 (18.0) | 14 (6.4) | 0.04 |
| Infection | 84 (34) | 8 (25) | 78 (36) | 0.22 |
| Arrhythmia | 54 (22) | 5 (15) | 50 (23) | 0.24 |
| Unknown/other | 65 (26) | 11 (34) | 51 (24) | 0.35 |
| Admissions | 0.01∗ | |||
| 2014 | 45 | - | - | |
| 2015 | 44 | - | - | |
| 2016 | 74 | - | - | |
| 2017 | 54 | - | - | |
| 2020 (COVID-19) | 32 | - | - | |
| Quality metrics | ||||
| Length of stay | 5.5 (3–9) | 4.0 (3–8) | 6.0 (3–10) | 0.16 |
| % of inpatient weight loss | 3.3 ± 5.2 | 2.9 ± 5.5 | 3.4 ± 5.1 | 0.66 |
| In-hospital mortality | 16 (6.4) | 3 (9.4) | 13 (5.9) | 0.47 |
| ICU admission | 16 (6.4) | 3 (9.0) | 13 (6.0) | 0.47 |
| ICU length of stay, days | 3.9 ± 2 | 5.3 ± 4 | 3.6 ± 2 | 0.32 |
| Non-invasive ventilation | 46 (18.0) | 1 (3.1) | 45 (21.0) | 0.02 |
| Discharge to Home | 202 (81) | 25 (78) | 178 (82) | 0.86 |
| Discharge medications | ||||
| ACE inhibitor/ARB | 136 (55) | 10 (35) | 124 (57) | 0.033 |
| Beta-blockers | 170 (68) | 25 (79) | 145 (67) | 0.20 |
| MRA | 86 (35) | 11 (36) | 74 (34) | 0.88 |
Values are mean ± SD, n (%), or mean (interquartile range). Ejection fraction was measured using the Simpson biplane method. Chronic kidney disease was defined as baseline eGFR <60 ml/min/1.73 m2.
ACEI = angiotensin-converting enzyme; ARB = angiotensin receptor blocker; CIED = cardiac implantable-electronic device; COPD = chronic obstructive pulmonary disease; COVID = corona virus; eGFR = estimated glomerular filtration rate; ICU = intensive care unit; MRA = mineralocorticoid agonist; NYHA = New York Heart Association.
The p value for the average number of admissions in the non-COVID-19 era were compared to those in the COVID-19 era.
Patients admitted during the COVID-19 era were significantly more symptomatic on presentation and there was a higher proportion with New York Heart Association (NYHA) functional class III/IV symptoms (96.9%/71.0%, respectively; p = 0.001). No major differences in HF quality metrics, including intensive care admission or in-hospital mortality, were recorded (Table 1). Length of hospital stay was numerically lower in the COVID-19 era, although this was not statistically significant (median, 4.0 vs. 6.0 days, respectively; p = 0.16). With regard to goal-directed medical therapy, prescription rates of beta-blockers and mineralocorticoid receptor antagonists were similar across the eras. However, there was a significant reduction in the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARB) in the COVID-19 era (35.7% vs 57.1%, respectively; p = 0.03).
In this study, evaluating early data for acute HF hospitalizations during the COVID-19 era, 3 key findings merit attention. First, there was a 41% reduction in hospitalizations due to HF. Second, patients hospitalized during the COVID-19 era had significantly higher NYHA functional classification. Third, despite comparable clinical characteristics of the patients across the eras, there was a significant reduction in the prescription of ACE inhibitors/ARBs in the COVID era.
Although some anecdotal reports have indicated a reduction in acute HF presentations, no data to date have been presented to support this notion. The significant reduction in HF hospitalizations in this study mirrors observations in the presentation of patients with ST-segment elevation myocardial infarction (3). The exact reasons for this remain unclear, but the following are possible explanations. Self-isolation and social distancing may have lowered the overall rate of respiratory infections that are known to be common triggers for clinical decompensation. Additionally, improved patient vigilance with both medication and dietary adherence may also have played a role. These factors coupled with patients’ reticence in seeking medical care due to perceptions of contracting COVID-19 in the hospital environment might have lowered HF presentation rates (1).
The Australian government commenced lockdown restrictions on March 16, 2020, to reduce the spread of COVID-19. Over the next 30 days, the number of cases in Australia rose from 310 to 6,400, and the first deaths were recorded (4). Fortunately, this was followed by a reduction in the number of new cases due to successful lockdown restrictions as there were only 588 new cases in the following 30 days. As such, the period of data collection reflects the peak of the Australian COVID-19 epidemic curve. These authors speculate that, as lockdown restrictions are eased, these social impacts will lessen and that HF admissions will return to levels observed in the pre-COVID era. The long-term sequelae of this interruption remains to be seen.
It is notable that the present cohort demonstrated a significant reduction in prescriptions for ACE inhibitors/ARBs in the COVID era. Lower use may be due to the widely publicized concerns regarding upregulation of the ACE2 receptor by these drug classes, given that this receptor is known to mediate SARS-CoV-2 cellular entry (5). However, in light of the strong evidence supporting use of these agents in patients with HF, underutilization of these therapies is not medically justifiable (6).
A limitation of these data reporting trends in hospitalizations is the variation in the timing of data sampling across the years. Seasonality may account for a variation of at most 20% in HF admissions (7).
In conclusion, this paper reports a 41% reduction in HF hospitalizations and a significant increase in the proportion of patients presenting with NYHA functional class III/IV symptoms in the COVID-19 era. Despite restructuring of management pathways, in-hospital clinical outcomes in patients admitted with HF remained unchanged. Underuse of ACE inhibitor and ARBs is of concern and may translate to adverse clinical outcomes. Examining reasons for the reduced hospital presentations and enhancing integrated multidisciplinary outpatient models of care in this pandemic may mitigate the collateral impact of COVID-19 in patients with HF.
Footnotes
Please note: Dr. Koshy is a recipient of the National Health and Medical Research Council of Australia/National Heart Foundation Post-Graduate Scholarship and Royal Australasian College of Physicians Blackburn Scholarship (1150874). All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Heart Failureauthor instructions page.
References
- 1.Mehra M., Ruschitzka F. COVID-19 Illness and Heart Failure: A Missing Link? J Am Coll Cardiol HF. 2020;8:512–514. doi: 10.1016/j.jchf.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Driscoll A., Dinh D., Prior D., Kaye D., Hare D., Neil C. Heart Lung Circ; 2020. The effect of transitional care on 30-day outcomes in patients hospitalised with acute heart failure. Apr 10 [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Australian Department of Health Coronavirus (COVID-19) health alert 2020. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert Available at:
- 5.Sparks M.A., South A., Welling P., Luther J.M., Cohen J., Byrd J.B. Sound science before quick judgement regarding RAS blockade in COVID-19. Clin J Am Soc Nephrol. 2020;15:714–716. doi: 10.2215/CJN.03530320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tomasoni D., Italia L., Adamo M., Inciardi R.M., Lombardi C.M., Solomon S.D. COVID 19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail. 2020;22:957–966. doi: 10.1002/ejhf.1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel N., Nalluri N., Deshmukh A., Pant S., Shah N., Badheka A. Seasonal trends of heart failure hospitalizations in the United States: a national perspective from 2000 to 2011. Int J Cardiol. 2014;173:562–563. doi: 10.1016/j.ijcard.2014.03.122. [DOI] [PubMed] [Google Scholar]