Abstract
Introduction
The transmission of COVID-19 virus since the outbreak of viral pneumonia due to SARS-CoV-2 gave rise to protective operative measures. Aerosol generating procedures such as laparoscopic surgery are known to be associated with increased risks of viral transmission to the healthcare workers. The safety of laparoscopy during the pandemic was then debated. We aimed to systematically review the literature regarding the safe use of laparoscopy during COVID-19.
Methods
We performed a systematic search using PubMed and ScienceDirect databases from inception to 1st May, 2020. The following search terms were used: ‘‘laparoscopic surgery and COVID-19’’; ‘‘minimally invasive surgery and COVID-19’’. Search items were considered from the nature of the articles, date of publication, aims and findings in relation to use of laparoscopic surgery during COVID-19. The study protocol was registered with PROSPERO register for systematic reviews (CRD42020183432).
Results
Altogether, 174 relevant citations were identified and reviewed for this study, of which 22 articles were included. The analysis of the findings in relation to laparoscopic surgery during the pandemic were presented in tabular form. We completed the common recommendations for performing laparoscopy during the COVID-19 pandemic in forms of pre-, intra- and postoperative phases.
Conclusion
There is no scientific evidence to date for the transmission of COVID-19 by laparoscopic surgery. Laparoscopy can be used with precautions because of its benefits compared to open surgery. If safe, conservative management is the primary alternative during the pandemic. We concluded that recommended precautions should be respected while performing laparoscopy during the pandemic.
Keywords: COVID-19, Laparoscopy, Laparoscopic surgery, Minimally invasive surgery, Pandemic, Surgery, SARS-CoV-2
Introduction
An outbreak of clusters of viral pneumonia due to a novel coronavirus (2019-nCoV/SARS-CoV-2) occurred in Wuhan, Hubei Province in China in December 2019.1 Since the outbreak, several groups have estimated the R0, as a starting point for projections of the course of the Coronavirus Disease 2019 (COVID-19).2 Unlike severe acute respiratory syndrome, patients with COVID-19 had the highest viral load near symptom presentation, which could account for the fast-spreading nature of this pandemic.3 The virus of the infection, has been identified in respiratory tract specimens one to two days before the onset of symptoms, and has persisted for up to eight days after the onset of symptoms in mild cases and for longer periods in more severe cases, peaking in the second week after contagion.4 Viral RNA has been detected in faeces, whole blood, serum, saliva, nasopharyngeal specimens, and urine.3 , 5
Aerosol generating procedures (AGPs) are associated with an increased risk of infection to the health-care workers (HCW). Aerosols are particles formed by solid or liquid particles diffused and suspended in the air.6 AGPs involve intubation, extubation, chest tube insertion, bronchoscopy, gastrointestinal endoscopy, laparoscopy, and the use of energy devices such as electrocautery. While, pneumoperitoneum is an essential method during laparoscopic surgery, the technique brings about the risk of aerosol exposure to the operating team.7 Aerosol exposure occurs during intentional or unintentional release of CO2 which is most likely to occur during insertion or removal of ports, introduction, and removal of instruments through the ports, specimen retrieval and removal of pneumoperitoneum at the end of surgery. Risks of smoke inhalation to surgeons and staff when carrying out laparoscopic surgery has also been documented.8 If COVID-19 particles are present within the body cavity of the patient in the operation room, the HCW, endures and increased risk of contagion beyond that during an open operation.7
Laparoscopic surgery is known in general to carry a lot of benefits for the patients, however, today the safety of laparoscopic surgery is debated out of fear for COVID-19 transmission, arising from the potential generation of SARS-CoV-2 contaminated aerosols from CO2 leakage and the creation of smoke from the use of energy devices.9 Therefore, we aimed to systematically review the literature and the recommendations regarding the safe use of laparoscopic surgery during the COVID-19 pandemic. We focused on the laparoscopic use of Co2, the possible gas leak, the possible viral contamination from laparoscopy, the benefits of laparoscopy and other management options such as conservative and open surgery.
Methods
We performed a systematic search of using PubMed and ScienceDirect databases from inception to 30 April 2020. The following search terms were used: ‘‘laparoscopic surgery and COVID-19’’; ‘‘minimally invasive surgery and COVID-19″, also grey citations were added.
Search items were considered from the nature of the articles, date of publication, forum of publication, aims and main findings in relation to use of laparoscopic surgery during COVID-19 pandemic. The study protocol was recorded with PROSPERO register for systematic reviews (CRD42020183432).
Inclusion criteria
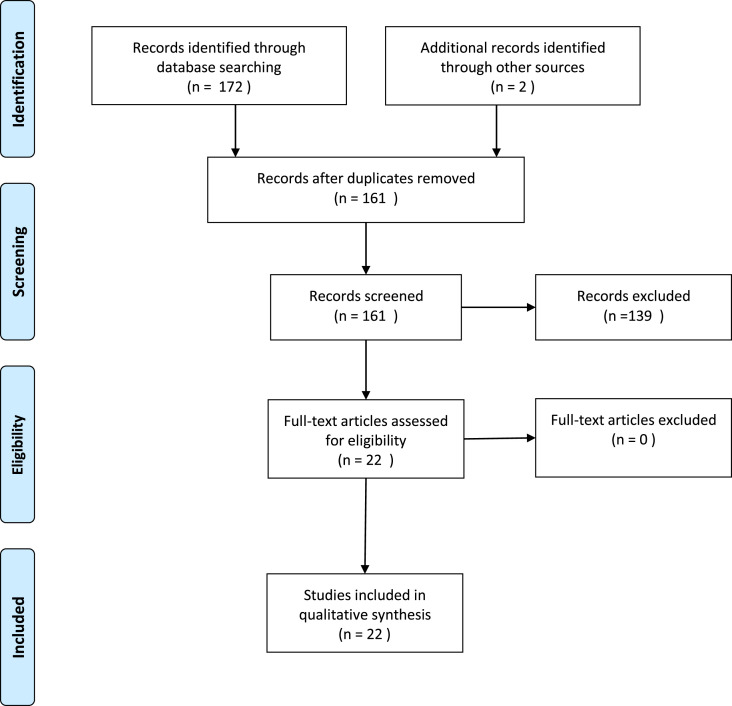
Using the search terms, we identidied citations about the use of laparoscopy under the COVID-19 pandemic and included the citations written in English (Fig. 1 ). The included references existed in the form of relevant published papers including systematic and narrative reviews, overview, expert opinion, perspectives, case presentation, commentary, correspondence, letter to Editor and peer reviewed societies’ recommendations.
Fig. 1.
Flow diagram of the systematic search.
Exclusion criteria
Citations not related to laparoscopy under COVID-19 were omitted. Likewise, search items not available in English or in full text were left out (Fig. 1).
Synthesis and analysis
The procedure comprised two authors’ inspection of titles, abstracts, and full-text papers, which were reviewed against the inclusion and exclusion criteria. The first author performed the detailed literature search. The final list of citations was completed by both authors. Search items were studied from the nature of the article, date of publication, as well as aims and findings in relation to laparoscopy as an appropriate and outstanding method for surgery during the COVID-19 pandemic. A narrative synthesis was performed to scrutinize the findings of the studies regarding guidelines and recommendations for the use of laparoscopy during the pandemic.
First, a preliminary synthesis was undertaken in form of thematic analysis involving listing articles in a tabular form. Then the results were discussed and structured after which they were summarized in a narrative synthesis. Furthermore, advantages and disadvantages from the health-care staff's safety perspective while working close to a patient subject to COVID-19 were clarified. Personal experiences in performing laparoscopy during the pandemic were at hand during this time when elective surgeries are postponed creating room for COVID-related emergencies. Future directions were articulated based on the results along with an evaluation of limitations and strengths of the full papers.
Results
Altogether, 174 relevant citations were identified and reviewed for this study (Fig. 1). After reading the titles and abstracts, the full texts were read for further evaluation. In total, 22 articles remained and were included in this study. The search items were read in English and the short timespan the pandemic has prevailed, made some accepted papers exist in press (Table 1 ).
Table 1.
Analytical review of the included citations.
| Author (Year) | Journal | Study | Purpose & focus | Findings/recommendations for laparoscopy under COVID-19 |
|---|---|---|---|---|
| Al Balas, Al Balas, Al Balas (2020)10 | The American Journal of Surgery | Overview | Surgery during the COVID-19 pandemic: laparoscopy or laparotomy? | Advocated careful attention during pneumoperitoneum creation and strict aerosol management even during the operation. Pneumoperitoneum pressure and CO2 ventilation should be as low as possible. Direct suction connected to a vacuum suction unit should be used for surgical smoke and pneumoperitoneum evacuation. |
| Altinbaş Tapisiz, Üstün (2020)11 | Turkish Journal of Medical Sciences | Review | The concepts related to laparoscopic gynaecological surgery during COVID-19 pandemic in the light of current literature, are listed. | Minimally invasive approaches shorten the recovery and reduces the hospitalization period of the patients. All precautions should be considered, both protective equipment as well as recommendations about any type of surgery that may have include a risk of aerosolization. |
| Aminnejad, Salimi, Bastanhagh (2020)12 | The Journal of Minimally Invasive Gynecology | Letter to the editor | Regarding “Understanding the “Scope” of the Problem: Why Laparoscopy is Considered Safe During the COVID-19 Pandemic" | No case of virus transmission through surgical plume or smoke has been confirmed yet, but no research has been conducted that refutes such a possibility. Yet, no space in the abdominopelvic cavity can be considered virus-free and importing a laparoscopic trocar to any point of this space carries the risk of spreading the virus throughout the operating theatre by gas insufflation. Laparoscopy can be performed with precautions to reduce the risk of virus transmission as much as possible. |
| Bogani, Raspagliesi, (2020)13 | The Journal of Minimally Invasive Gynecology | Letter to Editor | Minimally Invasive Surgery at the Time of COVID-19: The OR Staff Needs Protection | The release of aerosol through the trocar valves might potentially expose the operating theatre staff to SARS-CoV-2. Pneumoperitoneum pressure and the power settings of electrosurgery should be as low as possible. Apply filters to reduce possible spread of the virus. Adequate personal protective equipment is necessary for all staff working in the operative theatre. Isobaric minimally invasive technique and robotic-assisted surgery might reduce the risk of infection in the operating theatre staff. |
| Chew, Tan, Ng, Ng (2020)14 | Singapore Medical Journal | Commentary | Reconsidering elective surgery | In laparoscopic colorectal surgery: laparoscopy can lead to aerosolization of blood-borne viruses, although the applicability to SARS-CoV-2 remains unknown. In laparoscopic colorectal surgery, there may be risks of faecal spillage into the pneumoperitoneum due to bowel injury. There is no evidence to suggest a concurrent higher viral load in the pneumoperitoneum during laparoscopic surgery. For colorectal surgery specifically, transanal procedures may have to be approached with caution, especially in transanal minimally invasive surgery and transanal total mesorectal excision procedures. |
| Cohen, Liu, Abrao, Smart, Heniford (2020)15 | The Journal of Minimally Invasive Gynecology | Perspe-ctives | Perspectives on Surgery in the Time of COVID-19: Safety First | Nonoperative treatment is advocated with surgery delay until recovered for COVID-19 positive patients, unless they have a life-threatening emergency. If surgery cannot be delayed for a patient who is COVID-19 positive, open surgery should be performed. Laparoscopy can be performed in a patient whose COVID-19 status is unknown if the entire operating theatre team has access to necessary personal protective equipment and extreme care should be taken to prevent release of pneumoperitoneum. If these measures are not in place, open surgery is the alternative. The use of laparoscopy should be reserved for the patient who is COVID-19 negative with full deployment of personal protective equipment |
| De Simone, Chouillard, Di Saverio et al. (2020)16 | Annals of The Royal College of Surgeons of England | Systematic review | Reviewing the most current data on COVID-19 to provide essential suggestions on how to manage the acute abdomen during the pandemic. |
In surgical patients with COVID-19, great care must be taken when carrying out a laparoscopic procedure as there is a hypothetical risk for occupational exposure and infection of the operating theatre staff. Having reviewed the available literature on COVID-19, authors concur that when considering the laparoscopic approach in an emergency, every effort should be made to limit the leakage of gas through advocated techniques for laparoscopy. |
| Di Marzo, Cardi (2020)17 | The Journal of Minimally Invasive Gynecology | Commentary | Regarding “Understanding the “Scope” of the Problem: Why Laparoscopy is Considered Safe During the COVID-19 Pandemic" | High efficiency particulate arrestance filters are extremely effective in capturing a very high proportion, up to 100%, of nanoparticulate contaminants, ranging in size from 0.1 to 0.001 micron (diffusion regime) because they do not fly straight, collide with other fast-moving molecules, move around in random pathways and hit the filter fibres remaining stuck in them. The intersecting regime has just a small dip in efficiency that affects the particles of around 0.3 μm, defined as most penetrating particle size (MPPS). Typical HEPA filter varies from 0.2 to 0.3 micron depending on flow rate. Lowering the flow speed will result in making a simple HEPA perform as an ultra-low particulate arrestance (ULPA) filter. |
| Di Saverio, Marzo Khan, Pata et al. (2020)18 | Journal of Trauma and Acute Care Surgery | Expert opinion | Laparoscopy at all costs? Not now during COVID-19? | The use Non Operative Management strategies should be encouraged whenever possible and safe, even with established outpatient management and follow up for sub-acute, uncomplicated and/or mild abdominal conditions (e.g. Acute, non-severe cholecystitis, uncomplicated or maximum Hinchey 1a diverticulitis, uncomplicated appendicitis) by telephone or remote follow up if the patient is suitable for oral intake (food and antibiotics) and reliable is assessing remotely their response to treatment. The recommended use of filtration devices, smoke evacuation device connected to trocars, use of self-sealing trocars connected to negative pressure suction. Authors feel safer performing open surgery as much as possible mentioning that open surgery can be less time-consuming during the pandemic. Exploratory laparotomy can be performed without any use of cautery to avoid smoke production. Hot gallbladders are initially managed conservatively with antibiotics and/or percutaneous cholecystostomy drainage. Preoperative imaging should be implemented in all patients with lower abdominal pain to avoid diagnostic laparoscopies and negative appendicectomies. Perforated appendicitis needs urgent surgery by open surgery in all COVID positive or suspected patients. |
| Di Saverio, Pata, Gall et al. (2020)19 | Colorectal Disease | Advise and guidance | Coronavirus pandemic and Colorectal surgery: practical advice based on the Italian experience | The conservative management of COVID-19-positive patients with diseases of surgical interest should be as conservative as possible. Only life-threatening colorectal emergencies should be treated (i.e., intestinal perforation, obstruction, and bleeding). The use of laparoscopy in confirmed COVID-19 positive patient needing colorectal surgery must be carefully considered. It is advisable to use trocars with self-sealing type Hasson and to make the incision as small as practicable. Connect the trocar trephine to negative pressure suction with water seal. The insufflator must be turned off and the pneumoperitoneum must be emptied by negative pressure connected to a water seal before releasing the pneumoperitoneum. In COVID-19 positive emergency cases, authors adopted a selective use of laparoscopy when the appropriate equipment is available and safely used. Recommendations for operating theatre settings and use of laparoscopy have been described. |
| Francis, Dort, Cho (2020)20 | Surgical Endoscopy | Guidelines | SAGES and EAES recom-mendations for minimally invasive surgery during COVID-19 pandemic | Although specific evidence to COVID-19 and the risk for aerosol transmission during laparoscopy is lacking, every effort must be made to minimize this potential risk through following recommendations. |
| Kimmig, Verheijen, Rudnickin SERGS Council (2020)21 | Journal of Gynecologic Oncology | Position Statement | A statement of the Society of European Robotic Gynecological Surgery (SERGS) | Robot-assisted surgery (RAS) reduces hospital stay for patients who need complex-oncological-surgery, which allow making room for COVID-19 patients. RAS reduces not only contamination with body fluids and surgical gasses of the surgical area, but also the number of directly exposed medical staff when compared to open surgery. Surgical precautions under COVID-19 circumstances must be taken, with the addition of prevention of gas leakage. Evidently, if precautions cannot all be taken, e.g., by lack of equipment, consider if open surgery would be safer or whether indeed surgery would be feasible at all under the circumstances. |
| Mallick, Odejinmi, Clark (2020)22 | Facts, Views & Vision in Obgyn | Opinion article | Recommendations for laparoscopic surgery in suspected or confirmed COVID-19 | Non-surgical treatments are utilised if possible, to reduce the risk of horizontal transmission of SARS-CoV-2 virus to health care workers (HCW), and reduce the need for hospital admission, provided they are a safe alternative. COVID negative patients can proceed with the standard laparoscopy and routine surgical infection control procedures. The laparoscopy is undertaken by the most experienced surgeon for safe laparoscopy performed in the shortest time possible. Recommendations to protect operating staff during laparoscopy have been mentioned. Gynaecological operations that carry a risk of bowel involvement, however small should be performed by laparotomy. Total laparoscopic hysterectomy in malignancies, can continue to be undertaken in the pandemic. |
| Morris, Nickles Fader, Milad, Dionisi (2020)23 | The Journal of Minimally Invasive Gynecology | Overview | Why Laparoscopy is Considered Safe During the COVID-19 Pandemic | Performing laparoscopy with lower intraabdominal CO2 pressures and minimizing the use of energy limit the production of surgical plume and pneumoperitoneum. The use of a smoke evacuation/filtration system controls release and filtration of the surgical plume. Gas and plume evacuation and filtration is achieved with the use of ultralow particulate air filter (ULPA) rated to screen particles of 0.1 micron in diameter (e.g., the ConMed Airseal or Stryker Pneumoseal). High efficiency air filters (HEPA) filters particles of 0.3 micron in diameter. N95 masks filter out at least 95% of 0.3-micron particles. Laparoscopy can almost entirely contain the surgical plume in the abdominal cavity; therefore, avoid release of the pneumoperitoneum. The abdominal cavity should be actively desufflated through a filtration system or with a simple piece of tubing attached to a suction. Use of a containment bag for tissue extraction can limit loss of pneumoperitoneum. |
| Novara, Giannarini, De Nunzio, Porpiglia, Ficarra (2020)24 | European Urology | Overview | Risk of SARS-CoV-2 Diffusion when Performing Minimally Invasive Surgery During the COVID-19 Pandemic | Special care must be taken intraoperatively to reduce smoke formation (e.g., lowering electrocautery power settings, using bipolar electrocautery, electrocautery or ultrasonic scalpels sparingly to reduce surgical smoke). This is crucial when removing trocars at the end of a procedure, when making a skin incision for specimen retrieval, and in the conversion to open surgery. Generous use of suction to remove smoke and aerosol should be advocated. Care must be taken to limit smoke dispersal or spillage from trocars (e.g., lowering the pneumoperitoneum pressure). It can be beneficial to use pressure-barrier insufflator systems to maintain a forced-gas pressure barrier at the proximal end of the trocar. |
| Pawar, Pokharkar, Gori et al. (2020)25 | Journal of Laparo-endoscopic & Advanced Surgical Techniques | Case presenta-tion | Is there evidence for viral transmission through surgical smoke in laparoscopy? . |
A case of 28 years old female patient with carcinoma rectum had near total intestinal obstruction. She was operated on utilizing laparoscopic anterior resection. Safe gas evacuation was performed using the air seal (CONMED, Utica, NY) and high-efficiency particulate air (HEPA) filter. Precautions using N95 masks and personal protective equipment (PPE) is advised. Air filtration products like aerosol, HEPA filters are of great aid in safe evacuation of gases. Authors have done 12 laparoscopic colorectal cancer procedures using airseal and a HEPA filter since March 30, 2020. They believe that using laparoscopy even if there is risk, will be very minimal if all precautions are taken. |
| Schwarz, Tuech (2020)26 | British Journal of Surgery | Correspondence | Is the use of laparoscopy in a COVID-19 epidemic free of risk? | If the laparoscopy is indicated, it is recommended: to check all instruments and the proper functioning of the suction system, to use balloon trocars and create suitable holes for the introduction of leak-free trocars; not to create a leak in the presence of smoke obstructing the surgical field, but to extract the smoke by the vacuum suction device; and to aspirate the entire pneumoperitoneum before removing the trocars. Laparoscopy should be performed by an experienced surgeon. In case of doubt or lack of experience in laparoscopy, a laparotomy should be performed. The authors stated that there is a theoretical risk that should be weighed against the benefit of laparoscopy. |
| Tuech, et al. (2020)27 | Journal of Visceral Surgery |
Original article | What strategy for digestive and oncological surgery is good during the Covid-19? | Elective surgery for benign disorders should be postponed. For patients who are or may be infected by Covid-19 and who require emergency surgery, consider protection of HCWs. Laparoscopy is preferred if the patient's cardiorespiratory status is stable. Emergency surgery is the priority and elective surgery should be postponed. In cancer surgery, there is an added risk due to the pandemic that must be balanced against the risk incurred by deferring surgery. For each type of cancer: colon, pancreas, oesogastric, and hepatocellular carcinoma; authors stated morbidity and mortality rates and compared with the oncological risk incurred by deferring surgery and/or the tumour doubling time. |
| Vigneswaran Prachand, Posner, Matthews,Hussain (2020)28 | Journal of Gastro-intestinal Surgery | Review article | What Is the Appropriate Use of Laparoscopy over Open Procedures in the Current COVID-19 Climate? | Laparoscopy should be performed with the precautions as it still may be of benefit to the patients. Authors recommended avoiding traditional practices and creating a closed circuit for insufflation with the use of some sort of smoke evacuator device to avoid any release of pneumoperitoneum into the room. Desufflation at the end of the operation should be done through a smoke evacuator device or direct suction. Thereafter, care should be taken to evacuate the abdomen under direct vision for as long as possible and placing the tip of the trocar on suction away from bowel, either resting above the liver or turned up toward the abdominal wall. Any specimen to be removed should be done with the abdomen desufflated. All precautions should be taken whenever possible to minimize the risk of transmission regardless of known COVID-19 status. Based on this review of the current scientific knowledge, no scientific evidence was found to support the use of open surgery over laparoscopy or robotic surgery to reduce viral transmission of COVID-19; however, there is still much to discover about the viral transmission. |
| Veziant, Bourdel, Slim (2020)29 | Journal of Visceral Surgery | Review | Risks of viral contamination in healthcare professionals during laparoscopy in the COVID-19 pandemic, | The risk of contamination of HCWs may be greater in laparoscopy than in laparotomy if gas leakage occurs or exsufflation is poorly controlled. No contamination of HCWs by SARS-CoV-2 during a laparoscopy is reported. Personal protection equipment (PPE) for HCWs: surgeon, assistant, scrub nurse or circulating nurse are less exposed than anaesthetist and anaesthetist's nurse, who are directly in contact with patient's upper airways, the main source of contamination. Every member of the HCW team must have according to WHO guidelines, PPE with long-sleeved fluid protection gowns, lined gloves, goggles and masks. The risk of contamination of HCWs is highest during the insertion of trocars, extraction of the excised tissues and removal of trocars at the end of the operation. Recommendation in the use of laparoscopy included preferring the ‘closed’ technique for obtaining pneumoperitoneum. Prefer intracorporeal bowel anastomosis and extract excised tissue after complete emptying of the pneumoperitoneum. No literature suggests that laparoscopy should be replaced by laparotomy during the Covid-19 epidemic. |
| ALSGBI https://www.alsgbi.org/2020/04/22/laparoscopy-in-the-covid-19-environment-alsgbi-position-statement/ [30] |
Internet | ALSGBI Position Statement | Association of laparoscopic surgeons of Great Britain and Ireland (ALSGBI) position statement regarding the use of laparoscopic surgery during COVID-19 | Benefits of laparoscopy include less hospital stay and increased bed availability, decreased complications and faster recovery and less contamination compared to open surgery. Recommendations: Elective laparoscopic procedures should be performed in clean area. Laparoscopic surgery should be performed by experienced surgeon to minimize operation time and potential of aerosolization Use of closed-circuit smoke evacuation/Ultra low particulate air filtration system. Lowest insufflation pressure (12 mmhg). Minimal use of energy device. Routine closed evacuation of gas at the end of procedure. Initiation of elective surgery should include careful case selection, starting with a younger patient group (under 70 years), with fewer comorbidities (ASA <2), aiming for day case/reduced hospital stay as standard practice. The risks and consequences of COVID-19 infection should form part of the informed consent process. ALSGBI support the use of laparoscopy in cases where there are clear benefits to the patient and where the hospital and theatre resources allow this as a safe option for the patient and staff. |
| IGSG https://www. rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/6 April (update) [31] |
Internet | Intercollegiate guidance on COVID-19 | Updated Intercollegiate General Surgery Guidance on COVID-19 | Disadvantages of laparoscopy: Laparoscopy generally should not be used as it is considered to carry some risks of aerosol-type formation and infection and considerable caution is advised. Consider laparoscopy only in selected individual cases where clinical benefit to the patient substantially exceeds the risk of potential viral transmission to surgical and theatre teams in that particular situation. Where non-operative management is possible and reasonable (such as for early appendicitis and acute cholecystitis) this should be implemented. Appropriate nonoperative treatment of appendicitis and open appendicectomy offer alternatives. |
The analysis of the articles and findings or recommendations in relation to laparoscopic surgery during the pandemic presented in Table 1. The theme which arose concerned the possible viral transmission via aerosol generation under the use of different devices during laparoscopy. We summarized the recommendations or guidelines for the safe use of the laparoscopic surgery during the COVID-19 pandemic by listing the protective procedures during the pre-, intra-, and postoperative phases (Table 2 ).
Table 2.
Recommendations for the safe use of laparoscopy during the pandemic.
| Preoperative considerations during covid-19 pandemic |
|---|
|
Settings of surgical theatre: Two teams: One inside and one outside the theatre
|
Entrance order to operating theatre:
|
Other precautions:
|
| Intraoperative considerations during covid-19 pandemic |
|---|
|
| Postoperative considerations during covid-19 pandemic |
Exit from operating theatre:
|
Exit order:
|
Other precautions:
|
Discussion
Laparoscopic surgery is an aerosol generating procedure because the technique needs the creation and maintenance of a pneumoperitoneum through Co2 insufflation. It was confirmed that after 10 min of laparoscopic dissection by electrosurgery or ultrasound, the concentration of particles measuring 0.3–0.5 μm was elevated with laparoscopy compared to those in open surgery.32 The risk of contamination of operating theatre staff can be increased by laparoscopy due to the pneumoperitoneum gas leak which may contain high concentrations of suspended viruses.8 In contrast, a closed surgical site should lower the risk of contamination, implying that there is yet no hard evidence in the literature of viral transmission of COVID-19 during laparoscopy.7
During laparoscopy the creation of a surgical plume is harmful when it persists and decreases visualization, often obliging the surgeon to remove the scope from the surgical field and eliminate the obstructing aerosol particles.33 Compromised visualization can be dangerous with serious impact of the composition of surgical smoke and its effects on the operating theater workers. Explicitly, the use of e.g. ultrasonic scalpel generates ‘surgical smoke’ which with or without a heating, containing bio-aerosols with viable and non-viable cellular material, creates a risk of viral infection and triggers irritation to the lungs generating acute and chronic inflammatory changes.34 Previous researchers stated that surgical smoke is a toxin, like cigarette smoke, along with other dangers that exist during surgery.35 This is especially true when tissue is contaminated with infectious viruses is aerosolized by lasers. The expected debris from the various categories of energy devices used in the abdomen such as Electrocautery <0.1 microns, laser ablation 0.3 microns and Ultrasonic scalpel are 0.35–6.5 microns.34 So, although the ability to aerosolize COVID-19 in the abdomen is unknown, minimizing electrosurgical use and the avoidance of certain devices, such as ultrasonic scalpel, may reduce aerosolization of particles in general and thus reduce the potential risk of viral emission.
Several viruses have been associated in different degrees to the contamination of HCWs during surgery; the presence of certain viruses in surgical smoke during laparoscopy such as HBV has been confirmed. HBV has a smaller RNA compared to SARS-CoV-2.36 Namely, SARS-CoV-2 virus responsible for the COVID-19 is an RNA virus of 0.06–0.14 m in size. In infected patients it can be found in the oropharynx, the respiratory tract, and the whole of the digestive tract.3 , 5 The mechanism for viral transmission is thought to happen directly from human to human or by contaminated surfaces. It has also been suggested, although sufficient evidence is lacking, that an aerosolizing procedure on an infected person creates smaller droplets from the respiratory tract; the droplets are thought to be able to reach up to 1 m distance and thereby touching another person's nose, mouth, or eyes.37 This raises the question regarding the theoretical risk of aerosolization of virus with the use of electrosurgical devices and whether eliminating or minimizing the use of these devices reduces the supposed risk.
However, no contamination of HCWs by SARS-CoV-2 during laparoscopy has yet been reported, but healthcare systems and researchers advise precautious measures during the pandemic to avoid any risk of HCWs contamination. Elective surgeries should be postponed and operative management should only be strongly indicated. Conservative approaches should be the option of choice, if possible. When surgery is indicated, the debate about type of surgery arises: laparoscopic or open surgery?.38
Due to the lack of information on the nature of the new virus, it is wise to mention that in patients who are COVID-19 positive, nonoperative treatment and delay of surgery should be considered whenever possible and safe. Common examples include mild appendicitis, Hinchey 1 diverticulitis and non-complicated cholecystitis.39, 40, 41
The benefits of laparoscopy compared to open surgery have previously been pointed out.42 However, some recommend open surgery for COVID-19 patients, while open surgery would be less time consuming.15 We believe there will be no significant time difference between the two techniques if laparoscopic surgery is performed by experts.43 In addition, open surgery requires a longer hospital stay and carries more postoperative complications which might increase the risk of viral contamination during the postoperative recovery period. Others stated that there is a theoretical risk for laparoscopy that should be weighed against the benefit of laparoscopy.26
Presently, the risk of operating on patients who are infected with SARS-CoV-2 (COVID-19) is debated. This debate whether laparoscopy or open surgery is preferred during the pandemic can be understood when The Royal College of Surgeons recommended that surgeons should not in general consider laparoscopic surgery,31 the Society of American Gastrointestinal and Endoscopic Surgeon (SAGES) recommended the use of filters for the released CO2 during laparoscopy and robotic surgery.20 On the other hand, the Association of Laparoscopic Surgeons of Great Britain and Ireland (ALSGBI) supported the use of laparoscopy and the American College of Surgeons have stated there are insufficient data to recommend for/against an open versus laparoscopy approach and surgeons should choose the approach that minimizes the operation time and maximizes safety.30 , 44
Limitations of the study
Due to the urgency and importance of performing emergency operative treatments also under a pandemic, we reviewed the recommendations and findings related to the use of laparoscopic surgery. The main limitation of this study is that there was no research hits yet, of cohort or randomised controlled study found to date, due to the detection of the new virus and the lack of information of its viral nature. Therefore, grading the studies included in this review was not applicable, instead a narrative synthesis was performed.
Conclusion
There is no scientific evidence to date for the transmission of COVID-19 by laparoscopic surgery. Laparoscopy, if strongly indicated, can be used with precautions because of its benefits for the patient compared to open surgery. If possible and safe, conservative management is the primary alternative during the pandemic. Based on our review, we concluded that recommended precautions should be respected while performing laparoscopy during COVID-19 pandemic to protect HCWs from possible aerosolised virus contamination.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare no conflict of interests.
Acknowledgement
We would like to thank Mr Simon Monkhouse for standing behind his team and for inspiring us conducting this research by defending the value of laparoscopic surgery during the pandemic.
References
- 1.Report of clustering pneumonia of unknown etiology in wuhan city. Wuhan Municipal Health Commission; 2019. http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989 [Google Scholar]
- 2.Wang H., Wang Z., Dong Y., Chang R., Xu C., Yu X., Wang Y. Phase-adjusted estimation of the number of coronavirus disease 2019 cases in Wuhan, China. Cell discovery. 2020;6(1):1–8. doi: 10.1038/s41421-020-0148-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.To K.K.W., Tsang O.T.Y., Leung W.S., Tam A.R., Wu T.C., Lung D.C., et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020 March 28 doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y., Yan L.M., Wan L., Xiang T.X., Le A., Liu J.M., Zhang W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020 March 19 doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng L., Liu J., Xu W., Luo Q., Deng K., Lin B., et al. 2019 Novel Coronavirus can be detected in urine, blood, anal swabs and oropharyngeal swabs samples. medRxiv. 2020 doi: 10.1002/jmv.25936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Juan, Du Guoqiang. COVID-19 may transmit through aerosol. Ir J Med Sci. 2020:1–2. doi: 10.1007/s11845-020-02218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ESGE Recommendations on gynaecological laparoscopic surgery during covid-19 outbreak. 2020. https://esge.org/wp-content/uploads/2020/03/Covid19StatementESGE.pdf [PMC free article] [PubMed]
- 8.Zheng M.H., Boni L., Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020;272(1):e5–e6. doi: 10.1097/SLA.0000000000003924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Champault G., Taffinder N., Ziol M., Riskalla H., Catheline J.M.C. Cells are present in the smoke created during laparoscopic surgery. Br J Surg. 1997;84(7):993–995. doi: 10.1002/bjs.1800840724. [DOI] [PubMed] [Google Scholar]
- 10.Al-Balas M., Al-Balas H.I., Al-Balas H. Surgery during the COVID-19 pandemic: a comprehensive overview and perioperative care. Am J Surg. 2020 April 18 doi: 10.1016/j.amjsurg.2020.04018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiykaç A.Ş., Tapisiz Ö.L., Üstün Y. Gynecological laparoscopic surgery in the shade of COVID-19 pandemic. Turk J Med Sci. 2020 April 30 doi: 10.3906/sag-2004-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aminnejad R., Salimi A., Bastanhagh E. Regarding "understanding the "scope" of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J Minim Invasive Gynecol. 2020 Apr 25;(20) doi: 10.1016/j.jmig.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bogani G., Raspagliesi F. Minimally invasive surgery at the time of COVID-19: the OR staff needs protection. J Minim Invasive Gynecol. 2020 July–August;27(5):1221. doi: 10.1016/j.jmig.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chew M.H., Tan W.J., Ng C.Y., Ng K.H. Deeply reconsidering elective surgery: worldwide concerns regarding colorectal surgery in a COVID-19 pandemic and a Singapore perspective. Singap Med J. 2020 doi: 10.11622/smedj.2020070. ISSN:0037-5675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen S.L., Liu G., Abrao M., Smart N., Heniford T. Perspectives on surgery in the time of COVID-19: safety first. J Minim Invasive Gynecol. 2020;27(4):792–793. doi: 10.1016/j.jmig.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Simone B., Chouillard E., Di Saverio S., Pagani L., Sartelli M., Biffl W.L.,, Campanile F.C. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020:1–10. doi: 10.1308/rcsann.2020.0097. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Di Marzo F., Cardi M. Regarding 'understanding the "scope" of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J Minim Invasive Gynecol. 2020;S1553–4650(20):30215–30216. doi: 10.1016/j.jmig.2020.04.027. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Saverio S., Khan M., Pata F., Ietto G., De Simone B., Zani E., et al. Laparoscopy at all costs? Not now during COVID-19 and not for acute care surgery and emergency colorectal surgery: a practical algorithm from a Hub Tertiary teaching hospital in Northern Lombardy, Italy. J Trauma Acute Care Surg. 2020;88(6):715–718. doi: 10.1097/TA.0000000000002727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Saverio S., Pata F., Gallo G., Carrano F., Scorza A., Sileri P.,, Pellino G. Colorectal Disease; 2020. Coronavirus pandemic and Colorectal surgery: practical advice based on the Italian experience. [DOI] [PubMed] [Google Scholar]
- 20.Francis N., Dort J., Cho E., Feldman L., Keller D., Lim R., Wasco K. SAGES and EAES recommendations for minimally invasive surgery during COVID-19 pandemic. Surg Endosc. 2020:1–5. doi: 10.1007/s00464-020-07565-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kimmig R., Verheijen R.H., Rudnicki M. Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: a statement of the Society of European Robotic Gynaecological Surgery (SERGS) Journal of Gynecologic Oncology. 2020;31(3) doi: 10.3802/jgo.2020.31.e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mallick R., Odejinmi F., Clark T.J. Covid 19 pandemic and gynaecological laparoscopic surgery: knowns and unknowns. Facts, Views & Vision in Obgyn. 2020;12(1):3. [PMC free article] [PubMed] [Google Scholar]
- 23.Morris S.N., Fader A.N., Milad M.P., Dionisi H.J. Understanding the “scope” of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J Minim Invasive Gynecol. 2020;27(4):789–791. doi: 10.1016/j.jmig.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Novara G., Giannarini G., De Nunzio C., Porpiglia F., Ficarra V. Risk of SARS-CoV-2 diffusion when performing minimally invasive surgery during the COVID-19 pandemic. Eur Urol. 2020 Jul;78(1):e12–e13. doi: 10.1016/j.eururo.2020.04.015. Published online 2020 Apr 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pawar T., Pokharkar A., Gori J., Pandey D., Rohila J., Dsouza A., et al. The technique and justification for minimally invasive surgery in COVID-19 pandemic: laparoscopic anterior resection for near obstructed rectal carcinoma. J Laparoendosc Adv Surg Tech. 2020 doi: 10.1089/lap.2020.0241. [DOI] [PubMed] [Google Scholar]
- 26.Schwarz L., Tuech J.J. Is the use of laparoscopy in a COVID-19 epidemic free of risk? Br J Surg. 2020 Apr 28 doi: 10.1002/bis.11649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tuech J.J., Gangloff A., Di Fiore F., Michel P., Brigand C., Slim K., Schwarz L. Strategy for the practice of digestive and oncological surgery during the Covid-19 epidemic. Journal of visceral surgery. 2020;157(3):7–12. doi: 10.1016/j.jviscsurg.2020.03.008. suppl.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vigneswaran Y., Prachand V.N., Posner M.C., Matthews J.B., Hussain M. What is the appropriate use of laparoscopy over open procedures in the current COVID-19 climate? J Gastrointest Surg. 2020;1 doi: 10.1007/s11605-020-04592-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Veziant J., Bourdel N., Slim K. Risks of viral contamination in healthcare professionals during laparoscopy in the Covid-19 pandemic. Journal of Visceral Surgery. 2020;157(3):59–68. doi: 10.1016/j.jviscsurg.2020.04.010. Suppl.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ALSBI . ALSGBI. The Royal College of Surgeons of England, Lincoln's Inn Fields; London, WC2A 3PE: 2020. Laparoscopy-in-the-covid-19-environment-alsgbi-position-statement; pp. 35–43.https://www.alsgbi.org/2020/04/22/laparoscopy-in-the-covid-19-environment-alsgbi-positionstatement/ [Google Scholar]
- 31.IGSG Coronavirus-guidance-for-surgeons. 2020. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/6 ∖.
- 32.Li C.I., Pai J.Y., Chen C.H. Characterisation of smoke generatedduring the use of surgical knife in laparotomy surgeries. J AirWaste Manag Assoc. 2020;70:324–332. doi: 10.1080/10962247.2020.1717675. [DOI] [PubMed] [Google Scholar]
- 33.Devassy R., Gopalakrishnan S., De Wilde R.L. Surgical efficacy among laparoscopic ultrasonic dissectors: are we advancing safely? A review of literature. J Obstet Gynaecol India. 2015;65(5):293–300. doi: 10.1007/s13224-015-0774-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alp E., Bijl D., Bleichrodt R.P., Hansson B., Voss A. Surgical smoke and infection control. J Hosp Infect. 2006;62(1):1–5. doi: 10.1016/j.jhin.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 35.Barrett W.L., Garber S.M. Surgical smoke: a review of the literature. Surg Endosc. 2003;17(6) doi: 10.1007/s00464-002-8584-5. [DOI] [PubMed] [Google Scholar]
- 36.Kwak H.D., Kim S.H., Seo Y.S., Song K.J. Detecting hepatitis B virusin surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73:857–863. doi: 10.1136/oemed-2016-103724. [DOI] [PubMed] [Google Scholar]
- 37.Kim J.M., Chung Y.S., Jo H.J., Lee N.J., Kim M.S., Woo S.H., et al. Identification of coronavirus isolated from a patient in korea with COVID-19. Osong Public Health Res Perspect. 2020;11(1):3–7. doi: 10.24171/j.phrp.2020.11.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lambertini M., Toss A., Passaro A., Criscitiello C., Cremolini C., Cardone C., et al. 2020. Cancer care during the spread of coronavirus disease 2019 (COVID-19) in Italy: young oncologists' perspective. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Swanson S.M., Strate L.L. Acute colonic diverticulitis. Ann Intern Med. 2018;168(9):ITC65–ITC80. doi: 10.7326/AITC201805010. [DOI] [PubMed] [Google Scholar]
- 40.Hatzidakis A.A., Prassopoulos P., Petinarakis I., Sanidas E., Chrysos E., Chalkiadakis G., et al. Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol. 2002;12(7):1778–1784. doi: 10.1007/s00330-001-1247-4. [DOI] [PubMed] [Google Scholar]
- 41.Sakorafas G.H., Mastoraki A., Lappas C., Sampanis D., Danias N., Smyrniotis V. Conservative treatment of acute appendicitis: heresy or an effective and acceptable alternative to surgery? Eur J Gastroenterol Hepatol. 2011;23(2):121–127. doi: 10.1097/MEG.0b013e32834233b6. [DOI] [PubMed] [Google Scholar]
- 42.Velanovich V. Laparoscopic vs open surgery. Surg Endosc. 2000;14(1):16–21. doi: 10.1007/s004649900003. [DOI] [PubMed] [Google Scholar]
- 43.Emken J.L., McDougall E.M., Clayman R.V. Training and assessment of laparoscopic skills. J Soc Laparoendosc Surg: J Soc Laparoendosc Surg. 2004;8(2):195. [PMC free article] [PubMed] [Google Scholar]
- 44.American College of Surgeons COVID-19: elective case triage guidelines for surgical care. 2020. https://www.facs.org/covid-19/clinical-guidance/elective-case