Abstract
The increasing prevalence of Alzheimer disease (AD), higher risk among certain ethnoracial groups, and lack of effective therapies highlights the need to recruit and enroll diverse populations in prospective, observational studies and clinical trials. However, there is little known about the effectiveness of traditional media vs. social media outreach on recruitment in aging study studies. This study retrospectively examined the effectiveness and differences in using both traditional and social media materials for the recruitment of African American (AA) versus non-Hispanic white (NHW) participants for a prospective, longitudinal study examining preclinical AD and driving outcomes. Participants needed to be at least 65 years old, drive at least an average of once weekly, own a vehicle that was manufactured in 1996 or later, and agree to cognitive testing, psychometric testing, brain magnetic resonance imaging (MRI), brain amyloid positron emission tomography (PET), and cerebrospinal fluid collection via lumbar puncture. A total of 546 individuals contacted the study coordinator by phone or email. Of those individuals, 97 enrolled and 192 were not contacted secondary to filling enrollment capacity. Sixteen participants (16.5%) were AA and the remainder were NHW. Of the 354 individuals who inquired, approximately 73% declined or did not return calls. Social media was more effective with recruiting NHW participants, while traditional advertisement (newspaper) was more successful in recruiting AA participants in this urban setting. Prospective studies should balance participant burden and enrollment with a targeted, multi-tiered recruitment plan and sufficient budget to reach the population of interest.
Introduction
Alzheimer disease (AD) currently affects an estimated 5.8 million people in the United States, most often interfering with the lives of those who are over 65 years old (Alzheimer’s Association, 2019a). In individuals age 65 and over, one in ten have AD, whereas at age 80, the risk increases to one in three (Alzheimer’s Association, 2019a). However, prevalence measures show that African Americans (AAs), who make up approximately 13.4% of the US population (US Census Bureau, 2018), may be two times more likely to have the disease compared to their NHW counterparts (Alzheimer’s Association, 2019a). As the population of the United States begins to shift toward having more people of color, AD threatens to increase its numbers further, with approximately 14 million people affected by 2050 (Alzheimer’s Association, 2019a).
While the search for reasons about the source of this racial disparity in AD is progressing, there is a disconnect between the number of AAs with AD and the number reflected in those actively participating in research (Alzheimer’s Association, 2019a). Much of the research to date has been completed with non-Hispanic white (NHW) participants, and the scientific community realizes that it is essential that we study how and why the prevalence of the disease may differ between subgroups (Hill, et. al., 2015). As described recently by Babulal et al., we must examine genetics, biomarkers, and medical risk factors, as well as cultural differences and societal inequities among diverse racial and ethnic groups (Babulal et al., 2019). In order to understand all of the factors that affect these differences, AD studies have to start with enough non-white participants to answer these questions. The National Institutes of Health’s Funding Opportunity Announcement (FOA) on Health Disparities and Alzheimer’s Disease (NIH, 2015), the Alzheimer’s Association’s fellowship and grant programs to promote diversity (Alzheimer’s Association, 2019b), and other organizations are encouraging more diverse participant cohorts by providing focused grant opportunities for scientific research. The NIA Health Disparities Research Framework describes the importance of research on various populations, in order to develop new therapies and interventions generalizable to many groups (Hill et al., 2015). However, recruiting participants with diverse backgrounds is not a simple undertaking.
There is a long history and well-documented reasons why AAs are reluctant to enroll in research studies. Mistrust of research or institutions, lack of information about studies taking place or the outcomes of research, inconvenience, and insufficient clinicians or staff of color have all been cited as reasons for nonparticipation (Randolph, Coakley, & Shears, 2018; Williams et al., 2010). Additionally, some have suggested that AAs may experience more discomfort or misunderstanding due to researcher’s use of unfamiliar medical terminology. High level terminology (Epps, Skemp, & Specht, 2015), more fear of research treatments, side effects, and unnecessary procedures (Ford et al., 2013) compared to NHWs, and non-culturally specific means of recruitment and engagement may also cause AAs to have a reluctance to participate. It is incumbent upon researchers to understand these barriers and to explore ways to overcome them.
Past research points to some strategies that can improve positive recruitment outcomes among AAs. Many studies suggest that utilizing known community gatekeepers, recruiting in a trusted environment, hiring recruiters from the targeted demographic, developing trust, being open and transparent are of essential importance to recruitment (Ford et al., 2013; Randolph et al., 2018; Williams, et. al., 2011). One study, citing that AAs are more likely to use smartphones as their main method of accessing the internet, suggested the ability to use this innovative avenue for recruitment (James, et. al., 2017). Studies have shown that AA women are more likely to participate in research than are AA men, suggesting that engaging women in the recruiting process may be helpful in encouraging men to participate as well (Graham et al., 2018; James et al., 2017).
Little research has examined recruitment methods comparing traditional versus social media contact. One study described using traditional media advertising (newspapers, billboards, newsletters) and suggested that these advertisements, which accounted for approximately 15% of their recruitment, were most useful when used in conjunction with community-based efforts (Graham et al., 2018). In a study that utilized Facebook advertisements in Australia, more than sixteen thousand media clicks were received; however, no eligible individuals were recruited through this avenue and the race of participants was not documented (Miller et al., 2016). Another study using Facebook advertisement in Canada had success in recruitment, but as a study that did not mention race and was only collecting study data immediately online, it was less relatable to our current longitudinal, observational study (King, O’Rourke, & De Longis, 2014). With so little research investigating older adult recruitment online, studies are needed to add knowledge and fill that gap.
A study on preclinical AD and driving (R01AG043434; R01AG056466) sought to expand an existing cohort by recruiting additional participants, with a particular focus on increasing the percentage of AAs in the cohort. While some of the participants are referred by the Knight Alzheimer’s Disease Research Center (ADRC), this study sought to launch recruitment in the community by an interdisciplinary team (Psychology, Medicine, Social Work, Occupational Therapy). This retrospective study describes the methods used for recruitment of AA and NHW participants, including traditional media, social media, and in-person recruitment. While the objective did not set out to explicitly compare the effectiveness of various forms of recruitment, it is hopeful that this report will inform future outreach and recruitment efforts in AD studies.
Subjects and Methods
Participants were being recruited for an ongoing, longitudinal study at the Knight ADRC. All recruitment and study protocols were approved by the Washington University Institutional Review Board (IRB). Participants were required to be 65 years or older, cognitively normal with a Clinical Dementia Rating (CDR) of 0 (Morris, 1993), driving on average at least weekly, and agree to take part in an annual clinical assessment, psychometric assessment, and driving assessment (Roe et al., 2017a; Roe et al., 2017b). Additionally, participants had to agree to baseline and periodic biomarker measures (amyloid brain imaging and/or cerebrospinal fluid biomarker measures), as well as monitoring of their daily driving behavior using a commercial data logger plugged into the on-board diagnostics port of their vehicle (Babulal et al., 2016).
Study staff recruited participants through a number of avenues, including speaking engagements in the community, traditional media (newspaper; newsletter), and social media (online). Four speaking engagements were conducted, each of which discussed topics covering aging, driving, dementia, and aging research. Presentations were given by our team (G.M.B [other race], S.H.S [NHW]) at speaking engagements, and our team was generally not known by most of the audience. Events occurred at a public library (part of an Aging Ahead series [G.M.B]), a senior independent living community (part of Lifestyle Enrichment series [S.H.S]), a university-sponsored community education event (part of an Aging in Place series [G.M.B]), and a church (part of a weekly community health series [G.M.B]). All presentations in the community had no specific eligibility for attendees but targeted older adults (≥ 65 years). A standard PowerPoint presentation was used with talks varying from 5 to 45 minutes with 15 minutes for questions and answers. The presentation at the church was purposely selected because it was historically a black church and content was tailored for addressing disparities in aging and AD among AA older adults. Other venues were based upon community connections of the research team and venue availability/interest. At the end of each talk, a standard flyer was given out soliciting interest in aging and AD research, along with the inclusion/exclusion criteria, and contact information (phone and email) for the research coordinator.
A single flier was created in PowerPoint, which included the purpose of the study, inclusion/exclusion criteria, study commitment, and participant remuneration. Online and social media outlets were used to share an IRB-approved flier. The flier was posted to both the lab and study staff’s personal Twitter feeds (two of four staff were NHW), as well as personal and neighborhood Facebook pages. Neighborhood Facebook pages are based on geographic location and are only available to members of that area. The team was therefore limited to posting in their own neighborhoods. An advertisement with the flier was placed on Craigslist St. Louis. Advertisements were also placed on a local social media site, NextDoor, throughout several St. Louis metropolitan neighborhoods. Because of how NextDoor works with larger neighboring boundries, the team was able to place the postings about the study in the full metro area. Additionally, email newsletters with the flier were sent through Washington University’s Institute for Public Health. No cost was associated with creating the materials or to post/distribute the materials. The flier was posted for approximately two months on the different social media outlets.
Traditional media outlets were utilized, as well. Following an article in the university newsletter, a reporter from the local metro newspaper (St. Louis Post-Dispatch) interviewed two of the study investigators (G.M.B, C.M.R), as well as two engaged research participants, and subsequently ran a front-page, Sunday article about the study (link blinded). The reporter took two months to conduct the interviews and draft the article for publication. The Sunday distribution of the St. Louis Post-Dispatch is over 200k for print and over 18k for digital copies. There was no cost associated with publishing this front-page article. Furthermore, advertising space was purchased ($793.68 plus $250 for color) in the St. Louis American, a local weekly newspaper that focuses on the AA community. An advertisement using the flier we tailored to feature an older AA male driver was run on two occasions; however, placement was toward the back of the paper and was therefore not prominent. The Thursday distribution of the St. Louis American prints over 70k copies for over 845 distribution points and also is available online. Similar to the other methods, there was contact information for the research coordinator soliciting participant interest in the study.
Word-of-mouth or snowball sampling, also known as chain-referral sampling is a secondary source of participant referral. In this study, this was typically due to a referral from a person who is or was in the study previously and forwarded information about the study to another individual. As a result, we also examined whether interested participants originated from word-of-mouth/snowball sampling.
After initial interest was shown through a prospective participant’s phone call or email, testing was explained over the phone or by follow up email to participants. Participants were told that they would be asked to complete an annual clinical assessment, psychometric testing, driving evaluation, and sensory testing. A vehicle data logger would be installed in participant vehicles for monitoring of driving behaviors and driving patterns. At baseline, participants would be asked to complete a lumbar puncture for cerebrospinal fluid collection, structural magnetic resonance imaging (MRI), amyloid positron emission tomography (PET) scan, home sleep study, and blood draw for genetic testing.
During recruitment phone calls and emails, participants were asked about their contact information, address, demographics, vehicle make and model, and how they heard about the study. This information was kept in a secure spreadsheet. For participants who called or emailed for more information, but were not contacted, demographic data is not available. For analysis, demographic data by zip code was pulled from the 2010 census data (accessible via cdxtech.com).
Results
A total of 546 individuals contacted the study coordinator by phone or email. Of those, 394 were in response to a front-page featured article in the Sunday edition of the St. Louis Post-Dispatch, with nearly half of that subset calling during the first two days. Advertisements in the St. Louis American garnered 15 responses, social media (Facebook and NextDoor) 40 responses, university communications 12 responses, speaking engagements 19 responses (40-80 attendees per talk), and word-of-mouth/snowball sampling 66 responses. Twitter and Craigslist did not provide any interested individuals.
Further breakdown regarding recruitment from each source can be seen in Table 1. There were 81 NHW (83.5%) and 16 (16.5%) AA participant who enrolled across all referral sources. Demographics were available only for those who enrolled in the study, which can be seen in Table 2. AAs who enrolled came primarily from areas that had higher minority populations. AAs who enrolled were from zip codes that have an average of 68% minority population, and some came from areas that have up to 98% minority population. Similarly, NHW participants who enrolled came from areas that were, on average, 79% NHW, with some areas as much as 98% NHW. Both AA and NHW participants had, on average, a college degree, though AA education level was slightly lower than that of NHW.
Table 1.
Recruitment from all sources (n=546)
| Newly Enrolled Participants | |||||
|---|---|---|---|---|---|
| Non-Hispanic White | African American | Declined / No response* | Not processed* | Total | |
| St. Louis Post Dispatch | 43 (53.0%) | 4 (25.0%) | 175 | 172 | 394 |
| St. Louis American | 0 (0.0%) | 6 (37.5%) | 8 | 1 | 15 |
| Social media | 15 (18.5%) | 0 (0.0%) | 21 | 4 | 40 |
| University communication | 5 (6.2%) | 3 (18.8%) | 2 | 2 | 12 |
| Speaking engagements | 4 (4.9%) | 1 (6.2%) | 12 | 2 | 20 |
| Word-of-mouth /Snowball Sampling | 14 (17.3%) | 2 (12.5%) | 39 | 11 | 65 |
| Total | 81 (83.5%) | 16 (16.5%) | 257 | 192 | 546 |
Demographics not captured
Table 2.
Demographics of newly enrolled participants (n=97)
| Non-Hispanic White | African American | |
|---|---|---|
| Race, No. (%) | 81 (83.5) | 16 (16.5) |
| Gender | ||
| Women, No. (%) | 35 (36.1) | 12 (12.4) |
| Men, No. (%) | 46 (47.4) | 4 (4.1) |
| Education, mean (SD), y | 17.21 (2.68) | 16.08 (3.68) |
| Age, mean (SD), y | 73.09 (5.78) | 70.25 (3.77) |
| Zip code, mean (SD), %NHW | 79.27 (19.43) | 32 (25.48) |
Of the 546 individuals who contacted the study for more information, 192 were not contacted because enrollment goals were met for the study. Of the 354 individuals remaining, 72.6% either declined participation or did not respond to email responses or phone calls (Figure 1).
Figure 1:
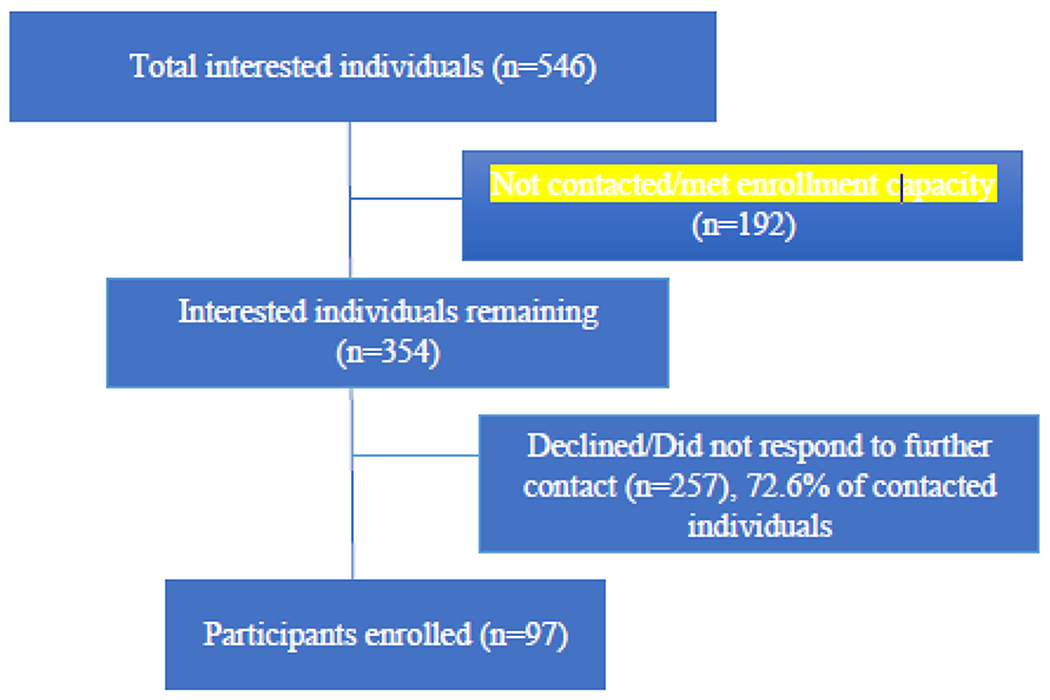
Participant recruitment, all sources.
Discussion
This case study retrospectively examined the effectiveness of traditional vs. social media materials on recruiting older adults into a study about preclinical AD and driving. Traditional print media (newspaper) seemed to elicit the most interest and attracted both NHW and AA individuals. Social media recruitment yielded mainly NHW individuals, while speaking engagements and word-of-mouth/snowball sampling were moderately successful with both groups. These findings highlight a number of important themes regarding strategies that may be effective for certain populations, challenges in recruitment of minority populations, and tailoring a multipronged approach for increasing participant recruitment.
Among adults age 65 or older, within the St. Louis Metro area (St. Louis City, as well as surrounding counties in both Missouri and Illinois) there are approximately four times the number of NHWs (~83%), compared to AAs (~14%) (Statistical Atlas, 2020a). Our recruitment effort was proportional compared to the racial breakdown in the metro area from which we drew participants. As mentioned, both AA and NHW participants averaged a college degree, as opposed to the St. Louis area, where approximately 17% of AA residents and 35% of NHW residents have a college degree or higher (Statistical Atlas, 2020b). Social media, in particular, appeared to be more successful with NHW individuals, as it yielded no enrollment of AA individuals. This difference is likely due to the social networks of the laboratory staff who shared the information with their own contacts and groups (two of four were NHW). The general newspaper article was successful in recruiting both NHWs and a small number of AAs, which is likely due to it being front page on a Sunday edition, having a targeted focus on recruiting for the specific study, including an interview of both an AA and NHW participant, and stressing the importance of aging and AD research. However, the targeted advertisement in the AA newspaper was particularly helpful in recruiting AAs into the study. Both newspaper advertisements highlight the importance of tailoring recruitment materials for the intended study population and being clear with the goal(s) of the study. Since this study sought older adults, study results suggest that the newspaper was the more effective source for soliciting participant likely due to their familiarity and use compared to social media.
Nearly three-quarters of individuals who inquired about the study proceeded to decline participation after learning details of the study or did not respond to email responses or phone calls. This study had a moderately high level of burden as it included brain imaging with radiotracers, cerebrospinal fluid collection, psychometric testing, a driving test, naturalistic driving GPS data collection, a home sleep study, and a clinical assessment that needed to include a collateral source attending with the participant. With all of these requirements being completed at multiple visits, not all interested individuals wanted to participate. AAs are nearly twice as likely to refuse participation in Alzheimer studies based on reluctance surrounding a lumbar puncture (Howell, et al. 2016). The reluctance in response to this burden is also reflected in the number of AA participants enrolled. Given the breadth of challenges recruiting AA older adults to aging studies, recruitment efforts are further exacerbated by requiring biomarkers, psychometric and clinical testing, and additional assessments of driving. These issues are documented in several recent editorials and perspective articles (Babulal, et. al., 2019; Barnes, 2019; Gilmore-Bykovskyi, et. al., 2019). Additionally, recruitment requires a large amount of staff time and resources committed, along with ongoing monitoring. Not all interested individuals were able to be contacted during this period due to the high number of inquiries. To mitigate these challenges, recruitment efforts should be included in the budget, and staff should plan to use a large amount of time during the recruitment period on outreach and advertising.
Social media was a useful, no-cost and low-effort method of engaging a number of individuals into the research. According to Pew Research Center, 40% of adults age 65 or older report using at least one social media site compared to 90% of young adults age 18-29 and 69% of middle age adults (age 50-64) (Pew Research Center, 2019). However, the overall reach of social media in this population may be limited. The advertisement in the general newspaper was free, while the advertisement in the AA newspaper was over $1000, yet it only yielded a fraction of overall interested participants. Furthermore, while there were huge benefits of a well-placed newspaper article, multiple avenues of recruitment were necessary to bring in a diverse group of participants. Recruitment should combine multiple efforts, which could include targeted speaking engagements in communities with a high AA population, collaborating with community partners, as well as additional advertisements in AA newspapers. The overall.
Some limitations of this study must be acknowledged. First, this is a case study of one study’s experience in recruitment, but was not a scientific study designed to compare recruitment methods nor which methods were more effective for NHWs and AAs. Future research targeting recruitment of racial and ethnically diverse samples must start with a comprehensive recruitment plan, timeline, and goals for any prospective study. For example, in terms of social media, AAs are more likely to use Instagram than Facebook or Twitter (Edison Research, 2019), and therefore, a focus on Instagram might have been more useful. Attention should be paid to recruiting samples with a range of socioeconomic status (SES) but more consideration and inclusion of participants from lower SES backgrounds and lower education levels. Both of these groups might be better targeted for inclusion with more focus on continuous community outreach. Often times, these participants are working fulltime and/or multiple jobs, which may not be conducive to traditional testing schedules. Therefore, adaptive testing in the evenings and weekends may help to improve enrollment. Due to the method of contact and IRB regulation on data capture for enrolled participants, demographic information is not available for participants who did not receive a full follow up call. This information would have better informed us about the full extent of the outreach efforts and distribution across races. Finally, our outreach team has only one AA advisor, and there were no AA laboratory members providing outreach in the community or fielding calls from prospective participants, which may have impacted the number of AA participants recruited.
It is also important to note that this study took place in St. Louis, Missouri, where the National Association for the Advancement of Colored People (NAACP), whose mission includes eliminating race-based discrimination, declared a travel advisory for African Americans (NAACP, 2017) beginning in August 2017. The advisory was based on statistics which showed that African Americans were 75% more likely in 2016 (NAACP, 2017), 85% more likely in 2017 (Kansas City Star Editorial Board, 2019), and 91% more likely in 2019 (Lou, 2019) to be stopped by law enforcement. According to the Missouri NAACP president, Nimrod Chapel, Jr., the advisory remains in place as of this writing (Kansas City Star Editorial Board, 2019). Recent work suggests there is a disproportionate number of older adult AA participants in longitudinal AD studies (Morris, et. al., 2019). The social and political environment in the state may influence how willing AA older adults might be to participate in driving research. Additionally, AAs are more likely to live in a home without a vehicle and to use public transportation. In 2015, 19.7% of AAs reported living in a household without access to a vehicle, while for NHWs this was only 6.5% (National Equity Atlas, 2020). Similarly, in urban areas, 34% of AAs report using public transportation daily or weekly, while the number is only 14% for NHWs (Pew, 2020). This climate, coupled with the historical mistrust secondary to research misconduct and inadequate human protection for human subjects, likely contribute to the overall reduced number of AA participants. Recent traffic tickets or being pulled over while driving will both be examined in the study. Future work should also look at history of law enforcement stops, stress around these experiences, and how this impacts driving in older adults.
Along with the limitations discussed above, it is important to consider how participants will be retained once they enroll. This study team encountered a number of participants who enrolled but subsequently failed to fulfill all study requirements or return for follow up. In the 18 months following our initial recruitment period, fourteen of our 97 new enrollees have left the study. Of those fourteen, eight are AA individuals, which is half of the sixteen AA participants enrolled. These participants left the study for a number of reasons, but the majority had the perception was that the study burden was too high, stating that they either did not have enough time or did not want to undergo the biomarker testing (lumbar puncture or amyloid PET scan). Future work needs to look at how participants, particularly AAs, can best be retained.
Prospective studies recruiting older adults should spend significant time on a detailed and multistage recruitment plan, along with a timeline, and sufficient budget to support traditional print costs (e.g. newspaper, fliers, newsletter), graphic design (logo, online advertisement), and speaking engagements (food, drinks, honorariums). Outreach and recruitment should combine both traditional and social media to increase the range for eliciting interested participants. Word-of-mouth or snowball sampling is an often overlooked source where individual may recommend the study to others family and friends. Researchers may consider selecting participants willing to talk about their experiences as ambassadors. More importantly, studies seeking a diverse participant pool (i.e. inclusion of ethnoracial minorities) need to tailor materials to the needs of the particular community, collaborate with community leaders, and invest time in the relationships to improve recruitment success. Finally, it is important collect demographic data on all interested individuals, connect with each individual who calls/emails, and analyze trends to inform whether the recruitment plan remains the same or needs to adjust.
Acknowledgments
Funding for this study was provided by the National Institute on Aging [R01-AG056466, R01-AG043434, R03-AG055482]. The authors thank the participants, investigators/staff of the Knight ADRC Clinical, Biomarker, Genetics and Neuroimaging Cores, and the investigators/staff of the Driving Performance in Preclinical Alzheimer’s Disease study.
Funding: Funding for this study was provided by the National Institute on Aging [R01-AG056466, R01-AG043434, R03-AG055482, P50-AG05681, P01-AG03991, P01-AG026276, R01AG057680, R01MH118031, R01AG052550]; Fred Simmons and Olga Mohan, the Paula and Rodger O. Riney Fund, the Daniel J Brennan MD Fund, and the Charles and Joanne Knight Alzheimer’s Research Initiative of the Washington University Knight Alzheimer’s Disease Research Center (ADRC).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Alzheimer’s Association. (2019a). 2019 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 15(3), 321–387. [Google Scholar]
- Alzheimer’s Association. (2019b). Alzheimer’s Association grant opportunities. Retrieved from https://www.alz.org/research/forresearchers/grants/types-of-grants
- Babulal G, Traub C, Webb M, Stout S, Addison A, Carr D, Ott B, Morris J, & Roe C (2016). Creating a driving profile for older adults using GPS devices and naturalistic driving methodology 5(2376). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babulal GM, Quiroz YT, Albensi BC, Arenaza-Urquijo E, Astell AJ, Babiloni C, Bahar-Fuchs A, Bell J, Bowman GL, Brickman AM, Chetelat G, Ciro C, Cohen AD, Dilworth-Anderson P, Dodge ΗH, Dreux S, Edland S, Esbensen A, Evered L, Ewers M, Fargo KN, Fortea J, Gonzalez H, Gustafson DR, Flead E, Flendrix JA, Flofer SM, Johnson LA, Jutten R, Kilborn K, Lanctot KL, Manly JJ, Martins RN, Mielke ΜM, Morris MC, Murray ΜE, Oh ES, Parra MA, Rissman RA, Roe CM, Santos OA, Scarmeas N, Schneider LS, Schupf N, Sikkes S, Snyder ΗM, Sohrabi HR, Stern Y, Strydom A, Tang Y, Terrera GM, Teunissen C, Melo van Lent D, Weinborn M, Wesselman L, Wilcock DM, Zetterberg H, & O’Bryant SE (2019). Perspectives on ethnic and racial disparities in Alzheimer’s disease and related dementias: Update and areas of immediate need. Alzheimer’s & Dementia, 15(2), 292–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes LL (2019). Biomarkers for Alzheimer dementia in diverse racial and ethnic minorities—a public health priority. JAMA neurology, 76(3), 251–253. [DOI] [PubMed] [Google Scholar]
- Epps F, Skemp L, & Specht J (2015). Using culturally informed strategies to enhance recruitment of african americans in dementia research: A nurse researcher’s experience. Journal of Research Practice, 11(1), 1–19. [Google Scholar]
- Edison Research. (2019). The social habit 2019. Retrieved from https://www.edisonresearch.com/the-social-habit-2019/
- Ford ΜE, Siminoff LA, Pickelsimer E, Mainous AG, Smith DW, Diaz VA, Soderstrom LH, Jefferson MS, & Tilley BC (2013). Unequal burden of disease, unequal participation in clinical trials: Solutions from African American and Latino community members. Health and Social Work, 38(1), 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore-Bykovskyi AL, Jin Y, Gleason C, Flowers-Benton S, Block LM, Dilworth-Anderson P, ... & Zuelsdorff M (2019). Recruitment and retention of underrepresented populations in Alzheimer’s disease research: A systematic review. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 5, 751–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham LA, Ngwa J, Ntekim O, Ogunlana O, Wolday S, Johnson S, Johnson M, Castor C, Fungwe TV, & Obisesan TO (2018). Best strategies to recruit and enroll elderly Blacks into clinical and biomedical research. Clinical Interventions in Aging, 13, 43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill CV, Perez-Stable EJ, Anderson NA, & Bernard MA (2015). The National Institute on Aging Health Disparities Research Framework. Ethnicity & disease, 25(3), 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell JC, Parker MW, Watts KD, Kollhoff A, Tsvetkova DZ, Hu WT (2016). Research lumbar punctures among African Americans and Caucasians: Perception precicts experience. Frontiers in Aging Neuroscience, 8, 296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James DC, Harville C, Sears C, Efunbumi O, & Bondoc I (2017). Participation of African Americans in e-Health and m-Health Studies: A Systematic Review. Telemedicine and e-Health, 23(5), 351–364. [DOI] [PubMed] [Google Scholar]
- Kansas City Star Editorial Board. (2019, May 2). Parson has opportunity — and experience — to show leadership on NAACP travel advisory, Editorial. Kansas City Star; Retrieved from https://www.kansascity.com/opinion/editorials/article229926319.html [Google Scholar]
- King DB, O’Rourke N, & De Longis A (2014). Social media recruitment and online data collection: A beginner’s guide and best practices for accessing low-prevalence and hard-to-reach populations. Canadian Psychology, 55(4), 240–249. [Google Scholar]
- Lou M (2019). Black drivers in Missouri are 91% more likely to be stopped than white drivers, a report finds. CNN. Retrieved from https://www.cnn.com/2019/06/11/us/missouri-traffic-stops-black-drivers-trnd/index.html [Google Scholar]
- Miller EG, Nowson CA, Dunstan DW, Kerr DA, Solah V, Menzies D, & Daly RM (2016). Recruitment of older adults with type 2 diabetes into a community-based exercise and nutrition randomised controlled trial. Trials, 17(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC (1993). The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology, 43(11), 2412–2414. [DOI] [PubMed] [Google Scholar]
- Morris JC, Schindler SE, McCue LM, Moulder KL, Benzinger TL, Cruchaga C, Fagan AM, Grant E, Gordon BA, Holtzman DM, & Xiong C (2019). Assessment of racial disparities in biomarkers for Alzheimer disease. JAMA neurology, 76(3), 264–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NAACP. (2017). Travel Advisory for the State of Missouri Retrieved from https://www.naacp.org/latest/travel-advisory-state-missouri/
- National Equity Atlas. (2020). Car Access. Retrieved from https://nationalequityatlas.org/indicators/Caraccess
- NIH. (2015). Health Disparities and Alzheimer’s Disease (R01), PAR-15–349. Retrieved from https://grants.nih.gov/grants/guide/pa-files/PAR-15-349.html
- Pew Research Center. (2019). Social Media Fact Sheet. Retrieved from https://www.pewresearch.org/internet/fact-sheet/social-media/
- Pew Research Center. (2020). Who relies on public transit in the US. Retrieved from https://www.pewresearch.org/fact-tank/2016/04/07/who-relies-on-public-transit-in-the-u-s/
- Randolph S, Coakley T, & Shears J (2018). Recruiting and engaging African-American men in health research. Nurse researcher, 26(1), 30–34. [DOI] [PubMed] [Google Scholar]
- Roe CM, Babulal GM, Head DM, Stout SH, Vernon EK, Ghoshal N, Garland B, Barco PP, Williams ΜM, Johnson A, Fierberg R, Fague MS, Xiong C, Mormino E, Grant EA, Holtzman DM, Benzinger TLS, Fagan AM, Ott BR, Carr DB, & Morris JC (2017a). Preclinical Alzheimer’s disease and longitudinal driving decline. Alzhelmers Dement (N Y), 3(1), 74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roe CM, Barco PP, Head DM, Ghoshal N, Selsor N, Babulal GM, Fierberg R, Vernon EK, Shulman N, Johnson A, Fague S, Xiong C, Grant EA, Campbell A, Ott BR, Holtzman DM, Benzinger TL, Fagan AM, Carr DB, & Morris JC (2017b). Amyloid Imaging, Cerebrospinal Fluid Biomarkers Predict Driving Performance Among Cognitively Normal Individuals. Alzheimer DIs Assoc Disord, 31(1), 69–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistical Atlas. (2020a). Race and ethnicity in the St. Louis area (Metro Area). Retreived from https://statisticalatlas.com/metro-area/Missouri/St-Louis/Race-and-Ethnicity
- Statistical Atlas. (2020b). Educational Attainment in the St. Louis Area. Retrieved from https://statisticalatlas.com/metro-area/Missouri/St-Louis/Educational-Attainment
- US Census Bureau. (2018). Population estimates, V2018. Retrieved from https://www.census.gov/quickfacts/fact/table/US/PST045218
- Williams ΜM, Meisel ΜM, Williams J, & Morris JC (2011). An interdisciplinary outreach model of African American recruitment for Alzheimer’s disease research. Gerontologist, 51(SUPPL. 1), S134–S141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MM, Scharff DP, Mathews KJ, Hoffsuemmer JS, Jackson P, Morris JC, & Edwards DF (2010). Barriers and facilitators of African American participation in Alzheimer disease biomarker research. Alzheimer Disease and Associated Disorders, 24(SUPPL. 1), S24–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]


