Abstract
Background:
The optimal surgical treatment for scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) remains unclear. To inform clinical decision-makers, we conducted a cost-effectiveness analysis comparing proximal row carpectomy (PRC) and four-corner arthrodesis (FCA).
Methods:
A Markov microsimulation model was used to compare clinical outcomes, costs, and health utilities between PRC and FCA. The model used a 10-year time horizon and a 1-month cycle length, and it was evaluated from the societal perspective. Utilities and clinical parameters including transition probabilities for debridement for infection, removal of implants, conversion to total wrist arthrodesis, revision FCA, and revision total wrist arthrodesis were obtained from published literature. Timing of complications was estimated from the literature. Direct medical costs were derived from Medicare ambulatory surgical cost data, and indirect costs for missed work due to surgical procedures and complications were included. The effectiveness outcome was quality-adjusted life years (QALYs). Probabilistic sensitivity analysis and 1-way threshold analysis for utilities were performed.
Results:
In the base-case model, PRC dominated FCA (i.e., PRC had lower cost and greater effectiveness). The mean (and standard deviation) for the total cost and QALYs per patient were $30,970 ± $5,931 and 8.24 ± 1.28, respectively, for PRC and $44,526 ± $11,205 and 8.23 ± 1.26, respectively, for FCA. In the probabilistic sensitivity analysis, PRC dominated FCA in 57% of the 1 million iterations. The cost-effectiveness acceptability curve indicated that PRC is the most cost-effective strategy regardless of the willingness-to-pay threshold up to $100,000/QALY.
Conclusions:
PRC dominated FCA in the base-case analysis and in the probabilistic sensitivity analysis. These results suggest that PRC is the optimal strategy for Stage-I or II SLAC and for SNAC in patients ≥55 years of age.
Level of Evidence:
Economic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Emphasis on health-care costs has grown over the past decade in the U.S., in part because of policy changes that have included value-based payment models1,2. For patients with Stage-I or II scapholunate advanced collapse (SLAC) or scaphoid nonunion advanced collapse (SNAC) arthritis for whom motion-sparing surgery is indicated, the optimal treatment remains unclear3 and has traditionally included either proximal row carpectomy (PRC) or four-corner arthrodesis (FCA)4,5. Because SLAC arthritis is the most common form of wrist degenerative arthritis6, defining the optimal surgical treatment would be an important step in improving patient outcomes while minimizing costs.
Clinical outcomes, or health states or utilities, are integral in determining the cost-effectiveness of a given treatment. Numerous studies have assessed the clinical outcomes of PRC and FCA3,6-22. Two systematic reviews of PRC and FCA outcomes did not identify any differences in patient-reported disability, subjective ratings of satisfaction, rate of conversion to total wrist arthrodesis, or increase in grip strength7,8. Despite these findings and reports that both PRC and FCA can be associated with the development of radiographic evidence of arthrosis at long-term follow-up6,23, some authors have stated that FCA may provide a more desirable result6,24-27. It is clear that controversy exists with regard to which surgery yields a superior clinical result.
Literature related to the direct and indirect costs of PRC and FCA is limited. In one report, the surgical encounter direct costs for FCA were 425% greater than those for PRC28. Similarly, a large database study indicated that cumulative surgical costs for PRC were significantly less than those for FCA ($7,171 versus $10,842) when postoperative costs of complications were included29.
Despite this prior literature, the optimal surgical treatment for patients with Stage-I or II SLAC or SNAC remains in question. The purpose of this study was to perform a cost-effectiveness analysis comparing PRC with FCA using a Markov microsimulation model from the societal perspective to determine the optimal treatment strategy.
Materials and Methods
Overview
This cost-effectiveness analysis was performed in accordance with the recommendations of the Second Panel on Cost-Effectiveness in Health and Medicine30. We used a Markov simulation model to estimate the effectiveness and cost-effectiveness of PRC and FCA in patients with SLAC or SNAC wrist arthritis31-33. The model, which had a cycle length (period of time in which patients may transition from one health state to another, or remain in the same health state) of 1 month, was evaluated from a societal perspective over a 10-year time horizon in a modeled population of 10,000 hypothetical 55-year-old patients. A 10-year time horizon was chosen because robust clinical postoperative data are lacking beyond this time frame in the literature, which precludes accurate calculation of long-term complication probabilities29,34. Both treatments were evaluated with respect to both effectiveness and cost. The effectiveness measure was quality-adjusted life years (QALYs), which encompass both duration and quality of life. Costs included those related to surgical treatment and associated care as well as indirect costs for each patient from the time of the initiation of treatment until death or the end of the 10-year time horizon (whichever occurred first).
Model Structure
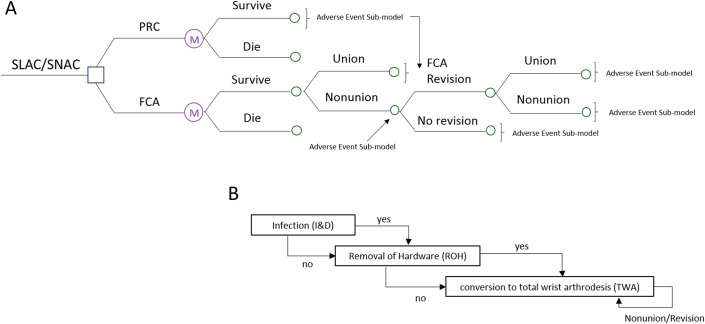
Figure 1-A depicts the Markov model structure. Patients were assigned a probability of survival status based on average mortality rates provided by the U.S. Social Security Administration in 201535. Patients who underwent FCA or total wrist arthrodesis had the potential to experience nonunion, which could lead to revision surgery. In addition, each surviving patient could experience adverse events associated with their treatment as depicted in Figure 1-B. Adverse-event probabilities were estimated from weighted averages of values reported in published clinical reports (Table I). Outcomes from the model included costs and QALYs. Both costs and utilities were discounted 3% annually. The model was programmed in TreeAge Pro 2018 (TreeAge Software).
Fig. 1.
Illustration of the structure of the Markov model (Fig. 1-A) and the adverse event submodel (Fig. 1-B). I&D = irrigation and debridement. The circled “M” refers to “Markov node,” which signifies that the cycle repeats itself (in this case, the cycle repeats itself monthly for the duration of the simulation period of 10 years).
TABLE I.
Cost and Probability Input Data for the Markov Model
| Event | Value | SD | Source |
| Lifetime probabilities | |||
| PRC* | |||
| Infection requiring irrigation and debridement | 0.30% | 0.50% | Literature3,18,33,34,36 |
| Removal of implants | 0.00% | 0.00% | Literature29,34 |
| Total wrist arthrodesis | 6.20% | 4.90% | Literature3,9,18,22,23,29,34,36-39 |
| Nonunion/total wrist arthrodesis revision† | 5.00% | 4.00% | Literature41-45,53 |
| FCA | |||
| Infection requiring irrigation and debridement | 2.20% | 4.30% | Literature3,18,34,36 |
| Removal of implants | 34.30% | 12.60% | Literature27,29,34,53,54 |
| Total wrist arthrodesis | 16.80% | 5.80% | Literature3,9,18,19,22,27,29,34,36-38 |
| Nonunion‡ | 12.90% | 10.10% | Literature19,36 |
| Revision FCA | 4.60% | 1.20% | Literature9,18,27,29,36 |
| Nonunion/total wrist arthrodesis revision† | 5.00% | 4.00% | Literature41-45,53 |
| Costs | |||
| Surgical | |||
| PRC | $7,069 | $3158 | Medicare46,47 |
| FCA | $12,119 | $7198 | Medicare46,47 |
| FCA revision | $12,119 | $7198 | Medicare46,47 |
| Infection requiring irrigation and debridement | $7,068 | $3519 | Medicare46,47 |
| Removal of implants | $6,840 | $3575 | Medicare46,47 |
| Total wrist arthrodesis | $8,893 | $5469 | Medicare46,47 |
| Total wrist arthrodesis revision | $8,893 | $5469 | Medicare46,47 |
| Indirect costs | |||
| Average median weekly earnings in 2013 | $776.5 | — | Bureau of Labor Statistics48 |
| Labor force rate (2013) | 60.4% | — | Bureau of Labor Statistics55 § |
| PRC | |||
| Missed days of work | $10,095 (3 mo) | — | Literature13,36/Bureau of Labor Statistics48 |
| Rate of return to work | 92.4% ($256/mo) | — | Literature3,9,11,13,15,19,23,37 |
| FCA | |||
| Missed days of work | $10,095 (3 mo) | — | Literature13,36/Bureau of Labor Statistics48 |
| Rate of return to work | 90.8% ($310/mo) | — | Literature3,9,13,15,19,27,53 |
| Irrigation and debridement | |||
| Missed days of work | $1,553 (2 wk) | — | Expert opinion/Bureau of Labor Statistics48 |
| Removal of implants | |||
| Missed days of work | $1,553 (2 wk) | — | Expert opinion/Bureau of Labor Statistics48 |
| Total wrist arthrodesis | |||
| Missed days of work | $9,303 (12.0 ± 2.7 wk) | — | Literature40-45,56/Bureau of Labor Statistics48 |
| Rate of return to work | 85.0% ($506/mo) | — | Literature40-44,56 |
No references describing revision PRC were identified; therefore, this potential scenario was not included as a possible complication.
This refers to the scenario of nonunion after total wrist arthrodesis for which a revision total wrist arthrodesis is performed.
This refers to nonunion after an index FCA.
The data were acquired by choosing the “Labor force” link followed by a customized search with the following parameters: both sexes, all races, all Hispanic or Latino or other origins, age 55 to 64 years, all education levels, all marital statuses, and civilian labor force participation rate for “labor force status.”
Input Parameters
A PubMed and Google Scholar search was performed using the keywords “four corner arthrodesis,” “proximal row carpectomy,” “total wrist arthrodesis,” “SLAC” or “scapholunate advanced collapse,” and “SNAC” or “scaphoid nonunion advanced collapse.” An additional query using the term “fusion” in place of “arthrodesis” was also performed, as applicable. Articles were reviewed, and those involving index surgical procedures for treatment of other disease processes and those that did not report rates of complications or return to work were excluded. Complication rates, reoperation rates, and rates of conversion to total wrist arthrodesis were extracted from the remaining articles. Articles that included appropriate data were reviewed for bibliographic citations related to the above keywords in a secondary search for complication and return-to-work rates. Data from 11 reports were used to define complication rates for PRC3,9,18,22,23,29,34,36-39, and 17 were used for FCA complication rates3,9,18,19,22,27,29,34,36-38,40-45 (Table I). One of these sources was a published abstract that contained data on the timing of complications following the index surgical procedures34. Weighted averages and standard deviations (SDs) were calculated for the following complications of PRC and FCA: infection requiring irrigation and debridement, removal of implants, revision, conversion to total wrist arthrodesis, nonunion after FCA, and revision after FCA (Table I). Weighted averages and SDs were calculated for revision total wrist arthrodesis, missed days of work, and likelihood of returning to any form of work following PRC, FCA, and total wrist arthrodesis. Given a lack of available data, we assumed that the rates of return to work following revision FCA or revision total wrist arthrodesis were identical to those following their respective index procedures.
Kaplan-Meier data from a study utilizing national Veterans Health Administration (VHA) Corporate Data Warehouse (CDW) data were used to populate the model with input parameters describing the timing of specific complications following PRC and FCA (Table II)34. The timing of total wrist arthrodesis following index PRC and FCA and the timing of other complications requiring surgery (irrigation and debridement, removal of implants, or revision FCA) were derived from this report or from the expert opinion of 2 board-certified hand orthopaedic surgeons for missing parameters. These input parameters describing the timing of complications were then assessed using sensitivity analysis.
TABLE II.
Time Frame for Adverse Event Input Data for the Markov Model
| Time Frame (mo) | Source* | |
| PRC | ||
| Infection requiring irrigation and debridement | 0-3 | Expert opinion |
| Total wrist arthrodesis | 6-232 | VHA CDW34 |
| Total wrist arthrodesis nonunion | 0-3 | Expert opinion |
| FCA | ||
| Infection requiring irrigation and debridement | 0-3 | Expert opinion |
| Removal of implants | 3-137 | VHA CDW34 |
| Total wrist arthrodesis | 6-162 | VHA CDW34 |
| FCA revision | 6-12 | Expert opinion |
| FCA nonunion | 6-12 | Expert opinion |
| Total wrist arthrodesis nonunion | 6-12 | Expert opinion |
VHA CDW = Veterans Health Administration Corporate Data Warehouse.
We assumed that irrigation and debridement for infection would not occur beyond 3 months following the index surgical procedures. We also assumed that revision FCA or revision total wrist arthrodesis due to total wrist arthrodesis nonunion would not occur until 6 months following the index surgery, to allow for a period of waiting for union to occur, and not beyond 12 months following the index surgery. Patients could not have multiple instances of the same complication (irrigation and debridement or removal of implants) following the index surgery or following revision FCA. A single surgical revision was possible following the index FCA and for nonunion after total wrist arthrodesis. The model did not allow for revision PRC given the absence of published rates of this potential complication. We also assumed that no patient had removal of implants following PRC.
Costs
Costs related to ambulatory index surgical procedures and for surgical procedures related to complications were calculated as the sum of Medicare surgeon, anesthesia, and facility payments obtained through a query of respective Current Procedural Terminology (CPT) codes (see Appendix 1). Average 2016 Medicare standardized payments were used for surgeon costs46, and ambulatory facility and anesthesia costs were obtained from the 2013 Florida State Ambulatory Surgery and Services Database (SASD)47. Surgical procedures and anesthesia services were identified by CPT code. For surgical procedures with >1 applicable CPT code, weighted averages for surgeon and facility costs were calculated and used in the model. Indirect costs were also included in the total cost of surgical procedures and complications, and were calculated as loss of income from estimates of missed work and the likelihood of returning to any form of work following surgical procedures as determined from published data or expert opinion (Table I). These estimates were multiplied by the average median earnings reported by the U.S. Bureau of Labor Statistics (BLS) for full-time wage and salary workers ($776.50/week in 2013 U.S. dollars)48. Total indirect costs of missed days of work or those associated with each surgical procedure/complication were added at the time of occurrence, taking into consideration BLS estimates of the percentage of patients in the work force by age. Monthly indirect costs of unemployment were added every month after the event happened until death or the end of the study cycle, whichever occurred first, since the remaining years differed from subject to subject in the model. We assumed that the surgical encounter costs for a revision of an FCA or a total wrist arthrodesis were the same as those for an initial FCA or total wrist arthrodesis, as revision-specific CPT codes do not exist. All costs were adjusted to 2013 U.S. dollars using the Personal Consumption Expenditures price index for health-care services. Due to a lack of values in the literature, we assumed that patients would be out of work for 2 weeks following irrigation and debridement or removal of implants. We also assumed that the time off from work would be equivalent for revision and index FCA and be equivalent for revision total wrist arthrodesis and total wrist arthrodesis.
Utilities
Effectiveness was measured in QALYs. Utility was measured on a scale on which 1.0 represented a state of perfect health and 0.0 represented death. Utility estimates for PRC and FCA with and without complications, and disutility of complications including total wrist arthrodesis, were obtained from a published study (Table III)49. The disutility of nonunion or revision following total wrist arthrodesis and the disutility of nonunion or revision following FCA were determined using these previously published utilities and by expert opinion. The disutility of irrigation and debridement or removal of implants was subtracted from the baseline utility at the time at which a patient underwent the procedure; this disutility persisted for 1 cycle (1 month), after which the pre-complication utility was reapplied. The disutility of total wrist arthrodesis, nonunion following total wrist arthrodesis, or a second FCA nonunion were permanently deducted from the premorbid utility.
TABLE III.
Annual Utility Input Data for the Markov Model
| Utility/Disutility | Utility/Disutility Value | Source |
| Utility for healthy state | ||
| PRC | 0.99 | Literature49 |
| FCA | 0.99 | Literature49 |
| Disutility for PRC | ||
| Infection requiring irrigation and debridement | −0.002 | Literature49 |
| Total wrist arthrodesis/total wrist arthrodesis revision | −0.02 | Expert opinion/literature49 |
| Total wrist arthrodesis nonunion | −0.002 | Expert opinion/literature49 |
| Disutility for FCA | ||
| Infection requiring irrigation and debridement | −0.008 | Literature49 |
| Removal of implants | −0.008 | Literature49 |
| Total wrist arthrodesis/total wrist arthrodesis revision | −0.02 | Expert opinion/literature49 |
| Total wrist arthrodesis nonunion | −0.008 | Expert opinion/literature49 |
| FCA revision | −0.03 | Expert opinion/literature49 |
| FCA nonunion | −0.006 | Expert opinion/literature49 |
Mortality
The mortality rate was obtained from the 2015 Social Security Area Population Life Tables and averaged between sexes35. An age-dependent mortality rate was applied in an identical manner for FCA and PRC, and it was not modified based on a subject experiencing a postoperative complication.
Sensitivity Analysis
One-way and probabilistic sensitivity analyses were performed as described in Appendix 2.
Results
Base Case
Base case analysis revealed 10-year mean total costs (and SDs) of $30,970 ± $5,931 for PRC and $44,526 ± $11,205 for FCA (Table IV). PRC yielded 8.24 ± 1.28 QALYs versus 8.23 ± 1.26 QALYs for FCA. Overall, PRC was $13,556 less costly and added 0.0104 QALY per patient compared with FCA. PRC was considered the dominant treatment strategy as it yielded lower costs and higher QALYs than FCA.
TABLE IV.
Cost-Effectiveness Analysis Results for Base Case
| Procedure | Mean Cost ± SD (2013$) |
Incremental Cost (2013$) | Mean Effect ± SD (QALYs) |
Incremental Effect (QALYs) | ICER ($/QALY) |
| PRC | $30,970 ± $5,931 | $0 | 8.2412 ± 1.2771 | 0.0000 | $0 |
| FCA | $44,526 ± $11,205 | $13,556 | 8.2308 ± 1.2594 | −0.0104 | −$1,301,322 |
Threshold Analysis on Utility Values
Threshold analyses demonstrated that our model was robust to utility or disutility parameter values (e.g., the conclusion was not reversed by changing these inputs over a wide range). The model switches from PRC being cost-effective to being not cost-effective at an incremental cost-effectiveness ratio (ICER) of $100,000/QALY if the utility of PRC is reduced to <0.97.
Probabilistic Sensitivity Analysis
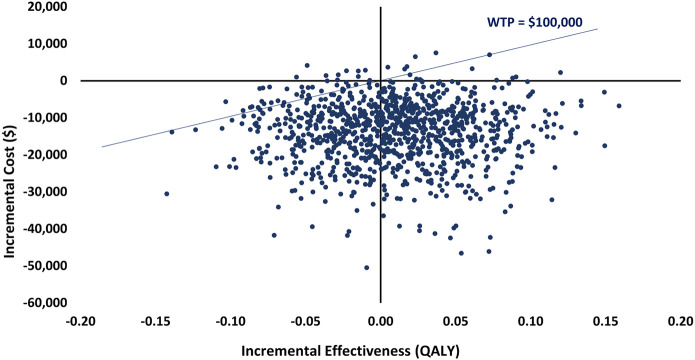
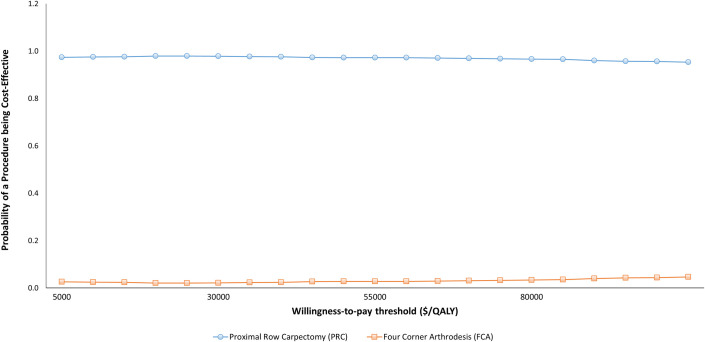
Probabilistic sensitivity analysis demonstrated that PRC dominated FCA in 57% of the 1 million iterations (Fig. 2). At a willingness-to-pay threshold of $100,000/QALY, PRC was cost-effective compared with FCA in 61% of the iterations. The cost-effectiveness acceptability curve indicates that PRC was the most cost-effective strategy regardless of the willingness-to-pay threshold up to $100,000/QALY (Fig. 3).
Fig. 2.
Scatterplot showing the distribution of incremental costs and incremental effectiveness of individual iterations of the probabilistic sensitivity analysis comparing the cost-effectiveness of PRC versus FCA for patients with SLAC or SNAC. The diagonal line represents a willingness-to-pay (WTP) threshold of $100,000 per QALY. Data points to the right and below this line indicate that PRC was considered cost-effective compared with FCA according to the WTP threshold.
Fig. 3.
Cost-effectiveness acceptability curve showing the change in the probability of cost-effectiveness of PRC and FCA treatment strategies over a range of willingness-to-pay threshold values.
Discussion
The main study finding was that PRC dominated FCA. In other words, PRC yielded better outcomes measured by QALYs and cost less than FCA. However, since the difference in QALYs was small, the main difference is decreased costs and rates of complications after PRC. Based on probabilistic sensitivity analysis, these findings were robust to variations in rates of complications or return to work as well as costs of index and subsequent surgical procedures. These findings were also robust to the utilities for PRC and FCA, as threshold sensitivity analysis demonstrated that the utility of PRC would have to drop from 0.99 to <0.97 in order to reverse this conclusion. Given the utility of 0.99 for FCA without complications, a utility of <0.97 for PRC without complications is unlikely given an abundance of research suggesting that the clinical outcomes of PRC and FCA are similar7,8. This utility threshold is also relatively low when considering that disutilities for complications following FCA are on the order of −0.006 for a nonunion to −0.02 for a total wrist arthrodesis49. Therefore, we conclude that PRC is the preferred treatment strategy for patients ≥55 years of age who have Stage-I or II SLAC or SNAC of the wrist.
Our findings differ slightly from a prior cost-effectiveness analysis by Daar et al., who concluded that FCA with successful screw fixation dominated PRC, FCA with plate fixation, and FCA with Kirschner-wire fixation50. Those authors also concluded that FCA with screw fixation and PRC were both cost-effective treatment strategies for SLAC and SNAC of the wrist, whereas the other 2 strategies were not cost-effective. However, their literature review was restricted to studies reporting FCA fixation types. This led to the exclusion of the article by Rahgozar et al.29, who observed a significantly greater rate of conversion to total wrist arthrodesis after FCA than after PRC in a commercial database study that included more patients (3,388) than all of the clinical reports combined used in the current study to extract complication rates. Therefore, the majority of patients in the reported literature were excluded from the study by Daar et al., which would introduce a bias in favor of FCA over PRC. Additionally, utilities that were derived using hand surgeons’ opinions in the study by Daar et al. warrant further evaluation. In contrast to published reports (including 2 systematic reviews7,8) suggesting no clinically relevant differences in functional outcomes between PRC and FCA3,9,18, the utility that Daar et al. calculated for a successful FCA with screw fixation was greater than that for PRC (0.81 and 0.78, respectively). Also, the utilities for patients with complications following PRC or FCA—including those in the range of 0.50 to 0.53 for total wrist arthrodesis—may be unrealistically low compared with previously reported utilities for wrist arthritis surgical procedures and their sequelae (≥0.90)49 and in light of published utilities in the range of 0.48 to 0.58 for end-stage congestive heart failure51 and approximately 0.55 for metastatic lung cancer52. It is improbable that a wrist condition should yield a health state as low as that associated with terminal diseases.
Limitations of the current study deserve mention. The literature lacks comprehensive long-term comparative data on outcomes, complication rates, and rates of conversion to total wrist arthrodesis after PRC and FCA. As a result, we restricted our study to a 10-year time period. However, it is possible that the addition of long-term data, should it be published in the future, could affect our results. Although inclusion of complications data from a large commercial database study29 provides information from thousands of patients potentially not included in other published clinical reports, our results may still be sensitive to publication bias—published results may not reflect the true results of PRC, FCA, or total wrist arthrodesis. The literature lacks granular detail on some of the model inputs such as the number of missed days of work following irrigation and debridement or removal of implants, and values assigned to these scenarios on the basis of expert opinion may be debatable. Although a prior comparison of PRC and FCA in young patients (<45 years old)18 showed similar outcomes, it is unclear if our results could be generalized to young patients as most of our complication data were derived from patients ≥55 years of age. Although several methods for determining utilities have been described, we utilized previously published utilities that did not account for the potential for disutility during recovery from PRC, FCA, or total wrist arthrodesis49. Although the 1-way sensitivity analysis suggests that our findings are relatively robust to the index surgery utilities, it is possible that alternative methods for utility calculation could affect our results. The union rate for FCA differs according to the method of fixation, as highlighted by Daar et al.50, and our analysis is limited in that it did not account for fixation type. Finally, there are limitations related to the costing methods used in this study. Indirect costs used for time off from work may differ for individual patients who do not work or those who have high levels of income. Although PRC yielded better utilities than FCA, the difference of 0.01 QALY between FCA and PRC is highly unlikely to be clinically relevant. Although we could not identify publications reporting rates of revision PRC, the true rate is unlikely to be 0% as assumed in this analysis; it is unclear if or how a small but non-zero rate may affect the results. Although commonly used, Medicare costs may not reflect costs of health care provided in systems with commercial or other payers and may be affected by coding errors. Similarly, we used Veterans Affairs (VA) data to describe the timing of complications; patients treated in the VA health system may differ from the general population.
PRC dominated FCA in the base-case analysis and in the probabilistic sensitivity analysis. These results suggest that PRC is the optimal strategy for Stage-I or II SLAC or SNAC of the wrist for patients who are ≥55 years of age.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A172).
Footnotes
Investigation performed at the University of Utah, Salt Lake City, Utah
Disclosure: The research reported in this publication was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A171).
References
- 1.Lee VS, Kawamoto K, Hess R, Park C, Young J, Hunter C, Johnson S, Gulbransen S, Pelt CE, Horton DJ, Graves KK, Greene TH, Anzai Y, Pendleton RC. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016. September 13;316(10):1061-72. [DOI] [PubMed] [Google Scholar]
- 2.Kawamoto K, Martin CJ, Williams K, Tu MC, Park CG, Hunter C, Staes CJ, Bray BE, Deshmukh VG, Holbrook RA, Morris SJ, Fedderson MB, Sletta A, Turnbull J, Mulvihill SJ, Crabtree GL, Entwistle DE, McKenna QL, Strong MB, Pendleton RC, Lee VS. Value Driven Outcomes (VDO): a pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015. January;22(1):223-35. Epub 2014 Oct 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dacho AK, Baumeister S, Germann G, Sauerbier M. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008. October;61(10):1210-8. Epub 2007 Oct 22. [DOI] [PubMed] [Google Scholar]
- 4.Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984. May;9(3):358-65. [DOI] [PubMed] [Google Scholar]
- 5.Harrington RH, Lichtman DM, Brockmole DM. Common pathways of degenerative arthritis of the wrist. Hand Clin. 1987. November;3(4):507-27. [PubMed] [Google Scholar]
- 6.Traverso P, Wong A, Wollstein R, Carlson L, Ashmead D, Watson HK. Ten-year minimum follow-up of 4-corner fusion for SLAC and SNAC wrist. Hand (N Y). 2017. November;12(6):568-72. Epub 2016 Dec 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saltzman BM, Frank JM, Slikker W, Fernandez JJ, Cohen MS, Wysocki RW. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015. June;40(5):450-7. Epub 2014 Oct 7. [DOI] [PubMed] [Google Scholar]
- 8.Mulford JS, Ceulemans LJ, Nam D, Axelrod TS. Proximal row carpectomy vs four corner fusion for scapholunate (Slac) or scaphoid nonunion advanced collapse (Snac) wrists: a systematic review of outcomes. J Hand Surg Eur Vol. 2009. April;34(2):256-63. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MS, Kozin SH. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg Am. 2001. January;26(1):94-104. [DOI] [PubMed] [Google Scholar]
- 10.DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004. November;86(11):2359-65. [PubMed] [Google Scholar]
- 11.Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg Am. 2003. July;28(4):561-9. [DOI] [PubMed] [Google Scholar]
- 12.Kendall CB, Brown TR, Millon SJ, Rudisill LE, Jr, Sanders JL, Tanner SL. Results of four-corner arthrodesis using dorsal circular plate fixation. J Hand Surg Am. 2005. September;30(5):903-7. [DOI] [PubMed] [Google Scholar]
- 13.Vanhove W, De Vil J, Van Seymortier P, Boone B, Verdonk R. Proximal row carpectomy versus four-corner arthrodesis as a treatment for SLAC (scapholunate advanced collapse) wrist. J Hand Surg Eur Vol. 2008. April;33(2):118-25. [DOI] [PubMed] [Google Scholar]
- 14.Bain GI, Watts AC. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am. 2010. May;35(5):719-25. Epub 2010 Apr 9. [DOI] [PubMed] [Google Scholar]
- 15.Aita MA, Nakano EK, Schaffhausser HL, Fukushima WY, Fujiki EN. Randomized clinical trial between proximal row carpectomy and the four-corner fusion for patients with stage II SNAC. Rev Bras Ortop. 2016. August 20;51(5):574-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chim H, Moran SL. Long-term outcomes of proximal row carpectomy: a systematic review of the literature. J Wrist Surg. 2012. November;1(2):141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wagner ER, Bravo D, Elhassan B, Moran SL. Factors associated with improved outcomes following proximal row carpectomy: a long-term outcome study of 144 patients. J Hand Surg Eur Vol. 2016. June;41(5):484-91. Epub 2015 Jul 30. [DOI] [PubMed] [Google Scholar]
- 18.Wagner ER, Werthel JD, Elhassan BT, Moran SL. Proximal row carpectomy and 4-corner arthrodesis in patients younger than age 45 years. J Hand Surg Am. 2017. June;42(6):428-35. Epub 2017 Apr 12. [DOI] [PubMed] [Google Scholar]
- 19.Berkhout MJ, Bachour Y, Zheng KH, Mullender MG, Strackee SD, Ritt MJ. Four-corner arthrodesis versus proximal row carpectomy: a retrospective study with a mean follow-up of 17 years. J Hand Surg Am. 2015. July;40(7):1349-54. Epub 2015 Feb 18. [DOI] [PubMed] [Google Scholar]
- 20.Richou J, Chuinard C, Moineau G, Hanouz N, Hu W, Le Nen D. Proximal row carpectomy: long-term results. Chir Main. 2010. February;29(1):10-5. Epub 2009 Nov 13. [DOI] [PubMed] [Google Scholar]
- 21.Ferreres A, Garcia-Elias M, Plaza R. Long-term results of lunocapitate arthrodesis with scaphoid excision for SLAC and SNAC wrists. J Hand Surg Eur Vol. 2009. October;34(5):603-8. Epub 2009 Aug 17. [DOI] [PubMed] [Google Scholar]
- 22.Williams JB, Weiner H, Tyser AR. Long-term outcome and secondary operations after proximal row carpectomy or four-corner arthrodesis. J Wrist Surg. 2018. February;7(1):51-6. Epub 2017 Jul 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wall LB, Didonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am. 2013. August;38(8):1498-504. Epub 2013 Jun 25. [DOI] [PubMed] [Google Scholar]
- 24.Ali MH, Rizzo M, Shin AY, Moran SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (N Y). 2012. March;7(1):72-8. Epub 2011 Nov 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cha SM, Shin HD, Kim KC. Clinical and radiological outcomes of scaphoidectomy and 4-corner fusion in scapholunate advanced collapse at 5 and 10 years. Ann Plast Surg. 2013. August;71(2):166-9. [DOI] [PubMed] [Google Scholar]
- 26.Neubrech F Mühldorfer-Fodor M Pillukat T. Jv Schoonhoven Prommersberger KJ. Long-term results after midcarpal arthrodesis. J Wrist Surg. 2012. November;1(2):123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trail IA, Murali R, Stanley JK, Hayton MJ, Talwalkar S, Sreekumar R, Birch A. The long-term outcome of four-corner fusion. J Wrist Surg. 2015. May;4(2):128-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kazmers NH, Stephens AR, Presson AP, Xu Y, Feller RJ, Tyser AR. Comparison of direct surgical costs for proximal row carpectomy and four-corner arthrodesis. J Wrist Surg. 2019. February;8(1):66-71. Epub 2018 Nov 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahgozar P, Zhong L, Chung KC. A comparative analysis of resource utilization between proximal row carpectomy and partial wrist fusion: a population study. J Hand Surg Am. 2017. October;42(10):773-80. Epub 2017 Sep 7. [DOI] [PubMed] [Google Scholar]
- 30.Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, Kuntz KM, Meltzer DO, Owens DK, Prosser LA, Salomon JA, Sculpher MJ, Trikalinos TA, Russell LB, Siegel JE, Ganiats TG. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016. September 13;316(10):1093-103. [DOI] [PubMed] [Google Scholar]
- 31.Beck JR, Pauker SG. The Markov process in medical prognosis. Med Decis Making. 1983;3(4):419-58. [DOI] [PubMed] [Google Scholar]
- 32.Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998. April;13(4):397-409. [DOI] [PubMed] [Google Scholar]
- 33.Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, Luce BR; ISPOR Task Force on Good Research Practices—Modeling Studies. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices—Modeling Studies. Value Health. 2003. Jan-Feb;6(1):9-17. [DOI] [PubMed] [Google Scholar]
- 34.Tyser AR, Garcia B, Stephens AR, Kazmers NH, Sauer B, Lu C. Risk of fusion or reoperation after FCA or PRC for stage II SLAC/SNAC: a propensity matched cohort study of 1,118 patients. J Hand Surg Am. 2018;43(9)(Supplement):S5-6. [Google Scholar]
- 35.U.S. Social Security Administration. Period life table, 2015. Accessed 2020 Apr 2. https://www.ssa.gov/oact/STATS/table4c6_2015.html [Google Scholar]
- 36.Krakauer JD, Bishop AT, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg Am. 1994. September;19(5):751-9. [DOI] [PubMed] [Google Scholar]
- 37.Tomaino MM, Miller RJ, Cole I, Burton RI. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision? J Hand Surg Am. 1994. January;19(1):134-42. [DOI] [PubMed] [Google Scholar]
- 38.Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am. 1995. November;20(6):965-70. [DOI] [PubMed] [Google Scholar]
- 39.Chedal-Bornu B, Corcella D, Forli A, Moutet F, Bouyer M. Long-term outcomes of proximal row carpectomy: A series of 62 cases. Hand Surg Rehabil. 2017. October;36(5):355-62. Epub 2017 Jul 26. [DOI] [PubMed] [Google Scholar]
- 40.Weiss AP, Hastings H., 2nd Wrist arthrodesis for traumatic conditions: a study of plate and local bone graft application. J Hand Surg Am. 1995. January;20(1):50-6. [DOI] [PubMed] [Google Scholar]
- 41.Sagerman SD, Palmer AK. Wrist arthrodesis using a dynamic compression plate. J Hand Surg Br. 1996. August;21(4):437-41. [DOI] [PubMed] [Google Scholar]
- 42.Hastings H, 2nd, Weiss AP, Quenzer D, Wiedeman GP, Hanington KR, Strickland JW. Arthrodesis of the wrist for post-traumatic disorders. J Bone Joint Surg Am. 1996. June;78(6):897-902. [DOI] [PubMed] [Google Scholar]
- 43.Field J, Herbert TJ, Prosser R. Total wrist fusion. A functional assessment. J Hand Surg Br. 1996. August;21(4):429-33. [DOI] [PubMed] [Google Scholar]
- 44.Houshian S, Schrøder HA. Wrist arthrodesis with the AO titanium wrist fusion plate: a consecutive series of 42 cases. J Hand Surg Br. 2001. August;26(4):355-9. [DOI] [PubMed] [Google Scholar]
- 45.Terzis JK, Barmpitsioti A. Wrist fusion in posttraumatic brachial plexus palsy. Plast Reconstr Surg. 2009. December;124(6):2027-39. [DOI] [PubMed] [Google Scholar]
- 46.Centers for Medicare & Medicaid Services Medicare provider utilization and payment data: physician and other supplier. 2016. Accessed 2018 Sep 13. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicare-provider-charge-data/physician-and-other-supplier.html
- 47.Healthcare Cost and Utilization Project (HCUP). HCUP State Ambulatory Surgery and Services Databases (SASD). Rockville: Agency for Healthcare Research and Quality; 2013. Accessed 2018 Sep 13. www.hcup-us.ahrq.gov/sasdoverview.jsp [Google Scholar]
- 48.Bureau of Labor Statistics, U.S. Department of Labor. Usual weekly earnings of wage and salary workers. Third quarter 2018. 2018. October 16 Accessed 2018 Nov 29. https://www.bls.gov/news.release/archives/wkyeng_10162018.pdf [Google Scholar]
- 49.Graham B, Detsky AS. The application of decision analysis to the surgical treatment of early osteoarthritis of the wrist. J Bone Joint Surg Br. 2001. July;83(5):650-4. [DOI] [PubMed] [Google Scholar]
- 50.Daar DA, Shah A, Mirrer JT, Thanik V, Hacquebord J. Proximal row carpectomy versus four-corner arthrodesis for the treatment of scapholunate advanced collapse/scaphoid nonunion advanced collapse wrist: a cost-utility analysis. Plast Reconstr Surg. 2019. May;143(5):1432-45. [DOI] [PubMed] [Google Scholar]
- 51.Göhler A, Geisler BP, Manne JM, Kosiborod M, Zhang Z, Weintraub WS, Spertus JA, Gazelle GS, Siebert U, Cohen DJ. Utility estimates for decision-analytic modeling in chronic heart failure—health states based on New York Heart Association classes and number of rehospitalizations. Value Health. 2009. Jan-Feb;12(1):185-7. Epub 2008 Jul 18. [DOI] [PubMed] [Google Scholar]
- 52.Sturza J. A review and meta-analysis of utility values for lung cancer. Med Decis Making. 2010. Nov-Dec;30(6):685-93. Epub 2010 May 6. [DOI] [PubMed] [Google Scholar]
- 53.Mavrogenis AF, Flevas DA, Raptis K, Megaloikonomos PD, Igoumenou VG, Antoniadou T, Dimopoulos L, Antonopoulos D, Spyridonos SG. Four-corner fusion of the wrist: clinical and radiographic outcome of 31 patients. Eur J Orthop Surg Traumatol. 2016. December;26(8):859-66. Epub 2016 Jul 25. [DOI] [PubMed] [Google Scholar]
- 54.Bedford B, Yang SS. High fusion rates with circular plate fixation for four-corner arthrodesis of the wrist. Clin Orthop Relat Res. 2010. January;468(1):163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.U.S. Bureau of Labor Statistics. Labor force statistics from the current population survey. 2013. Accessed 2019 Dec 3. https://www.bls.gov/cps/lfcharacteristics.htm#laborforce [Google Scholar]
- 56.Minami A, Kato H, Iwasaki N. Total wrist arthrodesis using bowed crossed K-wires. J Hand Surg Br. 1999. August;24(4):410-5. [DOI] [PubMed] [Google Scholar]