Abstract
Background:
Modern bearing surface options have increased implant survivorship after total hip arthroplasty (THA). We utilized data from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (NJR) to analyze implant survivorship after THAs with uncemented acetabular components with different bearing combinations.
Methods:
Polyethylene (PE) manufacturing properties supplied by the manufacturers were used to subdivide the NJR data set into cross-linked PE (XLPE) and conventional PE groups. Overall and cause-specific revisions for various bearing combinations were analyzed using Kaplan-Meier and multivariate Cox proportional hazard regression survival analyses.
Results:
Of 420,339 primary THAs, 8,025 were revised during an average follow-up period of 4.4 years (maximum, 13.3 years). In the Cox regression model with metal on conventional PE as the reference, the lowest risk of revision for any reason was for ceramicized metal on XLPE (hazard ratio [HR] = 0.58, 95% confidence interval [CI] = 0.48, 0.71), followed by ceramic on XLPE (HR = 0.66, 95% CI = 0.60, 0.72), ceramic on PE (HR = 0.74, 95% CI = 0.66, 0.82), ceramic on ceramic (HR = 0.77, 95% CI = 0.72, 0.82), and metal on XLPE (HR = 0.81, 95% CI = 0.76, 0.87). A similar pattern was observed when patients under the age of 55 years were analyzed independently. Younger age, male sex, and cementless stem fixation were associated with a higher risk of revision.
Conclusions:
In a fully adjusted model, ceramicized metal on XLPE and ceramic on XLPE were associated with the lowest risk of revision for any reason. This finding was sustained when patients under the age of 55 years were analyzed independently. On the basis of the NJR data set, use of XLPE markedly reduces the risk of revision.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Total hip arthroplasty (THA) is a highly successful treatment for relieving the pain and disability associated with degeneration of the hip joint1. Polyethylene (PE)-based bearing surfaces in THA have traditionally been considered the source of wear particles that can play a critical role in osteolysis and loosening2. Wear and the associated aseptic loosening are common reasons for revision in registry reports3. This is a particular concern in younger patients, who have a higher lifetime risk of revision4. With demand for joint replacement in younger patients increasing, bearing surface choice remains critical5.
The introduction of cross-linked PE (XLPE) has led to a significant improvement in wear rates and the need for revision6,7, although some reports have highlighted some material-specific implant failures8,9. This has previously not been stratified in the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (NJR) annual reports3.
Authors of previous registry studies have combined the outcomes of cemented and uncemented acetabular components when reporting bearing survivorship7,10. However, using an uncemented acetabular component provides the ability to use a ceramic-on-ceramic (CoC) bearing. The amalgamation of cemented and uncemented acetabular components has the potential to introduce bias due to the different failure modes reported2,11,12 and the different bearing combinations available. We therefore decided to analyze uncemented acetabular components independently.
The aim of this study was to analyze implant survivorship after THAs using uncemented acetabular components with different bearing surface articulations.
Materials and Methods
Data from 2 different sources were combined: revision outcomes from the NJR and PE manufacturing characteristics supplied by manufacturers. NJR outcomes were abstracted for all 464,396 primary THAs that were performed with an uncemented acetabular component between January 1, 2004, and July 28, 2016. Each product was linked to manufacturing characteristics supplied by manufacturers with use of its unique catalogue number. After linking and excluding records that were missing key covariate data, a final sample of 420,339 was analyzed. PE liners that received a total irradiation dose of <5 Mrad were classed as conventional PE, and liners that received ≥5 Mrad were classed as XLPE. This approach is consistent with previous registry reports7,13.
The end point of interest was first revision, defined as the exchange of ≥1 femoral or acetabular implant components14. If there was no revision up to July 28, 2016, the last follow-up visit, the observation was censored. Patients who died without revision having been performed were censored at the time of death. We investigated the risk of revision for any reason and the risk of revisions for the most common causes—i.e., infection, aseptic loosening, wear, dislocation, periprosthetic fracture, pain, and implant fracture. Multiple causes could be reported for the same revision.
Reporting joint replacements to the NJR was not mandatory in its early years, raising the issue of selective reporting3. To control for possible underreporting of revisions in those years of the NJR data set, we controlled for the yearly cohort effect. This analysis controls for the effect of the year of the primary THA implantation on prosthetic joint survival.
Bearing surface wear is a critical issue for young active patients undergoing joint arthroplasty. We therefore performed an additional analysis of patients who underwent THA before the age of 55 years.
Statistical Analysis
Overall and cause-specific revisions were analyzed using Kaplan-Meier (K-M) analyses adjusted for a competing risk of death to describe the cumulative incidence of revision by bearing combinations15. Revisions for other reasons were also treated as a competing risk in cause-specific analyses. Next, hazard ratios (HRs) for overall and cause-specific revisions were obtained with an age and sex-adjusted Cox proportional hazard regression analysis accounting for a competing risk of death. Finally, HRs for various bearing combinations were obtained by a multivariate Cox proportional hazard regression survival analysis accounting for a competing risk of death. HRs reflect the relative risk of revision compared with the reference group and are specific to the model and population analyzed16. The following variables were included: indication for the THA (e.g., osteoarthritis); yearly cohort effect (e.g., 2004); bearing combination (ceramic on polyethylene [CoP], metal on polyethylene [MoP], ceramic on cross-linked polyethylene [CoXLPE], metal on cross-linked polyethylene [MoXLPE], ceramicized metal on cross-linked polyethylene [CMoXLPE], and ceramic on ceramic [CoC]); and type of stem fixation (cemented or cementless). Finally, a similar analysis was performed including liner/head size but only for CoC, CoXLPE, MoXLPE, and CMoXLPE because of the low numbers of THAs with larger head sizes in the MoP and CoP groups. All analyses were performed with SAS/STAT software, version 9.4 for PC (SAS Institute). The NJR Research Committee and the Trust Research & Development department gave approvals for this study.
Results
Descriptive statistics by bearing combination group are shown in Table I. Age and sex distributions differed among the groups, with the CoC, CMoXLPE, and CoXLPE groups having higher percentages of patients under the age of 55 years. Only 5% of the stems were cemented in the CMoXLPE group. The average follow-up was 4.4 years, and the maximum follow-up exceeded 11 years for all groups.
TABLE I.
Baseline Characteristics and Revision Outcomes by Bearing Surface in Cementless Cups
| CoC | CoP | CoXLPE | MoP | MoXLPE | CMoXLPE | |
| No. | 128,345 | 17,816 | 66,116 | 64,737 | 134,088 | 9,237 |
| Female sex (%) | 54.4 | 60.4 | 56.5 | 63.0 | 61.3 | 56.9 |
| Age (%) | ||||||
| <55 yr | 28.4 | 10.7 | 16.0 | 3.0 | 3.6 | 16.7 |
| 55 to <65 yr | 37.2 | 30.7 | 31.7 | 16.1 | 14.4 | 27.4 |
| 65 to <75 yr | 27.3 | 39.9 | 37.6 | 41.9 | 40.1 | 35.6 |
| ≥75 yr | 7.1 | 18.7 | 14.8 | 39.0 | 42.0 | 20.4 |
| Cemented stem (%) | 17.4 | 18.1 | 41.5 | 48.0 | 44.9 | 5.0 |
| Head size (no.) | ||||||
| 22, 26, 28 mm | 16,940 | 14,184 | 11,377 | 52,915 | 32,098 | 1,352 |
| 32 mm | 39,748 | 3,586 | 30,421 | 11,807 | 59,399 | 5,095 |
| 36, 40, 44, 48 mm | 71,657 | 46 | 24,318 | 15 | 42,591 | 2,790 |
| Outcome (%) | ||||||
| Unrevised | 93.9 | 83.2 | 95.9 | 76.0 | 90.3 | 95.9 |
| Revised | 2.1 | 2.6 | 1.2 | 3.0 | 1.5 | 1.1 |
| Death | 4.0 | 14.1 | 2.9 | 21.0 | 8.2 | 2.9 |
| Follow-up (yr) | ||||||
| Average (stand. dev.) | 4.7 (2.9) | 7.4 (3.3) | 2.8 (2.2) | 7.0 (3.1) | 3.4 (2.4) | 2.7 (2.3) |
| Maximum | 13.3 | 13.3 | 12.4 | 13.3 | 12.8 | 11.3 |
| Revisions (no.) | ||||||
| Any cause | 2,707 | 466 | 770 | 1,941 | 2,036 | 105 |
| Infection | 402 | 58 | 161 | 270 | 407 | 18 |
| Malalignment | 271 | 59 | 54 | 205 | 166 | 8 |
| Aseptic loosening | 753 | 156 | 154 | 598 | 365 | 16 |
| Wear | 98 | 42 | 26 | 186 | 61 | 6 |
| Head dislocation | 405 | 132 | 185 | 570 | 505 | 27 |
| Pain | 465 | 77 | 79 | 272 | 203 | 10 |
| Periprosthetic fracture | 336 | 49 | 143 | 326 | 490 | 21 |
| Incorrect sizing | 34 | 6 | 8 | 21 | 21 | 1 |
| Liner dislocation | 76 | 11 | 24 | 39 | 49 | 2 |
| Implant fracture | ||||||
| Socket | 162 | 0 | 6 | 5 | 12 | 0 |
| Head | 55 | 6 | 7 | 2 | 0 | 1 |
| Stem | 58 | 10 | 6 | 24 | 33 | 2 |
| Other | 288 | 42 | 55 | 117 | 134 | 8 |
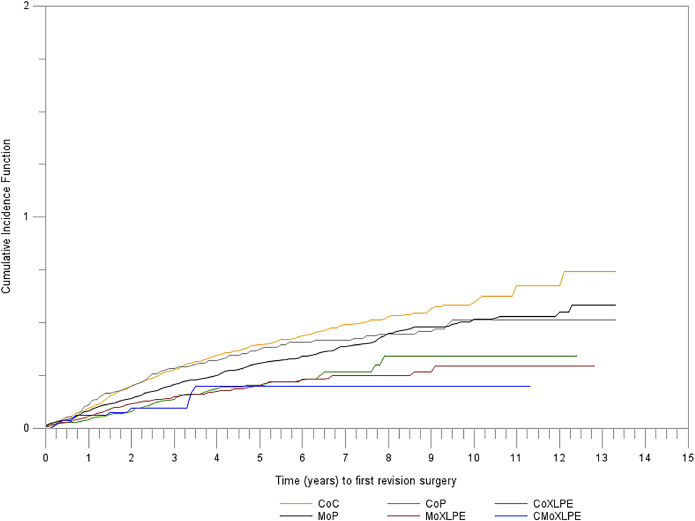
Cumulative Incidence of Revision
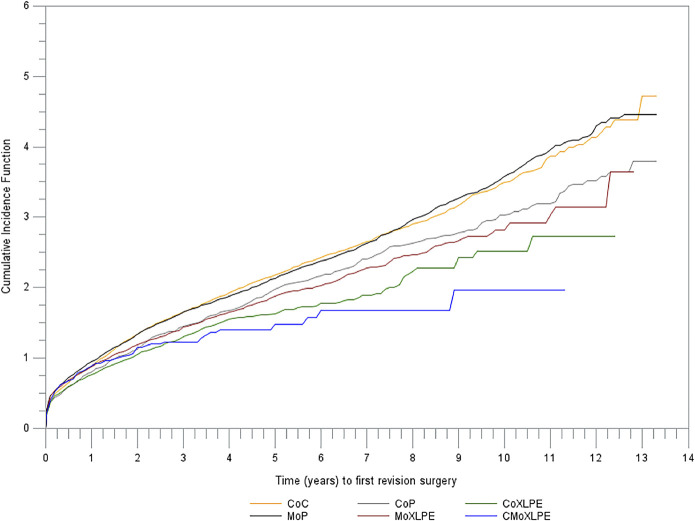
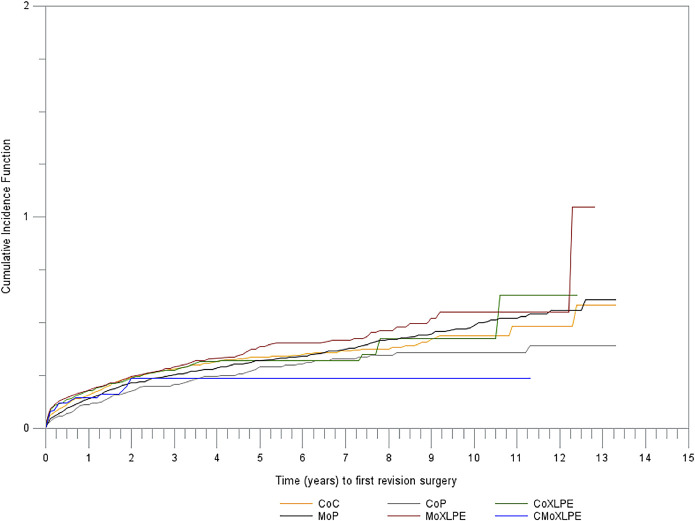
Of the 420,339 primary THAs with an uncemented acetabular component included in the analysis, 8,025 underwent revision (femoral or acetabular, or both). In our K-M analysis adjusted for a competing risk of death, the lowest cumulative incidence of revision for any reason at 10 years of follow-up was 1.96% for CMoXLPE (95% confidence interval [CI] = 1.35%, 2.76%), followed by 2.52% (95% CI = 2.14%, 2.95%) for CoXLPE, 2.81% (95% CI = 2.58%, 3.05%) for MoXLPE, 3.03% (95% CI = 2.75%, 3.33%) for CoP, 3.47% (95% CI = 3.29%, 3.65%) for CoC, and 3.53% (95% CI = 3.37%, 3.70%) for MoP (Fig. 1).
Fig. 1.
Cumulative incidence of revision for any reason by bearing combination (p < 0.0001).
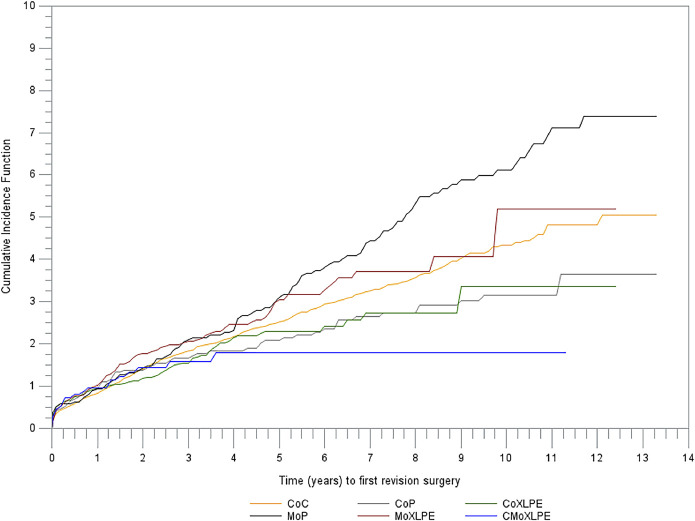
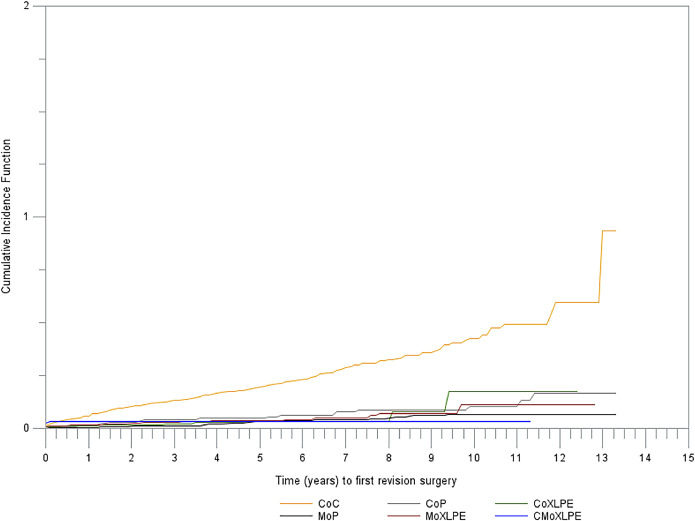
The cumulative incidence of revision at 10 years for patients under the age of 55 who underwent THA was 1.80% (95% CI = 1.11%, 2.78%) for CMoXLPE, 3.16% (95% CI = 2.36%, 4.13%) for CoP, 3.35% (95% CI = 2.16%, 4.95%) for CoXLPE, 4.34% (95% CI = 3.95%, 4.76%) for CoC, 5.20% (95% CI = 3.11%, 8.05%) for MoXLPE, and 6.12% (95% CI = 4.97%, 7.42%) for MoP (Fig. 2).
Fig. 2.
Cumulative incidence of revision for any reason by bearing combination in patients under the age of 55 years at the time of the primary THA (p < 0.0001).
Analysis of Reasons for Revision
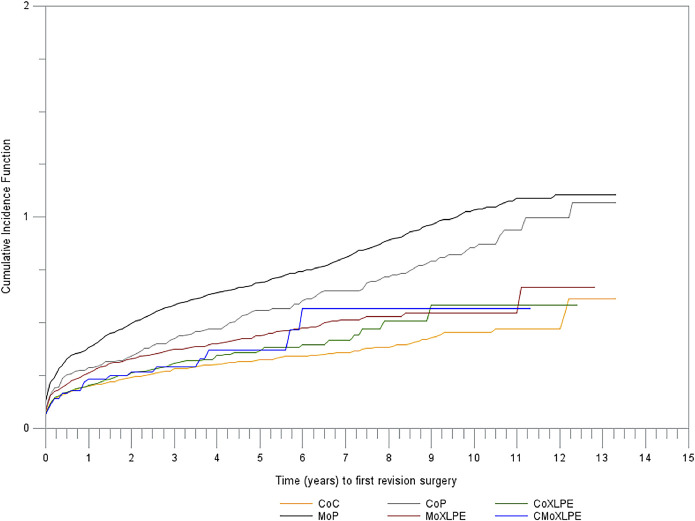
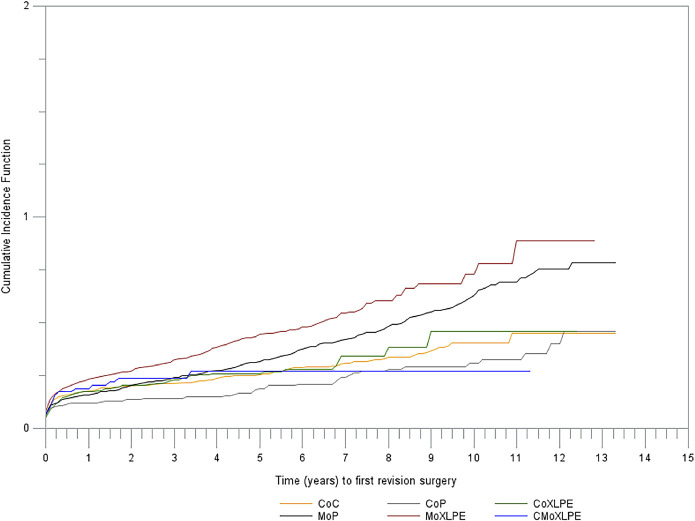
Aseptic Loosening and Wear
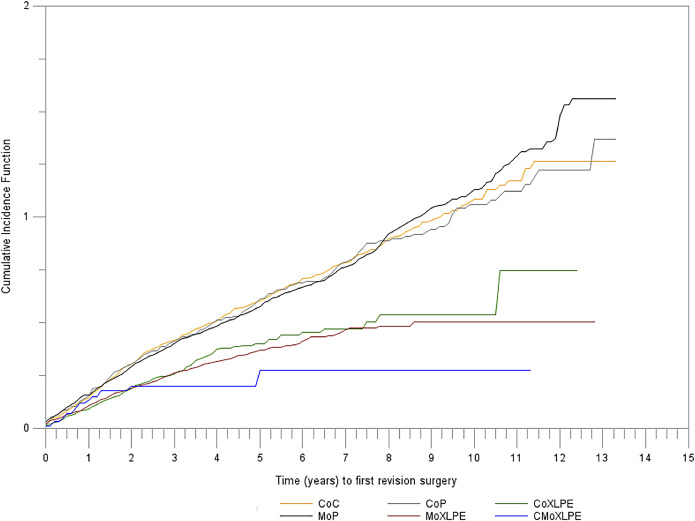
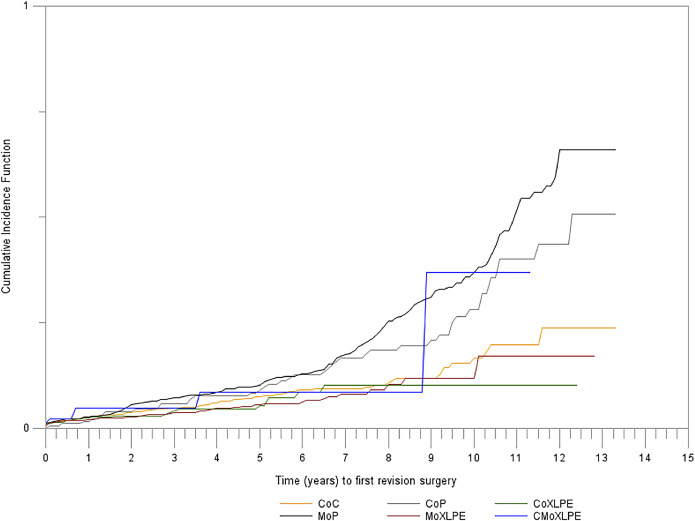
K-M estimates of the cumulative incidence of revision adjusted for a competing risk of death by reason for revision are presented in Figures 3-A through 3-G. The cumulative incidences of revision (of any component) for aseptic loosening (Fig. 3-A) or wear (Fig. 3-B) differed markedly among the bearing combinations.
Fig. 3-A.
Cumulative incidence of revision due to aseptic loosening by bearing combination (p < 0.0001).
Fig. 3-B.
Cumulative incidence of revision due to wear by bearing combination (p < 0.0001).
Fig. 3-C.
Cumulative incidence of revision due to infection by bearing combination (p = 0.1301).
Fig. 3-D.
Cumulative incidence of revision due to implant fracture by bearing combination (p < 0.0001).
Fig. 3-E.
Cumulative incidence of revision due to dislocation by bearing combination (p < 0.0001).
Fig. 3-F.
Cumulative incidence of revision due to periprosthetic fracture by bearing combination (p < 0.0001).
Fig. 3-G.
Cumulative incidence of revision due to pain by bearing combination (p < 0.0001).
The effect of bearing combination on the reason-specific risk of revision was further investigated in an age and sex-adjusted model, with MoP as the reference (Table II). The CMoXLPE and CoXLPE combinations demonstrated the lowest risk of revision due to aseptic loosening.
TABLE II.
Results of Cox Regression Analysis of Revisions According to Their Causes and Bearing Combination Adjusted for Age and Sex
| HR (95% CI) | ||||||
| CoC | CoP | CoXLPE | MoXLPE | CMoXLPE | MoP | |
| All revisions | 0.82 (0.77, 0.88) | 0.80 (0.72, 0.88) | 0.67 (0.61, 0.73) | 0.82 (0.77, 0.88) | 0.65 (0.54, 0.79) | 1.0 (reference) |
| Aseptic loosening | 0.65 (0.58, 0.73) | 0.77 (0.64, 0.92) | 0.46 (0.38, 0.55) | 0.55 (0.49, 0.63) | 0.34 (0.21, 0.56) | 1.0 (reference) |
| Wear | 0.38 (0.29, 0.51) | 0.68 (0.48, 0.95) | 0.36 (0.24, 0.55) | 0.40 (0.30, 0.53) | 0.59 (0.26, 1.35) | 1.0 (reference) |
| All reasons but aseptic loosening and wear | 0.92 (0.85, 1.00) | 0.79 (0.69, 0.90) | 0.78 (0.70, 0.86) | 0.95 (0.88, 1.03) | 0.77 (0.62, 0.96) | 1.0 (reference) |
| Infection | 0.76 (0.64, 0.90) | 0.69 (0.52, 0.92) | 0.84 (0.69, 1.02) | 1.07 (0.91, 1.25) | 0.68 (0.42, 1.09) | 1.0 (reference) |
| Dislocation | 0.43 (0.37, 0.49) | 0.81 (0.67, 0.98) | 0.49 (0.42, 0.59) | 0.61 (0.54, 0.69) | 0.51 (0.35, 0.76) | 1.0 (reference) |
| Periprosthetic fracture | 0.95 (0.81, 1.13) | 0.62 (0.46, 0.84) | 0.93 (0.76, 1.14) | 1.14 (0.99, 1.31) | 0.95 (0.61, 1.48) | 1.0 (reference) |
| Pain | 0.83 (0.70, 0.98) | 0.85 (0.66, 1.10) | 0.48 (0.37, 0.62) | 0.62 (0.52, 0.74) | 0.43 (0.23, 0.81) | 1.0 (reference) |
| Implant fracture | 5.60 (3.75, 8.36) | 1.65 (0.90, 3.03) | 1.04 (0.56, 1.95) | 1.38 (0.87, 2.19) | 1.48 (0.45, 4.89) | 1.0 (reference) |
Infection
There were no differences among the bearing groups in the K-M estimated cumulative incidence of revisions due to infection (Fig. 3-C). With MoP as the reference, the age and sex-adjusted HRs revealed a reduction in the risk of revision due to infection in the CoC and CoP groups.
Implant Fracture
The CoC group had the highest cumulative incidence of implant fracture (Fig. 3-D). With revision for implant fracture as the end point, the age and sex-adjusted HR was 5.60 (95% CI = 3.75, 8.36) for CoC. The HRs for the other bearing combinations did not differ from each other. A total of 1.3/1,000 implants with a CoC bearing had a ceramic liner fracture; 58.9% of the CoC implant fractures were due to ceramic liner breakage. The risk of fracture of the ceramic head was implantation-year dependent, being higher from 2003 to 2005 and lower from 2006 onward. There was no association between implantation year and ceramic liner fracture risk.
Other Reasons
The cumulative incidence of revision due to dislocation was higher for the bearing combinations that included conventional PE (Fig. 3-E). The cumulative incidence of revision due to periprosthetic fracture was higher for those that included a metal head (MoP and MoXLPE) (Fig. 3-F). The cumulative incidence of revision due to pain was highest for the CoC bearings (Fig. 3-G).
Multivariate Analysis
The effect of bearing surface on THA survival was further investigated with a Cox regression model controlling for age, sex, bearing combination, and stem fixation method (cemented or cementless). In this Cox model, with MoP as the reference, CMoXLPE and CoXLPE demonstrated the greatest reduction in the risk of any revision; all other bearing combinations showed a significant reduction in risk as well. This trend of reduced risk compared with that of MoP was upheld when patients under the age of 55 years were analyzed independently (Table III).
TABLE III.
Results of Cox Regression Analysis of Risk of Any Revision by Bearing Combination
| Characteristic | HR (95% CI) | |
| All Ages | <55 Years of Age | |
| Age | ||
| 55 to <65 yr | 0.85 (0.79, 0.91) | |
| 65 to <75 yr | 0.73 (0.68, 0.79) | |
| ≥75 yr | 0.68 (0.62, 0.73) | |
| <55 yr | 1.0 (reference) | |
| Sex | ||
| Male | 1.18 (1.13, 1.23) | 1.20 (1.08, 1.34) |
| Female | 1.0 (reference) | 1.0 (reference) |
| Bearing combination | ||
| CoC | 0.77 (0.72, 0.82) | 0.64 (0.52, 0.78) |
| CoP | 0.74 (0.66, 0.82) | 0.50 (0.36, 0.70) |
| CoXLPE | 0.66 (0.60, 0.72) | 0.61 (0.47, 0.78) |
| MoXLPE | 0.81 (0.76, 0.87) | 0.77 (0.59, 1.01) |
| CMoXLPE | 0.58 (0.48, 0.71) | 0.47 (0.30, 0.76) |
| MoP | 1.0 (reference) | 1.0 (reference) |
| Stem fixation | ||
| Cementless | 1.35 (1.28, 1.42) | 1.45 (1.26, 1.68) |
| Cemented | 1.0 (reference) | 1.0 (reference) |
The stem fixation method was associated with THA survival during exploratory analyses and was therefore included in the Cox model. In this multivariate model, cement fixation was associated with a significantly reduced risk of revision for any reason (HR for cementless fixation = 1.35, 95% CI = 1.28, 1.42). This finding was upheld in the analysis of those under 55 years of age (Table III).
Multivariate Analysis Including Head Size
Another Cox regression model was built to include head size (≤28 mm, 32 mm, or ≥36 mm). Because few THAs were done with larger head sizes in the MoP and CoP groups, this model included CoC, CoXLPE, CMoXLPE, and MoXLPE. In addition to those bearing combinations and head size, the model included age, sex, and stem fixation (cemented or cementless). The outcomes were revision of any component for any reason, revision due to dislocation, and revision due to aseptic loosening. With MoXLPE as the reference, CoC had the lowest risk of revision due to dislocation and CMoXLPE had the lowest risk of revision due to aseptic loosening. Cementless fixation was associated with a higher risk of revision for any reason as well as for aseptic loosening. CMoXLPE had the lowest risk of revision for any reason (Table IV).
TABLE IV.
Results of Cox Regression Analysis of Risk of Revision for Any Reason by Bearing Combination Adjusted for Head Size
| Characteristic | HR (95% CI) | ||
| All Causes | Dislocation | Aseptic Loosening | |
| Age | |||
| 55 to <65 yr | 0.82 (0.76, 0.89) | 0.84 (0.70, 1.02) | 0.79 (0.68, 0.91) |
| 65 to <75 yr | 0.76 (0.70, 0.82) | 0.86 (0.71, 1.04) | 0.61 (0.52, 0.71) |
| ≥75 yr | 0.76 (0.69, 0.84) | 1.01 (0.82, 1.26) | 0.43 (0.35, 0.53) |
| <55 yr | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
| Sex | |||
| Male | 1.16 (1.10, 1.23) | 1.05 (0.93, 1.19) | 1.34 (1.19, 1.50) |
| Female | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
| Bearing combination | |||
| CoC | 0.99 (0.93, 1.07) | 0.84 (0.72, 0.99) | 1.05 (0.90, 1.21) |
| CoXLPE | 0.84 (0.77, 0.92) | 0.90 (0.73, 1.06) | 0.85 (0.70, 1.03) |
| CMoXLPE | 0.75 (0.62, 0.92) | 0.90 (0.61, 1.34) | 0.52 (0.32, 0.86) |
| MoXLPE | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
| Stem fixation | |||
| Cementless | 1.33 (1.25, 1.42) | 1.03 (0.91, 1.18) | 2.26 (1.93, 2.65) |
| Cemented | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
| Head size | |||
| ≤28 mm | 1.07 (0.99, 1.15) | 2.13 (1.82, 2.48) | 0.85 (0.73, 1.00) |
| 32 mm | 0.92 (0.86, 0.98) | 1.27 (1.09, 1.47) | 0.79 (0.69, 0.91) |
| ≥36 mm | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
Discussion
To our knowledge, this is the first study utilizing NJR data that differentiated between XLPE and conventional PE when comparing different bearing combinations. Our analysis confirms a significant association between modern bearing surface combinations and THA survival, and corroborates previous analyses using data from the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR)7 and the Dutch Arthroplasty Register (LROI)10. However, registry data that do not stratify for PE modifications are used to inform policy17,18.
The latest report by the AOANJRR provided age and sex-adjusted HRs with MoXLPE as the reference13. In that report, CMoXLPE was the best performing combination, with a marked reduction in the HR from 3 months onward. CoC and CoXLPE did not differ significantly from MoXLPE. CMoXLPE showed a significant reduction in the risk of revision for any reason over the entire follow-up period. The AOANJRR urged caution in interpreting the CMoXLPE results because this is “a single company product, used with a small number of femoral stem and acetabular component combinations,” making it unclear whether this effect is due to the bearing combination or the femoral and acetabular prosthesis13. The same limitation applies to our study when investigating the CMoXLPE bearing combination.
The LROI performed a similar analysis of THA survival with different bearings10. With MoP as the reference in a multivariate model, they also reported a reduction in the risk of revision in association with CMoXLPE. The CoC and CoXLPE groups had similar HRs, which were significantly lower than the HRs of the MoP group. This finding agrees with the results of the multivariate analysis in our study. Neither the AOANJRR nor the LROI differentiated between cemented and cementless acetabular components, whereas our study included only cementless acetabular components to ensure that the failure modes and material properties did not act as confounding factors.
Authors of randomized controlled trials (RCTs) and meta-analyses have reached similar conclusions regarding survival of implants with modern bearings. In a direct-comparison meta-analysis that included 5 RCTs with a total of 779 THAs in patients younger than 65 years, Wyles et al. found no differences in short-to-midterm survivorship between CoC and CoXLPE or between CoC and MoXLPE19. Yin et al. identified no significant differences in survivorship among CoC, CoP, CoXLPE, and MoXLPE bearings in a network meta-analysis with a mean follow-up of 6.6 years (range, 2 to 12.4 years)20.
Unlike previous studies, our study stratified analysis by reasons for revision, and it showed that CMoXLPE is associated with a significant reduction in the risk of revision due aseptic loosening compared with MoXLPE.
CoC bearings have been recommended for young and active patients because of the low volumetric wear and biological response to the generated debris21-24. However, the data on the performance of CoC have been less encouraging in joint registries. On the basis of an age and sex-adjusted model, the AOANJRR reported no significant difference in the survival of CoC bearings compared with MoXLPE over a 17-year follow-up period13. An analysis of the Danish Hip Arthroplasty Register (DHR) revealed similar results, with a model adjusted for diagnosis, age, sex, comorbidity, head size, year of surgery, and duration of surgery showing a nonsignificant increase in the HR of revision for CoC bearings with MoP as the reference25. The maximum follow-up was 8.7 years. The authors did not differentiate between XLPE and conventional PE. The results of our analysis are in agreement with those of the previous registry studies; with the end point of revision for any reason and MoP as the reference, CMoXLPE had the lowest HR and CoXLPE and CoC were the next best performing bearing combinations.
Femoral head size has been extensively investigated and reported on, with the concern that increased head size may reduce the risk of dislocation at the expense of increased rates of aseptic loosening and other reasons26,27. The option of bearing surface can be closely linked to the head size and therefore may affect the reasons for revision. By accounting for head size in our multivariate model, we were able to demonstrate that the effect of the bearing surface on the risk of revision due to dislocation and aseptic loosening is independent of the head.
Our analysis included the femoral stem fixation method. Cemented stems were associated with a reduced risk of revision for any reason as well as due to aseptic loosening. This result is in agreement with a previous analysis of the NJR data set28. We were able to control for this important factor in our multivariate analysis.
We found that the risk of revision due to implant fracture was significantly higher for the CoC bearings than for the other bearings. Ceramic manufacturing has advanced to improve its material properties and specifically reduce fracture risk24. Ceramic component fractures have been reported in both CoC and CoP bearings29,30. We did not control for different types of ceramics in this analysis.
The effect of implantation year seen in our analysis of implant fracture is in agreement with other research concerning CoC bearings. In a study of revisions due to CoC bearing fracture in the NJR data set, Howard et al. reported a reduction in revisions due to fracture of the femoral head associated with the use of modern BIOLOX delta ceramics compared with older BIOLOX forte heads but no reduction in revisions for liner fractures with newer compared with older ceramics31. In study of data from the DHR, Varnum et al. reported a 33% increased risk of revision due to implant fracture in association with CoC bearings, with the fracture risk being 0.28% for heads and 0.17% for liners25. In the CoC bearing group, 77% of the heads and 81% of the liners were made of BIOLOX forte25.
Our study has several limitations. Because registry data are observational, it is not possible to control for all confounding factors, even after statistical modeling. The choice of bearing surface is likely to be affected by patient age and the assumed future need for revision. Patient activity levels, although not recorded in registry data, might be used by surgeons when deciding on THA bearings. Our analysis controlled for patient age, but activity level might be an unaccounted-for confounder. Reasons for revision of a THA in the data set do not include squeaking. It is therefore possible that CoC THAs that were actually revised for squeaking were recorded as being revised for pain or other reasons in the data set. Our study did not stratify ceramics by the material used. Future studies on the performance of modern ceramics in large data sets would add information to the debate regarding the optimal THA bearing. The maximum follow-up in our analysis was 13 years. During this time, surgical, manufacturing, and perioperative techniques evolved and may have affected implant survival. We included the yearly cohort effect in our analysis, but some unaccounted-for confounding may remain. Some wear-associated revisions might occur with longer follow-up; therefore, large registry studies with long follow-up will continue to be of interest. Finally, we did not stratify for chemically stabilized PE in this analysis because it was used in too few patients; therefore, it is not possible at this time to delineate if chemical stabilization will provide a protective effect on the wear characteristics of this bearing.
Our analysis of the NJR data set revealed that CMoXLPE and CoXLPE were associated with the lowest cumulative risk of revision for any reason. This finding was sustained when patients under the age of 55 years were analyzed independently. XLPE was associated with a markedly reduced risk of revision due to aseptic loosening at a maximum follow-up of 13 years.
Footnotes
Investigation performed at The Royal Orthopaedic Hospital NHS Foundation Trust, Birmingham, United Kingdom
Disclosure: This study was supported by an unrestricted research grant from Smith & Nephew, Inc. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A159).
References
- 1.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007. October 27;370(9597):1508-19. [DOI] [PubMed] [Google Scholar]
- 2.Harris WH. Wear and periprosthetic osteolysis: the problem. Clin Orthop Relat Res. 2001. December;393:66-70. [DOI] [PubMed] [Google Scholar]
- 3.NJR Editorial Board. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 15th annual report. 2018. Accessed 2020 Mar 11. https://www.hqip.org.uk/wp-content/uploads/2018/11/NJR-15th-Annual-Report-2018.pdf [Google Scholar]
- 4.Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, Cooper C, Carr AJ, Arden NK, Beard DJ, Price AJ. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017. April 8;389(10077):1424-30. Epub 2017 Feb 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009. October;467(10):2606-12. Epub 2009 Apr 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kurtz SM, Gawel HA, Patel JD. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res. 2011. August;469(8):2262-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Steiger R, Lorimer M, Graves SE. Cross-linked polyethylene for total hip arthroplasty markedly reduces revision surgery at 16 years. J Bone Joint Surg Am. 2018. August 1;100(15):1281-8. [DOI] [PubMed] [Google Scholar]
- 8.Tower SS, Currier JH, Currier BH, Lyford KA, Van Citters DW, Mayor MB. Rim cracking of the cross-linked longevity polyethylene acetabular liner after total hip arthroplasty. J Bone Joint Surg Am. 2007. October;89(10):2212-7. [DOI] [PubMed] [Google Scholar]
- 9.Blumenfeld TJ, McKellop HA, Schmalzried TP, Billi F. Fracture of a cross-linked polyethylene liner: a multifactorial issue. J Arthroplasty. 2011. June;26(4):666.e5-8. Epub 2010 Sep 18. [DOI] [PubMed] [Google Scholar]
- 10.Peters RM, Van Steenbergen LN, Stevens M, Rijk PC, Bulstra SK, Zijlstra WP. The effect of bearing type on the outcome of total hip arthroplasty. Acta Orthop. 2018. April;89(2):163-9. Epub 2017 Nov 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sköldenberg OG, Rysinska AD, Chammout G, Salemyr M, Mukka SS, Bodén H, Eisler T. A randomized double-blind noninferiority trial, evaluating migration of a cemented vitamin E-stabilized highly crosslinked component compared with a standard polyethylene component in reverse hybrid total hip arthroplasty. Bone Joint J. 2019. October;101-B(10):1192-8. [DOI] [PubMed] [Google Scholar]
- 12.Ranawat CS, Deshmukh RG, Peters LE, Umlas ME. Prediction of the long-term durability of all-polyethylene cemented sockets. Clin Orthop Relat Res. 1995. August;317:89-105. [PubMed] [Google Scholar]
- 13.Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, knee & shoulder arthroplasty: 2018 annual report. 2018. Accessed 2020 Mar 11 https://aoanjrr.sahmri.com/annual-reports-2018 [Google Scholar]
- 14.Davis ET, Pagkalos J, Kopjar B. Polyethylene manufacturing characteristics have a major effect on the risk of revision surgery in cementless and hybrid total hip arthroplasties. Bone Joint J. 2020. January;102-B(1):90-101. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457-81. [Google Scholar]
- 16.Ranstam J, Kärrholm J, Pulkkinen P, Mäkelä K, Espehaug B, Pedersen AB, Mehnert F, Furnes O; NARA study group. Statistical analysis of arthroplasty data. II. Guidelines . Acta Orthop. 2011. June;82(3):258-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carnes KJ, Odum SM, Troyer JL, Fehring TK. Cost analysis of ceramic heads in primary total hip arthroplasty. J Bone Joint Surg Am. 2016. November 2;98(21):1794-800. [DOI] [PubMed] [Google Scholar]
- 18.Fawsitt CG, Thom HHZ, Hunt LP, Nemes S, Blom AW, Welton NJ, Hollingworth W, López-López JA, Beswick AD, Burston A, Rolfson O, Garellick G, Marques EMR. Choice of prosthetic implant combinations in total hip replacement: cost-effectiveness analysis using UK and Swedish hip joint registries data. Value Health. 2019. March;22(3):303-12. Epub 2018 Nov 2. [DOI] [PubMed] [Google Scholar]
- 19.Wyles CC, Jimenez-Almonte JH, Murad MH, Norambuena-Morales GA, Cabanela ME, Sierra RJ, Trousdale RT. There are no differences in short- to mid-term survivorship among total hip-bearing surface options: a network meta-analysis. Clin Orthop Relat Res. 2015. June;473(6):2031-41. Epub 2014 Dec 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yin S, Zhang D, Du H, Du H, Yin Z, Qiu Y. Is there any difference in survivorship of total hip arthroplasty with different bearing surfaces? A systematic review and network meta-analysis. Int J Clin Exp Med. 2015. November 15;8(11):21871-85. [PMC free article] [PubMed] [Google Scholar]
- 21.Petit A, Catelas I, Antoniou J, Zukor DJ, Huk OL. Differential apoptotic response of J774 macrophages to alumina and ultra-high-molecular-weight polyethylene particles. J Orthop Res. 2002. January;20(1):9-15. [DOI] [PubMed] [Google Scholar]
- 22.Clarke IC, Gustafson A. Clinical and hip simulator comparisons of ceramic-on-polyethylene and metal-on-polyethylene wear. Clin Orthop Relat Res. 2000. October;379:34-40. [DOI] [PubMed] [Google Scholar]
- 23.Boutin P. [Total arthroplasty of the hip by fritted aluminum prosthesis. Experimental study and 1st clinical applications]. Rev Chir Orthop Reparatrice Appar Mot. 1972. Apr-May;58(3):229-46. French. [PubMed] [Google Scholar]
- 24.Hannouche D, Hamadouche M, Nizard R, Bizot P, Meunier A, Sedel L. Ceramics in total hip replacement. Clin Orthop Relat Res. 2005. January;430:62-71. [DOI] [PubMed] [Google Scholar]
- 25.Varnum C, Pedersen AB, Kjærsgaard-Andersen P, Overgaard S. Comparison of the risk of revision in cementless total hip arthroplasty with ceramic-on-ceramic and metal-on-polyethylene bearings. Acta Orthop. 2015;86(4):477-84. Epub 2015 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zijlstra WP, De Hartog B, Van Steenbergen LN, Scheurs BW, Nelissen RGHH. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop. 2017. August;88(4):395-401. Epub 2017 Apr 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lachiewicz PF, Soileau ES, Martell JM. Wear and osteolysis of highly crosslinked polyethylene at 10 to 14 years: the effect of femoral head size. Clin Orthop Relat Res. 2016. February;474(2):365-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kandala NB, Connock M, Pulikottil-Jacob R, Sutcliffe P, Crowther MJ, Grove A, Mistry H, Clarke A. Setting benchmark revision rates for total hip replacement: analysis of registry evidence. BMJ. 2015. March 9;350:h756. [DOI] [PubMed] [Google Scholar]
- 29.Habermann B, Ewald W, Rauschmann M, Zichner L, Kurth AA. Fracture of ceramic heads in total hip replacement. Arch Orthop Trauma Surg. 2006. September;126(7):464-70. Epub 2006 Jun 21. [DOI] [PubMed] [Google Scholar]
- 30.Abdel MP, Heyse TJ, Elpers ME, Mayman DJ, Su EP, Pellicci PM, Wright TM, Padgett DE. Ceramic liner fractures presenting as squeaking after primary total hip arthroplasty. J Bone Joint Surg Am. 2014. January 1;96(1):27-31. [DOI] [PubMed] [Google Scholar]
- 31.Howard DP, Wall PDH, Fernandez MA, Parsons H, Howard PW. Ceramic-on-ceramic bearing fractures in total hip arthroplasty: an analysis of data from the National Joint Registry. Bone Joint J. 2017. August;99-B(8):1012-9. [DOI] [PubMed] [Google Scholar]