Abstract
Background
Compared to other racial/ethnic groups, infant mortality rates (IMR) are persistently highestamong Black infants in the United States, yet there is considerable regional variation. We examined state and county-level contextual factors that may explain regional differences in Black IMR and identified potential strategies for improvement.
Methods and findings
Black infant mortality data are from the Linked Birth/Infant Death files for 2009–2011. State and county contextual factors within social, economic, environmental, and health domains were compiled from various Census databases, the Food Environment Atlas, and the Area Health Resource File. Region was defined by the nine Census Divisions. We examined contextual associations with Black IMR using aggregated county-level Poisson regression with standard errors adjusted for clustering by state. Overall, Black IMR varied 1.5-fold across regions, ranging from 8.78 per 1,000 in New England to 13.77 per 1,000 in the Midwest. In adjusted models, the following factors were protective for Black IMR: higher state-level Black-White marriage rate (rate ratio (RR) per standard deviation (SD) increase = 0.81, 95% confidence interval (CI):0.70–0.95), higher state maternal and child health budget per capita (RR per SD = 0.96, 95% CI:0.92–0.99), and higher county-level Black index of concentration at the extremes (RR per SD = 0.85, 95% CI:0.81–0.90). Modeled variables accounted for 35% of the regional variation in Black IMR.
Conclusions
These findings are broadly supportive of ongoing public policy efforts to enhance social integration across races, support health and social welfare program spending, and improve economic prosperity. Although contextual factors accounted for about a third of regional variation, further research is needed to more fully understand regional variation in Black IMR disparities.
Introduction
In the United States, non-Hispanic Black (hereafter referred to as Black) infants have the highest rates of adverse birth outcomes, including preterm birth and infant mortality [1]. Black infants are more than twice as likely to die in the first year of life as compared to non-Hispanic White infants (hereafter referred to as White) [1]. Examination of geographic variation can be instructive in identifying contextual risk and protective factors. While overall and White infant mortality rates (IMR) are highest in the South, Black IMR tends to be highest in the Midwest and lowest in the West and Northeast [1].
Studies of regional variation may help us to better understand the heterogeneity of the Black birth experiences in the United States and may provide new insights into sources of excess Black IMR. Previous studies have focused on the sources of the Black-White disparity [2–5], which can be lower by virtue of high White versus low Black IMR [6], and limited in the provision of Black-specific contextual information as they are often dominated by the characteristics of the larger White community [5]. Studies that have examined Black infant mortality either alone or in addition to White infant mortality have suggested associations with various contextual factors within social, economic, environmental, and health domains but none have examined their contribution to regional variation [7–23]. Moreover, several studies have shown that the predictors of Black IMR are different than those of White IMR, and thus support a priority focus on the higher Black IMR [2, 4, 23, 24].
The current study focuses on regions to allow for a broader common historical and sociopolitical understanding of the Black experience in the United States, which may be masked in state-level analyses [6]. It remains unclear whether state and county contextual factors can explain broad regional patterns in Black IMR and help to identify risk and protective factors that may ameliorate higher rates in the Midwest and replicate or extend the lower rates observed in the West and Northeast [1]. Such information could inform regional multi-state action approaches to reducing infant mortality [25].
The aims of this study were:1) to examine regional variation in Black IMR and social, economic, environmental and health contextual factors;2) to identify which contextual factors are associated with Black IMR in multivariable models; and 3) to assess how much of the regional variation in Black IMR can be explained by these factors.
Methods
Data and measures
Birth and mortality data for Black infants were obtained from the National Center for Health Statistics’ 2009–2011 linked birth/infant death files with county and state identifiers obtained by request from the National Association of Public Health Statistics and Information Systems [26]. The selected data years center upon 2010 given various covariates drawn from the 2010 Census. Regional units were defined by Census Divisions (hereafter referred to as regions). These nine regions are based on the Census Bureau’s framework of large units that are relatively similar in terms of population characteristics, economic, and historical development [27].
We constructed an aggregated county-level dataset with a count of Black births, Black infant deaths, and linked county and state-level characteristics. We limited the analysis to counties with complete data on covariates (2450 counties of the 2708 counties with Black births), which resulted in a loss of 29 deaths (retained 99.9% of deaths) and 3209 births (retained 99.8% of births). Ethical approval was not needed as fully anonymized vital records data are publicly available through a data use agreement with the National Center for Health Statistics.
Various state and county-level factors in the social, economic, environment and health domains were compiled from Census databases, the Food Environment Atlas, and the Area Health Resource File [28]. We used Black-specific data wherever possible. Of approximately 75variables initially compiled (S1 Appendix), 16 were selected for a final model based on prior literature on adverse birth outcomes or health disparities and consideration for both literature support and strength of association when deciding between collinear variables. S2 Appendix includes the level (state or county), year, data source, and calculation details for each of the variables included in the final model.
The final social variables in the model were percent Non-Hispanic Black population (state) [23], Black-White marriage rate (state) [21, 29], a hypersegregation index (county) [22–24, 30–32], Black incarceration rate (state) [7, 13, 33], and percent of voting age population casting votes (state) [11]. The Black-White marriage rate, calculated as the percentage of married Black individuals with a White spouse, was selected as a contextual measure of social integration [29, 34, 35]. The hyper segregation index was calculated based on dissimilarity (a measure of evenness, which is the proportion of Black residents required to change census tracts to get an even distribution of minorities in a county) and isolation (a measure of exposure, which is the extent to which members of the Black (minority) population are exposed only to each other, rather than to members of the White (majority) population [36, 37]. Other literature has indicated that looking at these two (of five) conventional measures of segregation is sufficient to assess hyper segregation [38, 39].
Economic variables included the Index of Concentration at Extremes (ICE) based on Black household income (county) [18, 40–42], and Black unemployment rate (county) [43]. The Black ICE is a measure of spatial economic polarization and ranges from -1 (all of the population is among the most deprived group; <20% percentile of household income) to 1 (all of the population is among the most privileged group; >80% percentile of household income) [19, 20]. The universe for the Black ICE is all Black households.
Environmental variables included daily fine particulate matter in micrograms per cubic meter (PM2.5)(county) [44, 45], grocery stores per 1,000 population (county) [46, 47], housing unit vacancy percent (county) [7, 10, 48], and National Center of Health Statistics’ 2006 urban/rural classification (county) [49, 50].
Health variables included Medicaid eligibility for pregnant women based on percent of federal poverty level (state) [17, 51, 52], maternal and child health (MCH) budget per capita (state) [53, 54], nurse midwives per 100,000 women aged 15–44 (county) [55–57], obstetricians/gynecologists per 100,000 women aged 15–44 (county) [14, 58–60], and percent of uninsured women aged 18–44 (county) [2, 7, 61].
Statistical analysis
Black IMR and contextual covariates were descriptively examined by region (Aim 1) using overall totals (sum of deaths and births) for IMR and means or proportions for covariates (weighted by births) to represent average contextual characteristic per Black birth in each region. Unadjusted and adjusted associations (Aim 2) between contextual characteristics and Black IMR were examined using aggregated county-level Poisson regression of deaths over birth counts with standard errors adjusted for clustering by state through generalized estimating equations [62]. This type of aggregated analysis offers a more efficient data structure with identical results as those obtained by linking individual observations to county or state characteristics [63]. Each county was linked to various county and state covariates. Relative rate ratios (RR) and absolute rate differences were estimated through average marginal prediction contrasts [64] and calculated relative to a reference for categorical variables and per standard deviation (SD)and mean plus SD for continuous variables, respectively. We compared unadjusted and model-adjusted region-level IMRs to estimate regional variation before and after adjustment and the proportion attributable to model characteristics (Aim 3). We used simple variance formulas for fixed differences rather than a random effects approach given the small number of regional units for reliable random effects variance estimation [62, 65]. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and SAS-callable SUDAAN 11.0.1 (RTI International, Research Triangle Park, NC).
Results
Regional variation in Black IMR
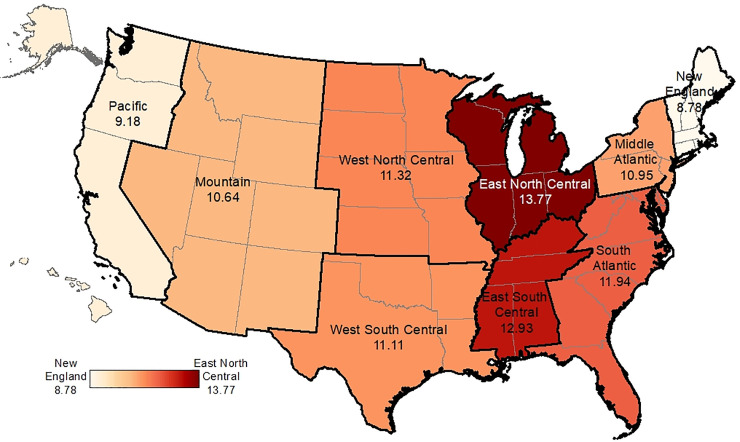
The overall Black IMR was 11.78 per 1,000, which varied 1.5-fold across regions (Table 1, Fig 1). Black IMR was lowest in New England and Pacific regions (8.78 and 9.19 per 1,000) and highest in East North Central and East South Central (13.77 and 12.92 per 1,000, respectively). Black births were not evenly distributed across the regions, with fewer births in areas where IMR was lower, ranging from about 2% in New England and the Pacific to over 30% in the South Atlantic.
Table 1. Black births, deaths and infant mortality rate by region, 2009–2011.
| Variable | Overall | New England (1) | Middle Atlantic (2) | East North Central (3) | West North Central (4) | South Atlantic (5) | East South Central (6) | West South Central (7) | Mountain (8) | Pacific (9) |
|---|---|---|---|---|---|---|---|---|---|---|
| Deaths | 20959 | 359 | 2545 | 3740 | 852 | 7118 | 2272 | 2701 | 388 | 985 |
| Births | 1778528 | 40867 | 232436 | 271546 | 75263 | 595902 | 175771 | 243045 | 36451 | 107246 |
| Black IMR | 11.78 | 8.78 | 10.95 | 13.77 | 11.32 | 11.94 | 12.93 | 11.11 | 10.64 | 9.18 |
| Percent of Deaths by Region | 1.71 | 12.14 | 17.84 | 4.07 | 33.96 | 10.84 | 12.89 | 1.85 | 4.70 | |
| Percent of Births by Region | 2.30 | 13.07 | 15.27 | 4.23 | 33.51 | 9.88 | 13.67 | 2.05 | 6.03 |
Abbreviations: IMR, infant mortality rate.
Fig 1. Black infant mortality rates per 1,000 live births by region, 2009–2011.
The overall Black IMR was 11.78 per 1,000, which varied 1.5-fold across regions ranging from 8.78 deaths per 1,000 in New England to 13.77 deaths per 1,000 in the East North Central region. The basemap (shapefile) was retrieved from Census TIGER/Line https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html and the color scheme is an option within ESRI ArcGIS Desktop https://www.esri.com/en-us/arcgis/products/arcgis-desktop/overview.
Regional variation in contextual factors
All covariates differed by region (Table 2). Variables with the largest variation by region, with coefficients of variation exceeding 50%, included the state-level non-Hispanic Black percentage, the state-level Black-White marriage rate, county hypersegregation, rurality, and the annual state MCH budget per capita. The average state non-Hispanic Black percentage was 17.3% and ranged from approximately 5% in Mountain and Pacific Regions to approximately 25% in the South Atlantic and East South Central. The average state percentage of Black marriages to Whites was 6.0% ranging from 3.3% in East South Central to 16.9% in the Mountain region. Overall, about 20% of Black births occurred in hypersegregated counties with high dissimilarity and isolation (Table 2). The East North Central and Middle Atlantic regions had the highest hypersegregation, where approximately 40–50% of births occurred in hypersegregated counties. By contrast, there were no hypersegregated counties in New England, Mountain, and Pacific regions. Overall, 9.9% of Black births occurred in rural counties, which ranged from under 2% in New England, Middle Atlantic, and East North Central regions to 28.6% in East South Central. The average annual state MCH budget per capita was about $16, ranging from under $3 in West North Central and Mountain regions to nearly $60 in the Pacific region.
Table 2. Descriptive statistics and variation by region, 2009–2011.
| Mean (SD) by Region, weighted by births | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean (SD) Overall | CV by Region | New England (1) | Middle Atlantic (2) | East North Central (3) | West North Central (4) | South Atlantic (5) | East South Central (6) | West South Central (7) | Mountain (8) | Pacific (9) |
| Social | |||||||||||
| Percent Non-Hispanic Black Population | 17.31 (9.21) | 56% | 6.86 (2.15) | 12.96 (1.66) | 12.44 (2.45) | 7.83 (3.47) | 23.65 (7.36) | 24.96 (9.55) | 17.68 (9.39) | 4.64 (2.15) | 5.4 (1.02) |
| Black-White marriage rate | 5.97 (4.44) | 54% | 12.35 (7.6) | 5.55 (1.49) | 7.02 (2.11) | 13.69 (6.44) | 3.94 (1.57) | 3.33 (2.55) | 4.2 (2.21) | 16.86 (6.84) | 12.25 (5.18) |
| Segregation Index | |||||||||||
| Both dissimilarity and isolation <0.6 | 64.70 | 31% | 76.20 | 40.43 | 36.79 | 73.55 | 71.78 | 54.82 | 83.36 | 99.99 | 99.93 |
| One index > = 0.6 | 14.06 | 78% | 23.80 | 17.89 | 11.61 | 0.48 | 16.41 | 23.42 | 11.43 | 0.01 | 0.07 |
| Both indices > = 0.6 | 21.24 | 103% | 0.00 | 41.67 | 51.60 | 25.97 | 11.81 | 21.76 | 5.21 | 0.00 | 0.00 |
| Black incarceration rate (per 100,000 in adult population) | 2324.31 (604.41) | 18% | 1815.56 (357.73) | 2167.93 (687.82) | 2412.82 (511.7) | 2558.89 (465.89) | 2073.73 (527.93) | 1996.64 (493.75) | 2841.42 (270.29) | 3094.99 (407.17) | 2963.89 (216.53) |
| Percent of voting age population casting votes for 2008 presidential electors | 64 (4.48) | 4% | 67.32 (0.87) | 60.91 (2.25) | 65.03 (2.99) | 68.33 (4.22) | 65.98 (2.45) | 62.72 (5.48) | 60.31 (6.61) | 61.95 (4.13) | 63.93 (1.28) |
| Economic | |||||||||||
| Black Index of Concentration at the Extremes | -0.26 (0.17) | 32% | -0.16 (0.1) | -0.19 (0.17) | -0.34 (0.11) | -0.34 (0.14) | -0.23 (0.19) | -0.38 (0.11) | -0.29 (0.15) | -0.2 (0.09) | -0.15 (0.11) |
| Black Civilian Unemployment Rate | 16.27 (4.27) | 12% | 15.45 (3.13) | 15.36 (2.89) | 20.61 (4.19) | 17.34 (4.54) | 15.56 (3.77) | 16.45 (4.54) | 13.44 (3.22) | 15.2 (3.44) | 17.19 (2.94) |
| Environment | |||||||||||
| Daily Fine Particulate Matter | 11.88 (1.41) | 11% | 10.91 (0.11) | 11.47 (0.72) | 12.97 (0.33) | 11.52 (1.43) | 12.51 (0.64) | 12.73 (0.53) | 10.72 (1.03) | 11.56 (1.79) | 8.45 (1.3) |
| Grocery Stores per 1,000 population in 2009 | 0.22 (0.12) | 36% | 0.21 (0.04) | 0.42 (0.2) | 0.21 (0.05) | 0.18 (0.07) | 0.2 (0.06) | 0.18 (0.06) | 0.18 (0.08) | 0.13 (0.02) | 0.21 (0.04) |
| Housing Unit Vacancy Percent | 10.6 (4.44) | 17% | 7.78 (4.24) | 8.19 (3.29) | 10.41 (2.57) | 9.4 (4.3) |
12.07 (5.29) | 11.64 (3.21) | 10.71 (4.25) | 11.92 (4.31) | 7.68 (2.69) |
| Rural Urban Classification | |||||||||||
| Large urban counties | 64.34 | 23% | 62.69 | 86.98 | 73.98 | 67.64 | 58.82 | 36.76 | 53.68 | 77.99 | 84.53 |
| Small and medium urban counties | 25.75 | 33% | 36.04 | 11.88 | 24.21 | 24.19 | 28.80 | 34.63 | 31.56 | 18.06 | 14.79 |
| Rural counties | 9.92 | 108% | 1.27 | 1.14 | 1.81 | 8.17 | 12.38 | 28.61 | 14.76 | 3.95 | 0.68 |
| Health | |||||||||||
| Medicaid eligibility for pregnant women as % FPL | 192.19 (29.6) | 11% | 216.44 (25.2) | 192.7 (7.5) | 203.99 (28.33) | 211.57 (50.5) | 193.41 (33.66) | 168.61 (24.16) | 187.4 (10.49) | 142.91 (20.46) | 197.77 (5.33) |
| Maternal and child health budget per person/capita | 15.84 (17.65) | 110% | 6.19 (4.07) | 28.93 (20.41) | 10.67 (6.84) | 2.53 (0.59) | 15.22 (11.97) | 9.18 (6.86) | 4.74 (2.47) | 2.98 (3.6) |
57.55 (22.3) |
| Certified Nurse Midwives per 100,000 women ages 15–44 | 19.44 (14.73) | 41% | 39.41 (13.33) | 25.52 (10.22) | 20.07 (10.05) | 19.28 (15.86) | 22.92 (16.25) | 10.77 (12.58) | 7.81 (7.82) | 21.95 (18.26) | 17.55 (12.61) |
| Obstetricians/Gynecologists per 100,000 women ages 15–44 | 67.52 (33.83) | 14% | 87.03 (27.5) | 71.8 (34.59) | 73.66 (26.53) | 74.07 (34.11) | 65.62 (37.67) | 65 (35.83) | 64.59 (33.48) | 55.72 (20.28) | 56.03 (17.05) |
| Percent Uninsured Females 18–44 years | 22.36 (7.56) | 29% | 8.53 (4.45) | 16.91 (4.23) | 18.18 (3.62) | 17.57 (6.2) | 24.05 (7.35) | 22.61 (4.81) | 30.75 (6.36) | 24.43 (4.31) | 23.82 (5.3) |
SD = Standard Deviation CV = Coefficient of Variation FPL = Federal Poverty Level.
Contextual associations with Black IMR
The following factors were associated with Black IMR in unadjusted models: Black-White marriage rate, Black ICE, Black unemployment, daily fine particulate matter, housing vacancy, rural/urban classification, and MCH budget per capita (Table 3). After adjustment, only the Black-White marriage rate, Black ICE, and MCH budget per capita remained associated. The Black-White marriage rate and Black ICE also had the largest adjusted associations. For every one SD increase in the state percentage of married Black individuals with White spouses (SD: 14%, not shown in tables), the Black IMR decreased by 19% (adjusted RR: 0.81, 95% confidence interval (CI):0.70–0.95), corresponding to two fewer deaths per 1,000 births. For every one SD increase in the county Black ICE(SD: 0.3, not shown in tables), the Black IMR was 15% lower (adjusted RR: 0.85, 95% CI:0.81–0.90), corresponding to 1.7 fewer deaths per 1,000 births. The adjusted RR of 0.96 (95% CI:0.92–0.99) for the state MCH budget per capita indicates that for every one SD increase (SD: $13 per capita, not shown in tables), the Black IMR decreased by 4%.
Table 3. Unadjusted and adjusted associations (rate ratio and rate difference) between contextual factors and the Black infant mortality rate, 2009–2011.
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| Variable | Rate Ratio (RR) (per SD continuous variables) with 95% CI | Rate Difference (RD) (mean + 1SD) per 1,000 with 95% CI | P-value Wald F | Rate Ratio (RR) (per SD continuous variables) with 95% CI | Rate Difference (RD) (mean + 1SD) per 1,000 with 95% CI | P-value Wald F |
| Social | ||||||
| Percent Non-Hispanic Black Population | 1.04 (0.98, 1.1) | 0.44 (-0.05, 0.93) | 0.18 | 0.95 (0.88, 1.04) | -0.56 (-1.22, 0.10) | 0.25 |
| Black-White marriage rate | 0.88 (0.77, 1.00) | -1.34 (-2.56, -0.12) | 0.05 | 0.81 (0.70, 0.95) | -1.97 (-3.09, -0.85) | 0.01 |
| Segregation Index | 0.23 | 0.64 | ||||
| Both dissimilarity and isolation <0.6 | ref | ref | ref | ref | ||
| One index > = 0.6 | 1.08 (0.97, 1.21) | 0.93 (-0.40, 2.26) | 1.03 (0.93, 1.13) | 0.33 (-0.77, 1.43) | ||
| Both indices > = 0.6 | 1.07 (0.95, 1.20) | 0.79 (-0.58, 2.16) | 1.03 (0.96, 1.12) | 0.39 (-0.49, 1.27) | ||
| Black incarceration rate (per 100,000 in adult population) | 0.98 (0.90, 1.07) | -0.24 (-0.92, 0.44) | 0.63 | 0.97 (0.90, 1.04) | -0.37 (-0.93, 0.19) | 0.34 |
| Percent of voting age population casting votes for 2008 presidential electors | 1.04 (0.99, 1.09) | 0.46 (-0.04, 0.96) | 0.15 | 1.02 (0.97, 1.07) | 0.20 (-0.46, 0.86) | 0.47 |
| Economic | ||||||
| Black Index of Concentration at the Extremes | 0.84 (0.79, 0.90) | -1.93 (-2.42, -1.44) | 0.00 | 0.85 (0.81, 0.90) | -1.66 (-2.2, -1.12) | 0.00 |
| Black Civilian Unemployment Rate | 1.22 (1.13, 1.31) | 2.55 (1.94, 3.16) | 0.00 | 1.00 (0.92, 1.08) | -0.05 (-0.67, 0.57) | 0.92 |
| Environment | ||||||
| Daily Fine Particulate Matter | 1.08 (1.04, 1.13) | 0.99 (0.49, 1.49) | 0.00 | 0.98 (0.92, 1.04) | -0.28 (-0.95, 0.39) | 0.42 |
| Grocery Stores per 1,000 population in 2009 | 0.96 (0.90, 1.02) | -0.48 (-1.02, 0.06) | 0.19 | 0.96 (0.91, 1.01) | -0.49 (-1.13, 0.15) | 0.11 |
| Housing Unit Vacancy Percent | 1.09 (1.03, 1.15) | 1.08 (0.39, 1.77) | 0.01 | 1.01 (0.97, 1.06) | 0.15 (-0.44, 0.74) | 0.52 |
| Rural Urban Classification | 0.00 | 0.22 | ||||
| Large urban counties | ref | ref | ref | ref | ||
| Small and medium urban counties | 1.12 (1.06, 1.20) | 1.40 (0.69, 2.11) | 1.05 (0.98, 1.13) | 0.60 (-0.14, 1.34) | ||
| Rural counties | 1.10 (1.00, 1.21) | 1.11 (0.01, 2.21) | 1.01 (0.92, 1.11) | 0.09 (-0.95, 1.13) | ||
| Health | ||||||
| Medicaid eligibility for pregnant women as % FPL | 0.98 (0.93, 1.03) | -0.23 (-0.77, 0.31) | 0.43 | 1.01 (0.96, 1.06) | 0.08 (-0.52, 0.68) | 0.78 |
| Maternal and child health budget per person/capita | 0.95 (0.93, 0.97) | -0.56 (-0.91, -0.21) | 0.00 | 0.96 (0.92, 0.99) | -0.51 (-1.07, 0.05) | 0.02 |
| Certified Nurse Midwives per 100,000 women ages 15–44 | 0.97 (0.91, 1.03) | -0.38 (-0.93, 0.17) | 0.29 | 0.97 (0.93, 1.00) | -0.38 (-0.95, 0.19) | 0.05 |
| Obstetricians/Gynecologists per 100,000 women ages 15–44 | 1.02 (0.99, 1.05) | 0.22 (-0.26, 0.70) | 0.26 | 1.02 (0.99, 1.06) | 0.25 (-0.28, 0.78) | 0.21 |
| Percent Uninsured Females 18–44 years | 0.98 (0.94, 1.03) | -0.22 (-0.68, 0.24) | 0.41 | 0.95 (0.91, 1.00) | -0.52 (-1.09, 0.05) | 0.08 |
| Geographic Region | ||||||
| Census Division | 0.00 | 0.06 | ||||
| New England (1) | 0.64 (0.48, 0.84) | -5.00 (-7.39, -2.61) | 0.67 (0.49, 0.90) | -4.30 (-6.93, -1.67) | ||
| Middle Atlantic (2) | 0.79 (0.69, 0.92) | -2.80 (-4.37, -1.23) | 0.95 (0.85, 1.06) | -0.60 (-1.93, 0.73) | ||
| East North Central (3) | ref | ref | ref | ref | ||
| West North Central (4) | 0.82 (0.69, 0.98) | -2.50 (-4.48, -0.52) | 0.83 (0.70, 0.98) | -2.10 (-3.94, -0.26) | ||
| South Atlantic (5) | 0.87 (0.8, 0.94) | -1.80 (-2.70, -0.90) | 0.95 (0.86, 1.05) | -0.60 (-1.80, 0.60) | ||
| East South Central (6) | 0.94 (0.88, 1.00) | -0.80 (-1.58, -0.02) | 0.91 (0.81, 1.03) | -1.10 (-2.57, 0.37) | ||
| West South Central (7) | 0.81 (0.75, 0.87) | -2.70 (-3.54, -1.86) | 0.83 (0.70, 0.97) | -2.20 (-4.00, -0.40) | ||
| Mountain (8) | 0.77 (0.67, 0.89) | -3.10 (-4.57, -1.63) | 0.95 (0.75, 1.20) | -0.70 (-3.50, 2.10) | ||
| Pacific (9) | 0.67 (0.61, 0.73) | -4.60 (-5.44, -3.76) | 0.92 (0.68, 1.24) | -1.10 (-4.53, 2.33) | ||
SD = standard deviation, FPL = federal Poverty Level, CI = confidence interval.
Regional variation explained by contextual factors
The regional variance in Black IMR decreased from 2.28 before adjustment to 1.48 after adjustment, representing a 35% reduction. (Table 4) There were five regions that had sizeable changes between unadjusted and adjusted IMRs, with differences exceeding 1 death per 1,000. The East North Central and East South Central regions had the highest unadjusted IMRs and had the largest decreases in IMR after adjustment. The Pacific, Mountain, and Middle Atlantic regions had large increases in Black IMR after adjustment. The South Atlantic and New England regions had the smallest changes in Black IMR after adjustment.
Table 4. Unadjusted and adjusted Black infant mortality rate by region and variance explained, 2009–2011.
| Region | Unadjusted IMR | Adjusted IMR | Percent change | Absolute change |
|---|---|---|---|---|
| New England (1) | 8.78 (6.67, 11.54) | 8.46 (6.26, 11.44) | -3.64% | -0.32 |
| Middle Atlantic (2) | 10.95 (9.52, 12.59) | 12.08 (11.12, 13.12) | 10.32% | 1.13 |
| East North Central (3) | 13.77 (13.3, 14.25) | 12.72 (11.61, 13.93) | -7.63% | -1.05 |
| West North Central (4) | 11.32 (9.5, 13.49) | 10.57 (9.15, 12.21) | -6.63% | -0.75 |
| South Atlantic (5) | 11.94 (11.17, 12.77) | 12.11 (11.12, 13.18) | 1.42% | 0.17 |
| East South Central (6) | 12.92 (12.29, 13.59) | 11.6 (10.53, 12.78) | -10.22% | -1.32 |
| West South Central (7) | 11.11 (10.43, 11.85) | 10.52 (9.38, 11.81) | -5.31% | -0.59 |
| Mountain (8) | 10.63 (9.3, 12.14) | 12.06 (9.92, 14.65) | 13.45% | 1.43 |
| Pacific (9) | 9.19 (8.52, 9.92) | 11.66 (8.87, 15.34) | 26.88% | 2.47 |
| Proportion of variance explained | ||||
| Variance | 2.28 | 1.48 | -35% | |
IMR = Infant mortality rate.
Discussion
The results from this state and county contextual examination of Black infant mortality revealed that the Black-White marriage rate, MCH budget per capita, and Black ICE explained approximately one-third of the regional variation in the Black IMR. The East North Central (the Midwest) and East South Central regions had the highest unadjusted Black IMR and had the largest decreases in Black IMR after adjustment, indicating that modeled covariates captured some of the contextual factors associated with their regional disadvantage. The Pacific, Mountain, and Middle Atlantic regions all had large increases in Black IMR after adjustment, indicating that these regions had certain advantages explained by the model. However, the New England IMR advantage was not explained by model covariates. Each of the three protective factors we identified represent distinct potential policy avenues to improve social integration, public health spending, and household income. These factors may inform state and local efforts to reduce Black IMR as well as potential multi-state regional action collaboratives [25].
In adjusted models, the state-level Black-White marriage rate was associated with the greatest relative risk reduction in Black IMR. The Black-White marriage rate can be viewed as a measure of inter-racial social intimacy and integration, where the majority and minority groups view each other with greater equality, familiarity, and trust [29]. Structural and social conditions, including residential segregation, interpersonal discrimination, and anti-miscegenation laws, have led to a history of prohibition against interracial marriage [34]. Thus, this measure can also be viewed more broadly as a reflection of racial intergroup acceptance, and the converse of multiple dimensions of racism—structural, cultural, and interpersonal. Changes in interracial marriage trends by region over time may reflect a counter measure of “latent” racism [35]. While other related contextual measures of racism, such as residential segregation or Black-White inequalities in education, income, and employment, have been associated with adverse Black birth outcomes [4, 23, 41, 66–68], the state-level Black-White marriage rate could be considered a novel positive indicator of integration in general. Although county-level hypersegregation was not associated with Black IMR before or after adjustment, more studies indicate an association with birth outcomes when measured at the census tract or Metropolitan Statistical Area (MSA) level [23, 69, 70].
It has been posited that increasing social expenditures, such as state MCH budgetary expenditures, may reduce IMR and racial disparities in IMR [71]. State MCH expenditures are part of the Title V MCH Block Grant with an expressed mission that includes reducing infant mortality and ensuring access to quality health services for vulnerable populations with lower incomes. Our novel finding associating higher state MCH expenditures with lower Black infant mortality is consistent with other evidence at both state and local-levels that have linked public health expenditures with infant health and birth outcomes [16, 53, 54, 72–76]. A recent Florida study that examined county-level MCH expenditures and infant mortality found that greater spending was associated with reductions in IMR, especially for the Black population, which may have a greater need and benefit from funded public health and social services [74]. Importantly, many prior studies controlled for state or county fixed effects to account for other unobserved differences that may be associated with increased public health spending [16, 54, 74, 76].
Higher Black ICE was also associated with lower Black IMR, consistent with a growing body of literature connecting ICE with birth outcomes at both county and city levels [18, 19, 41]. Unlike other economic measures, such as poverty, household income, or income inequality, ICE captures both privilege and deprivation and the relative balance between the two [20, 77]. Another version of ICE that captures racial economic polarization [19] was examined but was not associated with Black IMR after adjustment, perhaps due to other related measures such as Black-White marriage rates.
Limitations
A variety of other social, economic, environmental, and health characteristics were not associated with regional Black IMR in the mutually adjusted model, which may reflect high correlation between measures, and a combination of lack of content association and poor measurement. Several variables could only be measured at the state rather than county level (e.g. incarceration rates) and some were not measured specifically within the Black-community (e.g. voting percentages). This study posits substantial room for further development and contextual exploration of race-specific measures assessed at more granular geographic levels. Despite their persistent associations with the outcome, state MCH expenditures and the Black-White marriage rate also have limitations. State MCH expenditures were not specific to those related to women’s or infant health versus children’s health investments. For Black-White marriage, the restriction to married couples in an era of declining marriage [78] may reflect a measure of racial integration among higher socioeconomic status groups. It is also sensitive to same race partner availability, although we controlled for the percent of non-Hispanic Black population. In addition, state-level Black-White marriage may reflect mixed race on an individual-level or paternal White race, which is associated with better birth outcomes compared to single race Black and paternal Black race. While evidence suggests that this reflects social rather than genetic contributions [21], future research could explore the association of state-level Black-White marriage with birth outcomes among single race Black mothers and fathers. All states adopted the 2003 birth certificate revision that distinguishes single and multiple race as of 2016 with the first year of complete 2017 infant mortality follow-up released in 2019. Although more recent infant mortality data are available, we relied on the 2010 Census for several variables and IMR has not changed substantially; thus, results are still relevant.
There are also broader limitations of the study’s overall approach. The cross-sectional design limits assessment of causal relations. Only associations can be documented, which are subject to confounding by unmeasured policies and characteristics. Some conceptual contextual measures (e.g. racism, segregation, etc.) are difficult to operationalize and therefore may have been imprecisely measured. Variables may also operate at a different or more granular level than available in national vital records (e.g. neighborhood level). Further, individual characteristics were not included in the ecological models, though they are likely to mediate the contextual effects that were of primary interest. Finally, aggregating geographic units (counties into states into regions) can create a modifiable areal unit problem in which results depend on the boundaries and definitions applied. Although counties and states hold specific administrative and policy functions with standard boundaries, we selected the Census Bureau groupings of states into regions based on similar population characteristics, economic, and historical development [27], which also appeared to fit Black IMR patterns.
Implications
Conceptually, our approach addresses the contextual contributions to poor birth outcomes rather than individual behaviors, personal, health or genetic characteristics. Further longitudinal research to examine changes in contextual factors in relation to changes in outcomes would significantly strengthen inference. Additional research could also enhance and refine measurement at multiple scales to explain more of the variation in Black IMR and examine other adverse birth outcomes.
Programs to improve racial integration and economic opportunity may require policy and programmatic interventions, preferentially targeted to populations experiencing the worst outcomes. Placed-based transformations, such as Best Babies Zones, free college education, and paid parental leave, reflect efforts to address income inequality and structural racism [79–83]. The concentration of poverty within the Black community, a product of discrimination and unequal opportunity, remains a very serious problem for optimal reproductive health [84].
Conclusions
This study is part of the continuing efforts to understand the roots of the unacceptably high Black IMR in the United States. Three contextual factors, state Black-White marriage rate, county Black ICE, and state MCH budget, were strongly and independently associated with Black IMR, accounting for over a third of regional variation. These associations encourage continuing efforts to improve social integration across racial groups, increase public spending on MCH health and services programs, and address income disparities that together may influence Black IMR. Additional contextual research is needed to advance knowledge of causation and understanding of regional and other variations in poor reproductive outcomes within the heterogeneous Black community.
Supporting information
(DOCX)
(DOCX)
Data Availability
Data on infant births and deaths cannot be shared publicly because the data release policy for Vital Statistics Micro-data files indicates that the public use file does not have geographic identifiers. In order to do a regional analysis, restricted-use files for Linked Births/Infant Deaths were requested. Instructions on how to access the restricted data is available from the National Vital Statistics System at https://www.cdc.gov/nchs/nvss/nvss-restricted-data.htm. Data on contextual factors was retrieved from multiple publicly available sources listed in Appendix A of the manuscript. The data source for each variable is not linked, as the data set was created with variables that matched with the outcome of infant mortality based on county or state identifiers. This cannot be made publicly available since it contains protected information about geographic locations for the Linked Infant Birth/Death records.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Mathews TJ ED, Driscoll AK. State variations in infant mortality by race and Hispanic origin of mother, 2013–2015. Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- 2.Bird ST. Separate Black and White infant mortality models: differences in the importance of structural variables. Soc Sci Med. 1995;41(11):1507–12. Epub 1995/12/01. 10.1016/0277-9536(95)00029-7 . [DOI] [PubMed] [Google Scholar]
- 3.Rossen LM, Khan D, Schoendorf KC. Mapping geographic variation in infant mortality and related Black-White disparities in the US. Epidemiology. 2016;27(5):690–6. Epub 2016/05/20. 10.1097/EDE.0000000000000509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallace M, Crear-Perry J, Richardson L, Tarver M, Theall K. Separate and unequal: structural racism and infant mortality in the US. Health Place. 2017;45:140–4. Epub 2017/04/01. 10.1016/j.healthplace.2017.03.012 . [DOI] [PubMed] [Google Scholar]
- 5.Siddiqi A, Jones MK, Bruce DJ, Erwin PC. Do racial inequities in infant mortality correspond to variations in societal conditions? A study of state-level income inequality in the U.S., 1992–2007. Soc Sci Med. 2016;164:49–58. Epub 2016/07/30. 10.1016/j.socscimed.2016.07.013 . [DOI] [PubMed] [Google Scholar]
- 6.Brown Speights JS, Goldfarb SS, Wells BA, Beitsch L, Levine RS, Rust G. State-level progress in reducing the Black-White infant mortality gap, United States, 1999–2013. Am J Public Health. 2017;107(5):775–82. Epub 2017/03/23. 10.2105/AJPH.2017.303689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reno R, Hyder A. The evidence base for social determinants of health as risk factors for infant mortality: asystematic scoping review. J Health Care Poor Underserved. 2018;29(4):1188–208. Epub 2018/11/20. 10.1353/hpu.2018.0091 . [DOI] [PubMed] [Google Scholar]
- 8.Benmarhnia T, Huang J, Basu R, Wu J, Bruckner TA. Decomposition analysis of Black–White disparities in birth outcomes: the relative contribution of air pollution and social factors in California. Environmental Health Perspectives. 2017;125(10):107003 10.1289/EHP490 PMC5933346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nowak AL, Giurgescu C. The built environment and birth outcomes: asystematic review. MCN Am J Matern Child Nurs. 2017;42(1):14–20. Epub 2016/10/19. 10.1097/NMC.0000000000000299 . [DOI] [PubMed] [Google Scholar]
- 10.Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Soc Sci Med. 2005;60(10):2217–28. Epub 2005/03/08. 10.1016/j.socscimed.2004.10.010 . [DOI] [PubMed] [Google Scholar]
- 11.Chung H, Muntaner C. Political and welfare state determinants of infant and child health indicators: an analysis of wealthy countries. Soc Sci Med. 2006;63(3):829–42. 10.1016/j.socscimed.2006.01.030 . [DOI] [PubMed] [Google Scholar]
- 12.Gorman BK. Racial and ethnic variation in low birthweight in the United States: individual and contextual determinants. Health Place. 1999;5(3):195–207. Epub 2000/09/14. 10.1016/s1353-8292(99)00009-x . [DOI] [PubMed] [Google Scholar]
- 13.Wildeman C. Imprisonment and infant mortality. Social Problems. 2012;59(2):228–57. 10.1525/sp.2012.59.2.228 [DOI] [Google Scholar]
- 14.Heisler EJ. The U.S. infant mortality rate: international comparisons, underlying factors and federal programs. Congressional Research Service; Washington DC: 2011. 81–119 p. [Google Scholar]
- 15.Mays GP, Smith SA. Geographic variation in public health spending: correlates and consequences. Health Services Research. 2009;44(5 Pt 2):1796–817. 10.1111/j.1475-6773.2009.01014.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mays GPS, S.A. Evidence links increases in public health spending to declines in preventable deaths. Health Affairs. 2011;30(8):1585–93. 10.1377/hlthaff.2011.0196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wisdom JP, Berlin M, Lapidus JA. Relating health policy to women's health outcomes. Soc Sci Med. 2005;61(8):1776–84. Epub 2005/07/21. 10.1016/j.socscimed.2005.03.030 . [DOI] [PubMed] [Google Scholar]
- 18.Wallace M, Crear-Perry J, Theall K. Privilege and deprivation: associations between the Index of Concentration at the Extremes and birth equity in Detroit. Annals of Epidemiology. 2017;27(8):537 10.1016/j.annepidem.2017.07.057 [DOI] [Google Scholar]
- 19.Krieger N, Waterman PD, Batra N, Murphy JS, Dooley DP, Shah SN. Measures of local segregation for monitoring health inequities by local health departments. Am J Public Health. 2017;107(6):903–6. Epub 2017/04/21. 10.2105/AJPH.2017.303713 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the Index of Concentration at the Extremes. Am J Public Health. 2016;106(2):256–63. Epub 2015/12/23. 10.2105/AJPH.2015.302955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Sayed AM, Paczkowski M, Rutherford CG, Keyes KM, Galea S. Social environments, genetics, and Black-White disparities in infant mortality. Paediatr Perinat Epidemiol. 2015;29(6):546–51. Epub 2015/10/09. 10.1111/ppe.12227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hearst MO, Oakes JM, Johnson PJ. The effect of racial residential segregation on black infant mortality. Am J Epidemiol. 2008;168(11):1247–54. Epub 2008/11/01. 10.1093/aje/kwn291 . [DOI] [PubMed] [Google Scholar]
- 23.Mehra R, Boyd LM, Ickovics JR. Racial residential segregation and adverse birth outcomes: a systematic review and meta-analysis. Soc Sci Med. 2017;191:237–50. Epub 2017/09/25. 10.1016/j.socscimed.2017.09.018 . [DOI] [PubMed] [Google Scholar]
- 24.Williams AD, Wallace M, Nobles C, Mendola P. Racial residential segregation and racial disparities in stillbirth in the United States. Health Place. 2018;51:208–16. Epub 2018/05/02. 10.1016/j.healthplace.2018.04.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hirai AH, Sappenfield WM, Ghandour RM, Donahue S, Lee V, Lu MC. The Collaborative Improvement and Innovation Network (CoIIN) to Reduce Infant Mortality: an outcome evaluation from the US South, 2011 to 2014. American Journal of Public Health. 2018;108(6):815–21. Epub 2018/04/20. 10.2105/AJPH.2018.304371 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Linked Birth/Infant Death Records 2007–2015, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. [Internet]. [cited Jul 16, 2018]. Available from: http://wonder.cdc.gov/lbd-current.html
- 27.US Census Bureau. Statistical Groupings of States and Counties. In: US Department of Commerce, editor. Geographic Areas Reference Manual (GARM). Washington, DC: Geography Division, Bureau of the Census; 1994.
- 28.Hillemeier MM, Lynch J, Harper S, Casper M. Measuring contextual characteristics for community health. Health Services Research. 2003;38(6 Pt 2):1645–718. 10.1111/j.1475-6773.2003.00198.x PMC1360969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fryer RG Jr. Guess who's been coming to dinner? Trends in interracial marriage over the 20th century. Journal of Economic Perspectives. 2007;21(2):71–90. 10.1257/jep.21.2.71 [DOI] [Google Scholar]
- 30.Massey DS, Hajnal ZL. The changing geographic structure of Black-White segregation in the United States. Social Science Quarterly. 1995;76(3):527–42. [Google Scholar]
- 31.Massey DS, Tannen J. A research note on trends in Black hypersegregation. Demography. 2015;52(3):1025–34. 10.1007/s13524-015-0381-6 PMC4886656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Osypuk TL, Acevedo-Garcia D. Are racial disparities in preterm birth larger in hypersegregated areas? Am J Epidemiol. 2008;167(11):1295–304. Epub 2008/03/28. 10.1093/aje/kwn043 . [DOI] [PubMed] [Google Scholar]
- 33.Light MT, Marshall J. On the weak mortality returns of the prison boom: comparing infant mortality and homicide in the incarceration ledger. J Health Soc Behav. 2018;59(1):3–19. Epub 2017/12/29. 10.1177/0022146517748412 . [DOI] [PubMed] [Google Scholar]
- 34.Emens EF. Intimate discrimination: the state's role in the accidents of sex and love. Harvard Law Review. 2009;122(5):1307–402. [Google Scholar]
- 35.Gullickson A. Black/White interracial marriage trends, 1850–2000. Journal of Family History. 2006;31(3):289–312. 10.1177/0363199006288393 [DOI] [Google Scholar]
- 36.Massey DS, Denton NA. The dimensions of residential segregation. Social Forces. 1988;67(2):281–315. 10.2307/2579183 [DOI] [Google Scholar]
- 37.Iceland JW D.H.; Steinmetz E. Appendix B: Measures of residential segregation. Racial and Ethnic Residential Segregation in the United States: 1980–2000. Washington, DC: U.S. Government Printing Office; 2001. p. 119–23. [Google Scholar]
- 38.Johnston R, Poulsen M, Forrest J. Ethnic and racial segregation in U.S. metropolitan areas, 1980–2000: the dimensions of segregation revisited. Urban Affairs Review. 2007;42(4):479–504. 10.1177/1078087406292701 [DOI] [Google Scholar]
- 39.Reardon SF, O’Sullivan D. Measures of spatial segregation. Sociological Methodology. 2004;34(1):121–62. 10.1111/j.0081-1750.2004.00150.x [DOI] [Google Scholar]
- 40.Miranda ML, Messer LC, Kroeger GL. Associations between the quality of the residential built environment and pregnancy outcomes among women in North Carolina. Environ Health Perspect. 2012;120(3):471–7. Epub 2011/12/06. 10.1289/ehp.1103578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chambers BD, Baer RJ, McLemore MR, Jelliffe-Pawlowski LL. Using Index of Concentration at the Extremes as indicators of structural racism to evaluate the association with preterm birth and infant mortality-California, 2011–2012. J Urban Health. 2018. Epub 2018/06/06. 10.1007/s11524-018-0272-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paul DA, Mackley A, Locke RG, Stefano JL, Kroelinger C. State infant mortality: an ecologic study to determine modifiable risks and adjusted infant mortality rates. Matern Child Health J. 2009;13(3):343–8. Epub 2008/05/14. 10.1007/s10995-008-0358-9 . [DOI] [PubMed] [Google Scholar]
- 43.Bird ST, Bauman KE. The relationship between structural and health services variables and state-level infant mortality in the United States. Am J Public Health. 1995;85(1):26–9. Epub 1995/01/01. 10.2105/ajph.85.1.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Houston D, Li W, Wu J. Disparities in exposure to automobile and truck traffic and vehicle emissions near the Los Angeles–Long Beach Port Complex. American Journal of Public Health. 2014;104(1):156–64. 10.2105/AJPH.2012.301120 PMC3910024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones MR, Diez-Roux AV, Hajat A, Kershaw KN, O’Neill MS, Guallar E, et al. Race/ethnicity, residential segregation, and exposure to ambient air pollution: the Multi-Ethnic Study of Atherosclerosis (MESA). American Journal of Public Health. 2014;104(11):2130–7. 10.2105/AJPH.2014.302135 PMC4202969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gresham E, Byles JE, Bisquera A, Hure AJ. Effects of dietary interventions on neonatal and infant outcomes: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(5):1298–321. Epub 2014/10/22. 10.3945/ajcn.113.080655 . [DOI] [PubMed] [Google Scholar]
- 47.Lane SD, Keefe RH, Rubinstein R, Levandowski BA, Webster N, Cibula DA, et al. Structural violence, urban retail food markets, and low birth weight. Health Place. 2008;14(3):415–23. Epub 2007/10/12. 10.1016/j.healthplace.2007.08.008 . [DOI] [PubMed] [Google Scholar]
- 48.Anthopolos R, Kaufman JS, Messer LC, Miranda ML. Racial residential segregation and preterm birth: built environment as a mediator. Epidemiology. 2014;25(3):397–405. Epub 2014/04/01. 10.1097/EDE.0000000000000079 . [DOI] [PubMed] [Google Scholar]
- 49.Mohamoud YA, Kirby RS, Ehrenthal DB. Poverty, urban-rural classification and term infant mortality: a population-based multilevel analysis. BMC Pregnancy Childbirth. 2019;19(1):40 Epub 2019/01/24. 10.1186/s12884-019-2190-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ely DM, Hoyert DL. Differences Between Rural and Urban Areas in Mortality Rates for the Leading Causes of Infant Death: United States, 2013–2015. NCHS Data Brief. 2018;(300):1–8. Epub 2018/04/12. . [PubMed] [Google Scholar]
- 51.Currie J, Grogger J. Medicaid expansions and welfare contractions: offsetting effects on prenatal care and infant health? J Health Econ. 2002;21(2):313–35. Epub 2002/04/10. 10.1016/s0167-6296(01)00125-4 . [DOI] [PubMed] [Google Scholar]
- 52.Kaestner R, Lee WC. The effect of welfare reform on prenatal care and birth weight. Health Econ. 2005;14(5):497–511. Epub 2004/09/24. 10.1002/hec.921 . [DOI] [PubMed] [Google Scholar]
- 53.Becker ER, Teutsch SM. State maternal and child expenditures and low birthweight infants: a descriptive analysis. J Health Care Finance. 2000;27(1):1–10. Epub 2000/08/29. . [PubMed] [Google Scholar]
- 54.Bekemeier B, Yang Y, Dunbar MD, Pantazis A, Grembowski DE. Targeted health department expenditures benefit birth outcomes at the county level. Am J Prev Med. 2014;46(6):569–77. Epub 2014/05/21. 10.1016/j.amepre.2014.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.MacDorman MF, Declercq E. Trends and characteristics of United States out-of-hospital births 2004–2014: new information on risk status and access to care. Birth. 2016;43(2):116–24. 10.1111/birt.12228 [DOI] [PubMed] [Google Scholar]
- 56.Johantgen M, Fountain L, Zangaro G, Newhouse R, Stanik-Hutt J, White K. Comparison of labor and delivery care provided by certified nurse-midwives and physicians: a systematic review, 1990 to 2008. Womens Health Issues. 2012;22(1):e73–81. Epub 2011/08/26. 10.1016/j.whi.2011.06.005 . [DOI] [PubMed] [Google Scholar]
- 57.Vedam S, Stoll K, MacDorman M, Declercq E, Cramer R, Cheyney M, et al. Mapping integration of midwives across the United States: Impact on access, equity, and outcomes. PloS one. 2018;13(2):e0192523-e. 10.1371/journal.pone.0192523 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kozhimannil KB, Hung P, Henning-Smith C, Casey MM, Prasad S. Association between loss of hospital-based obstetric services and birth outcomes in rural counties in the United States, 2004–2014. JAMA. 2018;319(12):1239–47. 10.1001/jama.2018.1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shi L, Macinko J, Starfield B, Xu J, Regan J, Politzer R, et al. Primary care, infant mortality, and low birth weight in the states of the USA. Journal of Epidemiology and Community Health. 2004;58(5):374–80. 10.1136/jech.2003.013078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Larimore WL, Davis A. Relation of infant mortality to the availability of maternity care in rural Florida. J Am Board Fam Pract. 1995;8(5):392–9. Epub 1995/09/01. . [PubMed] [Google Scholar]
- 61.Straney LD, Lim SS, Murray CJ. Disentangling the effects of risk factors and clinical care on subnational variation in early neonatal mortality in the United States. PLoS One. 2012;7(11):e49399 Epub 2012/11/21. 10.1371/journal.pone.0049399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gardiner JC, Luo Z, Roman LA. Fixed effects, random effects and GEE: what are the differences? Statistics in medicine. 2009;28(2):221–39. 10.1002/sim.3478 . [DOI] [PubMed] [Google Scholar]
- 63.Loomis D, Richardson DB, Elliott L. Poisson regression analysis of ungrouped data. Occupational and Environmental Medicine. 2005;62(5):325–9. 10.1136/oem.2004.017459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Austin PC, Laupacis A. A tutorial on methods to estimating clinically and policy-meaningful measures of treatment effects in prospective observational studies: a review. Int J Biostat. 2011;7(1):6 Epub 2011/01/01. 10.2202/1557-4679.1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Snijders TAB, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. London; Thousand Oaks, Calif.: Sage Publications; 1999. viii, 266 p. [Google Scholar]
- 66.Chambers BD, Erausquin JT, Tanner AE, Nichols TR, Brown-Jeffy S. Testing the association between traditional and novel indicators of county-level structural racism and birth outcomes among Black and White women. J Racial Ethn Health Disparities. 2017. 10.1007/s40615-017-0444-z . [DOI] [PubMed] [Google Scholar]
- 67.Chae DH, Clouston S, Martz CD, Hatzenbuehler ML, Cooper HLF, Turpin R, et al. Area racism and birth outcomes among Blacks in the United States. Soc Sci Med. 2018;199:49–55. Epub 2017/04/30. 10.1016/j.socscimed.2017.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wallace ME, Mendola P, Liu D, Grantz KL. Joint effects of structural racism and income inequality on small-for-gestational-age birth. Am J Public Health. 2015;105(8):1681–8. Epub 2015/06/13. 10.2105/AJPH.2015.302613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mehra R, Keene DE, Kershaw TS, Ickovics JR, Warren JL. Racial and ethnic disparities in adverse birth outcomes: differences by racial residential segregation. SSM—population health. 2019;8:100417 Epub 2019/06/14. 10.1016/j.ssmph.2019.100417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sparks P, Sparks C, Campbell J. An application of Bayesian spatial statistical methods to the study of racial and poverty segregation and infant mortality rates in the US. GeoJournal. 2012. [Google Scholar]
- 71.Lorenz JM, Ananth CV, Polin RA, D'Alton ME. Infant mortality in the United States. Journal Of Perinatology. 2016;36:797 10.1038/jp.2016.63 [DOI] [PubMed] [Google Scholar]
- 72.Singh SR. Public health spending and population health: a systematic review. Am J Prev Med. 2014;47(5):634–40. Epub 2014/08/03. 10.1016/j.amepre.2014.05.017 . [DOI] [PubMed] [Google Scholar]
- 73.Bernet PM. Local public health agency funding: money begets money. J Public Health Manag Pract. 2007;13(2):188–93. Epub 2007/02/15. 10.1097/00124784-200703000-00016 . [DOI] [PubMed] [Google Scholar]
- 74.Bernet PM, Gumus G, Vishwasrao S. Effectiveness of public health spending on infant mortality in Florida, 2001–2014. Soc Sci Med. 2018;211:31–8. 10.1016/j.socscimed.2018.05.044 [DOI] [PubMed] [Google Scholar]
- 75.Becker ER, Principe K, Adams EK, Teutsch SM. Returns on investment in public health: effect of public health expenditures on infant health, 1983–1990. J Health Care Finance. 1998;25(1):5–18. Epub 1998/08/27. . [PubMed] [Google Scholar]
- 76.Bekemeier B, Grembowski D, Yang YR, Herting JR. Local public health delivery of maternal child health services: are specific activities associated with reductions in Black-White mortality disparities? Matern Child Health J. 2012;16(3):615–23. Epub 2011/04/21. 10.1007/s10995-011-0794-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Casciano R, Massey DS. Neighborhoods, employment, and welfare use: assessing the influence of neighborhood socioeconomic composition. Soc Sci Res. 2008;37(2):544–58. Epub 2008/12/17. 10.1016/j.ssresearch.2007.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cherlin AJ. American Marriage in the Early Twenty-First Century. The Future of Children. 2005;15(2):33–55. 10.1353/foc.2005.0015 [DOI] [PubMed] [Google Scholar]
- 79.Christopher G, Simpson P. Improving birth outcomes requires closing the racial gap. American Journal of Public Health. 2014;104 Suppl 1(Suppl 1):S10–S2. Epub 2014/02/. 10.2105/AJPH.2013.301817 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Taylor J NC, Hamm K, Phadke S. Eliminating racial disparities in maternal and infant mortality: a comprehensive policy blueprint. Center for American Progress, 2019. [Google Scholar]
- 81.Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63. Epub 2017/04/14. 10.1016/S0140-6736(17)30569-X . [DOI] [PubMed] [Google Scholar]
- 82.Williams DR, Mohammed SA. Racism and Health II: A needed research agenda for effective interventions. American Behavioral Scientist. 2013;57(8):1200–26. 10.1177/0002764213487341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pies C, Barr M, Strouse C, Kotelchuck M. Growing a Best Babies Zone: lessons learned from the pilot phase of a multi-sector, place-based initiative to reduce infant mortality. Matern Child Health J. 2016;20(5):968–73. Epub 2016/03/26. 10.1007/s10995-016-1969-1 . [DOI] [PubMed] [Google Scholar]
- 84.Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the Black-White gap in birth outcomes: a life-course approach. Ethnicity & disease. 2010;20(1 Suppl 2):S2–76. . [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
Data on infant births and deaths cannot be shared publicly because the data release policy for Vital Statistics Micro-data files indicates that the public use file does not have geographic identifiers. In order to do a regional analysis, restricted-use files for Linked Births/Infant Deaths were requested. Instructions on how to access the restricted data is available from the National Vital Statistics System at https://www.cdc.gov/nchs/nvss/nvss-restricted-data.htm. Data on contextual factors was retrieved from multiple publicly available sources listed in Appendix A of the manuscript. The data source for each variable is not linked, as the data set was created with variables that matched with the outcome of infant mortality based on county or state identifiers. This cannot be made publicly available since it contains protected information about geographic locations for the Linked Infant Birth/Death records.