Abstract
The persistence of the stape-dial artery is a rare vascular anomaly. It is mostly asymptomatic but sometimes cause conductive hearing loss, pulsatile tinnitus, or vertigo. The estimated prevalence of this rare postembryonic persistence ranged from 0.02% to 0.48%. Four different anatomical forms have been identified, and their preoperative diagnostic is essential. We report the case of an incidental discovery of pharyngo-hyo-stapedial artery, the most uncommon form of persistent stapedial artery. Its per-operative finding has become rare because tomodensitometry is performed in case of conductive hearing loss. The continuous improvement of imagery resolution will probably help to revise the incidence of this malformation.
Keywords: Ear, embryology, stapedial artery
INTRODUCTION
The stapedial artery is normally present during the development of the human embryo, and gives its stirrup shape to the stapes. The stapedial artery should normally regress at the seventh week of life, but its persistence after birth can occur. Hyrtl first described it in 1836. The estimated prevalence of this rare anomaly ranged from 0.02% to 0.48%. Four different anatomical forms of persistent stapedial artery have been identified, and their preoperative diagnostic is essential.
We report the case of an incidental discovery of pharyngo-hyo-stapedian artery, the most exceptional form of persistent stapedial artery.
CASE PRESENTATITON
A 24-year-old woman came to consultation for a long-standing pulsatile tinnitus, probably evolving since birth. Audiometry measurements showed conductive hearing loss on the right side (air-bone gap of 15 dB), and a normal left side. The otoscopic examination was normal.
A CT scan was performed to explore this unilateral pulsatile tinnitus. The temporal bone was normal on the left, but a vascular anomaly was detected on the right. The scanner showed a widening of the nerve of Jacobson foramen, ascending through a bony canal over the cochlear promontory (Figure 1) and joining an artery arising from a junction between the vertical and horizontal segments of the intra-petrous internal carotid artery (Figure 2). This artery continued upward, running through the stapes (Figure 3) and along the second part of the facial nerve, to exit in the middle skull base at the level of the geniculate ganglion (Figure 4). The foramen spinosum was absent on the right.
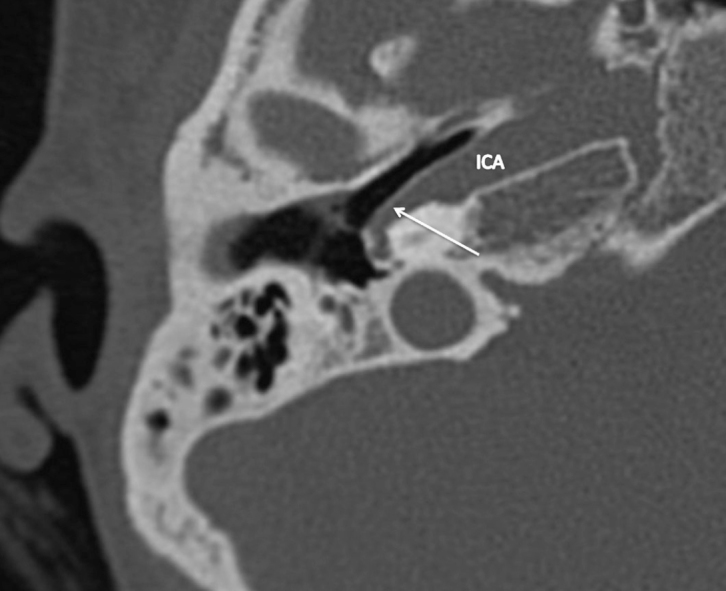
Figure 1.

Sagittal CT scan of right temporal bone showing an enlarged canal of the Jacobson’s nerve, ascending through a bony canal over the cochlear promontory (white arrow).
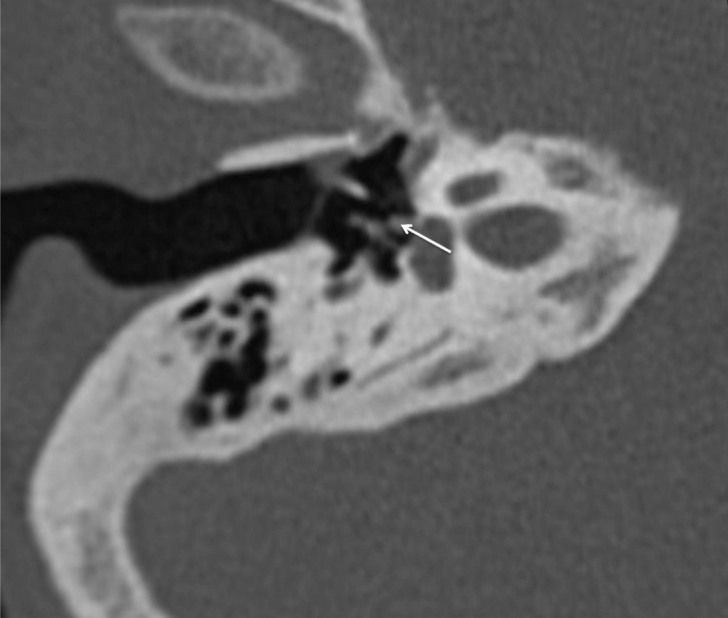
Figure 2.
Axial CT of the right temporal bone showing an artery (white arrow) arising from the junction between the vertical and horizontal segments of the intra-petrous internal carotid artery.
Figure 3.
Axial CT of the right temporal bone at the level of the stapes showing a persistent stapedial artery (white arrow).
Figure 4.
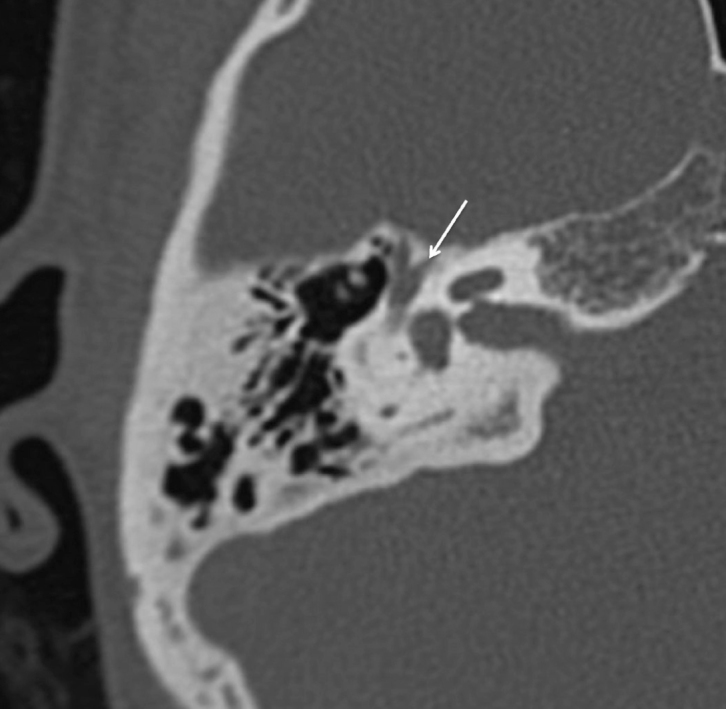
Axial CT scan of the right temporal bone at the level of the geniculate ganglion showing the exit of the persistent stapedial artery in the middle skull base (white arrow).
DISCUSSION
During the third week of gestation[1–2], the branchial arches arteries are formed, arising upward from the ventral aorta and ending backward on the dorsal aorta. During fetal development, six different arteries will be formed one after the other, from top to bottom. The ventral aorta will become the external carotid artery, and the dorsal aorta will become the internal carotid artery.
At six weeks, the stapedial artery arises from the hyoid artery (second arch) coming from the internal carotid artery and then divides into two branches: a superior one becoming the middle meningeal artery and an inferior one, toward the external carotid artery, running along the Jacobson nerve.
At seven weeks (Figure 5 A), the inferior branch of the stapedial artery has anastomosed with the external carotid artery. This anastomosis or pharyngeal artery will persist in its inferior part to create the inferior tympanic artery, which is a branch of the ascending pharyngeal artery.
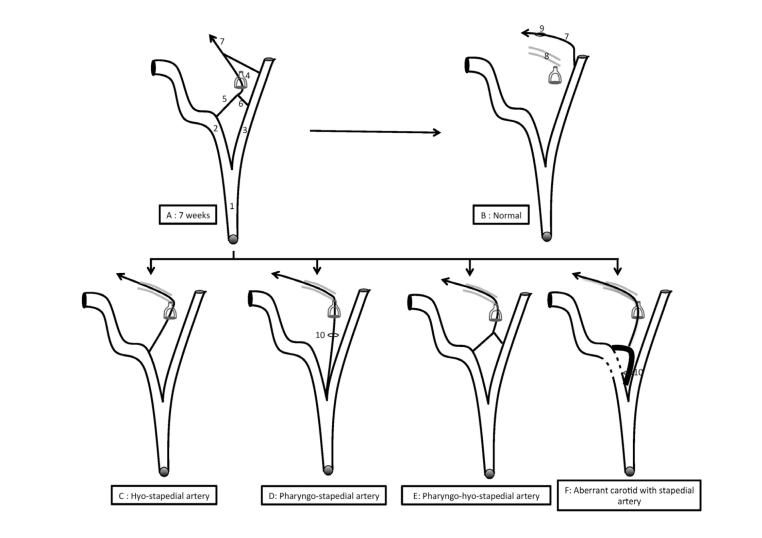
Figure 5. a–f.
Schematic representation of the embryology of the stapedial artery at seven weeks (a), its normal evolution (b), and the four anatomic variations (c, d, e, f).
- Common carotid artery
- Internal carotid artery
- External carotid artery
- Stapes
- Hyoid artery
- Pharyngeal artery
- Middle meningeal artery
- 2° portion of the fallopian canal
- Foramen spinosum
- Tympanic canaliculus
After seven weeks, the hyo-stapedial artery normally regresses, isolating the internal carotid artery from the middle meningeal artery arising then from the external carotid artery (Figure 5B). The hyo-stapedial artery will remain in the protympanum as the caroticotympanic artery.
The incidence of the stapedial artery persistence varies according to the series. It is described as 0.01%–0.02% of surgeries for otosclerosis[3] and as 0.48% of dissections reported by Moreano et al.[4]. To our knowledge, no radiological series have been published in the literature.
The so-called persistent stapedial artery has four different variants (Figure 5. C–F)[2–5]. The absence of foramen spinosum is common in all variants, the stapedial artery becoming then the middle meningeal artery arising in the middle skull base at the level of the geniculate ganglion. On the other hand, the absence of foramen spinosum is not necessarily correlated with a persistent stapedial artery because the middle meningeal artery can sometimes arise from the ophthalmic artery.
The four anatomical variants of the persistent stapedial artery are respectively (Figure 5. C–F):
-
- The hyoïdo-stapedial artery (Figure 5C)
The persistent stapedial artery directly arises from the intra-petrous internal carotid artery, enters into the tympanic cavity by the floor, and then runs along the promontory until passing between the two branches of the stapes. The artery then joins the fallopian canal in its second portion and then runs in the middle skull base at the level of geniculate ganglion to constitute the middle meningeal artery. Its persistence in this case is because the absence of development of the inferior branch of the stapedial artery at six weeks. In this case, the middle meningeal artery is a branch of the internal carotid artery.
-
- The pharyngo-stapedial artery (Figure 5D)
In this case, the pharyngeal artery may originate from the internal carotid artery or more frequently from the external carotid artery. It enters the tympanic cavity through the nerve of Jacobson, runs along the promontory, passes between the branches of the stapes, and then, as before, joins the fallopian canal to exit in the middle skull base at the level of the geniculate ganglion to constitute the middle meningeal artery. In this case, the middle meningeal artery is a branch of the ascending pharyngeal artery.
-
- The pharyngo-hyo-stapedial artery (Figure 5E).
This case, here presented, is a combination of the two previous forms: the stapedial artery comes from both the ascending pharyngeal artery and the hyoid artery (a direct branch of the internal carotid). There was no resorption, neither of the hyoid artery nor of the stapedial. This vascularization form is thus the closest form to the seventh week embryological.
This form is exceptional because until now, only one case had been described[6].
- The persistent stapedial artery associated with an aberrant internal carotid artery (Figure 5F).
In this case, the hyoid artery persists and replaces the vertical portion of the internal carotid artery.
From a clinical point of view, the persistence of the stapedial artery is usually asymptomatic, but it can sometimes cause conductive hearing loss because of stapes footplate blocking, pulsatile tinnitus, or vertigo.
Thus, imaging must be systematically performed in case of pulsatile tinnitus or conductive hearing loss with normal otoscopy. The scanner is the reference imaging exam.
In case of incidental per-operative finding, in particular for otosclerosis surgery, the usual attitude depends on the size of the vessel: if small and foot plate visible platinotomy can be done. In others cases, abstention is the rule, to avoid the occurrence of accidental hemorrhage during the platinotomy. In addition, cases of paralysis or facial paresis are described after intentional coagulation of the stapedial artery. Other authors have reported four cases of uncomplicated coagulation[3]. This surgical treatment could thus be proposed in the case of pulsatile tinnitus. The preoperative assessment should be supplemented by an arteriography or angio-MRI that will define the direction of circulation or confirm the diagnosis.
CONCLUSION
The persistence of the stapedial artery is a rare vascular anomaly mostly asymptomatic. Its per-operative finding has become rare because tomodensitometry is performed in case of conductive hearing loss testing with normal tympanic membrane. The continuous improvement of imagery resolution will probably make it possible to revise the incidence of this malformation.
Acknowledgements
We thank the woman described in this case for allowing us to share her details, and thank Laurence Curel for assistance in drawing submission process.
Footnotes
This study was presented at the “International Federation of Otorhinolaryngological Societies (IFOS) Congress”, 24-28 June 2017, Paris, France.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.S., F.C., J.M.; Design - M.S., F.C., J.M.;
Supervision: M.S., F.C., J.M.; Resource - M.S., F.C., J.M.; Materials - M.S., F.C.; Data Collection and/or Processing - M.S., F.C.; Analysis and/or Interpretation - M.S., F.C., J.M.; Literature Search - M.S., F.C.; Writing - M.S., F.C.; Critical Review - J.M.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Schuknecht HF, Gulya AJ. Anatomy of the temporal bone with surgical implications. Philadelphia: Lea and Febiger; 1995. [Google Scholar]
- 2.Hitier M, Zhang M, Labrousse M, Barbier C, Patron V, Moreau S. Persistent stapedial arteries in human: from phylogeny to surgical consequences. Surg Radiol Anat. 2013;35:883–91. doi: 10.1007/s00276-013-1127-z. [DOI] [PubMed] [Google Scholar]
- 3.Govaerts PJ, Marquet TF, Cremers C, Offeciers FE. Persistent stapedial artery: does it prevent successful surgery? Ann Otol Rhinol Laryngol. 1993;102:724–8. doi: 10.1177/000348949310200914. [DOI] [PubMed] [Google Scholar]
- 4.Moreano EH, Puparella MM, Zelterman D, Goycoolea MV. Prevalence of facial canal dehiscence and of persistent stapedial artery in the human middle ear: a report of 1000 temporal bones. Laryngoscope. 1994;104:309–20. doi: 10.1288/00005537-199403000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Altman F. Anomalies of the internal carotid artery and its branches; their embryological and comparative anatomical significance: report of a new case of persistent stapedial artery in man. Laryngoscope. 1947;57:313–39. doi: 10.1288/00005537-194705000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Lefournier V, Vasdev A, Bessou P, Boubagra K. A persistent pharyngohyostapedial artery: embryologic implications. AJNR Am J Neuroradiol. 1999;20:271–4. [PMC free article] [PubMed] [Google Scholar]