Abstract
OBJECTIVES
The objective of this study was to compare hearing results of fluoroplastic (Teflon) Causse Loop Piston with platinum/titanium (Big Easy) Piston in patients who underwent stapedotomy due to otosclerosis.
MATERIALS and METHODS
In this prospective randomized clinical trial study, Causse Loop Piston prosthesis was used in 76 ears and the Big Easy Piston prosthesis in 72 ears. The main outcomes were preoperative and postoperative pure tone audiometry and air-bone gap (ABG).
RESULTS
Postoperative ABG closure was not significantly different between both groups. However, the Causse Loop Piston resulted in a significant improvement of the air conduction (AC) in frequencies of 250, 500, and 1,000 Hz. In addition, the improvement of speech reception threshold (SRT) was significantly higher in Causse Loop Piston group.
CONCLUSION
We achieved similar postoperative ABG closure in short-term with both prostheses. However, at low frequencies, AC gain was higher in Causse Loop Piston group. In addition, patients in this group yielded better SRT.
Keywords: Otosclerosis, stapes surgery, ossicular prothesis, polytetrafluoroethylene, platinum, titanium
INTRODUCTION
In 1842, Kessel [1] reported the first stapes surgery. At that time, the procedure included either stapes mobilization or removal. In 1956, Shea [2] performed the first stapedectomy with Teflon prosthesis. A good prosthesis must be durable and provide acceptable hearing. The stapes prosthesis should not induce inflammatory reaction, and it has to be secured to long process of incus [3]. Nowadays, despite numerous material and design, piston style prosthesis such as Teflon Pistons with stainless steel or platinum wire loops are common types [3, 4]. In our center we have used the platinum/titanium Big Easy Piston for the past few years. It is a wire-piston prosthesis that is made of platinum in loop and shaft section and titanium in piston end. One of the clinical advantages of Big Easy Piston is the adequate opening of its loop with wide band and placement tab, which simplifies crimping it over the incus. In addition, it has a notch in the piston section that acts as a visual depth marker, which simplifies the placement of prosthesis into the vestibule.
Availability of numerous stapes prostheses in the market implies lake of consensus with respect to the ideal prosthesis. Hence, the advantage of one prosthesis over the other is still a gray area. Thus, we have decided to analyze the short-term stapedotomy results between fluoroplastic (Teflon) Causse Loop Piston and platinum/titanium (Big Easy) Piston.
MATERIALS AND METHODS
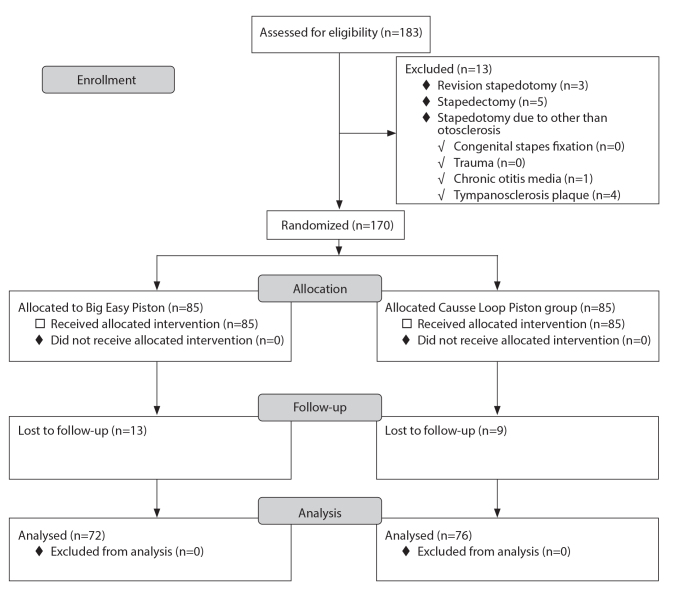
This single blind randomized clinical trial (RCT) study was carried out on ears that underwent stapedotomy between January 2012 and September 2017 at our referral otology center. The research protocol was reviewed and approved by the local university ethics committee (RCT code: IRCT2014011615496N3). All procedures were performed by the senior author. Informed consent was obtained from each patient. This trial protocol is summarized in the CONSORT flow diagram (Figure 1).
Figure 1.
CONSORT trial flow diagram.
At first, 183 ears that underwent primary stapedotomy were enrolled. Inclusion criteria were all patients who underwent primary stapedotomy, in whom we used Causse Loop Piston prosthesis or Big Easy Piston prosthesis. Exclusion criteria were all patients who had undergone revision stapedotomy and stapedectomy. In addition, patients who underwent stapedotomy for reasons other than otosclerosis, such as congenital stapes fixation, trauma, chronic otitis media, and tympanosclerosis plaque, were excluded. Patients with inadequate postoperative follow-up (less than 6 months) were also excluded. Finally, 170 patients were randomly classified into two groups. We used blocked randomization method on the basis of the type of prostheses—Causse Loop Piston prosthesis or Big Easy Piston prosthesis (both: Medtronic Xomed Surgical Products Inc., Jacksonville, FL, USA).
All surgical procedures were performed by trans-canal approach under local anesthesia (with injection of 1% lidocaine and 1:20,000 solution of epinephrine) and sedation with midazolam (5 mg, intravenous, administered 10 minutes before the procedure). The footplate was drilled by powered microdrill to the size of 0.7 mm. Fluoroplastic Causse Loop Piston (4 to 6 mm length, 0.6 mm diameter) or platinum/titanium Big Easy Piston (4 to 4.75 mm length, 0.5 mm diameter) was inserted between the long process of incus and oval window. The fenestrum was sealed with lobular fat. An independent otologist and audiometrist as assessors who examined the patients in postoperative period and checked hearing results were blinded to the study allocations. For evaluating hearing results, pure tone audiometry in 250, 500, 1,000, 2,000, and 4,000 Hz frequencies were checked. In our center, 3,000 Hz frequency as a usual audiometry is not evaluated. Therefore, the mean of 2,000 and 4,000 Hz frequencies was calculated, and the result was considered for 3,000 Hz frequency. In addition, air conduction (AC), bone conduction (BC), air-bone gap (ABG), preoperative and postoperative speech discrimination score (SDS), and speech reception threshold (SRT) were recorded. Preoperative audiogram was performed 1 week before the surgery. We analyzed the audiograms 6 months after the surgery.
Statistical Analysis
For statistical analysis, the Statistical Packages for the Social Sciences (SPSS) Statistics for Windows, version 18.0, (SPSS Inc., Chicago, IL, USA) was used. Chi-square test was used to compare categorical data. In addition, independent sample t-test or Mann-Whitney test was used to compare variables between groups, wherease paired t-test or Wilcoxon test was used to compare variables within groups. The p<0.05 were considered significant.
RESULTS
At first, 183 ears that had undergone stapedotomy were evaluated. As CONSORT diagram (Figure 1) shows, 13 ears were excluded because of other reasons such as revision stapedotomy, primary stapedectomy, fixation of stapes due to chronic otitis media, and tympanosclerosis plaque. Unequal number of ears within groups was a result of patients’ withdrawal—13 ears in Big Easy Piston group and 9 ears in Causse Loop Piston group were excluded. A total of 148 stapedotomies (in 125 patients) were included in our study. The Causse Loop Piston prosthesis was used in 76 stapedotomies. In this group, there were 38 (50%) men and 38 (50%) women with a mean age of 35.29±11.65 years. The Big Easy Piston prosthesis was used in 72 cases. This group consisted of 34 (47.2%) men and 38 (52.8%) women with a mean age of 33.31±10.33 years. The two groups were homogenous with respect to gender (p=0.735) and age (p=0.276) of the patients.
Analyses of preoperative and postoperative mean BC and AC in both groups are shown in Table 1. The two groups were homogeneous regarding preoperative mean BC and mean AC in frequencies of 500–3,000 Hz (p>0.05). Mean BC and mean AC in frequencies of 500–3,000 Hz had improved postoperatively in each prosthesis (p<0.05). We also compared the mean BC gain and mean AC gain in frequencies of 500–3,000 Hz between the two groups. Mean BC gain was not statistically significant in both the groups (p=0.104). However, Causse Loop Piston group statistically performed much better (4.2 dB more) than the Big Easy Piston group regarding mean AC gain (p=0.044), but it was not clinically significant.
Table 1.
Preoperative and postoperative mean BC and AC (dB) in frequencies of 500–3,000 Hz
| Preoperative | Postoperative | Gain | p | ||
|---|---|---|---|---|---|
| Mean BC (dB) | Causse Loop Piston | 13.6±7.3* | 6.6±5.7 | 7.0±8.8 | <0.0001 |
| Big Easy Piston | 12.8±6.5 | 7.9±5.9 | 4.9±6.6 | <0.0001 | |
| p-value | 0.483 | 0.175 | 0.104 | ||
| Mean AC (dB) | Causse Loop Piston | 46.9±11.7 | 17.7±10.0 | 29.2±12.6 | <0.0001 |
| Big Easy Piston | 45.2±9.9 | 20.2±10.1 | 25.0±12.5 | <0.0001 | |
| p-value | 0.343 | 0.132 | 0.044 |
Values are expressed as mean ±standard deviation (SD).
BC: bone conduction; AC: air conduction
Because preoperative AC, BC, and ABG in some frequencies were statistically significant between the two groups, the postoperative statistical analysis was not performed, and we only reported AC and BC gain and ABG closure to compare the two groups. Overall, in all frequencies, postoperative AC gain was higher in Causse Loop Piston group. In fact, Causse Loop Piston resulted in a significant AC gain at 250, 500, and 1,000 Hz frequencies when compared in the same frequencies with Big Easy Piston (p<0.05). In addition, postoperative gain in BC was not significantly different in each frequency in both the groups (p>0.05), except in 1,000 Hz frequency where Causse Loop Piston performed better. In fact, it was statistically borderline (p=0.05). Postoperative ABG closure was not significantly different in each frequency between the two groups (p>0.05) (Table 2).
Table 2.
Postoperative AC and BC gain (dB) in each frequency
| 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 3,000 Hz | 4,000 Hz | ||
|---|---|---|---|---|---|---|---|
| AC gain (dB) | Causse Loop Piston | 33.7* | 33.1 | 32.4 | 27.6 | 26.9 | 25.2 |
| Big Easy Piston | 28.2 | 27.7 | 26.7 | 25.5 | 23.7 | 22.5 | |
| p | 0.029 | 0.024 | 0.029 | 0.375 | 0.176 | 0.345 | |
| BC gain (dB) | Causse Loop Piston | 3.7 | 3.9 | 6.4 | 10.8 | 7.9 | 5.4 |
| Big Easy Piston | 1.5 | 1.8 | 3.2 | 9.2 | 5.8 | 3.1 | |
| p | 0.080 | 0.132 | 0.050 | 0.392 | 0.182 | 0.251 | |
| ABG closure (dB) | Causse Loop Piston | 30.2 | 29.2 | 26.0 | 16.8 | 18.9 | 19.8 |
| Big Easy Piston | 26.9 | 25.9 | 23.6 | 16.2 | 17.9 | 19.4 | |
| p | 0.082 | 0.095 | 0.173 | 0.776 | 0.560 | 0.877 |
Values are expressed as mean.
AC: air conduction; BC: bone conduction; ABG: air-bone gap
We classified mean ABG closure in frequencies between 500 and 3,000 Hz into four categories: ≤10, 11–20, 21–30, >30 dB. As shown in Table 3, about 92.5% of ears in Causse Loop Piston group and 94.2% of ears in Big Easy Piston group obtained ABG closure within 20 dB; hence, this difference was not significant (p=0.571).
Table 3.
Mean ABG closure distribution in frequencies of 500–3,000 Hz
| ABG closure (dB) | Causse Loop Piston | Big Easy Piston | p | ||
|---|---|---|---|---|---|
| ≤ 10 | 57.5% | 92.5% | 59.1% | 94.2% | 0.571a |
| 11–20 | 35.0% | 35.1% | |||
| 21–30 | 3.5% | 7.5% | 3.3% | 5.8% | |
| > 30 | 4.0% | 2.5% | |||
Comparison of ABG closure within 20 dB between groups.
ABG: air-bone gap
Preoperative and postoperative SDS and SRT are shown in Table 4. Preoperative SRT was not significant between the groups (p=0.167). Postoperative SRT significantly improved in both the groups (p<0.05). In the Causse Loop Piston group, SRT significantly improved by 8.1 dB more than the Big Easy group (p=0.000). Preoperative SDS was significant between the two groups (p=0.015); hence, we compared SDS improvement between the groups. This improvement in the Big Easy group was 2.9% more than the improvement in the Causse Loop Piston (p=0.041), but the difference was not clinically significant. Although the improvement of postoperative SDS was statistically significant in each group (p<0.05), it was not clinically significant.
Table 4.
Preoperative and postoperative SDS and SRT
| Preoperative | Postoperative | Improvement | pb | ||
|---|---|---|---|---|---|
| SDS (%) | Causse Loop Piston | 93.1±8.7* | 97.7±4.4 | 4.6±8.7 | <0.0001 |
| Big Easy Piston | 89.7±8.0 | 97.2±5.6 | 7.5±8.4 | <0.0001 | |
| p-valuea | 0.015 | _c | 0.041 | ||
| SRT (dB) | Causse Loop Piston | 50.1±11.9 | 18.3±10.7 | 31.8±12.8 | <0.0001 |
| Big Easy Piston | 47.7±8.8 | 24.0±9.1 | 23.7±11.2 | <0.0001 | |
| p-valuea | 0.167 | 0.001 | 0.0001 |
Values are expressed as mean ± standard deviation (SD)
Between group comparison.
Within group comparison (preoperative and postoperative).
The statistical analysis was not performed because preoperative SDS was not significant between the two groups.
SDS: speech discrimination score; SRT: speech reception threshold
In this study, there were two postoperative complications. In Big Easy Piston, one patient developed a small central tympanic membrane perforation. It was repaired by applying paper patch in the follow-up visit. In the Causse Loop Piston group, a patient developed transient incomplete facial nerve palsy because of dehiscence of tympanic portion of facial nerve; he recovered completely by oral prednisolone after 1 month. Sensorineural hearing loss (SNHL) was identified as a post-surgery BC threshold, which was >10 dB worse than the value before the operation. Incidence of SNHL in different frequencies is shown in Table 5. There were no postoperative cases with SNHL in mean frequency of 500–3,000 Hz, and postoperative SNHL was not significant in different frequencies between the two groups (p>0.05). In addition, as shown in Table 6, SNHL incidence greater than 10 dB at 4,000 Hz was not significant between the Causse Loop Piston and the Big Easy Piston.
Table 5.
Incidence of postoperative SNHL at different frequencies
| Number | 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 3,000 Hz | 4,000 Hz | 500–3,000 Hz | |
|---|---|---|---|---|---|---|---|---|
| Causse Loop Piston | 76 | 0 (0)* | 0 (0) | 1 (1.3) | 0 (0) | 1 (1.3) | 2 (2.6) | 0 (0) |
| Big Easy Piston | 72 | 2 (2.8) | 3 (4.2) | 4 (5.5) | 2 (2.8) | 3 (4.2) | 5 (6.9) | 0 (0) |
| p | 0.235 | 0.113 | 0.200 | 0.235 | 0.357 | 0.266 | 1 |
Values are expressed as N(%).
SNHL: sensorineural hearing loss
Table 6.
Incidence of postoperative SNHL at frequency of 4,000 Hz
| Number | 10–20 (dB) | 20–30 (dB) | >30 (dB) | Total (dB) | |
|---|---|---|---|---|---|
| Causse Loop Piston | 76 | 2 (2.6) * | 0 (0) | 0 (0) | 2 (2.6) |
| Big Easy Piston | 72 | 1 (1.4) | 3 (4.2) | 1 (1.4) | 5 (6.9) |
| p | 1 | 0.113 | 0.486 | 0.266 |
Values are expressed as N (%).
SNHL: sensorineural hearing loss
DISCUSSION
In this randomized clinical study, we evaluated the performances of two different types of prostheses. Our initial hypothesis was that there was no significant difference between them with respect to the postoperative ABG and SRT. In addition, we found no significant difference in postoperative ABG closure between these two prostheses. However, what stands out in our findings is that postoperative AC gain was significantly higher in Causse Loop Piston group at low frequencies (250, 500, and 1,000 Hz). Furthermore, SRT improvement was significantly greater in this group.
A possible explanation for this issue might be the size of the prosthesis diameter; evidence supports our claim. Our results are in agreement with numerous reports that believe a larger diameter results in a better hearing at low frequencies [5–8].
Although modern technology has led to the availability of biocompatible prostheses, there is still conflicting evidence regarding the superiority of one over the other. Literature review showed that ABG closure within 10 dB was achieved between 23 and 96% of all cases (Table 7). Our results are within the acceptable limit of this range, and therefore, it is not important to seek a specific type of prosthesis. But the more important issue is to have ample amount of experience and the ability to achieve reasonable postoperative ABG closure.
Table 7.
Literature review of postoperative hearing outcomes in stapes surgery regarding the type of prosthesis
| Author (year) | Types of prosthesis (number) | Duration of follow-up | ABG ≤10 dB (%) | ABG ≤20 dB (%) | Conclusion |
|---|---|---|---|---|---|
| Current study | Causse Loop Piston (76) | At least 6 months | 57.5 | 92.5 | Similar results with both prostheses. |
| Big Easy Piston (72) | 59.1 | 94.2 | Causse Loop Piston was moderately better in low frequencies. | ||
|
| |||||
| Faramarzi et al. [18] | Causse Loop Piston (63) | At least 6 months | 36.5 | 80.9 | Similar results with both prostheses. |
| Titanium Soft-Clip (57) | 38.6 | 86 | |||
|
| |||||
| Schrotzlmair [13] | Self -Crimping Nitinol (Thermo Dummy) (21) | 70.7 days | 76.2 | 95.2 | Better ABG closure with Self – Crimping than with Clip Piston àWengen. |
| Titanium K-Piston (28) | 89.6 days | 53.6 | 89.3 | ||
| Clip Piston àWengen(13) | 163.1 days | 23.1 | 69.2 | ||
|
| |||||
| Ying et al. [16] | SMart (Teflon-based Piston Nitinol) (190) | NR* | NR | NR | Revision rate of 11% in the SMart group and 4% in the De La Cruz group. |
| Manual–Crimp Platinum; De La Cruz (145) | |||||
|
| |||||
| Mangham [12] | Platinum Piston (144) | NR | 96 | 100 | No difference in ABG closure. |
| Nitinol–Teflon Piston (44) | 92 | 100 | Nitinol–Teflon group had smaller mean ABG in lower frequencies. | ||
|
| |||||
| Fayad et al. [9] | SMart Piston (306) | 5.6 months | 78.3 | 94.2 | No differences |
| Richards' Platinum Piston (110) | 84.2 | 98.0 | |||
|
| |||||
| Van Rompaey et al. [15] | Teflon (211) | 12 months | Overall 63.6 | Overall 92.6 | No difference |
| Teflon Wire (168) | |||||
| Titanium (112) | |||||
| Clip piston (49) | |||||
| Smart (74) | |||||
|
| |||||
| Huber et al. [10] | Conventional (75) | At least 12 months | 43 | 92 | No difference in ABG closure within 20 dB, but Nitinol was better in ABG closure within 10 dB. |
| Nitinol Smart (75) | 71 | 94 | |||
|
| |||||
| Mangham [11] | Teflon Piston 0.5 mm (74) | 1 year | 85 | NR | Teflon Piston achieved better result than Titanum Clip Piston. |
| Teflon Piston 0.6 mm (74) | 91 | ||||
| Titanium Clip Piston (33) | 84 | ||||
|
| |||||
| Tange and Grolman [14] | Titanium K-piston (63) | NR | 65 | 87.1 | No differences |
| Clip Piston àWengen (63) | 71 | 91 | |||
|
| |||||
| Brown and Gantz [4] | Platinum Wire Piston (39) | 20 months | NR | NR | No differences |
| Nitinol Piston (40) | 9 months | ||||
|
| |||||
| Massey et al. [3] | Kurz Titanium K- Piston (35) | 4 months | 71 | 97.1 | No differences |
| Teflon Platinum Wire (183) | 86 | 97.8 | |||
|
| |||||
| Zepeda-Lopez et al. [17] | Schuknecht Teflon Wire Piston (70) | NR | 57.1 | NR | Fluoroplastic Teflon was better in low frequencies and resulted in better ABG closure in all frequencies. |
| Fluoroplastic Teflon (76) | 93.4 | ||||
NR: not reported;
ABG: Air-Bone Gap
As Table 7 shows that there are numerous studies that exclusively compared different stapes prostheses [3, 4, 9–18].
Gentle crimping of prosthesis onto the incus is vital and one of the most difficult steps in stapes surgery [14, 19]. It is claimed that tight crimping would result in avascular necrosis in the long process of incus. In contrast, loose crimping presumably can cause erosion in the long process [20–22]. Big Easy Piston prosthesis needs manual crimping. Although Big Easy Piston’s loop has sufficient opening with a wide band, sometimes diameter of long process of incus is small and a gap may exist in between; therefore, we cannot achieve a uniform loop. In fact, it can cause an oval crimp in practice, which reduces contact surface, which might result in a loose connection leading to incus necrosis. Consequently, it might have serious side effects on postoperative hearing outcome [20, 21, 23–25]. On the contrary, the loop in Causse Loop Piston has a self-crimping memory, which makes it fast and simple to apply. Because of its Teflon nature, the loop always goes back to its previous closed shape uniformly. In a retrospective study by Tange and Grolman [14], no difference in postoperative ABG closure between titanium Piston (Clip Piston àWengen) and no crimping prothesis (K-Piston) was found. Similarly, other researchers reported no difference between Nitinol Piston and Teflon Piston [26] as well as between Nitinol and platinum prostheses [4, 9, 14]. In addition, in a study by Shiao et al. [27], it was detected that self-crimping Nitinol Piston yielded similar hearing results to Schuknecht’s stainless prostheses, which require manual crimping.
On the contrary, in a study by Schrotzlmair et al. [13], better ABG closure with self-crimping prosthesis than Clip Piston àWengen that needs crimping was found. This view was supported by Mangham[8] in a retrospective study, who found a significant ABG closure in lower frequencies when using self-crimping Nitinol-Teflon prosthesis compared with conventional platinum-Teflon prosthesis. Our findings are also similar to Zepeda-Lopez et al. [17], supporting the usage of more technically effortless fluoroplastic Teflon. They conducted a retrospective study on post-stapedectomy hearing results with 70 Schuknecht-type Wire/Teflon prostheses, which need crimping, and 76 fluoroplastic Teflon prostheses. They concluded that application of the Teflon prosthesis can lead to a considerable hearing improvement in low frequencies and also a significant improvement in ABG closure in all frequencies.
The clinical implication of this study is that there is no difference between these two prostheses regarding postoperative ABG closure. As hearing result is comparable in both prostheses, and in real world, cost is an important factor for making an appropriate decision, we suggest the more cost-effective one.
To the best of our knowledge, this is one of the first studies to examine the performance of Big Easy Piston versus fluoroplastic (Teflon) Causse Loop Piston. The strength of our analyses was that all patients in this study underwent stapedotomy by one surgeon; therefore, difference in the level of experience was not a confounding factor.
One of the drawbacks of this study was its short-term follow-up period. Some authors believe that a displaced or malfunctioning prosthesis is the main cause of 81–87% of revision cases [23]. In addition, many researchers believe that malfunctioning of prosthesis results from malcrimping [28, 29]; this might result in incus necrosis. Therefore, it seems that self-crimping, firmness, and uniform loop of Causse Loop prosthesis might result in less revision stapes surgery than the Big Easy Piston. Under this circumstance, we suggest further long-term hearing evaluation.
CONCLUSION
To sum up, both prostheses yield similar postoperative ABG closure in short-term. However, we found that postoperative AC gain was considerably higher in Causse Loop Piston group in low frequencies. In addition, patients in Cause Loop Piston achieved better SRT improvement.
MAIN POINTS.
Postoperative ABG closure was similar in both groups; fluoroplastic Causse Loop Piston and platinum/titanium (Big Easy) Piston in short-term.
Regarding to ABG closure within 20 dB, both groups were comparable.
In low frequencies, patients with Causse Loop Piston achieved more postoperative AC gain than patients with Big Easy Piston.
Acknowledgements
The authors would like to thank Mr. Hossein Argasi for his editorial assistances in Research Consulting Center (RCC) of Shiraz University of Medical Sciences. This manuscript is partly from a thesis by Niloofar Daneshian, MD.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran.
Informed Consent: Written informed consent was obtained from all the patients who participated from in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.M.; Design - F.M.; Supervision - F.M.; Resource - F.M., N.D.; Materials - F.M., N.D.; Data Collection and/or Processing - N.D.; Analysis and/or Interpretation - F.M., S.R.; Literature Search - F.M., S.R., N.D.; Writing - F.M., S.R.; Critical Reviews - F.M., S.R.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Hausler R. General history of stapedectomy. Adv Otorhinolaryngol. 2007;65:1–5. doi: 10.1159/000098661. [DOI] [PubMed] [Google Scholar]
- 2.Shea JJ., Jr Fenestration of the oval window. Ann Otol Rhinol Laryngol. 1958;67:932–51. doi: 10.1177/000348945806700403. [DOI] [PubMed] [Google Scholar]
- 3.Massey BL, Kennedy RJ, Shelton C. Stapedectomy outcomes: titanium versus teflon wire prosthesis. Laryngoscope. 2005;115:249–52. doi: 10.1097/01.mlg.0000154727.85539.76. [DOI] [PubMed] [Google Scholar]
- 4.Brown KD, Gantz BJ. Hearing results after stapedotomy with a nitinol piston prosthesis. Arch Otolaryngol Head Neck Surg. 2007;133:758–62. doi: 10.1001/archotol.133.8.758. [DOI] [PubMed] [Google Scholar]
- 5.Laske RD, Röösli C, Chatzimichalis MV, Sim JH, Huber AM. The Influence of Prosthesis Diameter in Stapes Surgery: A Meta-Analysis and Systematic Review of the Literature. Otol Neurotol. 2011;32:520–8. doi: 10.1097/MAO.0b013e318216795b. [DOI] [PubMed] [Google Scholar]
- 6.Marchese MR, Cianfrone F, Passali GC, Paludetti G. Hearing results after stapedotomy: role of the prosthesis diameter. Audiol Neurotol. 2007;12:221–5. doi: 10.1159/000101329. [DOI] [PubMed] [Google Scholar]
- 7.Rosowski JJ, Merchant SN. Mechanical and acoustic analysis of middle ear reconstruction. Am J Otol. 1995;16:486–97. [PubMed] [Google Scholar]
- 8.Teig E, Lindeman HH. Stapedotomy Piston Diameter - Is Bigger Better? Oto Rhino Laryn Nova. 1999;9:252–6. doi: 10.1159/00002793. [DOI] [Google Scholar]
- 9.Fayad JN, Semaan MT, Meier JC, House JW. Hearing results using the SMart piston prosthesis. Otol Neurotol. 2009;30:1122–7. doi: 10.1097/MAO.0b013e3181be645d. [DOI] [PubMed] [Google Scholar]
- 10.Huber AM, Veraguth D, Schmid S, Roth T, Eiber A. Tight stapes prosthesis fixation leads to better functional results in otosclerosis surgery. Otol Neurotol. 2008;29:893–9. doi: 10.1097/MAO.0b013e318184f4f0. [DOI] [PubMed] [Google Scholar]
- 11.Mangham CA., Jr Titanium CliP piston versus platinum-ribbon Teflon piston: piston and fenestra size affect air-bone gap. Otol Neurotol. 2008;29:8–12. doi: 10.1097/mao.0b013e31815c2575. [DOI] [PubMed] [Google Scholar]
- 12.Mangham CA., Jr Nitinol-teflon stapes prosthesis improves low-frequency hearing results after stapedotomy. Otol Neurotol. 2010;31:1022–6. doi: 10.1097/MAO.0b013e3181e9bee4. [DOI] [PubMed] [Google Scholar]
- 13.Schrotzlmair F, Suchan F, Kisser U, Hempel JM, Sroka R, Muller J. Promising clinical results of an innovative self-crimping stapes prosthesis in otosclerosis surgery. Otol Neurotol. 2013;34:1571–5. doi: 10.1097/MAO.0b013e3182a5d12d. [DOI] [PubMed] [Google Scholar]
- 14.Tange RA, Grolman W. An analysis of the air-bone gap closure obtained by a crimping and a non-crimping titanium stapes prosthesis in otosclerosis. Auris Nasus Larynx. 2008;35:181–4. doi: 10.1016/j.anl.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Van Rompaey V, Yung M, Claes J, Hausler R, Martin C, Somers T, et al. Prospective effectiveness of stapes surgery for otosclerosis in a multicenter audit setting: feasibility of the Common Otology Database as a benchmark database. Otol Neurotol. 2009;30:1101–10. doi: 10.1097/MAO.0b013e3181b4eebf. [DOI] [PubMed] [Google Scholar]
- 16.Ying YL, Hillman TA, Chen DA. Patterns of failure in heat-activated crimping prosthesis in stapedotomy. Otol Neurotol. 2011;32:21–8. doi: 10.1097/MAO.0b013e3181b4eebf. [DOI] [PubMed] [Google Scholar]
- 17.Zepeda-Lopez EG, Bello-Mora A, Felix-Trujillo MM. Poststapedectomy hearing gain: comparison of a Teflon (fluoroplastic ASTM F 754) prosthesis with a Schuknecht-type wire/Teflon prosthesis. Ear Nose Throat J. 2005;84:707–8. 10, 19. doi: 10.1177/014556130508401111. [DOI] [PubMed] [Google Scholar]
- 18.Faramarzi M, Gilanifar N, Roosta S. Comparison of Fluoroplastic Causse Loop Piston and Titanium Soft-Clip in Stapedotomy. Iran J Otorhinolaryngol. 2017;29:23–8. [PMC free article] [PubMed] [Google Scholar]
- 19.Sorom AJ, Driscoll CL, Beatty CW, Lundy L. Retrospective analysis of outcomes after stapedotomy with implantation of a self-crimping Nitinol stapes prosthesis. Otolaryngol Head Neck Surg. 2007;137:65–9. doi: 10.1016/j.otohns.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Brar T, Passey JC, Agarwal AK. Comparison of hearing outcome using a Nitinol versus Teflon prosthesis in stapedotomy. Acta Otolaryngol. 2012;132:1151–4. doi: 10.3109/00016489.2012.699196. [DOI] [PubMed] [Google Scholar]
- 21.Ueda H, Kishimoto M, Uchida Y, Sone M. Factors affecting fenestration of the footplate in stapes surgery: effectiveness of Fisch’s reversal steps stapedotomy. Otol Neurotol. 2013;34:1576–80. doi: 10.1097/MAO.0b013e3182a473eb. [DOI] [PubMed] [Google Scholar]
- 22.Huber AM, Ma F, Felix H, Linder T. Stapes prosthesis attachment: the effect of crimping on sound transfer in otosclerosis surgery. Laryngoscope. 2003;113:853–8. doi: 10.1097/00005537-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Kwok P, Fisch U, Strutz J, May J. Stapes surgery: how precisely do different prostheses attach to the long process of the incus with different instruments and different surgeons? Otol Neurotol. 2002;23:289–95. doi: 10.1097/00129492-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Skinner M, Honrado C, Prasad M, Kent HN, Selesnick SH. The incudostapedial joint angle: implications for stapes surgery prosthesis selection and crimping. Laryngoscope. 2003;113:647–53. doi: 10.1097/00005537-200304000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Aroesty JH, Lucente FE, Har-El G. Poststapedectomy incus necrosis. Otolaryngol Head Neck Surg. 1993;109:1083–4. doi: 10.1177/019459989310900619. [DOI] [PubMed] [Google Scholar]
- 26.Huttenbrink KB. Biomechanics of stapesplasty: a review. Otol Neurotol. 2003;24:548–57. doi: 10.1097/00129492-200307000-00004. discussion 57–9. [DOI] [PubMed] [Google Scholar]
- 27.McGee TM. The loose wire syndrome. Laryngoscope. 1981;91:1478–83. doi: 10.1288/00005537-198109000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Shiao AS, Kuo CL, Cheng HL, Wang MC, Chu CH. Controversial issues of optimal surgical timing and patient selection in the treatment planning of otosclerosis. Eur Arch Otorhinolaryngol. 2014;271:1007–14. doi: 10.1007/s00405-013-2529-6. [DOI] [PubMed] [Google Scholar]
- 29.Farrior J, Sutherland A. Revision stapes surgery. Laryngoscope. 1991;101:1155–61. doi: 10.1288/00005537-199111000-00003. [DOI] [PubMed] [Google Scholar]