Abstract
OBJECTIVES
The primary objective of this study was to evaluate how successful the reposition of retractable benign paroxysmal positional vertigo (BPPV) was when treating patients with the Thomas Richard Vitton (TRV) reposition chair.
MATERIALS and METHODS
This is a prospective clinical trial. A total of 81 BPPV patients who were referred to the tertiary Balance & Dizziness Centre at the Department of Otolaryngology, Head & Neck Surgery and Audiology, Aalborg University Hospital, Denmark were included and analyzed. All the patients were diagnosed and treated with the TRV reposition chair.
RESULTS
The patients were successfully treated after an average of 2.23 (± 1.66 SD) treatments with the TRV reposition chair. There was a significant difference between the number of treatments needed in the single semicircular canal group and the multicanal group. Seventeen (22.6%) of the patients experienced either dislocation of otoconia, relapse, or new onset of BPPV during the trial period. The number of patients with BPPV located to the anterior, lateral, and multiple semicircular canals in this study was significantly higher than that in similar studies. Six patients (7.4%) were classified as treatment failures.
CONCLUSION
We found the TRV reposition chair to be very successful in the diagnostics and treatment of patients with retractable and atypical BPPV. However, 7.4% experienced treatment failure.
Keywords: Benign paroxysmal positional vertigo, rotational chair, vertigo, repositioning maneuvers, TRV chair
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo, with an incidence between 10.7 and 64.0 cases per 100,000 persons, equivalent to a lifetime prevalence of 2.4% [1,2]. The incidence rises with increasing age, and the disease is typically seen in patients between 50 and 70 years of age, predominantly women [1]. One study estimated that 9% of elderly patients undergoing geriatric assessment for nonbalance-related complaints, suffer from BPPV [2].
Benign Paroxysmal Positional Vertigo is characterized by positional vertigo, which is defined as a rotating sensation induced by position changes relative to gravity [2]. Usually symptoms are short-lasting (seconds) and emerge when the patient turns their head, looks up, or turns over in bed.
Pathophysiologically, BPPV consists of otoconia from the utricle, which are dislocated into one or several of the semicircular canals (SCCs). These dislocated otoconia affect the sensory hair cells during movement via their mass, thereby creating an imbalance of signals sent to the central nervous system [3]. Disequilibrium in signals from the vestibular system results in a rotatory sensation (i.e., vertigo) [4].
Categorization of BPPV is based on whether the otoconia are floating freely within the endolymph of the SCCs or if otoconia are attached to the cupula. Free-floating otoconia are named canalolithiasis, and otoconia attached to the cupula are named cupulolithiasis [3,4]. Furthermore, BPPV can be subcategorized according to the affected SCC(s). Therefore, BPPV may be categorized as anterior-canal BPPV, lateral-canal BPPV, and/or posterior-canal BPPV occurring either uni- or bilaterally or as multicanal BPPV and further classified as being either canalolithiasis or cupulolithiasis [3, 4–6]. By far, posterior-canal BPPV is the most common subtype, including 85–95% of all BPPV cases, most likely because of its anatomical relation to the utricle [6]. Lateral-canal BPPV occurs in 5–15% of all BPPV cases, whereas anterior-canal BPPV and multicanal BPPV occurs only in a few percentage of BPPV cases [6, 7].
A diagnosis of BPPV requires both subjective symptoms (by means of positional vertigo) and objective observation of nystagmus triggered during specific positional tests [6]. The Dix-Hallpike maneuver (DH) and the supine roll test (SRT) are two common positional tests and, when used in combination, they test all six SCCs of BPPV [3].
Benign Paroxysmal Positional Vertigo often resolves within days or weeks without treatment, but early treatment can shorten the duration of the disease and improve quality of life [5]. Despite both conservative and active treatment, several patients still experience persistent BPPV [6].
Several canalith repositioning procedures (CRPs) exist. One of the most validated CRPs is the Epley maneuver developed by John Epley in 1992. This procedure has a reported efficacy rate of 80% when treating posterior canalolithiasis BPPV [5].
Lateral-canal BPPV, multicanal BPPV, and cupulolithiasis-type BPPV are found to be more difficult to treat; thus, 10–20% of all BPPV cases may be challenging to both diagnose and treat [4]. When considering the incidence of the disease, the proportion of patients with unresolved BPPV who might benefit from better treatments is, therefore, potentially quite large. In addition, the recurrence rates of BPPV have been reported to be as high as 27% within the first 6 months and 40–50% after 5 years of follow-up [3].
These issues have obviously been a contributing factor to the development of the three biaxial chairs for the reposition of BPPV: the Epley Omniax Rotator [8], the TRV reposition chair [9], and the rather new Rotundum positioning chair. Biaxial chairs enable exact positional testing and treatment. Because the patient is fixed to the chair, standardized diagnostic procedures and treatments can be implemented. All chairs allow 360° rotation of the patients in both the horizontal and vertical planes. This facilitates both diagnostic procedures and repositional maneuvers in patients who can, otherwise, not fully cooperate. Often, infrared video goggles are used in combination with these chairs, adding additional advantages to diagnostics like pupil auto tracking, measurement of nystagmus slow-phase velocity, and video recording of nystagmus.
Thus far, only a limited number of studies have investigated the use of mechanical rotation chairs in the treatment of BPPV, but both diagnostic and therapeutic benefits have been found in previous studies [1,4,10].
The primary objective of this study was to evaluate how successful the reposition of BPPV was when treating patients with retractable BPPV with the TRV reposition chair. The secondary objectives were (1) the number of treatments required for individual subtypes and combinations of BPPV and (2) the description of the study population according to localization and subtypes of BPPV.
MATERIALS AND METHODS
Patients
A total of 96 patients were initially evaluated and included in this study. Following the exclusion of patients, primarily because treatment at some point during the follow-up period deviated from the standard treatment protocol, this number was reduced to 81 patients (Figure 1). All patients were referred to the tertiary Balance & Dizziness Centre at the Department of Otolaryngology, Head & Neck Surgery and Audiology, Aalborg University Hospital, Denmark with intractable BPPV. The patients were classified as being intractable because all prior treatments were unsuccessful despite characteristic symptomology and diagnostic findings. All patients had undergone several (at least five) individual BPPV treatments (manual repositional maneuvers; e.g., standard Epley maneuver, log rolling maneuver, Semont maneuver on an examination bed) prior to referral, and patients had been symptomatic for an average of 16 months. The initial treatments were all carried out at regional ENT clinics, which are part of the primary care sector in Denmark. Inclusion criteria included positional vertigo and a positive result on the DH and/or SRT tests. Patients younger than 18 years and those who had previously undergone treatment with a mechanical repositioning chair were excluded from the study. In addition, patients requiring more than 10 treatments with the TRV reposition chair were considered resistant to TRV reposition chair treatment and classified as “treatment failures.”
Figure 1.
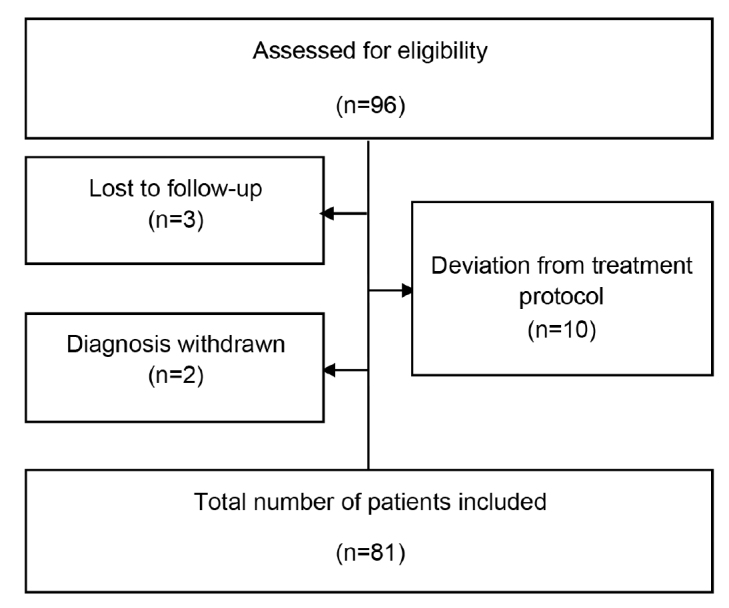
Trial profile.
Diagnosis
As mentioned, patients were given a diagnosis of BPPV if they experienced positional vertigo in combination with a positive result on the DH and/or SRT tests [11]. Both positional tests were carried out with the patients sitting in the TRV reposition chair. All patients were fitted with video Frenzel goggles (VF405®, Interacoustics, Middelfart, Denmark) during testing, thereby facilitating both precise and consistent diagnostics. Furthermore, these infrared video goggles enabled quantification of nystagmus characteristics with measurements of additional parameters such as direction (horizontal and vertical), beats per minute, and average slow-phase velocity (a-SPV).
On the basis of nystagmus characteristics observed during positional testing, the patients were divided into different BPPV subcategories (Table 1).
Table 1.
| Nystagmus characteristics | Subtypes of BPPV | |
|---|---|---|
| Canalolithiasis | Cupulolithiasis | |
| Posterior SCC | Upbeat nystagmus with rotatory component beating toward the ground (geotropic) during Dix-Hallpike testing. Ipsilateral affection. | As for canalolithiasis but without latency and also persistent nystagmus > 1 min. |
| Lateral SCC | Geotropic horizontal nystagmus during supine roll test in both positions with the highest frequency observed on the affected side. | Apogeotropic horizontal nystagmus during supine roll test in both positions with the highest frequency observed on the nonaffected side. |
| Anterior SCC | Downbeat nystagmus with rotatory component beating away from the ground (apogeotropic) during Dix-Hallpike testing. Contralateral affection. | As for canalolithiasis but without latency and also persistent nystagmus > 1 min. |
SCC: semicircular canal.
Treatment with the TRV Reposition Chair
The TRV reposition chair enables the repositioning of otoconia through different repositioning maneuvers [12]. The patients were assigned to different reposition maneuvers based on their BPPV subtype( s) and treated with one or more of the maneuvers listed in Table 2. At every visit, the patients received one treatment with the TRV reposition chair. The specific repositional maneuver assigned to the individual patient was chosen by the examining physician based on expert opinion in order to mimic current clinical practice.
Table 2.
Types of reposition maneuvers accessible for treatment of individual BPPV subtypes
| BPPV subtype | Reposition maneuver |
|---|---|
| Posterior BPPV | Standard Epley maneuver |
| Potentiated Epley maneuver | |
| Lateral BPPV | Barbeque-roll |
| Potentiated Epley maneuver | |
| Anterior BPPV | Deep head hanging reposition maneuver |
Patients with ipsilateral BPPV of both the posterior and lateral SCCs were treated simultaneously with the potentiated Epley maneuver because this treatment modality enabled targeting of both SCCs in one session with the TRV reposition chair. Patients diagnosed with bilateral BPPV initially underwent treatment of their most affected side (the side with the highest a-SPV and/or the most symptomatic side) during testing with the TRV reposition chair.
The standard Epley maneuver was conducted as described by John Epley in 1992 [13], but with the patient sitting in the TRV reposition chair.
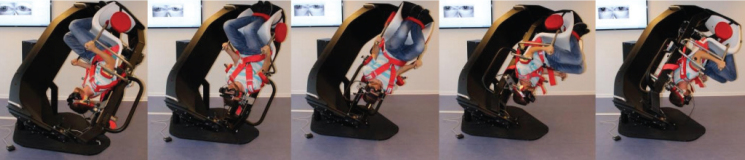
The potentiated Epley maneuver was carried out with ten sudden decelerations against the rubber stop of the TRV reposition chair in every 45° position (five positions) of a 180° turn before returning the patient to the upright position. Figure 2 illustrates all positions where patients had deceleration treatments applied.
Figure 2.
Illustration of the potentiated Epley maneuver with treatment of a left posterior BPPV. All five positions where decelerations were applied are depicted.
The potentiated Epley maneuver was also performed in a modified version with a 225° turn with a starting position 45° ahead of the standard DH position. This variant was used for all treatments of the cupulolithiasis BPPV subtypes. The Barbeque (BBQ)-roll maneuver was performed as described by Thomas Richard Vitton [12]. The deep head hanging reposition maneuver was performed ad modum the study by Yacovino et al. [14]. All treatments were carried out according to the manufacturers’ recommendations.
All patients were scheduled for a minimum of one follow-up after inclusion and initial treatment. The patients were continuously given a follow-up appointment as long as the treatment(s) was not considered successful; for example, no positional nystagmus could be evoked in the DH and/or SRT positional tests (objective measure), and patients did not experience any rotational vertigo during these tests (subjective measure). Follow-up visits were scheduled 2–4 weeks after the previous treatment. However, to a minor degree, rescheduling was sometimes necessary because some patients requested postponing their follow-up. The interval between follow-ups was, on average, 26 days. As a direct consequence of these follow-up conditions, one can conclude that, on average, no early relapses were observed 26 days following successful treatment.
Statistical Analysis
The overall treatment effect was described by descriptive statistics.
Treatment effect differences within BPPV subtypes were analyzed by inferential means and expressed in p-values and 95% confidence intervals. This calculation was done with a t-test, and the sensitivity was tested with a Wilcoxon rank sum test as data showed not to be fully normally distributed.
Results with a p-value <0.05 were considered significant.
Stata/MP 14.0 software was chosen for the processing of data, and this processing was carried out with assistance from a certified biostatistician.
RESULTS
Population characteristics are described in Table 3. Most patients had a uni- or bilateral sensorineural hearing loss (7% and 57%, respectively). In 38% of patients, the bilateral hearing loss was caused by presbycusis. A small minority of patients had other preexisting inner- and/or middle-ear-related comorbidities at the time of referral. Five patients (7%) had tinnitus, three (4%) had a unilateral vestibular schwannoma, two (3%) had Meniere’s disease, one (1%) had bilateral otosclerosis, and one (1%) had previously had vestibular neuritis. In patients with multicanal BPPV, the involved SCCs were distributed as depicted in Table 4. The overall average number of required treatments with the TRV reposition chair was 2.23 (± 1.66 SD) treatments when looking at all BPPV subtypes pooled together.
Table 3.
Population characteristics
| Characteristic | Value |
|---|---|
| Patients, n | |
| Initially included | 96* |
| Total included with BPPV | 81* |
| Age (years), mean (± SD) | 61.80 (±15.26) |
| Sex, n (%) | |
| Male | 27 (36.00) |
| Female | 48 (64.00) |
| Duration of symptoms pretreatment (months) | |
| Mean (± SD) | 16.03 (± 21.99) |
| Median | 9.00 |
| Affected SCC, n (%) | |
| p-CAN | 29 (38.67) |
| p-CUP | 0 |
| l-CAN | 10 (13.33) |
| l-CUP | 8 (10.67) |
| a-CAN | 4 (5.33) |
| Multicanal BPPV | 24 (32.00) |
P-CAN: posterior canalolithiasis; p-CUP: posterior cupulolithiasis; l-CAN: lateral canalolithiasis; l-CUP: lateral cupulolithiasis; a-CAN: anterior canalolithiasis; BPPV: benign paroxysmal positional vertigo.
All numbers and calculations are based on 75 patients (excluded and treatment failure patients are not included) except the top two values marked with *.
Table 4.
Distribution of multicanal BPPV
| Affected SCCs | Number (%) |
|---|---|
| Posterior bilateral | 5 (6.67) |
| Lateral bilateral | 4 (5.33) |
| Posterior + lateral | 13 (17.33) |
| Anterior + lateral | 2 (2.67) |
BPPV: Benign Paroxysmal Positional Vertigo; SCC: semicircular canal
The mean follow-up time between treatments with the TRV reposition chair was 25.75 days (± 11.32 SD).
Table 5 shows the average number of treatments required before negative positional testing was observed in the different subgroups of BPPV.
Table 5.
Average number of treatments required for successful treatment related to BPPV subtypes
| BPPV subtype | No. of treatments, n (±SD) |
|---|---|
| p-CAN | 1.62 (1.24) |
| p-CUP | N/A |
| l-CAN | 1.6 (0.97) |
| l-CUP | 3.13 (2.36) |
| a-CAN | 1.00 (0.00) |
| Multicanal BPPV | 3.13 (1.70) |
P-CAN: posterior canalolithiasis; p-CUP: posterior cupulolithiasis; l-CAN: lateral canalolithiasis; l-CUP: lateral cupulolithiasis; a-CAN: anterior canalolithiasis; BPPV: benign paroxysmal positional vertigo.
Patients with affection of one SCC received an average of 1.80 treatments before a normal positional test was observed together with concomitant resolution of symptoms. Patients with multicanal BPPV received 3.13 treatments on average before negative positional testing occurred. This corresponds to a difference of 1.33 treatments with a p-value of 0.0022 and a confidence interval of −2.14 to −0.51.
The total number of affected SCCs averaged 1.37 canals at the first treatment, 1.25 canals at the second treatment, and 1.32 canals at the third treatment.
During the trial period, 17 (22.6%) of the patients experienced either dislocation from one SCC to another or debut of BPPV in one of the contralateral SCCs.
Following the initial treatment with the TRV reposition chair, 45 (60%) patients experienced a subjective relief of their symptoms. Treatment failure was observed in six patients (7.4%) of the study population. All six patients were female, had a mean age of 78.3 years, and had been symptomatic for an average of 12 months (median 10.5 months) prior to referral. Five patients had normal inner ear findings following MRI of the temporal bone and one patient had a normal temporal bone CT scan. One patient was diagnosed with Meniere’s disease, one patient had had a cerebral hemorrhage, one patient had osteoporosis, and one patient had undergone surgery for otosclerosis prior to referral. No other inner- or middle ear comorbidities (or other relevant comorbidities) were observed in this group of patients. BPPV subtypes included lateral BPPV (66%) with equal distribution of canalo- and cupulolithiasis. In addition, one patient (17%) was diagnosed with posterior canalolithiasis and one patient (17%) had multicanal BPPV with a combination of posterior and lateral SCC affection.
DISCUSSION
Primary and Secondary Results
Overall, the rate of successful treatment with the TRV reposition chair was 92.4% within a population of retractable BPPV cases. Six patients (7.4%) required more than 10 treatments and were therefore classified as treatment failures. Following general exclusion and omission of the treatment failures, 75 patients were further analyzed. These patients were distributed as expected according to male/female ratio and age when compared with existing studies [5,11,15].
On average, the overall number of required treatments in the TRV reposition chair was 2.23 (± 1.66SD) when all BPPV subtypes were considered, and all of the analyzed patients were cured from their BPPV (however, one must bear in mind that six patients were excluded from this calculation because of treatment failure before the final analyses). Following only one treatment with the TRV reposition chair, 60% of the patients reported a relief of symptoms.
On average, patients with either lateral cupulolithiasis or multicanal BPPV received 3.13 treatments with the TRV reposition chair before negative positional testing was accomplished. This could partly be due to the diagnostic procedure when diagnosing lateral canal BPPV where the intensity of nystagmus (a-SPV) determines which side (left/right) is affected. Because some patients had very analogous a-SPV values when comparing the two sides, determination of laterality was sometimes very difficult. Initially, this might have led to treatment of the wrong and healthy side, and as a result more treatments had to be carried out before negative positional testing with the TRV reposition chair was accomplished. In order to accommodate more accurate testing of the lateral SCCs, addition of the “bow and lean test” could potentially have added more diagnostic accuracy when determining the affected side [2].
Furthermore, a condition with spontaneous nystagmus might disturb the diagnostic procedure of BPPV. It is known that lateral canal BPPV is associated with spontaneous nystagmus in up to 66–76% of the cases [16].
In this study, the BPPV subtype of canalolithiasis generally required fewer treatments than that required by the subtype of cupulolithiasis (Table 5). This observation fits well with other studies as lateral SCC cupulolithiasis, in particular, has been found to be more resistant to the treatment [6].
We found a significant difference in the average number of treatments required for the single SCC BPPV group versus the multicanal BPPV group of 1.33 treatments with a p-value of 0.0022 and a confidence interval of −2.14 to −0.51. There is no clear consensus in the literature regarding treatment response and prognosis of single SCC affection and multi-SCC affection. Some studies found inferior response to multi-SCC BPPV [4], whereas others did not find significant differences in the prognosis after treatment of single SCC BPPV and multi-SCC BPPV [7].
The distribution of BPPV subtypes in this study is not in accordance with that in the existing literature. In this study, there were 29 (38.67%) patients with posterior BPPV, 18 (24.00%) with lateral BPPV, four (5.33%) with anterior BPPV, and 24 (32.00%) with multicanal BPPV. Thus, there was a significantly higher proportion of patients with BPPV in the lateral and anterior SCCs as well as those with multicanal BPPV than that in previous studies [5,6,17]. Literature shows that these subcategories of BPPV have been found to be more resistant to treatment [4]. In addition, the duration of symptoms was, on average, 16.03 (±21.99) months with a median of 9.00 months at the time of initial treatment. When considering the natural history of BPPV, this is noticeable, because the disease normally resolves itself within weeks [5]. One must assume that the patients included in this study constitute a group of atypical and very intractable BPPV patients. This assumption is based on the fact that these patients all had extremely long durations of symptoms and also because of the atypical distribution of these patients’ BPPV subtypes. The causes of treatment failure in this study can only be speculative but might be explained by different variables potentially affecting treatment results: various inner ear anomalies and otolithic properties. The actual angle of the vertical SCCs may vary, the individual SCC may be very narrow in general or in specific parts of the canal, and the otoliths may also vary in number, size, and density, and may stick together, creating a blockage or an otolithic jam.
Prior Studies with Mechanical Chairs
Very few studies have been published on the efficacy of mechanical repositional chairs in the treatment of BPPV. The Rotundum chair is a very new invention, and currently, no articles have been published on its efficacy. Only a few studies have been published on the use of the two other chairs. A retrospective study with the TRV reposition chair on retractable BPPV cases found results quite similar to those in this study. Multicanal and cupulolithiasis-type BPPV required the highest number of treatments, and an overall symptom relief of 91.7–100% was observed after three treatments [4]. Another study, which dealt only with posterior BPPV, found that 85.2% required only one treatment with the TRV repositional chair. However, this study population is not directly comparable, as the previous study excluded all other types and combinations of BPPV except posterior canalolithiasis [18]. Studies on the 360° maneuver with a rotational chair have also been conducted; but these studies are not directly comparable with our population because these studies only dealt with patients with posterior BPPV [19]. Furthermore, we did not use the 360° maneuver. Previous studies with an automated positioning chair have also proven beneficial [4,20], but the results are not directly comparable as the TRV reposition chair is manually operated. A recent study with the TRV reposition chair dealt with dizziness handicap related to subtypes of BPPV, but it did not report any comparable effect on treatments with the TRV reposition chair [21].
Potential Disadvantages with the Use of A TRV Reposition Chair
There were not many drawbacks with the use of the TRV reposition chair. Some patients complained of claustrophobia upon fixation to the chair and wearing video Frenzel goggles with vision denied. For some patients, this might have led to discontinuation of treatment or a loss to follow-up. Furthermore, there was no way to monitor the actual impact of the decelerations applied by the individual examiner. This condition makes the individual treatments susceptible to varying degrees of both intra- and interexaminer variations. The individual examiner solely determined the number of decelerations inflicted and the position of the actual applications. Currently, the choice of maneuver is a matter of expert opinion because of a lack of evidence on the matter. For instance, a recent Danish study recommended only three decelerations applied at the starting and ending positions when performing the potentiated Epley maneuver [22]. In our study, we used 10 decelerations in all stop positions during the potentiated Epley maneuver. The optimal number of decelerations still needs further investigation, so that a proper balance between treatment effect and induction of contralateral BPPV can be accomplished.
The TRV reposition chair operates only in 45° intervals in the vertical plane. Some patients might have atypical inner ear anatomy, with the vertical SCCs located at different angles. If this is the case, patients may not be treated successfully with this chair.
Adding an infrared video goggle to the examination in the TRV reposition chair improves tracking of eye movements. For inexperienced examiners, a drawback to this might be that overinterpretation of minor (nonpathological) eye movements might occur. This will potentially lead to over diagnosis and redundant treatments.
In this study, 22.6% of patients experienced either dislocation from one SCC to another SCC ipsilaterally, BPPV relapse, or BPPV in one or more of the contralateral SCCs. This relatively large proportion of recurrent disease is, to some extent, expected. This is primarily because dislocation from the posterior to the lateral SCC and vice versa is seen in 6% of all BPPV cases during standard repositioning maneuvers [6]. In addition, relapses are reported as high as 27% during the first month following successful treatment [3]. Adding kinetic energy during reposition maneuvers might explain why so many patients develop contralateral BPPV following treatment.
Potential Disadvantages of Study Design
A total of 96 patients were initially included for this study, but 15 patients were excluded. This is a major concern when considering the dataset, as these patients comprise almost 16% of the entire study population. One can only speculate about the reasons for this high degree of loss to follow-up. Three patients did not have BPPV and were therefore excluded. Ten patients were excluded because deviation( s) from the treatment protocol of the project was/were deemed necessary at some point during the follow-up period. Lastly, two patients discontinued their treatment because of discomfort in the TRV reposition chair. Especially with the group of patients where a deviation from standard treatment protocol was deemed necessary, one must consider if selection bias may have affected the results. Did these patients have unknown pathologies or special properties within their inner ears that made them particularly resistant to standard treatments? However, in general, all of the excluded patients had multicanal BPPV with alternating sides of affection. Overall, the excluded patients were comparable with the analyzed population (gender, length of pretreatment vertigo, number of treatments, BPPV subtypes), except their mean ages. Within the group of treatment failures, the mean age was 78.3 years compared with a mean age of 61.8 years within the group of analyzed patients. This group also exclusively consisted of women, and most of these patients had lateral canal BPPV. Whether these characteristics might have influenced or contributed to the severity and retractability of their BPPV remains speculative.
The study was conducted as a prospective observational study. For ethical reasons, it was not possible to avoid treatment of one group of patients, and as a direct consequence, the study was carried out without any control group. Furthermore, if a control group should have been included in this study, a randomization between treatments with or without the TRV reposition chair should have taken place at the time of inclusion. As our study population had already undergone several unsuccessful manual reposition attempts at the time of referral, it was not considered appropriate with a randomization that included treatments already proven unsuccessful. However, a control group is preferable when the target measure is a treatment effect.
Potential Advantages with the Use of A TRV Reposition Chair
There were several benefits of using the TRV reposition chair for the diagnostics as well as the treatment of BPPV. First, patients did not have to follow complicated instructions. Fixation of the patient to the chair allows 360° rotation of the patient in both the horizontal and vertical planes, regardless of compromised patient compliance. This enabled precise and consistent reposition maneuvers for all treatments. In addition, fitting patients with video Frenzel goggles with accompanying software enabled visualization and quantification of any nystagmus elicited during the positional testing. This was particularly helpful when patients experienced multiple SCC affection, especially lateral SCC affection, where the nystagmus intensity helps to determine the side of pathology [3].
The reasons why the TRV reposition chair enabled treatment of retractable BPPV with excellent results are probably numerous. The precise and consistent movements of endolymph (and otoconia) within the specific planes of the SCCs made possible by the chair and the simultaneous use of video Frenzel goggles are two likely explanations. In addition, it is plausible to assume that the TRV reposition chair applies rotational energy to the endolymph during the BBQ roll maneuver, as the patient during this maneuver is kept in constant rotation. Kinetic energy is probably also applied to the otoconia via steep decelerations during the potentiated Epley maneuver. Overall, most of our patients underwent treatments where kinetic forces were applied to add additional effect to the standard treatments the patients had already received prior to referral.
The TRV reposition chair also facilitates standardization and alignment of especially the diagnostic part. The chair has fixed intervals of 45° rotations in the vertical plane enabling precise and repetitive positioning of the patient independent of the examiner. Therefore, especially in terms of diagnostics, the TRV reposition chair has a low degree of both intra- and interexaminer variations. In treatments with the TRV reposition chair, the actual positioning of the patient during reposition is also standardized and reproducible and therefore without any significant intra- and interexaminer variations.
Potential Advantages of Study Design
The natural history of BPPV usually includes spontaneous resolution of the disease within a few weeks following the onset of symptoms [5]. Therefore, we consider the observed effect of treatment(s) with the TRV reposition chair as being reliable and not just the result of random spontaneous relapses. On average, patients had been symptomatic for 16 months. Another significant strength of the design is the prospective course of the study and the relatively short intervals between appointments and repositioning maneuvers. All patients were treated with the TRV reposition chair, with a mean follow-up time of 25.75 days (±11.32 SD) between treatments. It was decided at project planning that an optimal follow-up time would be 2–4 weeks to obtain a reliable treatment effect. Wider intervals could be disturbed by relapses, thus underestimating the effect. The optimal follow-up time is disputed. However, a systematic review found several studies that apply 4 weeks between treatments [4]. During repositioning, in theory, otoconia are removed from the SCC(s) during the repositioning maneuver itself. This speaks against long follow-up intervals, when the effect of reposition is to be investigated, as long intervals may lead to underestimation owing to the relapsing nature of BPPV.
CONCLUSION
We conclude that the TRV reposition chair is an effective means of treating patients with retractable BPPV. However, 7.6% of patients experienced treatment failure. The TRV reposition chair is proved to be an excellent diagnostic tool for diagnosing BPPV. It enables precise diagnostics in subtypes of both canalo- and cupulolithiasis as well as to what SCC(s) is(are) affected uni- and/or bilaterally. Thus far, only a few studies have been published on the use of the TRV reposition chair in the treatment and diagnosis of retractable BPPV. Therefore, further studies are important for the future implementation and development of this promising treatment modality.
MAIN POINTS.
In combination with video Frenzel googles or Video Nystagmography (VNG) equipment, the TRV reposition chair offers precise diagnostics of BPPV according to subtype and laterality.
The TRV reposition chair offers effective treatment of patients with retractable BPPV.
In general, patients referred with retractable BPPV required an average of approximately two treatments.
Acknowledgements
Acknowledgments
Acknowledgments to the tertiary ENT Dizziness Clinic at Aalborg University Hospital, Aalborg, Denmark.
Footnotes
This study was presented at the International Congress of ORL-HNS 2019 (ICORL 2019), April 25-28, 2019, Seoul, South Korea.
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from all subjects who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.F.P., D.D.H.; Design - M.F.P., D.D.H.; Supervision - D.D.H.; Resource - D.D.H.; Materials - M.F.P., D.D.H.; Data Collection and/ or Processing - M.F.P., H.H.E., J.B.K., E.R.A., D.D.H.; Analysis and/or Interpretation - M.F.P., H.H.E., D.D.H.; Literature Search - M.F.P., D.D.H.; Writing - M.F.P., H.H.E., D.D.H.; Critical Reviews - M.F.P., H.H.E., J.B.K., E.R.A., D.D.H.
Conflict of Interest: The authors have no conflicts of Interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Tan J, Yu D, Feng Y, Song Q, You J, Shi H, et al. Comparative study of the efficacy of the canalith repositioning procedure versus the vertigo treatment and rehabilitation chair. Acta Otolaryngol. 2014;134:704–8. doi: 10.3109/00016489.2014.899711. [DOI] [PubMed] [Google Scholar]
- 2.Choung YH, Shin YR, Kahng H, Park K, Choi SJ. ‘Bow and lean test’ to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116:1776–81. doi: 10.1097/01.mlg.0000231291.44818.be. [DOI] [PubMed] [Google Scholar]
- 3.Büki B, Tarnutzer AA. Vertigo and dizziness. 1st ed. United States of America: Oxford University Press; 2014. [DOI] [Google Scholar]
- 4.West N, Hansen S, Moller MN, Bloch SL, Klokker M. Repositioning chairs in benign paroxysmal positional vertigo: Implications and clinical outcome. Eur Arch Otorhinolaryngol. 2016;273:573–80. doi: 10.1007/s00405-015-3583-z. [DOI] [PubMed] [Google Scholar]
- 5.Kim JS, Zee DS. Clinical practice. benign paroxysmal positional vertigo. N Engl J Med. 2014;370:1138–47. doi: 10.1056/NEJMcp1309481. [DOI] [PubMed] [Google Scholar]
- 6.Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, et al. Clinical practice guideline: Benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008;139(5 Suppl 4):S47–81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Soto-Varela A, Rossi-Izquierdo M, Santos-Perez S. Benign paroxysmal positional vertigo simultaneously affecting several canals: A 46-patient series. Eur Arch Otorhinolaryngol. 2013;270:817–22. doi: 10.1007/s00405-012-2043-2. [DOI] [PubMed] [Google Scholar]
- 8.Nakayama M, Epley JM. BPPV and variants: Improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005;133:107–12. doi: 10.1016/j.otohns.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Richard-Vitton T, Seidermann L, Fraget P, Mouillet J, Astier P, Chays A. Benign positional vertigo, an armchair for diagnosis and for treatment: Description and significance. Rev Laryngol Otol Rhinol (Bord) 2005;126:249–51. [PubMed] [Google Scholar]
- 10.Wang J, Chi FL, Jia XH, Tian L, Richard-Vitton T. Does benign paroxysmal positional vertigo explain age and gender variation in patients with vertigo by mechanical assistance maneuvers? Neurol Sci. 2014;35:1731–6. doi: 10.1007/s10072-014-1822-5. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, et al. Clinical practice guideline: Benign paroxysmal positional vertigo (update) Otolaryngol Head Neck Surg. 2017;156:S1–S47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 12.Richard Vitton T, Petrak MBD. The TVR chair: Introductory concepts. Hear Rev. 2013;20:52–4. [Google Scholar]
- 13.Epley JM. The canalith repositioning procedure: For treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107:399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 14.Yacovino DA, Hain TC, Gualtieri F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol. 2009;256:1851–5. doi: 10.1007/s00415-009-5208-1. [DOI] [PubMed] [Google Scholar]
- 15.Babac S, Djeric D, Petrovic-Lazic M, Arsovic N, Mikic A. Why do treatment failure and recurrences of benign paroxysmal positional vertigo occur? Otol Neurotol. 2014;35:1105–10. doi: 10.1097/MAO.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 16.Hajiabolhassan F, Tavanai E. Spontaneous nystagmus in benign paroxysmal positional vertigo: Is it a new sign? Acta Med Iran. 2013;51:903–6. [PubMed] [Google Scholar]
- 17.Soto-Varela A, Santos-Perez S, Rossi-Izquierdo M, Sanchez-Sellero I. Are the three canals equally susceptible to benign paroxysmal positional vertigo? Audiol Neurootol. 2013;18:327–34. doi: 10.1159/000354649. [DOI] [PubMed] [Google Scholar]
- 18.Tan J, Yu D, Feng Y, Song Q, You J, Shi H, Yin S. Comparative study of the efficacy of the canalith repositioning procedure versus the vertigo treatment and rehabilitation chair. Acta Otolaryngol. 2014;134:704–8. doi: 10.3109/00016489.2014.899711. [DOI] [PubMed] [Google Scholar]
- 19.Li JC, Epley J. The 360-degree maneuver for treatment of benign positional vertigo. Otol Neurotol. 2006;27:71–7. doi: 10.1097/01.mao.0000188350.52053.d6. [DOI] [PubMed] [Google Scholar]
- 20.Nakayama M, Epley J. BPPV and Variants: Improved Treatment Results with Automated, Nystagmus-Based Repositioning. Otolaryngol Head Neck Surg. 2005;133:107–12. doi: 10.1016/j.otohns.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 21.Martens C, Goplen FK, Aasen T, Nordfalk KF, Nordahl SHG. Dizziness handicap and clinical characteristics of posterior and lateral canal BPPV. Eur Arch Otorhinolaryngol. 2019;276:2181–9. doi: 10.1007/s00405-019-05459-9. [DOI] [PubMed] [Google Scholar]
- 22.West N, Hansen S, Bloch S, Moller MN, Klokker M. Behandling af benign paroksysmal positionel vertigo. Ugeskr Læger. 2017;179:V11160784. [PubMed] [Google Scholar]