Abstract
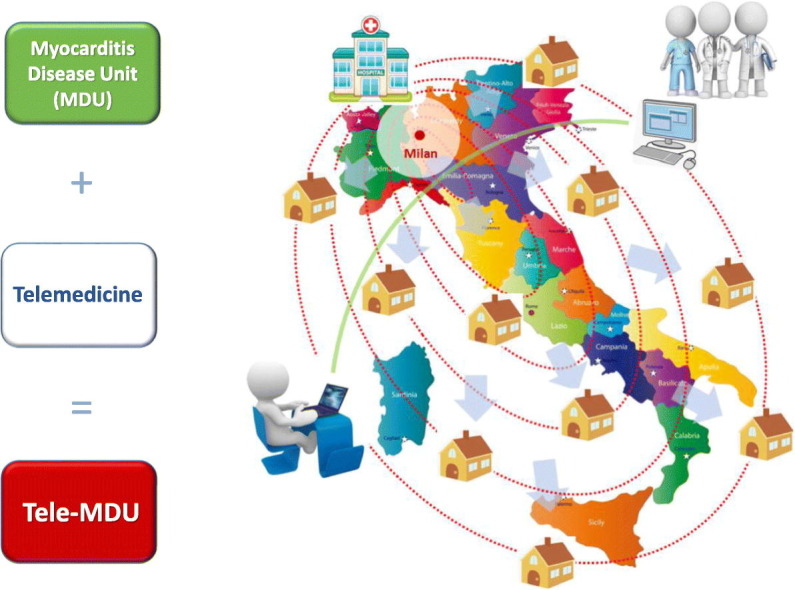
Myocarditis Disease Unit (MDU) is a functional multidisciplinary network designed to offer multidisciplinary assistance to patients with myocarditis. More than 300 patients coming from the whole Country are currently followed up at a specialized multidisciplinary outpatient clinic. Following the pandemic outbreak of the SARS-CoV-2 infection in Italy, we present how the MDU rapidly evolved to a “tele-MDU”, via a dedicated multitasking digital health platform.
Graphical Abstract
Novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection causing the COVID-19 worldwide pandemic is a clinical priority with incalculable impact on global health and economy.1 Following the Government and local institutions indications, mobilization of citizens was heavily restricted. Subsequently, because of both quarantaine precautions and limited access to hospitals, patients with chronic diseases are at high risk of follow-up discontinuation, potentially leading to dangerous effects. However, modern technologies may offer an alternative way to keep contact with patients and monitoring the evolution of their diseases. We present how our multidisciplinary “disease unit” for myocarditis rapidly evolved, to comply with the COVID-19-related national health emergency. No extramural funding was used to support this work. The authors are solely responsible for the design, analyses and editing of the paper.
Myocarditis Disease Unit
In last years, efforts have been made at our Institution, to offer multidisciplinary assistance to patients with myocarditis. In fact, myocarditis is an extremely complex disease from multiple viewpoints: clinical, since almost all cardiological presentations have been described at the disease onset, ranging from infarct-like chest pain, to heart failure, to a broad spectrum of arrhythmias2; diagnostic, since baseline workup includes both endomyocardial biopsy (EMB), as the recognized gold standard for histotyping and etiology definition, and noninvasive panoramic imaging techniques like cardiac magnetic resonance of positron emission tomography2 , 3; prognostic, since natural history ranges from mild self-limiting disease, to acute-phase fatal complications, or chronic evolution towards dilated cardiomyopathy2 , 4; therapeutical, since on top of cardiological treatment, etiology-specific therapy including immunosuppression may be required.2 , 5
In 2013 we created a dedicated Myocarditis Disease Unit (MDU) at our institution, to provide multidisciplinary care to all our patients with myocarditis. In particular, as a third-level referral center for arrhythmia management, we mainly focused on myocarditis patients with arrhythmic manifestations.6 , 7 Patient follow-up occurs according to a defined time schedule, by clinical and multimodal diagnostic reassessment. Furthermore, weekly MDU meetings are planned, to discuss about new clinical cases, and the most demanding ones.
MDU composition and operative tasks are presented in Figures S1 and S2. Currently, 315 patients with myocarditis are actively followed by the MDU at our Institution. Of them, 105 live in Milan and suburbs (33%), 82 in different Lumbardy areas (26%), and 128 in other Italian regions (41%).
Evolution to a “Tele-MDU”
Following the pandemic outbreak of the SARS-CoV-2 infection, the Italian Government directives forced citizens to a drastic reduction of their mobility. As an additional limiting factor, our Institution was selected as a COVID-19 referral center within a defined hub-and-spoke network involving all surrounding hospitals.8 Subsequently, the entire in-hospital activity was rapidly reorganized, to face the ongoing healthcare emergency. In particular, in-hospital length of stay for the non-COVID patients was reduced to a minimum; all non-life saving procedures, including non-emergent EMB, were indefinitely postponed; and all outpatients clinics, including the myocarditis polyambulatory, were forced to a temporary closure.8
Thus, to meet the needs of both our historical patient cohort, and the newly-diagnosed myocarditis cases, we rapidly reorganized the entire MDU to transfer our multidisciplinary activity on a virtual platform.
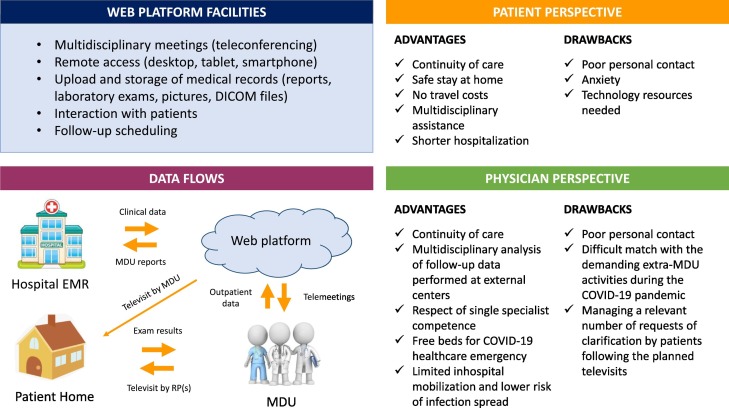
HealthMeeting®, developed by Wezen Technologies s.r.l., is a HTML5 web platform designed to organize multidisciplinary activities. Participants can attend meetings by using any kind of desktop, tablet or smartphone device. Medical reports and images are integrated in the platform through a middleware managing all HL7 and DICOM data flows. A bidirectional link connects the platform with the local hospital software, containing clinical data of both inpatients and outpatients visited at our Institution. Communication is allowed among medical specialists via video and audio teleconferencing. Patients can be invited to join meetings, but do not have direct access to the platform. Privacy and sensitive data are protected by both cybersecurity, and special support from the legal office at our Institution. In particular, all the involved physicians were required to fill dedicated registration forms. Ad-hoc informed consent was also obtained from all patients before their enrollment. For both patients and physicians, the software supporting the platform was offered at no costs. The main features of the platform are summarized in Figure 1 and online supplements.
Figure 1.
Applications of telemedicine to MDU. Telemedicine applications to MDU are summarized. Left panel: The main facilities of the adopted web platform (top) are presented together with the new organization of data flows (bottom) at the time of COVID-19 pandemic. Although all myocarditis patients were discussed by tele-MDU, to optimize resources most of the televisits were performed by designated referral physicians (RPs) via hybrid models of care (including video/phone calls, secure email, or in-person visits for urgent cases). Right panel: The main advantages and drawbacks felt by both patients (top) and physicians (bottom) are reported. Further detail are reported in online supplements.
COVID-19, disease caused by the severe acute respiratory syndrome coronavirus 2 during the current worldwide pandemics; EMR, Electronic Medical Records; MDU, Myocarditis Disease Unit; RPs, referral physicians.
Application and results
Referring to our MDU, the platform allowed for multiple tasks: (1) creating a “multidisciplinary report” with specific indications by any specialist involved, regarding diagnostic tests, follow-up exams, and treatment modification; (2) sharing reports with the patient; (3) reporting regular updates about patients follow-up, including required exams and pictures upload, with respect to the time schedule planned at a real outpatient checkup visit; (4) discussing updates among members of the “tele-MDU”; (5) communicating multidisciplinary recommendations to the patient, anytime during follow-up, until the discharge from MDU.
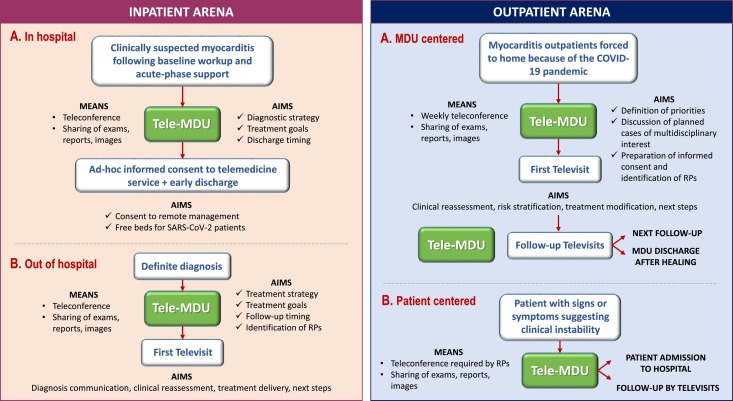
As shown in Figure 2 , tele-MDU was applied to both inpatient and outpatient arenas. In particular, the new cases of clinically suspected myocarditis underwent forced early discharge from hospital, while still waiting for the results of EMB: by digital health technology, results of EMB were communicated to patients and, following an oral tele-interview to exclude any contraindication, optimal etiology-based treatment was promptly started.2 , 5 Deployment of such a system on inpatients allowed for subsequent transition of care to the outpatient setting. Provided patient written informed consent, there were no restrictions to tele-MDU application, and the model was virtually extended to the whole outpatient cohort. Although all cases were discussed in a team, to optimize resources and save time, most of the televisits were performed by designated referral physicians (Figure 1). Hybrid models were applied, including video/phone calls, secure email correspondence, and in-person visits for urgent cases. Priority was given to patient requiring prompt decision making, as those at beginning/termination of immunosuppressive therapy, or those with any sign or symptom suggesting clinical instability. Otherwise, the chronological order of visits was followed, as prior to the forced polyambulatory closure during the COVID-19 pandemic. Exams strictly requiring in-person visit were performed at external centers nearby patient home. Whenever applicable, remote monitoring was activated for all device carriers.8
Figure 2.
Tele-MDU functions at the time of COVID-19 pandemic
Tele-MDU functions during the COVID-19 pandemic are shown for both the inpatient (left panel) and outpatient arenas (right panel). Left panel: Inpatient arena: during the in-hospital phase (A), patients were discharged as soon as clinically acceptable, even before knowing the results of endomyocardial biopsy; the definite diagnosis of myocarditis, and subsequent therapeutic and follow-up plans were communicated via telemedicine (B). Right panel: Outpatient arena: in clinically stable outpatients, follow-up timeline was defined by the tele-MDU (A), according to the predefined polyambulatory agenda; in the presence of symptoms or signs suggesting clinical instability, as assessed by the referral physician and notified to the MDU, a patient-centered approach was applied (B): in particular, additional MDU telemeetings were planned, or at least a priority was assigned, to ensure a prompt decision making.
COVID-19, disease caused by the severe acute respiratory syndrome coronavirus 2 during the current worldwide pandemics; MDU, Myocarditis Disease Unit; RPs, referral physicians.
By 4-month initial experience, we applied our tele-MDU model to 144 patients. Full details are reported in Table I . Of note, we reported no inpatients with SARS-CoV-2 genome in myocardium, and no opportunistic COVID-19 infections among outpatients on active immunosuppression. Also, there were compliance issues and no lost to follow-up.
Table I.
Results of a 4-month tele-MDU experience.
| Parameters | Units | Values |
|---|---|---|
| Inpatients Followed by tele-MDU (Feb-May 2020): N = 29/29 (100%) | ||
| Age | Mean ± SD | 43 ± 11 |
| Male gender | N (%) | 18 (62) |
| SARS-CoV-2 infection | N (%) | 4 (14) |
| Discharged without EMB results | N (%) | 28 (97) |
| Inhospital days spared based on planned stay | Mean ± SD | 6 ± 2 |
| EMB-proven myocarditis | N (%) | 20 (69) |
| SARS-CoV-2 viral genome in myocardium | N (%) | 0 (0) |
| Antiviral therapy | N (%) | 4 (14) |
| Immunosuppressive therapy | N (%) | 18 (62) |
| Outpatients Followed by tele-MDU (Feb-May 2020): N = 115/315 (37%) | ||
| Age | Mean ± SD | 47 ± 13 |
| Male gender | N (%) | 78 (68) |
| Pediatric cases | N (%) | 2 (2) |
| Living outside Milan | N (%) | 76 (66) |
| Blood exams | N (%) | 115 (100) |
| Holter ECG | N (%) | 83 (72) |
| Device remote monitoring (ICD or ILR) | N (%) | 51 (44) |
| Echocardiogram | N (%) | 102 (89) |
| CMR | N (%) | 18 (16) |
| FDG-PET | N (%) | 4 (3) |
| Genetic test | N (%) | 5 (4) |
| Ongoing immunosuppressive therapy | N (%) | 82 (71) |
| Treatment starting | N (%) | 4 (3) |
| Treatment termination | N (%) | 6 (5) |
| Inhospital admission for new EMB | N (%) | 3 (3) |
| Deaths | N (%) | 0 (0) |
| New disease-related hospitalizations | N (%) | 2 (2) |
| New ICD implants following ILR home-monitoring | N (%) | 1 (1) |
| Hospitalizations for SARS-CoV-2 infection | N (%) | 1 (1) |
| Documented SARS-CoV-2 positivity | N (%) | 3 (3) |
| Lost in follow-up | N (%) | 0 (0) |
| Total MDU televisits N = 149 in 144 patients | ||
| Direct engagement by tele-MDU | N (%) | 9 (6) |
| Indirect engagement by RPs | N (%) | 140 (94) |
| -Video call | Fraction | 8/140 |
| -Phone call | Fraction | 81/140 |
| -Secure email | Fraction | 117/140 |
| Televisit followed by in-person visit | N (%) | 3 (2) |
| Single missed calls | N (%) | 22 (15) |
| Multiple missed calls | N (%) | 1 (1) |
| Device connection problems | N (%) | 2 (1) |
| Perception of poor compliance | N (%) | 3 (2) |
| Requests of single clarification following televisit | N (%) | 45 (30) |
| Requests of multiple clarifications following televisit | N (%) | 31 (21) |
Results of tele-MDU application to 144 patients with newly or previously diagnosed myocarditis are shown in our 4-month experience. For patients living outside Milan, follow-up exams requiring in-person presence were all performed at external centers nearby home; results were transmitted to a referral physician, who subsequently shared data with the tele-MDU. The only hospitalization for SARS-CoV-2 infection pneumonia occurred in a patient more than 1 year after immunosuppression withdrawal: the patient was admitted to the local hospital, and discharged after 10 days with no complications. In the meanwhile, the MDU referral physician was unable to contact the patient: that was the single reported case of multiple missed calls.
CMR, cardiac magnetic resonance; EMB, endomyocardial biopsy; FDG-PET, 18F-fluorodeoxyglucose positron emission tomography; ICD, implantable cardioverter defibrillator; ILR, implantable loop recorder; MDU, Myocarditis Disease Unit; RPs, referral physicians; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SD, standard deviation.
Our research has multiple points worth highlighting: (1) to our knowledge, this is the first report about myocarditis management by multidisciplinary MDU; (2) thanks to the great coordinated efforts among the multiple operative units involved, the transition to tele-MDU was remarkably rapid; (3) to optimize hospital resources during a healthcare emergency, tele-MDU was primarily considered for inpatients, and subsequently translated to outpatients, offering a novel scenario for telemedicine application.
Limitations and challenges
Although requiring further optimization, our model reflects the provision of care of a “home hospital”, which was previously demonstrated effective in reducing cost, health care use, and readmissions, while improving patient experience.9 , 10 At this stage, constant patient-clinician engagement was maintained not only by platform, but also by email, telephone, video, and in-person reassessment, consistently with the hybrid models of care.11 The transition to tele-MDU was generally well-accepted by all the participants, also because of the young age of the participants. Challenges could be expected by extending our model to other settings, like elderly patients with chronic diseases and subjects with low socioeconomic status or limited access to technology.12 Figure 1 summarizes the main limitations of our model, as felt from both patient and physician viewpoints: ad-hoc questionnaires could be helpful to collect more accurate data. In our experience, the limited sample size allowed easy definition of priorities by in-person assessment of the MDU physicians: strategies for developing automated priority codes or creating direct connections with the polyambulatory agenda could be implemented in the future for a more fluid management of follow-up visits. Finally, because of the disease complexity and multidisciplinary expertise required, our model for myocarditis might be not easily reproduced outside tertiary centers.
Conclusion
We presented our multidisciplinary MDU and its rapid evolution to offer continuity of care to all our patients with previously- or newly-diagnosed myocarditis. Based on our expectations and preliminary findings, telemedicine is an effective way to follow-up patients suffering from a complex disease requiring constant multidisciplinary surveillance.
Of note, we felt that remote monitoring allowed to directly engage quarantined people in their homes; to actively promote communication between patients and their caregivers; to work out and communicate patient-tailored diagnostic and therapeutic strategies; and to monitor disease evolution.
In the current COVID-19 crisis, physicians are called to familiarize themselves with the technologies available at their own and other institutions, to guarantee the best remote care for their patients.
Acknowledgements
All people working hard in our country in this difficult period are strongly acknowledged for their massive efforts and daily care for critically ill patients suffering from SARS-CoV-2 infection. In particular, we would like to thank all nurses, anesthesiologists, infectious diseases specialists, and the whole emergency personnel working at our institution.
Footnotes
Funding: None.
Disclosures: All the authors have no conflicts of interest to disclose regarding the content of this paper.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ahj.2020.07.015.
Appendix. Supplementary data
Supplementary material
References
- 1.Wang C., Horby P.W., Hayden F.G. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caforio A.L., Pankuweit S., Arbustini E. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636–2648. doi: 10.1093/eurheartj/eht210. [DOI] [PubMed] [Google Scholar]
- 3.Palmisano A., Vignale D., Peretto G. Hybrid FDG-PET/MR or FDG-PET/CT to detect disease activity in patients with persisting arrhythmias after myocarditis. JACC Cardiovasc Imaging. 2020 doi: 10.1016/j.jcmg.2020.03.009. S1936-878X(20)30266-7. [DOI] [PubMed] [Google Scholar]
- 4.Ammirati E., Cipriani M., Moro C. Clinical presentation and outcome in a contemporary cohort of patients with acute myocarditis: multicenter Lombardy Registry. Circulation. 2018 Sep 11;138:1088–1099. doi: 10.1161/CIRCULATIONAHA.118.035319. [DOI] [PubMed] [Google Scholar]
- 5.De Luca G., Campochiaro C., Sartorelli S. Therapeutic strategies for virus-negative myocarditis: a comprehensive review. Eur J Intern Med. 2020;77:9–17. doi: 10.1016/j.ejim.2020.04.050. S0953–6205(20)30170–9. [DOI] [PubMed] [Google Scholar]
- 6.Peretto G., Sala S., Rizzo S. Arrhythmias in myocarditis: state of the art. Heart Rhythm. 2019 May;16:793–801. doi: 10.1016/j.hrthm.2018.11.024. [DOI] [PubMed] [Google Scholar]
- 7.Peretto G., Sala S., Rizzo S. Ventricular arrhythmias in myocarditis: characterization and relationships with myocardial inflammation. J Am Coll Cardiol. 2020 Mar 10;75:1046–1057. doi: 10.1016/j.jacc.2020.01.036. [DOI] [PubMed] [Google Scholar]
- 8.Mazzone P., Peretto G., Radinovic A. The COVID-19 challenge to cardiac electrophysiologists: optimizing resources at a referral center. J Interv Card Electrophysiol. 2020;18:1–7. doi: 10.1007/s10840-020-00761-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levine D.M., Ouchi K., Blanchfield B. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172:77–85. doi: 10.7326/M19-0600. [DOI] [PubMed] [Google Scholar]
- 10.Leff B. Defining and disseminating the hospital-at-home model. CMAJ. 2009;180:156–157. doi: 10.1503/cmaj.081891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yellowlees P., Chan S.R., Burke Parish M. The hybrid doctor-patient relationship in the age of technology—telepsychiatry consultations and the use of virtual space. Int Rev Psychiatry. 2015;27:476–489. doi: 10.3109/09540261.2015.1082987. [DOI] [PubMed] [Google Scholar]
- 12.Hjelm N.M. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11:60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material