Abstract
Contrast-enhanced chest computed tomography (CT) is not considered part of the evaluation of myocardial infarction. However, acute myocardial infarction has been detected on contrast-enhanced chest CT as areas of decreased myocardial enhancement in patients evaluated for other indications, such as pulmonary embolism and aortic dissection. We present a case of acute myocardial infarction on a nongated chest CT in a 67-year-old male who presented with atypical chest pain and initial nondiagnostic electrocardiogram. This case highlights that acute myocardial infarction may be detectable on contrast-enhanced CT. When evaluating contrast-enhanced chest CT's for other etiologies of chest pain, radiologists should look for potential myocardial perfusion abnormalities that can provide clues to the presence of myocardial infarction.
Keywords: Contrast-enhanced chest computed tomography, Acute myocardial infarction, Atypical chest pain, Decreased myocardial enhancement
Introduction
Acute myocardial infarction (MI) is diagnosed by the presence of clinical symptoms of myocardial ischemia, elevated cardiac biomarkers, new ischemic electrocardiogram changes, and imaging evidence of new loss of viable myocardium or new regional wall motion abnormalities by echocardiography or magnetic resonance [1]. However, a substantial number of patients may have atypical or no symptoms on initial presentation, while some others may have unrevealing electrocardiogram changes and/or troponin levels, leading to a misdiagnosis and under-treatment of these patients with subsequent poor clinical outcomes [2,3]. Contrast-enhanced chest computed tomography (CT) is not considered part of the evaluation of MI. However, acute MI has been detected on contrast-enhanced chest CT as areas of decreased myocardial enhancement in patients evaluated for other indications, such as pulmonary embolism and aortic dissection [4]. CT scanning is a fast and noninvasive tool; considering that time is of the essence in restoring coronary flow to save the viable myocardium in patients with acute coronary syndrome, CT chest could be of utility in evaluating patients with acute MI, especially in those with unrevealing cardiac work up or atypical presentation.
Case report
A 67-year-old man with hypertension and gastritis presented to the emergency department with two days of abdominal pain radiated to the middle of the chest and back. Physical examination was notable for elevated blood pressure (180/96 mmHg) and epigastric tenderness. Electrocardiogram (ECG) upon arrival showed prominent Q-waves in V1-V3 (Fig. 1). Laboratory tests revealed elevated serum troponin I (0.797 ug/L) and creatine kinase (613 U/L) levels. CT scan of the chest with contrast was performed to rule out aortic dissection and pulmonary embolism which showed demarcated perfusion abnormality in the anterior, septal and apical myocardium (Fig. 2). A repeat ECG showed ST-segment elevation in leads V2-V3, I, and AVL with prominent Q-waves in V1-V4 and reciprocal ST-segment depression in lead II, III and AVF, confirming an anteroseptal MI (Fig. 3). Transthoracic echocardiogram demonstrated a large region of apical akinesis extending into the mid septum and mid anterior segment with a left ventricular ejection fraction of 35%. The patient underwent coronary catheterization which showed 80% stenosis of the left main (LM) coronary artery, 100% stenosis of the mid-left anterior descending artery (LAD) and 99% stenosis of the first diagonal branch (Fig. 4). Successful percutaneous coronary intervention of LM to proximal LAD and mid LAD was done, reestablishing normal coronary flow.
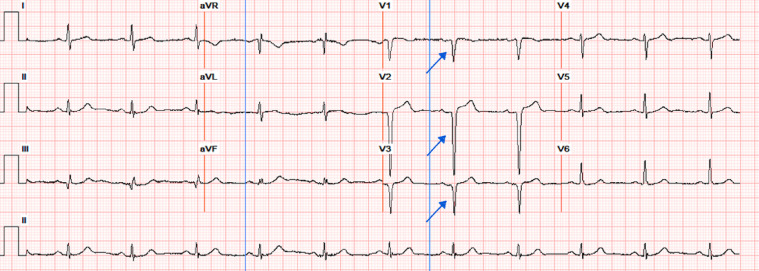
Fig. 1.
12 lead ECG demonstrating prominent Q-waves in V1-V3.
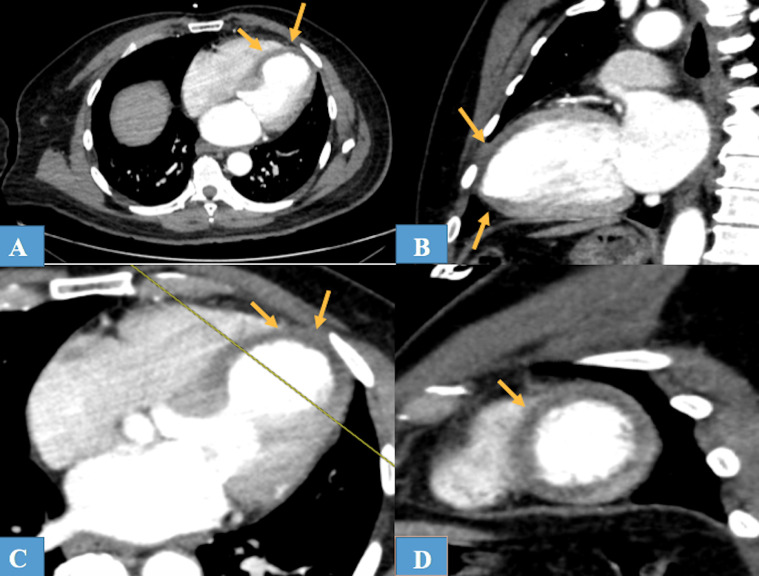
Fig. 2.
CT scan of the heart following iodine-contrast injection. Horizontal long axis (A), vertical long axis (B) and short axis with localizer (C and D). Note sharply demarcated area of decreased enhancement of the anterior, septal and apical segments of the left ventricle.
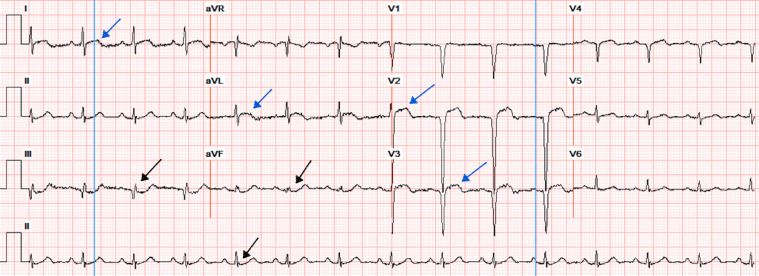
Fig. 3.
12 lead ECG demonstrating ST segment elevation in V2-V3, I, AVL (blue arrows) with Q-waves in V1-V4, and reciprocal ST depression in II, III, and AVF (black arrows).
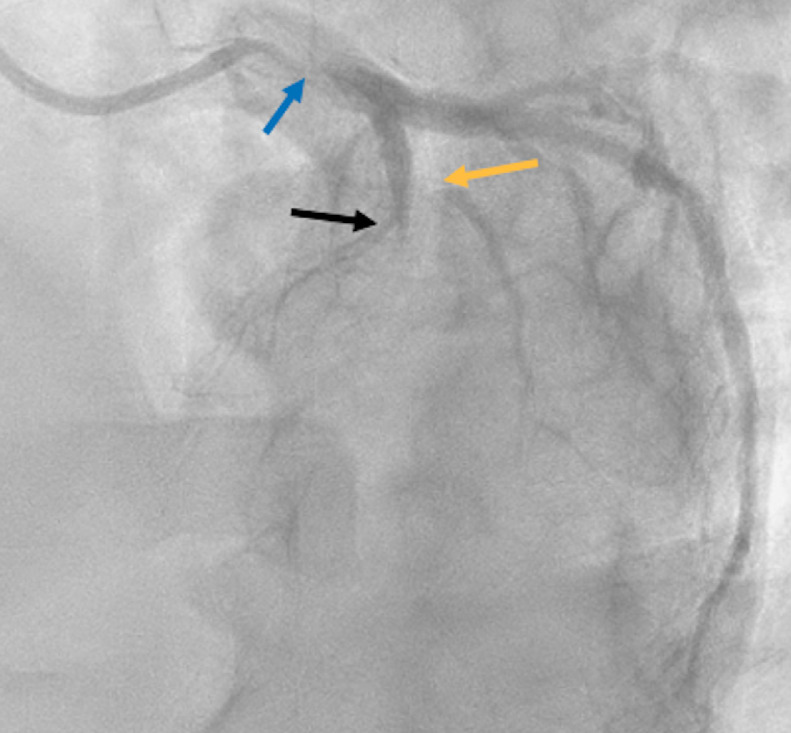
Fig. 4.
Cardiac catheterization imagine indicating 80% stenosis of the left main coronary artery (blue arrow), total occlusion of the mid left anterior descending artery (black arrow), and 99% stenosis of the first diagonal branch (yellow arrow).
Discussion
Contrast-enhanced chest CT is not commonly used for the evaluation of acute coronary syndrome [1]. Nonetheless, CT has a leading role in the diagnosis of entities with similar clinical presentations to those with acute MI, such as pulmonary embolism and aortic dissection [5]. Although MI is generally better seen on cardiac-gated CT and cardiac MRI, advancements in multidetector CT have enhanced the visualization of cardiac pathology on routine CT by decreasing the prevalence of beam-hardening artifacts [6]. In one study of 18 patients presenting with chest discomfort and primary scan indications of pulmonary malignancy, pulmonary embolism, or aortic dissection, MI was incidentally found in 15 patients as a focal area of decreased left ventricular myocardial enhancement in a specific coronary arterial distribution with a suggested sensitivity of CT for detecting an initial acute MI of 83% and specificity of 95% [4]. However, although encouraging, these findings have not been reproduced in cohort studies. Moreover, there are some limitations when detecting MI on nongated CT. The time interval between MI and visual detection on CT scan is not well established and can vary between 1-26 days after the onset of symptoms [4]. In addition, the late phase-contrast administration is required to visualize perfusion abnormalities, which is not routinely performed in a pulmonary artery protocol [7]. Last, both acute and chronic MI can be detected as areas of hypodensity or perfusion defects in a coronary artery territory. Even though it has been suggested that longstanding MI can have ventricular dilation and significantly lower CT attenuation compared with an acute MI, these findings have only been reported in cardiac CT studies [8]. Therefore, although contrast-enhanced CT findings look promising and may be useful, especially in patients who present with atypical chest pain, further studies are needed to assess the complete role and significance of contrast-enhanced chest CT in the evaluation of acute M
Conclusion
This case highlights that acute MI may be detected on contrast-enhanced CT. Although further studies are needed to assess the complete role and significance of contrast-enhanced chest CT in the evaluation of acute MI, radiologists should be aware of this and scan the myocardium for potential perfusion abnormalities when evaluating chest CT's in patients who present with chest pain or clinical picture atypical for acute MI and undergo contrast-enhanced chest CT to rule out other diagnoses (eg, PE, aortic dissection). Looking for myocardial perfusion abnormality can provide clues to the presence of MI contributing to an early diagnosis and treatment.
Footnotes
Conflicts of Interest: The authors declare that there is no conflicts of interest.
References
- 1.Thygesen K., Alpert J.S., Jaffe A.S. Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018) Circulation. 2018;138:e618–e651. doi: 10.1161/CIR.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 2.Brieger D., Eagle K.A., Goodman S.G. GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126:461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 3.Canto J.G., Shlipak M.G., Rogers W.J. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283:3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 4.Gosalia A., Haramati L.B., Sheth M.P., Spindola-Franco H. CT detection of acute myocardial infarction. AJR. 2004;182:1563–1566. doi: 10.2214/ajr.182.6.1821563. [DOI] [PubMed] [Google Scholar]
- 5.Heiken J.P., Brink J.A., Vannier M.W. Spiral (helical) CT. Radiology. 1993;189:647–656. doi: 10.1148/radiology.189.3.8234684. [DOI] [PubMed] [Google Scholar]
- 6.Mckie S.J., Hardwick D.J., Reid J.H., Murchison J.T. Features of cardiac disease demonstrated on CT pulmonary angiography. Clin Radiol. 2005;60:31–38. doi: 10.1016/j.crad.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Mahnken A.H., Bruners P., Katoh M. Dynamic multi-section CT imaging in acute myocardial infarction: preliminary animal experience. Eur Radiol. 2006;16:746–752. doi: 10.1007/s00330-005-0057-5. [DOI] [PubMed] [Google Scholar]
- 8.Nieman K., Cury R.C., Ferencik M. Differentiation of recent and chronic myocardial infarction by cardiac computed tomography. Am J Cardiol. 2006;98:303–308. doi: 10.1016/j.amjcard.2006.01.101. [DOI] [PubMed] [Google Scholar]