Abstract
This cross-sectional study assesses the rate of COVID-19 infection among health care workers in a large community hospital.
New York City and its surrounding metro area have emerged as an epicenter of the coronavirus disease 2019 (COVID-19) outbreak worldwide. A recent population survey1 for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibodies among those in New York state shows a prevalence of 21.2% in New York City and 16.7% in Long Island. Across the US, up to 11% of reported COVID-19 cases were found to be in health care professionals,2 but the true prevalence of COVID-19 among health care workers is unknown. The aim of the present study is to establish the rate of COVID-19 among health care workers by widespread screening for SARS-CoV-2 exposure.
Methods
Employees were tested with a reverse transcriptase–polymerase chain reaction (RT-PCR) test and an antibody test from March 1 to April 30, 2020, at a large tertiary community hospital in Roslyn, New York. The health system began offering antibody testing (Anti-SARS-CoV-2 ELISA [IgG] [EUROIMMUN US]; SARS-CoV2-IgG [Abbott]) on April 16, 2020, and encouraged all employees to be tested. Antibody testing was performed in workers who were asymptomatic or were previously symptomatic with no symptoms for at least 14 days. Hospital employees who had symptoms of COVID-19 were offered the RT-PCR test (cobas SARS-CoV-2 [Roche] and Xpert Xpress SARS-CoV-2 [Cepheid]). All testing was on a voluntary basis. Personal protective equipment (PPE) policy was based on US Centers for Disease Control and Prevention guidelines3 and was dependent on risk of exposure. All employees caring for patients with COVID-19 were required to wear an N95 mask, isolation gown, and gloves. Health care workers involved with procedures that could generate aerosolized virus dispersal, such as mechanical intubation, required additional eye protection. Both χ2 and t tests were used to generate P values and 95% CIs to analyze categorical variables. All statistical analyses were performed using SAS version 9.4 (SAS Institute). The Institutional Review Board at St Francis Hospital approved the study and waived the need for informed consent due to its retrospective nature and anonymization of all employee data.
Results
Among 3046 employees, 1699 (56%) underwent antibody testing, 617 (20%) underwent RT-PCR testing, and 359 (12%) underwent both. The average (SD) age among all employees was 42.8 (13.8) years and 2137 (70%) were women (Table). When comparing employees who elected to undergo either form of testing vs those who did not, there were no meaningful differences with respect to age, job title, or work area.
Table. Breakdown of the Reverse Transcriptase–Polymerase Chain Reaction (RT-PCR) and Antibody Results in Employees.
| Category | No. of employees | Age, mean (SD), y | Positive/tested, fraction (%) | Total COVID-19, No. (%) | ||
|---|---|---|---|---|---|---|
| Antibody | RT-PCR | Tested | Positive | |||
| All | 3046 | 42.8 (13.8) | 167/1699 (9.8) | 184/617 (29.8) | 1958 (64.3) | 290 (14.8) |
| Sex | ||||||
| Female | 2137 | 41.8 (13.5) | 118/1259 (9.4) | 132/461 (28.6) | 1450 (67.9) | 210 (14.5) |
| Male | 909 | 45.3 (14.1) | 49/440 (11.1) | 52/151 (34.4) | 508 (55.9) | 80 (15.7) |
| P value | .31 | .18 | .49 | |||
| Ethnicity | ||||||
| White | 1748 | 44.3 (14.4) | 94/1069 (8.8) | 92/346 (26.6) | 1192 (68.2) | 156 (13.1) |
| Black | 412 | 46.8 (12.3) | 24/168 (14.3) | 37/93 (39.8) | 233 (56.6) | 46 (19.7) |
| Hispanic | 407 | 41.4 (13.7) | 28/239 (11.7) | 31/88 (35.2) | 270 (66.3) | 47 (17.4) |
| Asian | 380 | 40.7 (12.4) | 19/182 (10.4) | 25/74 (33.8) | 216 (56.8) | 34 (15.7) |
| P value | .11 | .25 | .03 | |||
| Position | ||||||
| Ancillary | 660 | 46.5 (14.3) | 39/322 (12.1) | 38/115 (33.0) | 385 (58.3) | 62 (16.1) |
| Environmental | 189 | 48.8 (12.7) | 12/100 (12.0) | 15/35 (42.8) | 123 (65.1) | 23 (18.7) |
| Nurse | 1695 | 39.4 (13.0) | 99/1043 (9.5) | 111/376 (29.5) | 1183 (70.0) | 174 (14.7) |
| Physician | 196 | 52.1 (11.7) | 9/79 (11.4) | 6/24 (25.0) | 88 (44.9) | 12 (13.6) |
| Technologist | 306 | 43.9 (13.1) | 9/155 (5.8) | 14/60 (23.3) | 179 (58.5) | 19 (10.6) |
| P value | .27 | .30 | .33 | |||
| Department | ||||||
| ER | 120 | 41.6 (13.3) | 9/88 (10.2) | 11/35 (31.4) | 101 (84.2) | 18 (17.8) |
| Floor | 781 | 36.1 (12.7) | 60/489 (12.3) | 58/137 (42.3) | 542 (69.8) | 95 (17.5) |
| ICU | 544 | 41.7 (12.5) | 22/321 (6.9) | 38/146 (26.0) | 378 (69.5) | 52 (13.8) |
| Operational | 741 | 47.1 (13.9) | 42/400 (10.5) | 40/124 (32.3) | 459 (61.9) | 67 (14.6) |
| Procedural | 456 | 43.0 (12.7) | 22/243 (9.1) | 27/118 (22.9) | 291 (63.8) | 39 (13.4) |
| Other | 404 | 48.1 (12.9) | 12/158 (7.6) | 10/52 (19.2) | 187 (46.3) | 19 (10.2) |
| P value | .17 | .004 | .16 | |||
Abbreviations: COVID-19, coronavirus disease 2019; ER, emergency room; ICU, intensive care unit.
There were 167 employees (9.8%) who tested positive for antibodies. There was no significant difference in antibody positive rates across job titles or work areas (Figure). When comparing the prevalence of antibodies among hospital employees with the rate reported by the State of New York for the general public on Long Island, hospital employees had a significantly lower positive rate (9.9% vs 16.7%, P < .001).
Figure. Health Care Workers Who Tested Positive for SARS-CoV-2 Antibodies by Job Title and Department.
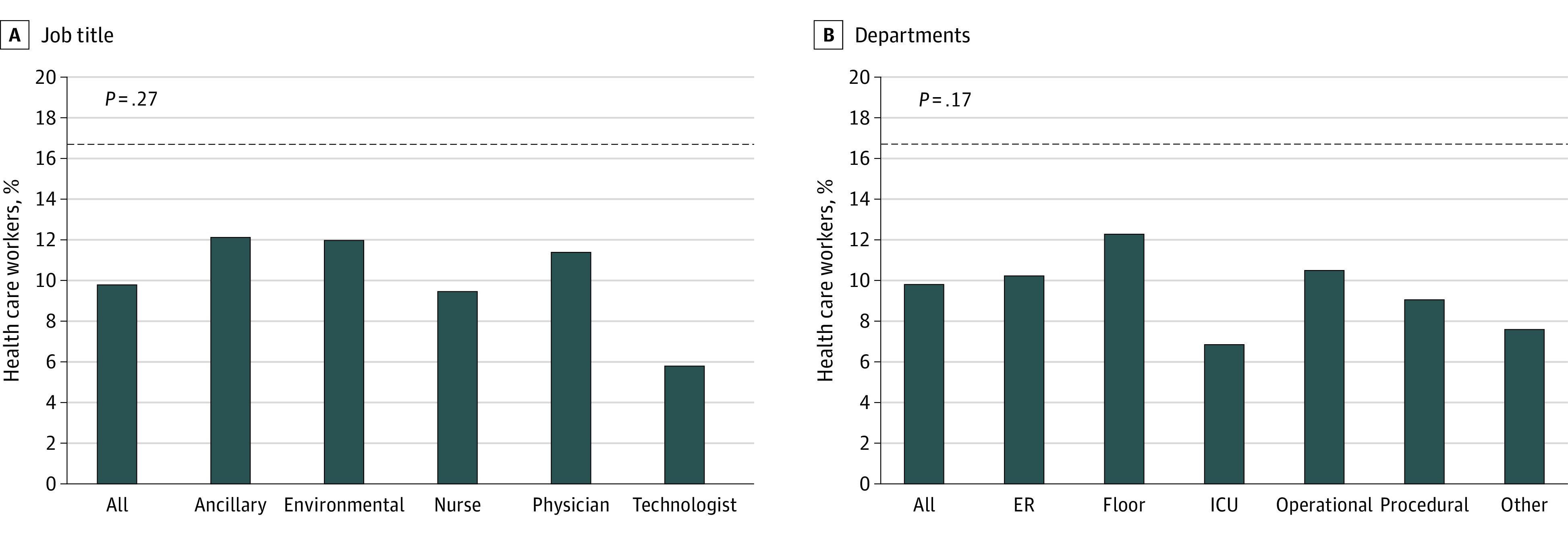
Percentage of employees who tested positive for antibodies based on job title (A) and department (B). The dotted line indicates the general population on Long Island. A total of 1699 employees were surveyed, including 322 in ancillary services, 100 in environmental health, 1043 nurses, 79 physicians, and 155 technologists. Of the 1699 employees, 88 worked in the emergency room (ER), 489 on the hospital floor, 321 in the intensive care unit (ICU), 400 in operational services (ie, employees who rotate through all areas of the hospital), 243 in procedural services (eg, operating room, cardiac procedures, diagnostic radiology procedures, endoscopy), and 158 in other services.
Employees with positive antibody test results were similar in age (41.5 [SD, 13.5] vs 43.4 [SD, 13.7] years, P = .09) and sex (women 9.4% vs men 11.1%, P = .31). There was no significant difference between race as a whole (Table). There was no significant difference in infection rates among those working in high vs low exposure areas (10.9% vs 10.9%, P = .99).
Discussion
The findings of the present study indicate that the rate of SARS-CoV-2 infection among health care workers is lower than what has been reported for the general public in the surrounding region. Given that health care workers in hospitals are exposed to a much higher density of the virus, this is strong evidence that current PPE practices are protective, easing health care workers’ concern and psychological distress.4
Limitations
Limitations of this study are that it is a single-center analysis from a large community hospital that has the capability to adequately supply PPE to all health care workers. The present results may therefore not be applicable to all health care settings. Testing for COVID-19 was offered on a voluntary basis, with most employees complying. While no differences were observed between those tested and those not tested, a potential selection bias cannot be completely excluded.
Conclusions
In conclusion, PPE, when available and properly used, confers protection and lower infection rates of COVID-19 among health care workers when compared with reported infection rates in the general public.
References
- 1.Amid ongoing COVID-19 pandemic, Governor Cuomo announces State Health Department will partner with Attorney General James to investigate nursing home violations. April 23, 2020. Accessed July 30, 2020. https://www.governor.ny.gov/news/amid-ongoing-covid-19-pandemic-governor-cuomo-announces-state-health-department-will-partner
- 2.CDC COVID-19 Response Team . Characteristics of health care personnel with COVID-19—United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):477-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Infection control guidance for healthcare professionals about coronavirus (COVID-19). Centers for Disease Control and Prevention. Updated June 3, 2020. Accessed May 1, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control.html
- 4.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]


