Abstract
AIM
To understand the impact of COVID-19 on radiology trainee experience and well-being.
MATERIALS AND METHODS
A questionnaire designed to capture the impact of COVID-19 on radiology training, working patterns, and well-being was sent to all speciality trainees in a regional UK radiology school. The survey was distributed at the beginning of May 2020 and responses collected over 2 weeks. Trainees were questioned about changes that had occurred over a time period starting at the beginning of the COVID-19 pandemic. All survey responses (n=29) were anonymised and the results were subsequently analysed.
RESULTS
Sixty-two percent (29 of 47) of trainees within the deanery, who were spread across seven different hospital sites, responded to the questionnaire. All trainees felt that overall radiology workload had decreased in response to COVID-19. Seventy-two percent (21/29) stated that their workload had significantly decreased. Seventy percent (19/27) reported decreased subspecialty experience, and 19% (5/27) reported a complete lack of subspecialty training. Twenty-four percent (7/29) of trainees were redeployed from radiology to clinical ward-based work. Forty-eight percent reported experiencing a worsening in their well-being compared to before the pandemic.
CONCLUSION
The first wave of the COVID-19 pandemic had a significant impact on training and well-being. Lessons learnt from this report should help prepare for a second-wave of COVID-19 or future pandemics.
Introduction
COVID-19 has to date infected over 6 million people worldwide and caused more than 350,000 deaths.1 Healthcare settings across the world have responded to this pandemic by modifying the way in which services are delivered and by redistributing their resources to create capacity. In the UK, most elective activity was cancelled in preparation for the first wave, with only emergency and urgent cancer work being performed.2 Staff have been re-distributed throughout community and hospital healthcare settings, with many redeployed to unfamiliar environments and roles. Hospital doctors have been redeployed from non-medical specialties onto medical rotas, so that doctors in specialties without routine ward-based patient contact, such as radiology, have been brought in to deliver direct clinical care for patients.
We present the results of a trainee-led survey conducted within a regional radiology school in England, UK, which explored the experience of radiology speciality trainees during these unprecedented times. The objectives were to assess the impact of the COVID-19 pandemic on workload, training, and trainee well-being, with the overarching aim of reporting key learning points from this experience, which could inform future planning by radiology schools in the event of a second-wave of COVID-19 or future pandemics.
Materials and methods
An online questionnaire (Electronic Supplementary Material Appendix S1) was distributed to all 47 radiology registrars training within a regional radiology school during the time of the first wave of COVID-19 in the UK. All survey responses were anonymised and the results were subsequently analysed. Ethical approval was not necessary for this survey as it was not considered to be research by NHS Health Research Authority criteria.3
Questionnaire
The questionnaire was designed to capture the impact of the pandemic on radiology training, working patterns, and well-being. To ensure that the survey was robust, it was piloted internally before distributing the final version. A link to the online questionnaire was sent to all 47 radiology trainees currently within the region on 5 May 2020. The link was distributed via a group on a mobile communications application, which was the most active local form of communications amongst the registrar body. Completion of this survey was entirely voluntary and a reminder to complete the survey was sent 11 May 2020. Responses were collected over 2 weeks. Trainees were questioned about changes that had occurred over a time period starting at the beginning of the COVID-19 pandemic in the UK (March 2020), up to the time of survey completion (May 2020). This timing was chosen, approximately 2 months into the pandemic, as by this time many radiology specialist trainees were well integrated into medical rotas and radiology departmental workflow changes in response to COVID-19 were well established.
Results
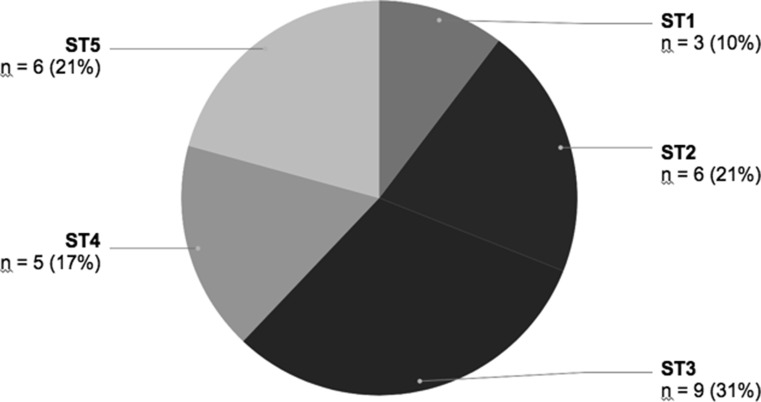
Twenty-nine of 47 (62%) radiology trainees within the school completed the questionnaire. The responses came from registrars working at university and district general hospitals across seven different hospital sites. The stage of training of the respondents ranged from speciality training (ST) years 1–5, with trainees from each year represented (Fig 1 ). All specialist trainees were working full time when the survey was completed, apart from one trainee who was in the third trimester of pregnancy and was on special leave following national guidance released by the Royal College of Obstetricians and Gynaecologists.
Figure 1.
The distribution of survey respondents by trainee year group.
Impact on workload
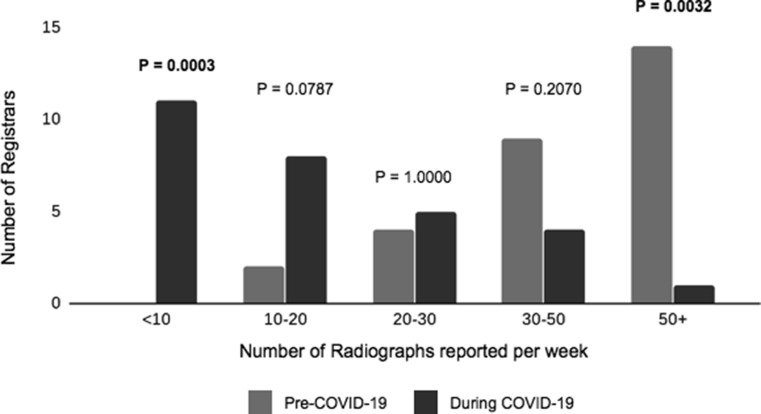
All trainees felt that overall radiology workload had decreased in response to COVID-19 and 72% (21/29) stated workload had significantly decreased. The current annual radiograph reporting targets within the deanery are 1,000, 2,000 and 3,000 for ST1, ST2 and ST3+, respectively. To meet these targets, it is generally advised that trainees in ST2 to ST5 aim to report at least 50 radiographs per week. At the time of survey completion, only one (3%) respondent was able to report >50 radiographs per week, whereas before the pandemic 48% (14/29) were reporting >50 radiographs per week, a statistically significant change (p=0.0032). Nearly 38% (11/29) were able to report only <10 radiographs per week, whereas before the pandemic no trainees were reporting <10 radiographs per week (Fig 2 ). This was found to be a statistically significant reduction in weekly plain film reporting figures using Fisher exact analysis (p=0.0003).
Figure 2.
A bar chart demonstrating differences in the number of radiographs reported weekly before and during the first wave of COVID-19.
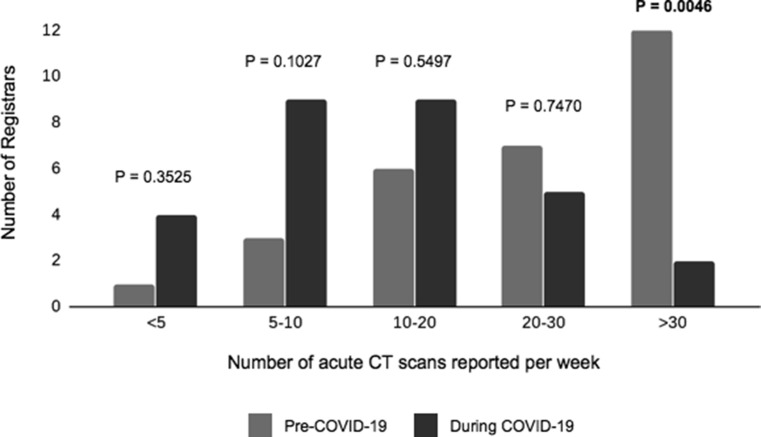
No specific targets for annual computed tomography (CT) or ultrasound reporting are set by the Deanery. Therefore, the parameters for assessing reporting figures for these studies were chosen by consensus amongst the authors, based on their experience of average pre-COVID workloads during on-call and routine outpatient sessions. There was a change in the number of acute CT examinations reported by trainees per week (Fig 3 ). Although 41% (12/29) were reporting >30 acute CT examinations per week before the pandemic, only 7% (2/29) were able to report this number at the time of survey (p=0.0046). Prior to the pandemic, only 34% (10/29) were reporting <20 acute CT examinations; however, this number increased to 76% (22/29) during the first wave of COVID-19.
Figure 3.
A bar chart demonstrating the difference in number of weekly acute CT examinations reported by trainees before and during the first wave of COVID-19.
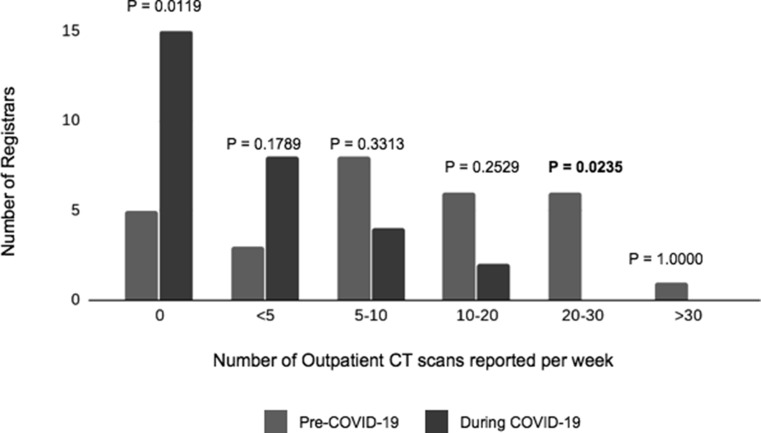
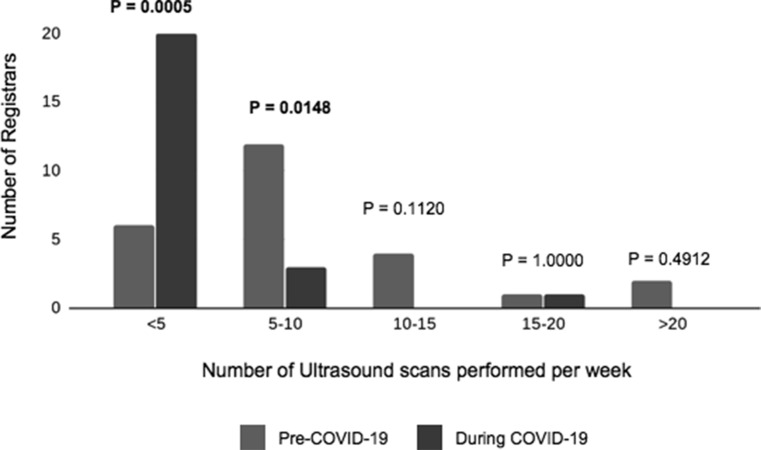
Before the pandemic, >80% of respondents were routinely reporting outpatient CT examinations; however, this fell to 50% during the pandemic (Fig 4 ). Of those who had competency to independently perform ultrasound examinations, 64% (16/25) performed between five and 15 examinations per week before the pandemic, whereas 80% (20/25) were only performing fewer than five ultrasound examinations per week during the pandemic (Fig 5 ). A similar trend was noted with magnetic resonance imaging (MRI) and interventional procedures. Seventy-three percent (16/29) reported a decreased workload in weekly MRI reporting. Eighty-five percent (17/29) reported fewer interventional procedures performed.
Figure 4.
A bar chart demonstrating the number of weekly outpatient CT reported by trainees before and during the first wave of the pandemic.
Figure 5.
A bar chart showing changes in weekly ultrasound experience.
Reporting of COVID-19 imaging investigations
With regards to specific training for reporting imaging performed to investigate COVID-19, only 7% (2/29) registrars received such teaching regularly and 41% (12/29) registrars received minimal training on the subject. The remaining registrars familiarised themselves with the imaging findings associated with the novel virus through peer teaching and/or using online resources, such as those provided by the British Society of Thoracic Imaging (BSTI).4 , 5
When asked whether they felt confident, mostly confident, or not confident reporting COVID-19-related chest radiographs, 52% felt confident and 45% felt mostly confident, with only one respondent (3%) feeling unconfident reporting these studies. For CT examinations, 41% felt confident and 48% felt mostly confident, with only two respondents (7%) not feeling confident with reporting CT findings of COVID-19 infection.
Departmental guidance on reporting COVID-19 imaging varied across the region. Forty-one percent of respondents had received clear departmental guidance that was being adhered to and 21% had received clear departmental guidance, which was mostly being followed. Twenty-eight percent had received suggestions of how to report these studies with no formal guidance disseminated, leading to much variation amongst departmental reports. One trainee reported having no local departmental guidance and two trainees were unsure whether any such guidance existed.
BSTI guidance on the reporting of COVID-19 studies included suggestions for tracking codes.4 , 5 Sixty-six percent of the respondents were adding audit or tracking codes to the end of their reports; however, 21% were not using such codes and 14% of respondents were unsure whether their department was tracking COVID-19 studies in this way.
Most trainees (90%) had access to a departmental PACS folder containing example cases of COVID-19 imaging. One respondent did not have access to such a folder and two were unsure of whether such a resource existed in their workplace.
Registrars had mostly (83%) been updated on departmental changes to imaging pathways during the pandemic, with the remainder of respondents feeling that this was not applicable to their practice (10%) or that they had not been updated (7%).
Teaching
When responding to the survey, 72% were attending a mix of face-to-face and virtual teaching sessions with just 27% having face-to-face teaching only. Twenty-four percent and 14% reported an increase in consultant and registrar-led teaching, respectively; however, 28% reported receiving no consultant-led teaching, 24% reported a decrease in consultant-led teaching, and 41% reported a decrease in peer-to-peer teaching during this time. Unfortunately, 10% could not access radiology teaching due to being redeployed and no sessions delivered over teleconferencing platforms were recorded.
Sub-specialty training
Sub-specialty training was reported to have reduced. Seventy percent (19/27) reported decreased subspecialty experience whereas 19% (5/27) reported a complete lack of subspecialty training. Regarding the factors responsible for this, 75% reported fewer subspecialty examinations were being performed and as a result, 54% experienced competition to first-report the examinations being performed. In addition, 61% stated that they were spending less time in the radiology department than usual. When asked if they thought their training would need to be extended to account for this period of decreased exposure to radiology, 69% felt it was too early to say but potentially would consider extending their training, 31% did not feel their training length would be impacted.
Despite any potential reductions in radiology workload and experience during this time, trainees reported that many aspects of training had in fact improved during this time period. For example, there had been more time for project work and reading around subjects encountered and for personal study and background reading. There was also better access to online resources, increased structured teaching from consultants, and more time for feedback for studies reported.
On-call commitments
When questioned as to whether there was an increased on-call commitment within radiology during the pandemic, 18 of the 29 respondents answered “no”. There was no consistent response across the region regarding the systems in place for covering acute radiology on-calls arising due to registrar sickness and/or isolation or for covering vacant on-call slots created by redeployment.
Working from home
Thirty-one percent (9/29) of trainees were offered the option of working from home. Of these, five (56%) worked from home 1 day a week or less. Although a third of those trainees working from home had access to radiology information systems (RIS)/picture archiving and communication systems (PACS) at home, a third had not received departmental guidance regarding what sort of work could or should be done from home.
Working outside of radiology (redeployment)
Of the 29 survey respondents, seven (24%) trainees had been redeployed from radiology to clinical ward-based jobs. Of those, 43% (3/7) reported feeling “anxious” about being redeployed, one person (14%) had felt “underprepared” and three (43%) responded as being “happy to help when and where needed”. For those registrars who were unable to be redeployed when asked, the majority (8/10) had felt supported; however, two reported feeling unsupported. Eighty-six percent (6/7) of those trainees redeployed were offered either online or face-to-face medical refresher training or inductions prior to redeployment; however, 43% (3/7) reported that the training offered was not enough. When asked how much notice they were given of being redeployed, all respondents reported a notice period of 3 days or less. Redeployment was discussed with 71% (5/7) of these trainees by their department lead before they commenced work on the wards; however, 57% (4/7) were not asked at which grade they would feel confident to work at and 43% (3/7) had not been FIT tested for filtering face piece class 3 (FFP 3) masks prior to redeployment. In terms of the nature of redeployment, three (43%) trainees worked a full-time medical rota with on-call duties (including back-to-back long days and night shifts) and four (57%) performed in-hours ward cover on designated days.
On a scale of 1–5 (1: poorly supported, 5: very well supported), four of seven (57%) trainees rated the level of support offered on the wards positively as 4 or 5. One trainee reported feeling poorly supported on the wards, with a score of 2. Using the same scale, two of seven (29%) trainees rated the level of support offered by their radiology departments as 4 or 5, with two (29%) trainees giving a score of 2.
Overall, 71% (5/7) of trainees rated their redeployment experience as either better than expected or as expected, with two (29%) trainees rating the experience as worse than expected. Six (86%) of those redeployed were able to get annual leave requests approved during this period. Five (71%) reported doing no, or almost no, radiology work during the time that they were redeployed. Five (71%) reported that they had been “surplus to requirement” in their new roles.
Trainee well-being
When asked about how COVID-19 and its related effects had impacted on trainee well-being, 48% (14/29) reported experiencing a worsening in their overall well-being compared to before the pandemic, but 45% (13/29) reported no change in their well-being and 7% (2/29) reported feeling better during this time.
Most registrars (93%) were aware of who to contact if they needed to access well-being support; however, two respondents were unsure of how to access such help.
Discussion
The first wave of the COVID-19 pandemic led to a significant change in the structure of healthcare provision within the UK and around the world. To provide effective care for patients infected with the SARS-CoV-2 virus, and to protect those unaffected, initial guidance from the NHS2 was to suspend all elective activity and to perform urgent or emergency procedures only. Part of the extensive restructuring of hospital resources undertaken to combat the anticipated workload from COVID-19 included pooling doctors from all specialties into a new medical workforce and assigning them to novel rotas. As a result of the cessation of elective activities and a reduction in the number of hospital attendances for non-COVID-related diseases, the demand for radiology services decreased during this time.
The present study surveyed trainees from a radiology school to assess the impact of these changes on their training and well-being. To the authors' knowledge, this is the first survey assessing the impact of COVID-19 on radiology trainee experience and well-being during this pandemic in the UK.
There was significant variation among different hospitals in their response to COVID-19, and this was reflected in trainee responses to questions about training, rotas, redeployment, and the reporting of COVID-19 imaging across different hospitals. As such, each individual trainee's experience during this time will have been different and influenced by a number of factors, some of which have been identified by this survey. For example, the results of this survey confirmed that the demand on radiology services had significantly decreased throughout the region during the pandemic. The results showed that the number of radiographs, CT, and MRI examinations reported by registrars reduced during this time compared to before the pandemic and that there was also a reduction in subspecialty training time.
Within the region, it is traditionally the responsibility of the registrars and reporting radiographers where applicable to report the emergency department (ED) appendicular radiographs. During the pandemic, the process of taking the radiographs had become more labour intensive for the radiographers as most radiographs were being taken outside of the department with portable machines and with two radiographers. This meant that reporting radiographers no longer had time to report the ED radiographs. Despite this, the majority of registrars were reporting significantly lower volumes of plain films per week. This is due to the fact that fewer ED plain films were being taken because of reduced ED attendances. In addition, consultants and registrars were competing for any reporting, due to the decrease in overall departmental workload.
Other factors influencing trainee experience at this time included a reduction in one-on-one training time with consultants because of new consultant rotas, which included more time working from home as part of departmental strategies to protect the consultant workforce. There was also an impact from social distancing rules, particularly for those colleagues who were having to shield within or outside of the usual workplace. Such factors are likely to have contributed to the desire expressed by some trainees to extend the length of their training.
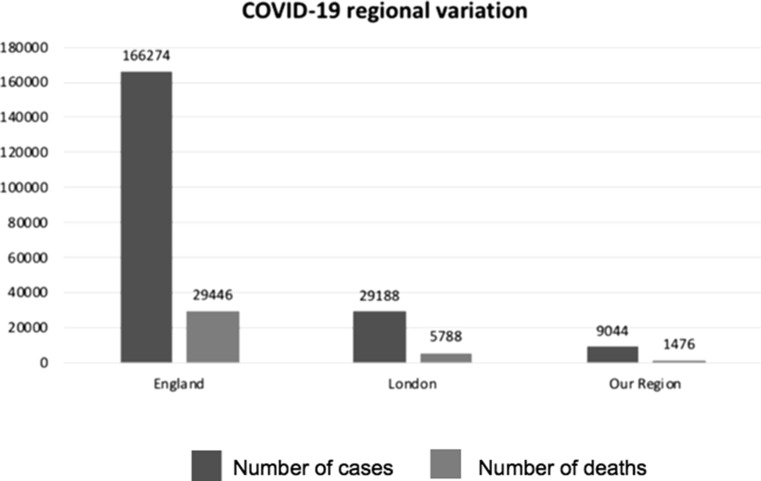
The prevalence of COVID-19 varied throughout the radiology school region, which was reflected in the numbers of registrars and consultants redeployed across the different sites. Overall, the prevalence of COVID-19 was low within the region when compared to the rest of the UK, and therefore, any interruptions in training may have been less than that experienced by the trainees in some other UK Deaneries.
Freeing up of resources in anticipation of a large workload generated by COVID-19 coupled with a reduction in numbers of acute and elective examinations, has meant that there has been more time during the working week to potentially be used for teaching within radiology departments. An initial obstacle in delivering teaching was doing so safely whilst maintaining social distancing rules of individuals being at least 2 m apart. Traditionally, teaching in radiology has been face-to-face “hot-seat” style teaching, which is difficult to achieve in groups whilst adhering to social distancing; however, departments quickly adapted and became familiar with various teleconferencing platforms as a way to hold virtual multidisciplinary team (MDT) meetings,6 with the added benefit of being able to be used for virtual teaching sessions. Teaching over teleconference platforms has negated problems with large group teaching whilst maintaining social distancing, and in fact, allows registrars and trainers from across the region to be involved. Unfortunately, online teaching sessions that took place during this time were not recorded for the benefit of those trainees that could not attend due to redeployment, but this was most likely due to an initial unfamiliarity of the virtual conferencing platforms. This is perhaps something that can be considered for the future. The increasing use of online learning resources driven by the pandemic has led to recent reports highlighting various ways in which radiology departments can adapt in not only maintaining social distancing but also trainee education.7 , 8 Going forward, this could be the new normal way of teaching, as it gives much flexibility for trainees and trainers alike. From the beginning of June 2020, the region is having weekly webinars with good attendance. Indeed, the Royal College of Radiologists were quick to respond to the pandemic and to embrace learning online. They made great efforts to mitigate against any potential loss of training brought about by the pandemic by releasing a series of online lectures and teaching resources.
The COVID-19 pandemic has led to major changes to the working patterns of the majority of healthcare, and departments have had to be responsive, adaptable, and innovative. The global pandemic alone has caused stress and anxiety across the world. For radiology, there have been many changes to workload and working patterns,6 which for some has meant returning to clinical medicine, with very little time for mental or physical preparation. Changes at work will undoubtedly have had an impact on wellbeing, and in some reported cases, those have been for the better.
All of the redeployed specialist trainees reported being given very little notice of redeployment and of their new rotas. As this was the case for all redeployed trainees across the board, it is likely to reflect the complexity of re-structuring and organising the entire medical and hospital workforce. Nevertheless, delays in communication clearly contributed to overall trainee anxieties relating to redeployment. Trainees also reported that improvements could have been made to the process of radiology departments volunteering their staff for redeployment. Some trainees would have welcomed an opportunity to first meet with the heads of department to explore the level of medicine that they would feel comfortable working at and to discuss personal circumstances, some of which may have prevented redeployment, prior to being added to a medical rota. Although this would have been ideal, the pace at which restructuring happened in response to the increasing numbers of COVID-19 cases, rendered it difficult to organise in a timely fashion. Despite the above, nearly 43% of the respondents felt that their redeployment experience was better than expected.
To mitigate against any impact on radiology training during this time, the Head of School directed trainees in the region to supplement learning with library cases from PACS, and the Deanery recommended the RCR's online learning resources. The Deanery also adapted the paperwork submitted by trainees ahead of their annual review of competency (ARCP) to include details of redeployment to identify those trainees, who may need additional support.
In the event of a second wave, several learning points can be drawn upon from the present survey with regards to planning and executing the redeployment of doctors from non-medical specialties to jobs in clinical medicine. The amount of time between information on re-deployment to being redeployed was just 3 days, and this may have been responsible for the perceived anxiety by the trainees. Information about redeployment should, therefore be communicated as early as possible in order for the trainees to prepare and plan for redeployment. Having that time to prepare would help significantly reduce any redeployment related anxiety. Further, induction could be streamlined and online education prior to redeployment might also help. Another suggestion would be to have a “buddy” system wherein the redeployed doctor would be attached to a ward-based doctor, whose familiarity with the processes and pathways of patient care would help the redeployed doctors immensely.
Colleagues who may have had to be sent home or out of the department for personal health reasons, should be actively involved including providing them access to PACS/CRIS from home, providing access to online teaching, and giving support with radiology project work. Most of all, they should be advised to maintain regular contact with their supervisors during this time so that they may agree a plan to ensure that any time lost to training has as minimal impact on their individual training as possible. Employing even some of these recommendations would likely lessen any negative impact on trainee well-being and may even improve their overall experience.
Departmental workload is expected to change in the coming months, but how this will manifest is still unknown. If the virus-related admissions remain low, there will be a significant demand on radiology services because of resumption of elective surgical activities as highlighted in a recent report9 and also from imaging significant backlogs of patients whose imaging was deferred during the pandemic. Another possibility is that of a second wave of COVID-19 with a further restriction in imaging and further redeployment. It is noteworthy that in some hospitals not only radiology trainees, but also consultant radiologists were redeployed.
The size of the trainee cohort is one of the limitations; however, this was a trainee-led survey and the aim was for the responses to be true and transparent and reflect the views of the trainees without being under any pressure. Hence, it was anonymised and voluntary, which potentially explains the response rate. The response rate to the survey, nonetheless, is considered adequate in any voluntary survey. Moreover, the results echoed the findings highlighted by a recent American report, which emphasised similar issues.10 Another limitation to consider is that there may be a respondent bias. Trainees from six of the seven hospitals responded to the survey, whereas no response was obtained from one hospital where trainees were not redeployed to medicine. It is, therefore likely that those redeployed are more likely to complete the survey.
Regional variations in COVID-19 burden across the regions within the UK and also across continents may make the results less generalisable. Fig. 6 shows the variation in the number of cases and deaths with COVID-19 until 5 May11 (when the survey started). The region did not suffer as much as London and the rest of England11; however, the results provide insight into radiology trainee perspectives during COVID-19 pandemic. It is important to highlight that plans for first wave of COVID-19 were made on the worst-case scenario basis rather than titrating to number of local cases; however, it is possible that a higher incidence of COVID-19 in other regions may have added to anxiety and could be explored in future regional/national surveys. It is recommended that similar trainee information be gathered, which would enable planning for regional variations and supporting trainees during these challenging times.
Figure 6.
Number of cases and deaths across England, London, and the region until 5 May 202011 (when questionnaire was sent to trainees).
In conclusion, COVID-19 has had a significant impact on training and trainee well-being, as highlighted by this survey of radiology trainees. During the first wave, there have been significant changes to departmental workflows, radiology workload, and the nature of daily work. The lessons learnt from the training scheme are presented within this report and should help with preparations in the event of a second wave or future pandemic.
Author contributions
Guarantor of integrity of the entire study: Sowmya Veerasuri.
Study concepts and design: Sowmya Veerasuri, Monique Vekeria, Sian Davies.
Literature research: Sowmya Veerasuri.
Clinical studies: N/A.
Experimental studies/data analysis: Sowmya Veerasuri, Monique Vekeria, Sian Davies, Richard Graham, Jonathan Rodrigues.
Statistical analysis: Sowmya Veerasuri, Jonathan Rodrigues.
Manuscript preparation: Sowmya Veerasuri, Monique Vekeria, Sian Davies.
Manuscript editing: Sowmya Veerasuri, Monique Vekeria, Sian Davies, Richard Graham, Jonathan Rodrigues.
Conflict of interests
The authors declare no conflict of interest.
Acknowledgements
The authors thank all the radiology trainees who responded to this survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.crad.2020.07.022.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organisation Coronavirus disease (COVID-19) situation report 135. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200603-covid-19-sitrep-135.pdf?sfvrsn=39972feb_2 Available at:
- 2.NHS England and NHS Improvement . 17 March 2020. Important and urgent — next steps on NHS response to COVID-19.https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf Available at: Accessed 2 May 2020. [Google Scholar]
- 3.NHS Health Research Authority Is my study research? http://www.hra-decisiontools.org.uk/research Available at:
- 4.British Society of Thoracic Imaging BSTI COVID-19 CXR report proforma. https://www.bsti.org.uk/media/resources/files/BSTI_COVID_CXR_Proforma_v.3-1.pdf Available at:
- 5.British Society of Thoracic Imaging BSTI CT reporting proforma: COVID-19 version 2. https://www.bsti.org.uk/media/resources/files/BSTI_COVID_CT_Proforma_v2_13.04.2020.pdf Available at:
- 6.Hudson B.J., Loughborough W.W., Oliver H.C. Lasting lessons learnt in the radiology department from the battle with COVID-19. Clin Radiol. 2020;S0009–9260(20):30214–30222. doi: 10.1016/j.crad.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chong A., Kagetsu N.J., Yen A. Radiology residency preparedness and response to the COVID-19 pandemic. Acad Radiol. 2020;27(6):856-861. doi: 10.1016/j.acra.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.England E., Kanfi A., Flink C. Radiology residency program management in the COVID era — strategy and reality. Acad Radiol. 2020;S1076–6332(20):30273–30277. doi: 10.1016/j.acra.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020 doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvin M.D., George E., Deng F. The impact of COVID-19 on radiology trainees. Radiology. 2020:201222. doi: 10.1148/radiol.2020201222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gov.UK. Coronavirus COVID-19) in the UK. https://coronavirus-staging.data.gov.uk Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.