Abstract
Coronavirus disease 2019 (COVID-19) rapidly spread worldwide in the first quarter of 2020 and resulted in a global crisis. Investigation of the potential association of the spread of the COVID-19 infection with climate or ambient air pollution could lead to the development of preventive strategies for disease control. To examine this association, we conducted a longitudinal cohort study of 28 geographical areas of Japan with documented outbreaks of COVID-19. We analyzed data obtained from March 13 to April 6, 2020, before the Japanese government declared a state of emergency. The results revealed that the epidemic growth of COVID-19 was significantly associated with increase in daily temperature or sunshine hours. This suggests that an increase in person-to-person contact due to increased outing activities on a warm and/or sunny day might promote the transmission of COVID-19. Our results also suggested that short-term exposure to suspended particles might influence respiratory infections caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Further research by well-designed or well-controlled study models is required to ascertain this effect. Our findings suggest that weather has an indirect role in the transmission of COVID-19 and that daily adequate preventive behavior decreases the transmission.
Keywords: COVID-19, Epidemic growth, Particulate matter, Sunshine, Temperature
Graphical abstract
Highlights
-
•
Association between COVID-19 infection and climate or air pollution was examined.
-
•
Epidemic growth of COVID-19 was associated with increased temperature or sunshine hours.
-
•
Increase of contact among persons on a warm or sunny day may promote infection.
-
•
Short-term exposure to suspended particles may influence the respiratory infection.
-
•
Correct knowledge and adequate preventive behavior decrease its transmission.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a new pandemic infectious disease. It was first identified in December 2019 in a cluster of viral pneumonia cases linked to a wet market in Wuhan, the capital of Hubei Province, China (Zhu et al., 2020a). COVID-19 had rapidly spread from Wuhan to many other countries in the world through global travel by March 2020 (Chen et al., 2020; Lu et al., 2020; Phan et al., 2020; Xu et al., 2020a). The World Health Organization (WHO) declared COVID-19 as a global pandemic on March 11, 2020 (WHO, 2020a).
SARS-CoV-2 is mainly transmitted human-to-human through close contact, respiratory droplets, fomites, and contaminated surfaces. Its transmission is similar to that of other respiratory viruses such as influenza or human coronavirus (Cheng et al., 2020; Lai et al., 2020; Sungnak et al., 2020; WHO, 2020b). Airborne transmission may occur via airborne particles smaller than 5 μm in diameter. Some outbreak reports related to indoor crowded spaces have suggested the possibility of airborne transmission, combined with droplet transmission such as during choir practice, in restaurants, or in fitness classes (Wiersinga et al., 2020; WHO, 2020b). A recent experimental study using transgenic mice expressing human angiotensin-converting enzyme 2 (hACE2) indicated that SARS-CoV-2 can be experimentally transmitted among hACE2 mice by close contact, through respiratory droplets, but is hardly transmitted through exposure to the airborne particles (Bao et al., 2020). A recent study also indicated that the role of airborne particles as a carrier for the virus diffusion is not evident (Bontempi, 2020a).
Many similar infectious diseases displayed seasonal patterns in their incidence (Fares, 2013; Fisman, 2017; Pascual and Dobson, 2005). Infections with severe acute respiratory syndrome coronavirus (SARS-CoV), influenza virus, human rhinovirus, and respiratory syncytial virus were directly associated to ambient air temperature and humidity (Barreca et al., 2012; Casanova et al., 2010; Chan et al., 2011; Ikäheimo et al., 2016; Jaakkola et al., 2014; Paynter, 2015; Tan et al., 2005). The association of respiratory viral infection with ambient air pollution has also been reported (Ciencewicki and Jaspers, 2007; Croft et al., 2019). Therefore, environmental factors such as climate and ambient air pollution may play an important role in the progression and spread of the disease.
Many studies have shown the influence of environmental factors including temperature, humidity, and/or ambient air pollution on the spread of COVID-19. Most studies reported a positive association of the spread with air pollution (Fattorini and Regoli, 2020; Li et al., 2020a; Xu et al., 2020b; Zhu et al., 2020b). Studies suggested an optimum range of 5°C–15 °C in temperature for its transmission (Gunthe et al., 2020; Sajadi et al., 2020). However, the association with climate conditions has not been consistent and is controversial. A positive association with an increase in ambient air temperature has been suggested (Bashir et al., 2020; Li et al., 2020a; Menebo, 2020; Tosepu et al., 2020; Xie and Zhu, 2020). Conversely, several studies suggest a negative association (Liu et al., 2020a; Méndez-Arriaga, 2020; Prata et al., 2020; Qi et al., 2020; Ujiie et al., 2020; Wu et al., 2020). Some studies have shown an association with an increase in humidity (Baker et al., 2020), whereas others have suggested an association with lower air humidity (Ahmadi et al., 2020; Liu et al., 2020a; Wu et al., 2020). Furthermore, some studies showed no association with temperature (Jüni et al., 2020; Yao et al., 2020) or humidity (Gunthe et al., 2020; Tosepu et al., 2020).
Climatic conditions and ambient air pollution vary across the world. Thus, the influence of environmental factors on the spread of the disease needs to be studied in each country. In addition, studies postulating that the date of infection (i.e., exposure to SARS-CoV-2) corresponded to the observation date of environmental factors are scarce. An average time interval between transmission and reporting of confirmed COVID-19 cases was suggested to be 14 days (Dong et al., 2020; Jüni et al., 2020; Lauer et al., 2020). Thus, Jüni et al. analyzed the epidemic growth of the disease concerning the stipulated incubation period (14 days) with reference to the environmental factors to ascertain the strength of the association (Jüni et al., 2020). However, further matching between the date of infection and the observation date of the environmental factors is important to examine the associations. The objective of this study was to evaluate the effect of climate and/or air pollution on the spread of COVID-19. Our study sought to estimate the date of infection and to determine the influence of environmental factors on spread of the disease.
2. Methods
2.1. Study design and areas
A longitudinal cohort study involving different geographical areas of Japan with documented outbreaks of COVID-19 was designed to determine the association between the epidemic growth and the environmental factors within the same epidemic period. The number of cases dramatically increased from mid-March in Japan. This prompted the Japanese government to release the first emergency declaration in seven main epidemic areas (Saitama, Chiba, Tokyo, Kanagawa, Osaka, Hyogo, and Fukuoka) on April 7, 2020. Then, the second emergency declaration was imposed nationwide on April 16 (Fig. S1). Japanese government asked people to avoid unnecessary outings, avoid crowded areas, practice social distancing, wear masks, and change their behavior (Tashiro and Shaw, 2020). Conscious behavioral changes were strongly observed after those declarations, and the number of COVID-19 cases decreased consequently (Fig. S1). The trend of the number of cases after the emergency declaration does not indicate the epidemic growth of the disease. In addition, if the data after emergency declaration is included in our analysis, the results could include bias that was influenced by the change of people's behavior due to the intervention by the government. Thus, to examine the association of the epidemic growth with the environmental factors, we determined the analysis period from March 13 to April 6, 2020 before the emergency declaration. Weather and air pollution levels are changed in a short term. The number of confirmed cases has been daily reported. However, the differences of operating speed in testing practices of COVID-19 infection affect count of the number of confirmed cases in a day. The time window of five days is short enough that no substantial changes in testing strategy are expected so that the confirmed cases in each region represent a constant level of the true actual cases (Jüni et al., 2020). Thus, we divided the analysis period into five periods (with 5-day slots): March 13–17, March 18–22, March 23–27, March 28–April 1, and April 2–6. This was done to evaluate the association in a longitudinal manner.
2.2. Data collection
2.2.1. Case of COVID-19
We collected data during the COVID-19 outbreak in Japan (May 22, 2020), as a comma-separated values file from the online dashboard provided by the J.A.G JAPAN Corporation (J.A.G JAPAN, 2020). The J.A.G JAPAN Corporation has collected data on a daily basis and provided these data as the license of NonCommercial 4.0 International (CC BY-NC 4.0). These data include necessary information about all COVID-19 cases reported by the Ministry of Health, Labour and Welfare (MHLW) and the local governments of Japan. All this information has been submitted together with sex, age groups, identified date [when COVID-19 was identified as positive by the SARS-CoV-2 reverse transcription polymerase chain reaction (RT-PCR) test], and the date of onset of symptoms. In addition, residential area, occupation, history of traveling abroad, data sources from the MHLW and local governments, and so forth have been also recorded. The COVID-19 cases infected in Japan were included in this study. The COVID-19 cases in the Diamond Princess cruise ship docked at Yokohama were excluded. The incubation period for COVID-19 was reported at approximately 5 days from virus exposure to symptoms onset (Guan et al., 2020; Lauer et al., 2020; Li et al., 2020b). Thus, cases returning from foreign country that entered to Japan within 5 days before onset of the disease, cases identified as positive by the RT-PCR test at the airport quarantine depot, and cases living in a foreign country were excluded from our study.
We identified the date of onset of the symptoms in each case from collected data. The median of the time interval between the date of onset and the date identified as positive by the RT-PCT test was 6 days from January to April 12. The mean value was approximately 6.5 days. Thus, in the absence of a date of onset of symptoms, we estimated the date of onset by subtracting 6 days from the date identified as a positive. Furthermore, we estimated the date of infection from the date of onset. As described above, the incubation period for COVID-19 was approximately 5 days. Thus, we deduced the date of infection by subtracting 5 days from the date of onset.
We counted the number of cases daily from their date of infection in terms of municipality, including Tokyo. We included all areas with at least cumulative 50 cases in this study since the beginning of the epidemic (set on January 15, 2020; Fig. S1) as of April 7, 2020. Areas affected by large localized cluster occurrence were excluded from the study.
2.2.2. Demographics
We obtained demographic data from the surveyed areas. This includes population, percentage of inhabitants aged ≥65 years, total land surface area (km2), inhabitable area (km2), taxable income, tax debtor, life expectancy at birth (MIAC, 2019), and health expenditure (Cabinet Office, 2020). We calculated the urban density (using population and inhabitable area) and taxable income per person (using taxable income and tax debtor).
2.2.3. Environmental data
The daily meteorological data were obtained from Japan Meteorological Agency (JMA, 2020). This includes mean, minimum, and maximum ambient air temperature; precipitation; sunshine hours; wind speed; vapor pressure; relative humidity; and minimum relative humidity. The mean absolute humidity was calculated by vapor pressure and saturated water vapor pressure at its corresponding temperature. If the vapor pressure was not available, the absolute humidity was determined from relative humidity and its corresponding temperature (Shaman and Kohn, 2009).
Data of hourly ambient air pollutants were collected from the Atmospheric Environmental Regional Observation System (AEROS) provided by the Ministry of the Environment (MOE, 2020). These pollutants include nitrogen monoxide (NO), nitrogen dioxide (NO2), photochemical oxidant (Ox), suspended particle matter (SPM), and fine particulate matter (PM2.5). The daily mean data for each pollutant were calculated based on the hourly data. In the absence of these data from the Japan Meteorological Agency, data were obtained from the AEROS stations. The 5-day mean data during March 13–17, March 18–22, March 23–27, March 28–April 1, and April 2–6 were used for statistical analyses.
2.3. Index for the epidemic growth
Rate ratios (RR) were calculated as the cumulative count of confirmed cases in an area since the beginning of the epidemic as of March 13, March 18, March 23, March 28, and April 2 divided by the cumulative count of confirmed cases since the beginning of the epidemic as of March 17, March 22, March 27, April 1, and April 6, respectively. The observational period was 5 days across all areas. A rate ratio of two indicates that the number of cases doubled within 5 days.
2.4. Statistical analyses
We used weighted random-effects regression analysis with accommodation of correlated longitudinal data to determine the association between the logarithm of the rate ratio of COVID-19 and the exposure variables (Jüni et al., 2020), including regional climate and air pollution. Associations were expressed as ratios of rate ratios (RRRs) per 1 °C increase in temperature; 1 mm increase in precipitation; 1 h increase in sunshine hours; 1 m/s increase in mean wind speed; 5% increase in relative humidity; 1 g/kg (dry air) increase in absolute humidity; 1 ppm increase in NO, NO2, and Ox; and 1 μg/m3 increase in SPM and PM2.5. The sites of analyses were geographical areas with five longitudinal periods. The logarithm of the RR of COVID-19 (dependent variable) and exposure variables (independent variables) were well defined at the level of geographical areas with five longitudinal periods. RRR values one of >1 indicate that an increase in a continuous exposure variable is associated with an increase in the epidemic growth.
We determined the association of epidemic growth with exposure variables using univariate and multivariable analyses for 28 geographical areas, divided to five periods from March 13 to April 6, 2020 with a longitudinal manner. In the multivariable analyses, we examined the association of epidemic growth with exposure variables on the regional climate or air pollutants, adjusting for male inhabitants, inhabitants aged ≥65 years, urban density, taxable income, health expenditure, and life expectancy at birth as the possible specified covariates. After correlations (using Pearson's test) among exposure variables were examined, further multivariable models were examined to determine the robustness of the associations with exposure variables. We used p < 0.05 to indicate statistical significance. All data analyses were performed using SPSS statistical software, version 26 (IBM Corp, Armonk, NY, USA).
3. Results
3.1. Characteristics of surveyed areas
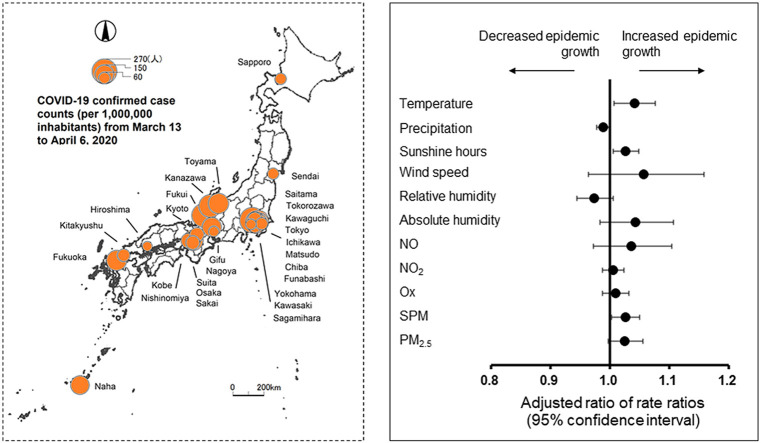
We included 28 geographical areas and enrolled 6529 cases in our analyses after reviewing the inclusion and exclusion criteria (Fig. 1 ). These areas were urban in nature, with a population of >200,000 (Table S1). The baseline characteristics of the surveyed areas are displayed in Table 1 . The median case count per 1 million inhabitants for the 28 geographical areas during entire study period was 132.5 [interquartile rage (IQR) 67.3–171.1]. The median RR representing epidemic growth was 1.63 (IQR, 1.18–2.06) during March 13–17, 1.97 (IQR, 1.54–3.00) during March 18–22, 1.83 (IQR, 1.62–2.34) during March 23–27, 1.61 (IQR, 1.31–1.78) during March 28–April 1, and 1.32 (IQR, 1.24–1.41) during April 2–6, respectively. The highest RR value was observed during March 18–22, followed by March 23–27. The median percentage of the inhabitants aged ≥65 years was 24.0% (IQR 22.9–25.9) and the median life expectancy at birth (i.e., lifetime) was 84 years (IQR, 84.1–84.6). Those indicate a high rate of elderly people in Japan.
Fig. 1.
Geographic patterns of COVID-19 confirmed case counts (per 1,000,000 inhabitants) in 28 geographical areas of Japan from March 13 to April 6, 2020.
Table 1.
Status of epidemic growth during COVID-19 outbreak and demographic characteristics in analyzed geographical areas (n = 28).
| Variable | Median | IQR |
|---|---|---|
| No. of cases | ||
| March 13–17 | 4 | 1–7 |
| March 18–22 | 9 | 7–20 |
| March 23–27 | 20 | 13–32 |
| March 28–April 1 | 23 | 15–35 |
| April 2–6 | 26 | 17–36 |
| Entire period | 80 | 61–120 |
| Case count (per 1,000,000 inhabitants) | ||
| March 13–17 | 7.58 | 1.00–8.35 |
| March 18–22 | 17.54 | 9.59–17.96 |
| March 23–27 | 29.63 | 18.17–39.98 |
| March 28–April 1 | 41.85 | 18.25–54.05 |
| April 2–6 | 35.94 | 20.28–43.36 |
| Entire period | 132.54 | 67.33–171.07 |
| Rate ratio | ||
| March 13–17 | 1.63 | 1.18–2.06 |
| March 18–22 | 1.97 | 1.54–3.00 |
| March 23–27 | 1.83 | 1.62–2.34 |
| March 28–April 1 | 1.61 | 1.31–1.78 |
| April 2–6 | 1.32 | 1.24–1.41 |
| Population (1,000,000 inhabitants) | 0.90 | 0.48–1.49 |
| Male inhabitant (%) | 48.6 | 47.9–49.7 |
| Inhabitants aged ≥65 years (%) | 24.0 | 22.9–25.9 |
| Urban density (1000 inhabitants/km2) | 6.3 | 4.4–8.2 |
| Taxable income (1,000,000 JPY/inhabitant) | 3.5 | 3.4–3.8 |
| Health expenditure (1,000,000 JPY/inhabitant) | 0.19 | 0.18–0.20 |
| Life expectancy at birth (year) | 84.3 | 84.1–84.6 |
Abbreviations: IQR, interquartile rage; JPY, Japanese Yen.
The environmental exposure data are shown in Table 2 . In the entire surveyed period, the median values of mean temperature and mean daily maximum temperature were 11.6 °C (IQR, 9.3–12.8) and 16.0 °C (IQR, 13.4–17.9), respectively, indicating typical early spring in Japan. The median values of precipitation and sunshine hours were 2.2 mm (IQR, 0.0–6.1) and 7.1 h (IQR, 5.6–8.2), respectively, indicating moderately containing a fine day. The median values of mean NO, NO2, Ox, SPM, and PM2.5 were 1.7 ppb (IQR, 1.1–2.6), 12.2 ppb (IQR, 8.4–14.8), 34.6 ppb (IQR, 31.8–38.7), 11.4 μg/m3 (IQR, 9.3–14.1), 9.5 μg/m3 (IQR, 7.2–11.2), respectively. The maximum values of mean daily maximum NO, NO2, Ox, SPM, and PM2.5 were 7.8 ppb (converted to 9.6 μg/m3), 28.0 ppb (converted to 52.6 μg/m3), 51.5 ppb (converted to 103.0 μg/m3), 22.9 μg/m3, and 19.9 μg/m3. The ambient environmental quality standards within short time exposure to NO2, Ox, SPM, and PM2.5 in Japan were 40–60 ppb for 24 h, 60 ppb for 1 h, 200 μg/m3 for 1 h, and 35 μg/m3 for 24 h, respectively (Kawamoto et al., 2011). SPM is defined as airborne particles with a diameter ≤10 μm. SPM is particulates collected through an instrument which completely (100%) excludes particulate matter with aerodynamic diameter > 10 μm. PM10 is defined as airborne particles that pass through a size regulator inlet with a 50% efficiency cut off at 10 μm aerodynamic diameter. If the nomenclature of PM is used, SPM would be called PM7 (Wakamatsu, 2011). The main Ox component in photochemical air pollution is ozone (O3; up to 90%) (Stokinger and Coffin, 1968). Ambient ozone is a marker for hazardous Ox types in air (WHO, 2006). The WHO air quality guidelines of shot time exposure for NO2, O3, PM10, and PM2.5 were 200 μg/m3 for 1 h, 100 μg/m3 for 8 h, 50 μg/m3 for 24 h, 25 μg/m3 for 24 h (WHO, 2006). Overall, the results of air pollutants had not exceeded the ambient environmental quality standards and the WHO air quality guidelines overall.
Table 2.
Ambient environmental exposure levels in analyzed geographical areas (n = 28).
| Variable | March 13–17 | March 18–22 | March 23–27 | March 28–April 1 | April 2–6 |
|---|---|---|---|---|---|
| Mean temperature (°C) | 8.1 (6.8–8.8) | 13.6 (12.6–14.6) | 11.6 (10.6–12.5) | 10.3 (9.5–12.0) | 12.0 (11.4–13.0) |
| Mean daily minimum temperature (°C) | 3.4 (1.9–4.5) | 7.6 (5.7–9.3) | 6.8 (4.6–8.2) | 6.3 (5.6–9.2) | 7.0 (5.8–8.2) |
| Mean daily maximum temperature (°C) | 13.1 (11.8–13.9) | 19.3 (17.9–20.3) | 16.4 (15.6–17.6) | 13.9 (13.0–15.7) | 17.3 (16.1–18.1) |
| Precipitation (mm) | 3.4 (2.2–5.2) | 0.2 (0.0–1.0) | 2.0 (0.0–4.3) | 11.0 (9.0–16.2) | 0.0 (0.0–0.4) |
| Sunshine hours (h) | 6.4 (5.8–7.1) | 8.3 (7.6–9.4) | 7.5 (7.0–7.9) | 1.0 (0.4–2.3) | 9.2 (7.2–9.6) |
| Mean wind speed (m/s) | 3.0 (2.2–3.6) | 3.0 (2.3–3.9) | 3.0 (2.1–3.5) | 2.8 (2.1–3.7) | 3.4 (2.5–3.9) |
| Mean relative humidity (%) | 62.2 (58.3–64.2) | 55.4 (51.6–60.2) | 54.7 (50.7–60.5) | 79.2 (75.3–83.4) | 54.0 (50.8–57.9) |
| Mean daily minimum relative humidity (%) | 38.0 (35.2–42.7) | 33.1 (28.9–39.4) | 33.0 (28.8–38.4) | 65.9 (59.5–69.0) | 31.3 (29.2–35.0) |
| Mean absolute humidity (g/kg, DA) | 4.1 (3.9–4.3) | 5.3 (5.0–5.5) | 4.7 (4.3–5.3) | 6.4 (6.1–6.8) | 4.6 (4.3–4.9) |
| NO (ppb) | 2.1 (1.4–2.6) | 2.0 (1.1–3.0) | 2.8 (1.9–3.5) | 1.3 (1.0–1.7) | 1.3 (0.8–1.7) |
| NO2 (ppb) | 12.9 (8.7–14.3) | 14.3 (9.1–18.6) | 14.4 (12.9–17.4) | 10.2 (8.0–12.8) | 9.7 (7.2–11.0) |
| Ox (ppb) | 32.5 (30.1–34.6) | 36.9 (34.2–40.0) | 34.1 (32.8–35.5) | 30.7 (25.9–33.0) | 40.7 (38.5–42.2) |
| SPM (μg/m3) | 9.6 (8.9–10.7) | 15.2 (13.6–16.8) | 12.5 (11.2–15.6) | 10.1 (7.2–12.4) | 11.1 (9.7–12.5) |
| PM2.5 (μg/m3) | 7.8 (6.5–9.6) | 11.7 (10.5–13.9) | 10.6 (8.2–12.9) | 6.9 (6.0–7.9) | 9.8 (8.3–11.2) |
Values are expressed as median (interquartile rage). Abbreviations: DA, dry air; Ox, photochemical oxidant; NO, nitrogen monoxide; NO2, nitrogen dioxide; PM2.5, fine particulate matter; SPM, suspended particulate matter.
3.2. Exposure variables
Univariate analyses of variables showed significant positive association between the epidemic growth and sunshine hours and mean wind speed. In addition, there was a significant negative association with NO2 (Table 3 ). No significant association was found with mean temperature, mean daily minimum temperature, mean daily maximum temperature, precipitation, mean relative humidity, mean daily minimum relative humidity, and air pollutants (NO, Ox, SPM, or PM2.5). Fig. S2 shows bubble plots of the RR of COVID-19 on these variables. However, after adjusting for demographic variables with multivariable regression analyses, the associations became insignificant except for the association with the sunshine hours. Conversely, the associations with overall mean temperature [RRR, 1.04; 95% confidence interval (CI), 1.01–1.08], mean daily minimum temperature (RRR, 1.03; 95% CI, 1.00–1.06), mean daily maximum temperature (RRR, 1.04; 95% CI, 1.01–1.08), and SPM (RRR, 1.03; 95% CI, 1.00–1.05) became positively significant (Table 3).
Table 3.
Correlation between epidemic growth of COVID-19 and ambient environmental factors.
| Variable | Ratio unit | Univariate |
Multivariable |
||
|---|---|---|---|---|---|
| RRR (95% CI) | p value | Adjusted RRR (95% CI) | p value | ||
| Mean temperature | 1 °C | 1.03 (1.00–1.06) | 0.056 | 1.04 (1.01–1.08) | 0.018* |
| Mean daily minimum temperature | 1 °C | 1.02 (1.00–1.04) | 0.053 | 1.03 (1.00–1.06) | 0.037* |
| Mean daily maximum temperature | 1 °C | 1.04 (1.00–1.08) | 0.060 | 1.04 (1.01–1.08) | 0.020* |
| Precipitation | 1 mm | 0.99 (0.98–1.00) | 0.091 | 0.99 (0.98–1.00) | 0.060 |
| Sunshine hours | 1 h | 1.03 (1.00–1.05) | 0.035* | 1.03 (1.01–1.05) | 0.011* |
| Mean wind speed | 1 m/s | 1.13 (1.04–1.23) | 0.005** | 1.06 (0.96–1.16) | 0.238 |
| Mean relative humidity | 5% | 0.98 (0.95–1.02) | 0.344 | 0.97 (0.94–1.01) | 0.105 |
| Mean daily minimum relative humidity | 5% | 0.98 (0.95–1.01) | 0.220 | 0.98 (0.96–1.00) | 0.058 |
| Mean absolute humidity | 1 g/kg, DA | 1.03 (0.98–1.09) | 0.259 | 1.04 (0.98–1.11) | 0.159 |
| NO | 1 ppb | 0.96 (0.90–1.02) | 0.200 | 1.04 (0.97–1.10) | 0.278 |
| NO2 | 1 ppb | 0.98 (0.97–1.00) | 0.033* | 1.01 (0.99–1.02) | 0.540 |
| Ox | 1 ppb | 1.02 (1.00–1.04) | 0.082 | 1.01 (0.99–1.03) | 0.402 |
| SPM | 1 μg/m3 | 1.01 (0.98–1.05) | 0.356 | 1.03 (1.00–1.05) | 0.026* |
| PM2.5 | 1 μg/m3 | 1.01 (0.98–1.04) | 0.698 | 1.03 (1.00–1.06) | 0.083 |
Values are expressed as ratios of rate ratios (95% CIs) and 2-sided p values. Significant at * p < 0.05, ** p < 0.01. Multivariable analysis is adjusted for male inhabitant, inhabitants aged ≥65 years, urban density, taxable income, health expenditure, and life expectancy at birth; Abbreviations: DA, dry air; CI, confidence interval; RRR, ratio of rate ratio; NO, nitrogen monoxide; NO2, nitrogen dioxide; Ox, photochemical oxidant; SPM, suspended particulate matter; PM2.5, fine particulate matter.
NO2 is a product of combustion processes such as vehicle exhaust and is found in the atmosphere generally in close association with other primary pollutants, including suspended particles. It is a precursor of ozone, and it coexists alongside other photochemical oxidants (WHO, 2006). Correlations among exposure variables showed that NO2 was highly correlated with Ox (r = −0.449, p < 0.001), SPM (r = −0.497, p < 0.001), and PM2.5 (r = −0.532, p < 0.001; Table S2). In the presence of sunlight, emissions of volatile organic compounds and nitrogen oxide (NOx) lead to the production of high concentrations of secondary particulate matter (Jiang et al., 2016; Kroll and Seinfeld, 2008). The correlation between mean temperature and sunshine hours was very low (r = 0.108, p = 0.253; Table S1). Based on these findings, we further examined to determine the strength of the associations with individual exposure variables (Table 4 ). For Model 1, we used mean temperature and sunshine hours, while adjusting for demographic variables. In addition, we used mean temperature and NO2 (Model 2) and mean temperature and SPM (Model 3), while adjusting for demographic variables. Model 1 showed a significant positive association with mean temperature (RRR, 1.05; 95% CI, 1.01–1.08) and sunshine hours (RRR, 1.02; 95% CI, 1.00–1.04). Model 2 (RRR, 1.04; 95% CI, 1.01–1.08) and Model 3 (RRR, 1.03; 95% CI, 1.00–1.07) showed a significant positive association with mean temperature. No association was found with NO2 and SPM in Model 2 and Model 3.
Table 4.
Multivariable regression models on the association with epidemic growth of COVID-19.
| Variable | Ratio unit | Model 1 |
Model 2 |
Model 3 |
|||
|---|---|---|---|---|---|---|---|
| Adjusted RRR (95% CI) | p value | Adjusted RRR (95% CI) | p value | Adjusted RRR (95% CI) | p value | ||
| Male inhabitant | 1% | 1.05 (0.92–1.20) | 0.473 | 1.02 (0.95–1.10) | 0.587 | 1.03 (0.95–1.10) | 0.485 |
| Inhabitants aged ≥65 years | 1% | 1.00 (0.95–1.06) | 0.949 | 0.98 (0.93–1.02) | 0.350 | 0.98 (0.94–1.02) | 0.403 |
| Urban density | 1000 inhabitants/km2 | 0.95 (0.91–1.00) | 0.038* | 0.93 (0.90–0.97) | <0.001** | 0.93 (0.90–0.97) | <0.001** |
| Taxable income | 1,000,000 JPY/inhabitant | 0.85 (0.52–1.38) | 0.512 | 0.90 (0.64–1.28) | 0.556 | 0.94 (0.66–1.33) | 0.719 |
| Health expenditure | 1000 JPY/inhabitant | 1.00 (0.99–1.01) | 0.686 | 1.00 (1.00–1.01) | 0.756 | 1.00 (1.00–1.01) | 0.681 |
| Life expectancy at birth | 1 year | 1.10 (0.87–1.40) | 0.426 | 1.02 (0.83–1.26) | 0.850 | 1.00 (0.81–1.24) | 0.989 |
| Mean temperature | 1 °C | 1.05 (1.01–1.08) | 0.013* | 1.04 (1.01–1.08) | 0.018* | 1.03 (1.00–1.07) | 0.048* |
| Sunshine hours | 1 h | 1.02 (1.00–1.04) | 0.039* | – | – | – | – |
| NO2 | 1 ppb | – | – | 1.01 (0.99–1.02) | 0.468 | – | – |
| SPM | 1 μg/m3 | – | – | – | – | 1.02 (0.99–1.04) | 0.144 |
Values are expressed as ratios of rate ratios (95% CIs) and 2-sided p values. Significant at * p < 0.05, ** p < 0.01. Abbreviations: JPY, Japanese Yen; CI, confidence interval; RRR, ratio of rate ratio; NO2, nitrogen dioxide; SPM, suspended particulate matter.
4. Discussion
In this longitudinal cohort study of 28 geographical areas with 6529 confirmed COVID-19 cases, the epidemic growth of COVID-19 during the follow-up period from March 13 to April 6, 2020, indicating typical early spring in Japan, was not significantly associated with precipitation, wind speed, relative humidity, absolute humidity, NO, NO2, Ox, and PM2.5. However, we found significant associations with mean temperature, mean daily minimum temperature, and mean daily maximum temperature. We also found a significant association with sunshine hours.
One assumption for these results is elucidated by the relationship between climatic conditions and human activities or behaviors. A study in Tokyo reported that the use of parks positively increased in an ambient temperature of 7°C–27 °C. This was due to increased exercise, playing, getting fresh air, or associations within the community (Thorsson et al., 2007). A Swedish study showed that the total attendance in the park increased especially during warm weather (−3.6 °C–20.1 °C). The participants also assessed the current weather conditions as being good for outdoor activity with clear skies, high air temperatures, and low wind speeds (Eliasson et al., 2007). A Canadian study conducted from November 2007 to May 2008 also showed that a 5 °C increase in ambient temperature was associated with a 14% increase in pedestrians. A shift from snowy to dry conditions was associated with a 23% increase in pedestrians, and a 5% increase in a sunlit area was associated with a 2% increase in pedestrians (de Montigny et al., 2012). The COVID-19 virus is primarily transmitted among people through respiratory droplets and contact routes (Burke et al., 2020; Chan et al., 2020; Huang et al., 2020; Li et al., 2020b; Liu et al., 2020b). High rates of secondary infection have been reported among household members and those in close contact with COVID-19 cases during travel (who are likely to get within 1–2 m) (Bi et al., 2020; Li et al., 2020c). The WHO has adapted a 1-m social distancing policy, based primarily on the assumption that SARS-CoV-2 is transmitted in large isolated droplets within this range (WHO, 2020b). A recent experimental study indicated that ultraviolet light from the sunlight inactivated SARS-CoV-2 (Bianco et al., 2020). However, our results suggest that an increased person-to-person contact due to increased outing activities on warm and/or sunny days will promote the transmission of the virus.
Our study revealed a significant association of the epidemic growth of COVID-19 with SPM in the multivariable analysis, after adjusting for demographic variables. This association disappeared after the mean temperature was entered in the model (Model 3). However, ambient air concentration of SPM was highly correlated with mean temperature (r = 0.419, p < 0.001). Thus, there is an underlying association of the epidemic growth of COVID-19 with SPM.
Coarse particles represented by SPM and PM10 include those inhalable particles having a high probability of deposition in the nasopharyngeal region of the human respiratory tract. The fine fraction of PM10 is cut off from the coarse fraction at 2.5 μm in an aerodynamic diameter (called PM2.5) and has a high probability of deposition in the tracheobronchial and alveolar regions of the human respiratory tract (Oberdörster et al., 2005; USEPA, 2019). Epidemiological findings showed a relationship between short-term exposure to coarse particles and respiratory infection (USEPA, 2019). The SARS-CoV-2 infection primarily targets the respiratory tract. Angiotensin-converting enzyme 2 (ACE2) is the cellular receptor for SARS-CoV-2. This virus engages the ACE2 as the entry receptor. The spike glycoprotein of the virus mediates viral entry via binding with the human ACE2 (Hoffmann et al., 2020; Yan et al., 2020). Recent COVID-19 study reports that ACE2 expression is highest in the nose and that it decreases following a gradient along the lower respiratory tract, from proximal (high) to distal (low) pulmonary epithelial cultures (Hou et al., 2020). The findings highlight the susceptibility of the nasal pathways to SARS-CoV-2 with subsequent aspiration-mediated virus seeding to the lung in its pathogenesis. Several studies indicate that chronic exposure to air pollutants delays/complicates the recovery of COVID-19 cases and leads to more severe and lethal forms of the disease. However, studies on the role of respiratory viruses in the pathogenesis of respiratory infections are still scarce (Domingo and Rovira, 2020; Domingo et al., 2020). Our results suggest that suspended particles may influence a respiratory infection by SARS-CoV-2. Ambient air concentrations of SPM were low in our study. Although one Chinese study suggested positive associations of short-term exposure to PM2.5, PM10, carbon monoxide, NO2, and O3 with COVID-19 confirmed cases (Zhu et al., 2020b), further research is recommended for verification, especially in areas having higher air concentration of coarse particles or by a well-controlled animal study or an in vitro study.
For evaluating the effects of climate and/or air pollution on the spread of COVID-19 infection (i.e., epidemic growth), we analyzed those data before emergency declaration that would not be influenced by the change of people's behavior due to the intervention by government. This is a strength of our study. However, our study had some limitations. First, we estimated the date of infection from the date of onset and the reported mean incubation period of COVID-19. When the date of onset was not available, we estimated the date of onset from the date when COVID-19 was identified as positive by the RT-PCR test. Thus, actual dates of infection could not be estimated. However, the identified or reported cases (not estimated dates of infection) and their approximate concordant measurement time points have often been used in a nationwide or global epidemiological study on the associations of the COVID-19 infection with the climate or air pollutants. Our study on the basis of the estimated date of infection could strength the evidence of the associations. Second, we analyzed only 28 geographical areas with 6529 cases on the municipality basis. This sample size of the surveyed area was not large enough. However, we used a longitudinal study design to examine possible effects of exposure variables on the epidemic trend of the disease. Longitudinal study designs are relatively stronger than cross-sectional ones. Third, data on climate and ambient air pollutants were collected for urban areas of each geographical area, which may not have accurately represented area's climatic patterns. Fourth, although we used data before the emergency declaration in the seven main infected areas, our results may have had a possible influence of behavioral patterns before the declaration. The postponement of the 2020 Tokyo Olympic and Paralympic Games was released on March 24, 2020 (TOCOPG, 2020). Tokyo Governor called for voluntary stay at home for Tokyo residents on March 25, 2020. However, we used the data of the nationwide 28 geographical areas in Japan. The effect of this bias would be limited because the number of COVID-19 cases has clearly decreased after the emergency declaration. Fifth, we could not consider host factors, such as immunity or susceptibility, which play an important role in disease transmission and testing. Finally, although we considered the effects of several demographic factors in the multivariable analyses, the virus transmission is a complex. An interdisciplinary, multi-dimensional approach to understand the epidemic growth of COVID-19 will be also required (Bontempi, 2020b; Bontempi et al., 2020).
In conclusion, the epidemic growth of COVID-19 was not associated with precipitation, wind speed, humidity, NO, NO2, Ox, and PM2.5. Conversely, it was significantly associated with increase in daily temperature or sunshine hours during the study period. This suggests that an increase in person-to-person contact due to increased outing activities on a warm and/or sunny day might promote the transmission of COVID-19. Our results also suggested that short-term exposure to suspended particles might influence respiratory infections caused by SARS-CoV-2. However, further research with a well-controlled animal study or an in vitro study is recommended. Our findings suggest that weather is likely to play an indirect role in the transmission of COVID-19. However, the most important thing is that people should have knowledge and understand that SARS-CoV-2 is mainly transmitted human-to-human through close contact, respiratory droplets, fomites, and contaminated surfaces and that daily adequate preventive behavior decreases its transmission.
Credit author statement
Kenichi Azuma, Naoki Kagi, Hoon Kim, Motoya Hayashi. KA, Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Validation; Visualization; Writing - original draft; Writing - review & editing. NK, Conceptualization; Data curation; Investigation; Validation; Writing - original draft; Writing - review & editing. HK, Conceptualization; Validation; Writing - review & editing. MH, Conceptualization; Project administration; Validation; Writing - review & editing.
Ethical considerations on human subjects or experimental animals: study approval
Not applicable because we used only published data and did not use any personal information.
Funding sources supporting the work
No funder supported this work.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to express our deepest gratitude to J.A.G JAPAN Corporation for useful data collection on the COVID-19 Japanese cases. We also thank Nanako Noguchi and Mizuki Harada for help with data collection on climate and ambient air pollution.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110042.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S.J., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JMA . Japan Meteorological Agency; Tokyo: 2020. Search of Past Weather Data.https://www.data.jma.go.jp/obd/stats/etrn/index.php accessed on June 11, 2020. [Google Scholar]
- Baker R.E., Yang W., Vecchi G.A., Metcalf C.J.E., Grenfell B.T. Susceptible supply limits the role of climate in the early SARS-CoV-2 pandemic. Science. 2020 doi: 10.1126/science.abc2535. eabc2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao L., Gao H., Deng W., Lv Q., Yu H., Liu M., Yu P., Liu J., Qu Y., Gong S., Lin K., Qi F., Xu Y., Li F., Xiao C., Xue J., Song Z., Xiang Z., Wang G., Wang S., Liu X., Zhao W., Han Y., Wei Q., Qin C. Transmission of SARS-CoV-2 via close contact and respiratory droplets among hACE2 mice. J. Infect. Dis. 2020;jiaa281 doi: 10.1093/infdis/jiaa281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreca A.I., Shimshack J.P. Absolute humidity, temperature, and influenza mortality: 30 years of county-level evidence from the United States. Am. J. Epidemiol. 2012;176(Suppl. 7):S114–S122. doi: 10.1093/aje/kws259. [DOI] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal B., Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., Liu X., Wei L., Truelove S.A., Zhang T., Gao W., Cheng C., Tang X., Wu X., Wu Y., Sun B., Huang S., Sun Y., Zhang J., Ma T., Lessler J., Feng T. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect. Dis. 2020;(20) doi: 10.1016/S1473-3099(20)30287-5. http://doi: 10.1016/S1473-3099(20)30287-5 S1473-3099. 30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianco A., Biasin M., Pareschi G., Cavalleri A., Cavatorta C., Fenizia F., Galli P., Lessio L., Lualdi M., Redaelli E., Saulle I., Trabattoni D., Zanutta A., Clerici M. UV-C Irradiation is highly effective in inactivating and inhibiting SARS-CoV-2 replication. SSRN. 2020 doi: 10.2139/ssrn.3620830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. First data analysis about possible COVID-19 virus airborne diffusion due to air particulate matter (PM): the case of Lombardy (Italy) Environ. Res. 2020;186:109639. doi: 10.1016/j.envres.2020.109639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: more efforts are necessary to address interdisciplinary research. Environ. Res. 2020;188:109775. doi: 10.1016/j.envres.2020.109775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E., Vergalli S., Squazzoni F. Understanding COVID-19 diffusion requires an interdisciplinary, multi-dimensional approach. Environ. Res. 2020;188:109814. doi: 10.1016/j.envres.2020.109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke, R.M., Midgley, C.M., Dratch, A., Fenstersheib, M., Haupt, T., Holshue, M., et al., Active monitoring of persons exposed to patients with confirmed COVID-19 — United States, January–February 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 245–246. [DOI] [PMC free article] [PubMed]
- Cabinet Office . 2020. Database [visualization] on the Index for Economy, Finance, and Life. Director-General for Policy Planning, Cabinet Office, Tokyo, March 2020.https://www5.cao.go.jp/keizai-shimon/kaigi/special/reform/mieruka/db_top/index.html accessed on May 30, 2020. [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.S., Lam S.Y., Poon L.L., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011:73469. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F.W., Yuan S., Kok K.H., To K.K.W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y., Sridhar S., Chan J.F.W., Ho P.L., Yuen K.Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control Hosp. Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J., Jaspers I. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- Croft D.P., Zhang W., Lin S., Thurston S.W., Hopke P.K., Masiol M., Squizzato S., van Wijngaarden E., Utell M.J., Rich D.Q. The Association between respiratory infection and air pollution in the setting of air quality policy and economic change. Ann. Am. Thorac. Soc. 2019;16:321–330. doi: 10.1513/AnnalsATS.201810-691OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Montigny L., Ling R., Zacharias J. The effects of weather on walking rates in nine cities. Environ. Behav. 2012;44:821–840. [Google Scholar]
- Domingo J.L., Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020;187:109650. doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo J.L., Marquès M., Rovira J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ. Res. 2020;188:109861. doi: 10.1016/j.envres.2020.109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliasson I., Knezb I., Westerberg U., Thorsson S., Lindberg F. Climate and behaviour in a Nordic city. Landsc. Urban Plann. 2007;82:72–84. [Google Scholar]
- Fares A. Factors influencing the seasonal patterns of infectious diseases. Int. J. Prev. Med. 2013;4:128–132. [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264:114732. doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisman D.N. Seasonality of infectious diseases. Annu. Rev. Publ. Health. 2007;28:127–143. doi: 10.1146/annurev.publhealth.28.021406.144128. [DOI] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D.S.C., Du B., Li L., Zeng G., Yuen K.Y., Chen R. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunthe S.S., Swain B., Patra S.S., Amte A. On the global trends and spread of the COVID-19 outbreak: preliminary assessment of the potential relation between location-specific temperature and UV index. J. Public Health: From Theory to Practice. 2020 doi: 10.1007/s10389-020-01279-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou Y.J., Okuda K., Edwards C.E., Martinez D.R., Asakura T., Dinnon K.H., III., Kato T., Lee R.E., Yount B.L., Mascenik T.M., Chen G., Olivier K.N., Ghio A., Tse L.V., Leist S.R., Gralinski L.E., Schäfer A., Dang H., Gilmore R., Nakano S., Sun L., Fulcher M.L., Livraghi-Butrico A., Nicely N.I., Cameron M., Cameron C., Kelvin D.J., de Silva A., Margolis D.M., Markmann A., Bartelt L., Zumwalt R., Martinez F.J., Salvatore S.P., Borczuk A., Tata P.R., Sontake V., Kimple A., Jaspers I., O'Neal W.K., Randell S.H., Boucher R.C., Baric R.S. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;11447 doi: 10.1016/j.cell.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikäheimo T.M., Jaakkola K., Jokelainen J., Saukkoriipi A., Roivainen M., Juvonen R., Vainio O., Jaakkola J.J.K. A decrease in temperature and humidity precedes human rhinovirus infections in a cold climate. Viruses. 2016;8(9):244. doi: 10.3390/v8090244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola K., Saukkoriipi A., Jokelainen J., Juvonen R., Kauppila J., Vainio O., Ziegler T., Rönkkö E., Jaakkola J.J., Ikäheimo T.M. Decline in temperature and humidity increases the occurrence of influenza in cold climate. Environ. Health. 2014;13(1):22. doi: 10.1186/1476-069X-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- J.A.G JAPAN Corporation . J.A.G JAPAN Corporation; Tokyo: 2020. Dashboard & Map of Coronavirus COVID-19 Japan Case (2019-nCoV)https://gis.jag-japan.com/covid19jp/ accessed on May 30, 2020. [Google Scholar]
- Jiang H., Jang M., Sabo-Attwood T., Robinson S.E. Oxidative potential of secondary organic aerosols produced from photooxidation of different hydrocarbons using outdoor chamber under ambient sunlight. Atmos. Environ. 2016;131:382–389. [Google Scholar]
- Jüni P., Rothenbühler M., Bobos P., Thorpe K.E., da Costa B.R., Fisman D.N., Slutsky A.S., Gesink D. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ (Can. Med. Assoc. J.) 2020;192:E566–E573. doi: 10.1503/cmaj.200920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamoto T., Pham T.T., Matsuda T., Oyama T., Tanaka M., Yu H.S., Uchiyama I. Historical review on development of environmental quality standards and guideline values for air pollutants in Japan. Int. J. Hyg Environ. Health. 2011;214:296–304. doi: 10.1016/j.ijheh.2011.05.007. [DOI] [PubMed] [Google Scholar]
- Kroll J.H., Seinfeld J.H. Chemistry of secondary organic aerosol: formation and evolution of low-volatility organics in the atmosphere. Atmos. Environ. 2008;42:3593–3624. [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., Azman A.S., Reich N.G., Lessler J. The incubation period of coronavirus disease 2019 (covid-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Xu X.L., Dai D.W., Huang Z.Y., Ma Z., Guan Y.J. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Zhang B., Lu J., Liu S., Chang Z., Cao P., Liu X., Zhang P., Ling Y., Tao K., Chen J. The characteristics of household transmission of COVID-19. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa450. ciaa450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T., Yan J., Shi Y., Ren X., Niu J., Zhu W., Li S., Luo B., Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multicity study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Liao X., Qian S., Yuan J., Wang F., Liu Y., Wang Z., Wang F.S., Liu L., Zhang Z. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg. Infect. Dis. 2020;26:1320–1323. doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Méndez-Arriaga F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020;735:139560. doi: 10.1016/j.scitotenv.2020.139560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737:139659. doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MIAC . Statistics Bureau, Ministry of Internal Affairs and Communications Japan; Tokyo: 2019. Statistical Observations of Municipalities 2019. June 2019. [Google Scholar]
- MOE . Ministry of the Environment; Tokyo: 2020. Atmospheric Environmental Regional Observation System (AEROS)http://soramame.taiki.go.jp/Index.php accessed on June 11, 2020. [Google Scholar]
- Oberdörster G., Oberdörster E., Oberdörster J. Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ. Health Perspect. 2005;113:823–839. doi: 10.1289/ehp.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascual M., Dobson A. Seasonal patterns of infectious diseases. PLoS Med. 2005;2(1):e5. doi: 10.1371/journal.pmed.0020005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paynter S. Humidity and respiratory virus transmission in tropical and temperate settings. Epidemiol. Infect. 2015;143:1110–1118. doi: 10.1017/S0950268814002702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan L.T., Nguyen Thuong V., Luong Q.C., Nguyen Thinh V., Nguyen H.T., Le H.Q., Nguyen T.T., Cao T.M., Pham Q.D. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N. Engl. J. Med. 2020;382:872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., Su Q., Wang W., Wang X., Zhang Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of Coronavirus Disease 2019 (COVID-19) JAMA Netw. Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaman J., Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc. Natl. Acad. Sci. Unit. States Am. 2009;106:3243–3248. doi: 10.1073/pnas.0806852106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokinger H.E., Coffin D.L. Biologic effects of air pollutants. In: Arthur C.S., editor. Air Pollution. Volume I, Air Pollution and its Effects. 2nd ed. Academic Press; London), New York: 1968. [Google Scholar]
- Sungnak W., Huang N., Bécavin C., Berg M., Queen R., Litvinukova M., Talavera-López C., Maatz H., Reichart D., Sampaziotis F., Worlock K.B., Yoshida M., Barnes J.L. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 2020;26:681–687. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J., Mu L., Huang J., Yu S., Chen B., Yin J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community Health. 2005;59:186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashiro A., Shaw R. COVID-19 pandemic response in Japan: what is behind the initial flattening of the curve? Sustainability. 2020;12(13):5250. doi: 10.3390/su12135250. [DOI] [Google Scholar]
- Thorsson S., Honjo T., Lindberg F., Eliasson I., Lim E.M. Thermal comfort and outdoor activity in Japanese urban public places. Environ. Behav. 2007;39:660–684. [Google Scholar]
- TOCOPG . 2020. Olympic Games Postponed to 2021. The Tokyo Organising Committee of the Olympic and Paralympic Games., Tokyo.https://tokyo2020.org/en/news/joint-statement-from-international-olympic-committee-and-tokyo2020 accessed on June 25, 2020. [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O.A.I., Lestari H., Bahar H., Asfian P. Correlation between weather and covid-19 pandemic in jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ujiie M., Tsuzuki S., Ohmagaria N. Effect of temperature on the infectivity of COVID-19. Int. J. Infect. Dis. 2020;95 doi: 10.1016/j.ijid.2020.04.068. 303–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USEPA . Office of Research and Development, U.S. Environmental Protection Agency; Research Triangle Park, NC: 2019. Integrated Science Assessment for Particulate Matter. EPA/600/R-19/188. [PubMed] [Google Scholar]
- Wakamatsu S. Overseas trends of PM2.5 and future challenges in measurement, monitoring and componential analysis. J. Jpn. Soc. Atmos. Environ. 2011;46:77–83. (in Japanese with English abstract) [Google Scholar]
- WHO . WHO/SDE/PHE/OEH/06.02; Geneva: 2006. WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide, Global Update 2005, Summary of Risk Assessment. World Health Organization. [Google Scholar]
- WHO . World Health Organization; Geneva: 2020. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. [Google Scholar]
- WHO . World health Organization; Geneva: 2020. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions. Scientific Brief on 9 July 2020. [Google Scholar]
- Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus Disease 2019 (COVID-19): a review. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., Du M., Liu M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Yan C., Fu Q., Xiao K., Yu Y., Han D., Wang W., Cheng J. Possible environmental effects on the spread of COVID-19 in China. Sci. Total Environ. 2020;731:139211. doi: 10.1016/j.scitotenv.2020.139211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan R., Zhang Y., Li Y., Xia L., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., Wang W. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55:2000517. doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W.A. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.