Abstract
Materials and Methods
The study was a parallel randomized controlled trial. Patients admitted to the transplantation ward participated in the study. Fifty-three eligible patients were allocated into the foot reflexology group (n = 26) and the control group (n = 27) by using the stratified randomization method. Finally, 25 participants in each group finished the study. The intervention group received foot reflexology for 30 minutes once a day for three consecutive days, and no reflexology was applied in the control group. The intervention started on the second day after surgery. Pain, fatigue, and quality of sleep were measured on the first, second (before intervention), third, fourth, and eleventh days after surgery. Data were collected using visual analogue scale for measuring pain and fatigue and Verran and Snyder-Halpern sleep scale for measuring quality of sleep.
Results
In each group, 25 patients finished the study. The mean pain score in the foot reflexology and control groups decreased from 9.44 ± 0.96 and 9.36 ± 0.91 on the day of surgery to 1.32 ± 0.94 and 4.32 ± 1.68 on the eleventh day after surgery, respectively. The mean fatigue score in the reflexology and control groups decreased from 8.76 ± 1.27 and 8.6 ± 1.26 on the day of surgery to 1.24 ± 1.2 and 3.92 ± 1.63 on the eleventh day after surgery, respectively. The mean sleep score in the foot reflexology and control groups increased from 33.38 ± 11.22 and 39.59 ± 12.8 on the day of surgery to 69.43 ± 12.8 and 56.27 ± 8.03 on the eleventh day after surgery, respectively. While pain, fatigue, and sleep quality scores improved in both groups, those in the intervention group showed significantly greater improvement compared with the control group (P < 0.001). No significant difference was found between the two groups in the use of acetaminophen on the first, second, third, fourth, and eleventh days after surgery (P > 0.05).
Conclusion
Foot reflexology may reduce pain and fatigue and improve sleep quality of patients after kidney transplantation.
1. Introduction
Kidney transplantation is the most effective treatment for end-stage kidney disease worldwide [1]. According to the statistics from the Global Observatory on Donation and Transplantation, the cases of kidney transplantation were 90,306 worldwide in 2017 [2]. In Iran, 48.8% of kidney failure patients are undergoing kidney transplantation [3]. Evidence suggests that successful kidney transplantation can improve quality of life, life expectancy, and reduce health costs [4]. However, patients may experience different physical difficulties such as cardiovascular and neurologic complications [5], sexual dissatisfaction [6], or mental disorders such as anxiety, depression, or stress [7]. Patients may also experience postoperative pain, fatigue, and sleep disorders [8].
Some patients experience severe pain on their back, chest, inguinal area, the surgery area, and head after kidney transplantation surgery [9, 10], and postsurgical pain is a major therapeutic problem in these patients [11]. This pain may become worse if not managed properly [12]. An inverse association is available between pain and blood pressure, and uncontrolled postoperative pain leads to hypotension and other postoperative disorders [13]. Fatigue and lack of energy are other common postoperative symptoms [14]. Few studies have shown that patients under kidney transplantation experience more fatigue than healthy subjects [15]. The prevalence of postoperative fatigue was 48.3% in one study, which was 41.5% three months later and 38.1% six months later [16]. Fatigue can affect quality of sleep of kidney transplant recipients. On the other hand, sleep deprivation in these patients can cause fatigue, depression, pain, and stress [17, 18].
Different complementary and alternative medicine (CAM) methods such as foot reflexology are used for managing symptoms among some patients after kidney transplantation [19]. Foot reflexology is a special form of massage that accompanies with the pressure of the fingers, especially the thumbs on the reflex areas usually in the feet. These areas are believed to associate with all parts of the body, and applying pressure on them can affect the physiological responses of the body. They are thought to improve recovery and return homeostasis [20]. Foot reflexology can regulate blood circulation and hemodynamic variables [21]. The underlying mechanisms of reflexology are not well understood. Reflexology is assumed to facilitate relaxation, release endorphins, and modulate pain-impulse transmission and pain perception [22]. Subsequently, relaxation can effect quality of sleep and fatigue [23–25]. In addition, touch and massage of reflex points in the foot may reduce patients' pain. Diseases are caused by the blockage of energy in the body, and stimulation of reflex points may eliminate these obstructions and release energy in the body [26].
Several studies have examined the effects of foot reflexology on symptoms such as pain, fatigue, and quality of sleep of patients [19, 27–30]. Other studies showed a positive effect of foot reflexology on pain and anxiety of patients after general and spinal surgery [29, 30] and during chemotherapy and after breast cancer surgery [31, 32]. Different studies showed the positive effects of reflexology on alleviating fatigue in patients [33, 34]. Asltoghiri et al. showed the improvement of sleep disorders using reflexology [35]. Lee considered foot reflexology as a useful intervention to decrease fatigue and promote quality of sleep [36]. Moreover, the results of a systematic review showed that reflexology was safe and effective for insomnia, but further studies with greater accuracy and power are needed [37].
The complementary and alternative therapies have been increasingly used in recent decades, and nurses prefer to use noninvasive methods with minimal side effects [36]. Since reflexology does not have major side effects [37], nurses can use it to improve the quality of nursing care. However, decisions are still being made with caution due to insufficient research studies. No study has investigated the effect of reflexology on pain, fatigue, and quality of sleep after kidney transplantation; therefore, the current study tested the hypothesis that the mean scores of pain, fatigue, and quality of sleep in patients after kidney transplantation surgery were different between the foot reflexology and control groups after the intervention and one week later.
2. Materials and Methods
2.1. Study Type and Setting
This study was a parallel randomized controlled trial. Patients taken to the transplantation department of Afzalipour Hospital, Kerman, Iran, were studied from April 2018 to May 2019.
2.2. Sample Size and Sampling
According to a pilot study (5 samples in each group) (on the fourth day after surgery, the mean and standard deviation in the pilot reflexology group were 3.2 ± 2.17 and the mean and standard deviation in the pilot control group were 5.2 ± 1.3), the sample size was estimated to be 21 individuals for each group with a confidence coefficient of 95% and type II error of 10%. Due to the probability of dropout, 25 samples were selected in each group. It is noteworthy that the pilot samples were included in the final analysis. Furthermore, power analysis calculated with G∗Power software indicates that (power = 90%, P=0.05) 46 participants would be needed (23 per group) to detect an effect size of 0.2. Inclusion criteria were the minimum age of 15 years old, the first turn of the kidney transplantation, no ulcers or injuries in feet, especially the sole, complete postoperative consciousness, no history of using foot reflexology, no addiction to drug use or alcohol, and no mental disorder. Exclusion criteria were the patient's return to the operating room during the study, the patient's need to a sedative, and any symptoms indicative of transplant rejection (with the doctor's diagnosis). Sixty patients were examined for the inclusion criteria, of whom seven were not eligible due to different reasons such as a second transplant, no age fulfillment, and mental disorder. In addition, there were three dropouts due to returning to the operating room and rejection of the transplant. Finally, 25 samples in each group completed the study, and their data were analyzed (Figure 1). Eligible patients were selected by convenience sampling and allocated to the intervention and control groups with the stratified randomization method using gender and age (±2) as strata. In other words, the first sample was randomly allocated either to the intervention or control groups (using the lottery), and the subsequent samples were randomly allocated to both groups according to the matching variables. The first author assessed the participants according to the inclusion criteria and allocated them into the groups.
Figure 1.
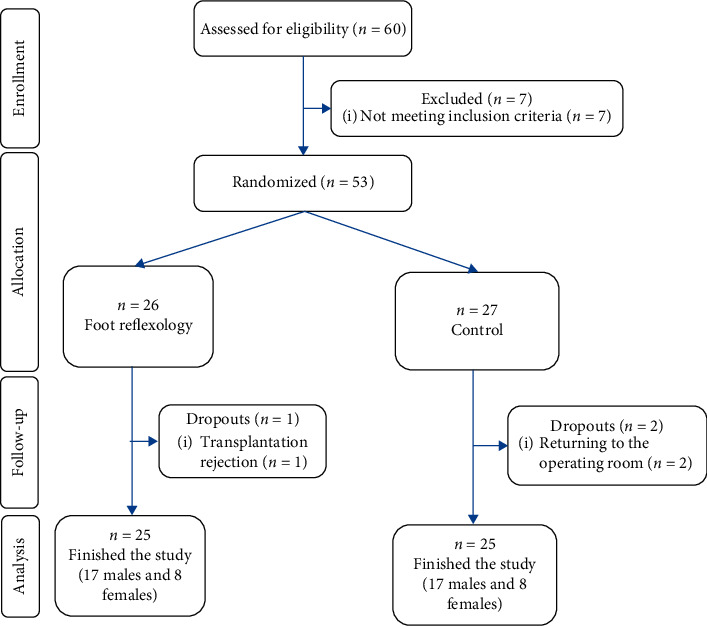
The flow diagram of the study.
2.3. Data Collection Tools
The data collection tool was a four-part questionnaire including demographic information, the sedation and analgesic checklist, visual analogue scale (VAS), and Verran and Snyder-Halpern sleep scale. The demographic questionnaire included age, sex, marital status, educational level, family income, smoking history, type of dialysis, date of operation, name of the surgeon, the duration of kidney failure, underlying diseases such as digestive diseases, diabetes, and hypertension, the patient's drugs (narcotics and sedation), and routine tests in the transplantation department such as hemoglobin, white blood cells, blood urea, platelets, creatinine, sodium, potassium, calcium, glucose, and liver enzymes. Sedation and analgesic checklist included midazolam, ketamine, fentanyl, cisatracurium, thiopental, lidocaine, morphine, and acetaminophen.
The visual analogue scale (VAS) was used to measure pain and fatigue [38]. The VAS is a self-administered visual scale that includes a 10 cm horizontal line graded from 0 to 10. Zero indicates no pain/fatigue, 1 – 3 indicates mild pain/fatigue, 4 – 7 indicates moderate pain/fatigue, and 8 – 10 indicates severe pain/fatigue. Many studies have confirmed the VAS reliability and validity [39, 40].
The Verran and Snyder-Halpern sleep scale was used to measure quality of sleep. This scale has 15 items that assess sleep in patients. This tool measures the participant's quality of sleep on the last night. It also includes various sleep parameters, such as sleep disrupters, number of waking cycles, difficulty in falling asleep, and sleep duration. The instrument is based on the scale value of 0 to 100 mm. The total score of the questionnaire is also between 0 and 100. The higher the score, the better the quality of sleep [41]. The reliability and validity of this scale have been confirmed in Iran [42].
2.4. Data Collection
The researchers referred to the research setting and started sampling after obtaining permission from the hospital management and the transplantation department. Demographic and background information was first assessed using the medical record and, if necessary, by asking the patients. Then, they were randomly divided into intervention and control groups according to the inclusion criteria. Pain, fatigue, and quality of sleep were measured on the first day of surgery to have the basis data. Pain, fatigue, and quality of sleep were measured on the second day after surgery before the intervention. We started the intervention on the second day to be sure that patients were in stable condition and attendance of the researchers in the ward did not interfere with the routine care. The intervention was conducted for three consecutive days. Again, pain, fatigue, and quality of sleep were measured immediately and one week after the intervention (i.e., the fourth day and eleventh day after surgery). The length of intervention was considered 3 sessions (daily) by reviewing the similar studies and consulting with the surgeon. In our center, patients are regularly discharged from the transplantation ward after 12–14 days. Therefore, we have chosen one-week follow-up.
The number of acetaminophen tablets (500 mg) taken by patients was also measured on the first, second, third, fourth, and eleventh days of surgery.
2.5. Intervention Protocol
The reflexology was applied to the intervention group according to the previous studies from the second day after surgery in the late hours of the evening shift and at least 4 hours after the last time when the patient received sedatives [30, 43, 44]. The evening shift was chosen because of the proximity to the patient's sleep hours and low workload of personnel. The patient's privacy was observed before the reflexology. The patient was placed in a relaxed position in a quiet and bright environment, and the researcher sat down on a chair at the bottom of the patient's bed and applied the reflexology. First, the researcher warmed her hands and cleaned the patient's feet with a warm wet napkin. Then, the feet were gently massaged for 3 minutes [33]. The researcher placed one hand at the back of big toe while applying pressure on the pituitary and pineal gland points. She took the heel of the foot with her left hand and applied pressure on the spinal points with the right-hand thumb [45]. She moved back and forth the patient's outer edge of the foot with her thumb [46]. The massage was applied with slow speed and regular rhythm with a tolerable pressure. The level of pressure was dependent on patients self-reporting of not feeling any pain regarding applying pressure. The massage of reflex zones lasted for nine minutes. Lastly, the foot was gently massaged for 3 minutes the same as the beginning of the procedure. Therefore, the protocol was performed for 15 minutes [34, 47] on each foot (30 minutes each session) in 3 sessions [48]. No lubricant was used for the application of the reflexology. It is noteworthy that the reflexology protocol was approved by the Iranian Art Massage Institute (https://artmassage.ir/). No reflexology was applied in the control group, and routine care of the transplantation department was taken. A nurse who did not know the assignment of the samples in the two groups completed patient's pain, fatigue, and quality of sleep scales by interviewing the participants immediately and one week after the intervention. It should be noted that the first researcher carried out all interventions. A Chinese medicine expert trained the first researcher in a 24-hour reflexology course. In addition, the first researcher received certification from the training center, i.e., the Iranian Art Massage Institute (https://artmassage.ir/).
2.6. Data Analysis
SPSS 18 was used to analyze the data. Independent t-test (or Mann–Whitney U test), chi-squared test, or Fisher's exact tests were used to determine the similarity of the two groups in terms of underlying and confounding variables at the beginning of the study. Repeated measures ANOVA or Friedman test was used to determine the mean difference in the pain, fatigue, and quality of sleep between the two groups.
2.7. Ethical Considerations
The ethics committee of Kerman University of Medical Sciences approved the protocol of the study(No.IR.KMU.REC.1397.071, IRCT20170116031972N6;https://en.irct.ir/trial/31687). The researchers explained research goals and protocol to the participants before their inclusion in the study, and if they had been willing to participate in the study, written informed consent would have been obtained from all eligible participants.
3. Results
The mean age of the participants in the foot reflexology group was 38.12 ± 12.87, and the mean age of them in the control group was 38.56 ± 12. The majority (81. 32%) of the samples in both groups were female. 60% of the samples in the foot reflexology group and 68% of the control group were married. 12% of the samples in both groups were uneducated. 48% of the samples in the foot reflexology group and 60% of the control group had diploma or more. 40% of the samples of both groups had family income less than a million toman (P > 0.05).
No significant difference was found between the two groups in the variables of sex, marital status, education level, and income level (P > 0.05). Furthermore, no significant difference was found between the two groups in clinical variables including duration of kidney failure (month), duration of dialysis (month), type of dialysis, history of diabetes, hypertension, heart diseases, and cigarette smoking (P > 0.05). No significant difference was observed between the two groups of foot reflexology and control in the results of laboratory tests before the kidney transplantation surgery (P > 0.05). One surgeon performed the surgery for the two groups, and they received similar medications during kidney transplantation. It should be noted that all surgical procedures lasted approximately 3 hours.
The mean pain score in the foot reflexology group decreased from 9.44 ± 0.96 on the day of surgery to 1.32 ± 0.94 on the eleventh day after surgery (P < 0.001). The mean pain score in the control group decreased from 9.36 ± 0.91 on the day of surgery to 4.32 ± 1.68 on the eleventh day after surgery (P < 0.001). Pain score significantly decreased three days after foot reflexology compared with the control group (P < 0.001). A significant decrease was found despite the completion of the intervention on the eleventh day after surgery (P < 0.001) (Table 1). No significant difference was found between the two groups in the use of acetaminophen on the first (P > 0.99), second (χ2 = 0.14, P=0.5), third (χ2 = 1.05, P=0.25), fourth (Fisher's exact test = 0.17, P=0.5), and eleventh days after surgery (Fisher's exact test = 0.34, P=0.5).
Table 1.
Comparison of mean score of pain in intervention and control groups.
| Group | ||||||
|---|---|---|---|---|---|---|
| Pain | Intervention | Control | Mann–Whitney U test | P value | ||
| Mean | SD | Mean | SD | |||
| The first day of surgery | 9.44 | 0.96 | 9.36 | 0.91 | −0.64 | 0.52 |
| Before intervention (the second day after surgery) | 8.28 | 1.24 | 7.96 | 1.14 | −1.15 | 0.25 |
| Immediately after intervention (the fourth day after surgery) | 3.48 | 1.26 | 5.72 | 1.7 | −4.31 | <0.001 |
| One week after intervention (the eleventh day after surgery) | 1.32 | 0.94 | 4.32 | 1.68 | −5.53 | <0.001 |
| Friedman test | 71.76 | 71.94 | — | |||
| P value | <0.001 | <0.001 | — | |||
The mean fatigue score in the reflexology group decreased from 8.76 ± 1.27 on the day of surgery to 1.24 ± 1.2 on the eleventh day after surgery (P < 0.001). The mean fatigue score in the control group decreased from 8.6 ± 1.26 on the day of surgery to 3.92 ± 1.63 on the eleventh day after surgery (P < 0.001). Fatigue score significantly decreased three days after foot reflexology in comparison with the control group (P < 0.001). A significant decrease was seen despite the completion of intervention on the eleventh day after surgery (P < 0.001) (Table 2).
Table 2.
Comparison of mean score of fatigue in intervention and control groups.
| Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| Fatigue | Intervention | Control | Statistical test ∗ | P value | Mean difference | P value ∗∗ | ||
| Mean | SD | Mean | SD | |||||
| The first day of surgery | 8.76 | 1.27 | 8.6 | 1.26 | 12.74 | 0.001 | 0.16 | 0.66 |
| Before intervention (the second day after surgery) | 7.52 | 1.16 | 7.2 | 1.68 | 0.32 | 0.44 | ||
| Immediately after intervention (the fourth day after surgery) | 3.32 | 1.41 | 5.56 | 1.66 | −2.24 | <0.001 | ||
| One week after intervention (eleventh day after surgery) | 1.24 | 1.2 | 3.92 | 1.63 | −2.68 | <0.001 | ||
| Sphericity test | 300.34 | 89.81 | — | |||||
| P value | <0.001 | <0.001 | — | |||||
∗Repeated measures analysis of variance. ∗∗Adjusted for multiple comparisons.
The mean sleep score in the foot reflexology group increased from 33.38 ± 11.22 on the day of surgery to 69.43 ± 12.8 on the eleventh day after surgery (P < 0.001). The mean sleep score in the control group increased from 39.59 ± 12.8 on the day of surgery to 56.27 ± 8.03 on the eleventh day after surgery (P < 0.001). The sleep score significantly increased three days after foot reflexology compared with the control group (P=0.01). Such an increase continued despite the completion of intervention on the eleventh day after surgery (P < 0.001) (Table 3).
Table 3.
Comparison of mean score of quality of sleep in intervention and control groups.
| Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| Quality of sleep | Intervention | Control | Statistical test ∗ | P value | Mean difference | P value ∗∗ | ||
| Mean | SD | Mean | SD | |||||
| The first day of surgery | 33.38 | 11.22 | 39.59 | 12.8 | 10.84 | <0.001 | −6.21 | 0.07 |
| Before intervention (the second day after surgery) | 41.98 | 13.92 | 42.15 | 11.78 | −0.17 | 0.96 | ||
| Immediately after intervention (the fourth day after surgery) | 60.60 | 10.75 | 52.23 | 11.76 | 8.38 | 0.01 | ||
| One week after intervention (the eleventh day after surgery) | 69.43 | 8.74 | 56.27 | 8.03 | 13.17 | <0.001 | ||
| Greenhouse–Geisser test | 76.12 | 19.22 | — | |||||
| P value | <0.001 | <0.001 | — | |||||
∗Repeated measures analysis of variance. ∗∗Adjusted for multiple comparisons.
In addition, no adverse effects were reported or observed during the intervention and follow-up period.
4. Discussion
The results of the present study showed that foot reflexology alleviated pain and fatigue and improved quality of sleep after kidney transplantation surgery. The effects of foot reflexology on pain, fatigue, and quality of sleep were clinically important. However, reflexology did not reduce acetaminophen consumption.
Few studies have investigated the effect of reflexology on pain of patients after kidney transplantation surgery. Most studies have examined reflexology effects on pain of patients after other surgeries. Other studies also confirmed the effect of reflexology on pain after abdominal hysterectomy [49], abdominal surgery [50], postoperative cancer cystectomy [51], abdominal and chest surgery [52], amputation of the lower extremity [53], and spinal surgery [30]. Koras and Karabulut found that although the pain intensity in patients undergoing laparoscopic cholecystectomy did not change for 5 minutes after reflexology, the intensity of pain reduced 30, 60, 90, and 120 minutes after reflexology [54]. Bhagya et al. reported that foot reflexology reduced pain of patients after open-heart surgery and sternotomy, cesarean section, and digestive system surgeries [29]. Mohammad Aliha et al. and Koras et al. also reported that foot reflexology reduced the consumption of analgesics and sedatives [52, 54]. These results do not support our findings. The difference in results may be because the patients in the study of Mohammad Aliha et al. were studied only during 24 hours after surgery and those in the study of Koras et al. were studied for 2 hours [52, 54]. However, in the current study, patients received the intervention from the second day after surgery and were examined for 11 days. Another reason for the inconsistency between our results and those of Mohammad Aliha et al. and Koras et al. [52, 54] may be the low rate of acetaminophen prescription in the present study. According to our data, only 4 to 28 percent of the participants took acetaminophen during their hospitalization after surgery and no other analgesics were prescribed for them. In general, most people struggle to deal with postoperative pain [20, 49]. Reflexology is assumed to increase secretion of endorphins and modulate pain impulse which positively affects pain perception [22]. Touch and massage of reflexology points, such as the pituitary, solar plexus, and spinal reflex zones, may reduce pain of patients after kidney transplantation.
The results of the current study showed severe fatigue in the foot reflexology group on the first and second days after the surgery, but the pain was moderate on the fourth day and mild on the eleventh day. The intensity of fatigue in the control group was severe on the first and second days after surgery, but it was moderate on the fourth and eleventh days. The intensity of fatigue significantly reduced three days after foot reflexology compared with the control group, and the effect of foot reflexology continued until the eleventh day after surgery. Few studies have investigated the effect of reflexology on fatigue after the kidney transplantation surgery or other surgeries [55], and no similar article was found on kidney transplanted patients. In the study of Mohammadi et al., the patients in the intervention group received a 30-minute foot reflexology on the second day after coronary artery bypass surgery (preferably the left foot). The results of the study showed reduction of fatigue in the intervention group 10 minutes after the intervention compared with the control group. However, the intensity of fatigue was not significantly different between the intervention and control groups 30 minutes and 24 hours after the intervention [55]. Mohammadi et al. do not support the results of the current study. It seems that the duration of the intervention and a different study population have influenced the treatment. Mohammadi et al. applied reflexology on patients only once, while the present study and Bagheri et al. applied reflexology on patients for three consecutive days. Furthermore, reflexology was applied on both feet of the patient in the current study while it was applied on the patient's foot in the study of Mohammadi et al. The index and thumb fingers are pressed on certain points of the foot that are associated with organs, glands, and other parts of the body. The blockage of energy in the body is assumed to be the cause of diseases, and reflexology massage of solar plexus can alleviate fatigue [44, 56].
The results of the current study showed the improvement of quality of sleep in both groups on the 4th and 11th days after surgery. The sleep score in the foot reflexology group increased by 36 at the end of the study, while the control group obtained nearly 17 points. A 19-point difference between the two groups shows the clinical importance of foot reflexology for the quality of sleep. Few studies have investigated the effect of reflexology on the quality of sleep of the patients after kidney transplantation surgery or other surgeries [26]. According to Kheyri et al., elderly women in the intervention group received foot reflexology twice a day (morning and night for 20 minutes) on the second and third days after abdominal surgery. The results of this study showed the improvement of quality of sleep in elderly women in the intervention group compared with the control group [26]. Several studies have also confirmed the positive effects of the foot reflexology on quality of sleep of the hemodialysis patients [28, 57]. Foot reflexology can stimulate the nervous system and provoke the dopamine secretion which may improve quality of sleep [58]. Since no research determined the effect of foot massage on quality of sleep after kidney transplantation surgery, further research is needed to confirm the effect of this intervention on these patients.
The present study has some limitations. Given that the transplantation rooms have two beds, in one case, one patient from the reflexology group and one patient from the control group were in one room adjacent to each other. However, a partition was used to reduce the effect of the intervention on the mentioned case in the control group. As the level of pressure was dependent on the patient tolerance, it was impossible to apply a uniform pressure for all patients. However, the level of pressure should naturally be adjusted with patient tolerance. In addition, the individual differences regarding the different perception of pain and fatigue are among the limitations of this research. The use of only one type of scale for measuring pain and fatigue can reduce the actual rate of perceived pain and fatigue. In addition, we used VAS for assessing fatigue. Although there are some more specific fatigue scales, we chose VAS as it was not time-consuming and was easy to understand in acute phase after kidney transplantation surgery. In addition, the first researcher allocated the samples into groups, which may be associated with bias. According to our literature review, this is the first study conducted on hospitalized patients under kidney transplantation surgery, and we adhered to minimum conditions of a randomized controlled trial. Therefore, the halo effect could not be rejected. Finally, the study setting was one of the referral transplantation centers in southeast Iran, so the results should be generalized with caution.
5. Conclusion
The results of the current study showed a significant reduction in the mean scores of pain and fatigue in the group of foot reflexology massage after the intervention compared with the control group. In addition, the quality of sleep score in the foot reflexology group significantly improved immediately and one week after the intervention compared with the control group. Therefore, foot reflexology may somewhat reduce pain and fatigue and improve sleep quality. Foot reflexology is a simple, low-cost, and applicable treatment that can be easily taught to nurses in various departments of the health care center. Given the limited evidence, further studies are needed to confirm the effects of foot reflexology on the symptoms after kidney transplantation surgery.
Acknowledgments
We would thank all patients and the nursing staff of the kidney transplantation units of Afzalipour Hospital for their cooperation.
Abbreviations
- VAS:
Visual analogue scale.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Disclosure
The approved research project code is 96001077.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
AS and MD developed the study idea and protocol. MA and MRE supervised the study sampling. AS performed the sampling and wrote the first draft of the manuscript. MD analyzed the data. All authors read and confirmed the final version of the manuscript.
References
- 1.Ghonemy T., Farag S., Soliman S., El-okely A., El-hendy Y. Epidemiology and risk factors of chronic kidney disease in the El-Sharkia Governorate, Egypt. Saudi Journal of Kidney Diseases and Transplantation. 2016;27(1):p. 111. doi: 10.4103/1319-2442.174137. http://www.sjkdt.org/text.asp?2016/27/1/111/174137. [DOI] [PubMed] [Google Scholar]
- 2. http://www.transplant-observatory.org/contador1/, Transplant-observatory.org [Internet]. Global Observatory on Donation and Transplantation, Organs Transplanted Annually (2017) [cited 2020 Jul 2]. Availeble from:
- 3.Mousavi S. S., Soleimani A., Mousavi M. B. Epidemiology of end-stage renal disease in Iran: a review article. Saudi Journal of Kidney Diseases and Transplantation: An Official Publication of the Saudi Center for Organ Transplantation, Saudi Arabia. 2014;25(3):697–702. doi: 10.4103/1319-2442.132242. [DOI] [PubMed] [Google Scholar]
- 4.Soltannezhad F., Farsi Z. An investigation of quality of life in kidney transplant patients. Journal of Military Care Sciences. 2015;2(3):72–167. doi: 10.18869/acadpub.mcs.2.3.167. [DOI] [Google Scholar]
- 5.Dogan U., Yaprak M., Dogan E. A., Onac M., Yılmaz V. T., Aydinli B. Cardiovascular and neurologic complications in kidney transplant recipients: a focused appraisal of symptoms. Transplantation Proceedings. 2019;51(4):1101–1107. doi: 10.1016/j.transproceed.2019.02.005. https://linkinghub.elsevier.com/retrieve/pii/S0041134518318402. [DOI] [PubMed] [Google Scholar]
- 6.Mota R. L., Fonseca R., Santos J. C., et al. Sexual dysfunction and satisfaction in kidney transplant patients. The Journal of Sexual Medicine. 2019;16(7):1018–1028. doi: 10.1016/j.jsxm.2019.03.266. https://linkinghub.elsevier.com/retrieve/pii/S1743609519307246. [DOI] [PubMed] [Google Scholar]
- 7.Mollahadi M., Tayyebi A., Ebadi A., Daneshmandi M. Comparison between anxiety, depression and stress in hemodialysis and kidney transplantation patients. Journal of Critical Care Nursing. 2010;2(4):p. 155. [Google Scholar]
- 8.Mıhçıokur S., Doğan G., Kocalar G., Erdal R., Haberal M. Emergency department visits after kidney, liver, and heart transplantation in a hospital of a university in Turkey: a retrospective study. Experimental and Clinical Transplantation : Official Journal of the Middle East Society for Organ Transplantation. 2019;17(Suppl 1):264–269. doi: 10.6002/ect.MESOT2018.P120. http://www.ectrx.org/forms/ectrxcontentshow.php?doi_id=10.6002/ect.MESOT2018.P120. [DOI] [PubMed] [Google Scholar]
- 9.Miller R. D., Eriksson L. I., Fleisher L. A., Wiener-Kronish J. P., Cohen N. H., Young W. L. Miller’s Anesthesia E-Book. Elsevier Health Sciences. Amsterdam, Netherlands: Elsevier Health Sciences; 2014. [Google Scholar]
- 10.Amini Z., Mostafa R., Hamid Reza B., Akram S., Leila J., Azadeh K. The effects of foot reflexology on the level of depression in patients under hemodialysis. Journal of Nursing Education. 2017 10;5(6):33–39. doi: 10.21859/jne-05065. http://jne.ir/browse.php?a_id=765&sid=1&slc_lang=en. [DOI] [Google Scholar]
- 11.Cuñetti L., Manzo L., Peyraube R., Arnaiz J., Curi L., Orihuela S. Chronic pain treatment with cannabidiol in kidney transplant patients in Uruguay. Transplantation Proceedings. 2018;50(2):461–464. doi: 10.1016/j.transproceed.2017.12.042. [DOI] [PubMed] [Google Scholar]
- 12.Thapa P., Euasobhon P. Chronic postsurgical pain: current evidence for prevention and management. The Korean Journal of Pain. 2018;31(3):155–173. doi: 10.3344/kjp.2018.31.3.155. doi: 10.3344/kjp.2018.31.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De La Coba P., Bruehl S., Garber J., Smith C. A., Walker L. S. Is resolution of chronic pain associated with changes in blood pressure-related hypoalgesia? Annals of Behavioral Medicine. 2018;52(7):552–559. doi: 10.1093/abm/kax021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bossola M., Pepe G., Vulpio C. Fatigue in kidney transplant recipients. Clinical Transplantation. 2016;30(11):1387–1393. doi: 10.1111/ctr.12846. [DOI] [PubMed] [Google Scholar]
- 15.Goedendorp M. M., Hoitsma A. J., Bloot L., Bleijenberg G., Knoop H. Severe fatigue after kidney transplantation: a highly prevalent, disabling and multifactorial symptom. Transplant International. 2013;26(10):1007–1015. doi: 10.1111/tri.12166. [DOI] [PubMed] [Google Scholar]
- 16.Ying H., Olorundare I., Desai N., et al. Changes in fatigue after kidney transplantation. American Journal of Transplantation. 2016;16 [Google Scholar]
- 17.Ronai K. Z., Szentkiralyi A., Lazar A. S., et al. Association of symptoms of insomnia and sleep parameters among kidney transplant recipients. Journal of Psychosomatic Research. 2017;99:95–104. doi: 10.1016/j.jpsychores.2017.05.019. https://linkinghub.elsevier.com/retrieve/pii/S0022399917301149. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigue J. R., Mandelbrot D. A., Hanto D. W., Johnson S. R., Karp S. J., Pavlakis M. A cross-sectional study of fatigue and sleep quality before and after kidney transplantation. Clinical Transplantation. 2011;25(1):13–21. doi: 10.1111/j.1399-0012.2010.01326.x. [DOI] [PubMed] [Google Scholar]
- 19.Markell M. S., Terebelo S. Complementary medicine use, symptom burden and non-adherence in kidney transplant recipients. Explore. 2018;14(6):414–419. doi: 10.1016/j.explore.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Nasiri K., Eyvanbagha R., Nazari N. Physiological and therapeutic effects of reflexology in Iran : a systematic review. Depiction of Health. 2016;7(1):49–61. http://dohweb.tbzmed.ac.ir. [Google Scholar]
- 21.Jones J., Thomson P., Irvine K., Leslie S. J. Is there a specific hemodynamic effect in reflexology? A systematic review of randomized controlled trials. The Journal of Alternative and Complementary Medicine. 2013;19(4):319–328. doi: 10.1089/acm.2011.0854. [DOI] [PubMed] [Google Scholar]
- 22.Hudson B. F., Davidson J., Whiteley M. S. The impact of hand reflexology on pain, anxiety and satisfaction during minimally invasive surgery under local anaesthetic: a randomised controlled trial. International Journal of Nursing Studies. 2014;52(12):1789–1797. doi: 10.1016/j.ijnurstu.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Rosinta U., Modjo R. The effect of progressive muscle relaxation in reducing fatigue among nurses in mental hospital. Indian Journal of Public Health Research & Development. 2019;10(2):p. 289. doi: 10.5958/0976-5506.2019.00303.6. [DOI] [Google Scholar]
- 24.Demiralp M., Oflaz F., Komurcu S. Effects of relaxation training on sleep quality and fatigue in patients with breast cancer undergoing adjuvant chemotherapy. Journal of Clinical Nursing. 2010;19(7-8):1073–1083. doi: 10.1111/j.1365-2702.2009.03037.x. [DOI] [PubMed] [Google Scholar]
- 25.Alparslan G. B., Orsal Ö., Unsal A. Assessment of sleep quality and effects of relaxation exercise on sleep quality in patients hospitalized in internal medicine services in a university hospital. Holistic Nursing Practice. 2016;30(3):155–165. doi: 10.1097/hnp.0000000000000147. http://www.ncbi.nlm.nih.gov/pubmed/27078810. [DOI] [PubMed] [Google Scholar]
- 26.Kheyri A., Bastani F., Haghani H. Effects of reflexology on sleep quality of elderly women undergoing abdominal surgery. Journal of Client-Centered Nursing Care. 2016;30:11–18. doi: 10.32598/jccnc.2.1.11. http://jccnc.iums.ac.ir/article-1-80-en.html. [DOI] [Google Scholar]
- 27.Roshanravan M., Jouybari L., Bahrami Taghanaki H., Vakili M., Sanagoo A., Amini Z. Effect of foot reflexology on fatigue in patients undergoing hemodialysis: a sham-controlled randomized trial. Journal of Mazandaran University of Medical-Sciences. 2016;26(137):32–41. http://jmums.mazums.ac.ir/article-1-7701-en.html. [Google Scholar]
- 28.Farrokhian R., Soleimani M.-A., Sheikhi M. R., Alipour M. Effect of foot reflexology massage on sleep quality in hemodialysis patients: a randomized control trial. Scientific Journal of Hamedan Nursing and Midwifery Faculty. 2017;24(4):213–220. doi: 10.21859/nmj-24041. http://nmj.umsha.ac.ir/article-1-1575-en.html. [DOI] [Google Scholar]
- 29.Bhagya S. R., Hepsi N., Nageshwar V. Foot reflexology: effect on pain and anxiety in post-operative patient. International Education & Research Journal. 2017;3(5):49–51. [Google Scholar]
- 30.Sahbaee F., Abedini S., Ghandehari H., Zare M. The effect of foot Reflexology Massage on pain of scoliosis patients undergoing spinal surgery. Anesthesiology and Pain. 2015;5(4):63–71. [Google Scholar]
- 31.Dikmen H. A., Terzioglu F. Effects of reflexology and progressive muscle relaxation on pain, fatigue, and quality of life during chemotherapy in gynecologic cancer patients. Pain Management Nursing. 2019;20(1):47–53. doi: 10.1016/j.pmn.2018.03.001. https://linkinghub.elsevier.com/retrieve/pii/S1524904217306112. [DOI] [PubMed] [Google Scholar]
- 32.Ucuzal M., Kanan N. Foot massage: effectiveness on postoperative pain in breast surgery patients. Pain Management Nursing. 2014;15(2):458–465. doi: 10.1016/j.pmn.2012.03.001. https://linkinghub.elsevier.com/retrieve/pii/S1524904212000380. [DOI] [PubMed] [Google Scholar]
- 33.Özdemir G., Ovayolu N., Ovayolu Ö. The effect of reflexology applied on haemodialysis patients with fatigue, pain and cramps. International Journal of Nursing Practice. 2013;19(3):265–273. doi: 10.1111/ijn.12066. [DOI] [PubMed] [Google Scholar]
- 34.Hesami M., Kalhor M., Roshani D., Fathi M. The effect of reflexology on fatigue in cancer patients receiving chemotherapy. Crescent Journal of Medical and Biological Sciences. 2019;6(2):151–157. https://www.cochranelibrary.com/central/doi/10.1002/central/CN-01817643/full. [Google Scholar]
- 35.Asltoghiri M., Ghodsi Z. The effects of Reflexology on sleep disorder in menopausal women. Procedia-Social and Behavioral Sciences. 2012;31:242–246. doi: 10.1016/j.sbspro.2011.12.049. https://linkinghub.elsevier.com/retrieve/pii/S1877042811029788. [DOI] [Google Scholar]
- 36.Lee J., Han M., Chung Y., Kim J., Choi J. Effects of foot reflexology on fatigue, sleep and pain: a systematic review and meta-analysis. Journal of Korean Academy of Nursing. 2011;41(6):p. 821. doi: 10.4040/jkan.2011.41.6.821. http://synapse.koreamed.org/DOIx.php?id=10.4040/jkan.2011.41.6.821. [DOI] [PubMed] [Google Scholar]
- 37.Yeung W.-F., Chung K.-F., Poon M. M.-K., et al. Acupressure, reflexology, and auricular acupressure for insomnia: a systematic review of randomized controlled trials. Sleep Medicine. 2012;13(8):971–984. doi: 10.1016/j.sleep.2012.06.003. https://linkinghub.elsevier.com/retrieve/pii/S1389945712002572%2038. [DOI] [PubMed] [Google Scholar]
- 38.Hjollund N. H., Andersen J. H., Bech P. Assessment of fatigue in chronic disease: a bibliographic study of fatigue measurement scales. Health and Quality of Life Outcomes. 2007;5((12)):1–5. doi: 10.1016/j.sleep.2012.06.003. https://hqlo.biomedcentral.com/articles/10.1186/1477-7525-5-12#Tab1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carlsson A. M. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16(1):87–101. doi: 10.1016/0304-3959(83)90088-x. [DOI] [PubMed] [Google Scholar]
- 40.Nazemizadeh M., Jalalodini A., Rezvani M., Yosefian N., Pournamdar Z., Ghalge M. The effect of foot reflexology massage on pain intensity in patients with chronic low back pain visited to physical therapy unit in baghiathallah hospital in tehran. Complementary Medicine Journal of Faculty of Nursing & Midwifery. 2012;2(3):1–8. https://www.sid.ir/En/Journal/ViewPaper.aspx?ID=334946. [Google Scholar]
- 41.Snyder-Halpern R., Verran J. A. Instrumentation to describe subjective sleep characteristics in healthy subjects. Research in Nursing & Health. 1987;10(3):155–163. doi: 10.1002/nur.4770100307. http://www.ncbi.nlm.nih.gov/pubmed/3647537. [DOI] [PubMed] [Google Scholar]
- 42.Mashayekhi F., Mirzai Saifabad R., Baghery P. Validity and reliability of the verran and snyder-halpern sleep scale in Iranian population. Journal of Mazandaran University Medical Scinces. 2016;25(132):200–209. http://jmums.mazums.ac.ir/article-1-6794-fa.html, URL: [Google Scholar]
- 43.Yılar Erkek Z., Aktas S. The effect of foot reflexology on the anxiety levels of women in labor. The Journal of Alternative and Complementary Medicine. 2018;24(4):352–360. doi: 10.1089/acm.2017.0263. [DOI] [PubMed] [Google Scholar]
- 44.Imani N., Shams S. A., Radfar M., Ghavami H., Khalkhali H. R. Effect of applying reflexology massage on nitroglycerin-induced migraine-type headache:a placebo-controlled clinical trial. Agri : Agri (Algoloji) Dernegi’nin Yayin Organidir = The Journal of the Turkish Society of Algology. 2018;30(3):116–122. doi: 10.5505/agri.2018.43815. [DOI] [PubMed] [Google Scholar]
- 45.Embong N. H., Soh Y. C., Ming L. C., Wong T. W. Revisiting reflexology: concept, evidence, current practice, and practitioner training. Journal of Traditional and Complementary Medicine. 2015;5(4):197–206. doi: 10.1016/j.jtcme.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yoosefian Miandoab N., Ezzati Z., Arbabi F., Manoochehri H., Zayeri F. The effect of reflexotherapy on chemotherapy-induced vomiting of patients. Advances in Nursing & Midwifery. 2012;22(76):60–80. [Google Scholar]
- 47.Wyatt G., Sikorskii A., Tesnjak I., et al. A randomized clinical trial of caregiver-delivered reflexology for symptom management during breast cancer treatment. Journal of Pain and Symptom Management. 2017;54(5):670–679. doi: 10.1016/j.jpainsymman.2017.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Özdelikara A., Tan M. The effect of reflexology on chemotherapy-induced nausea, vomiting, and fatigue in breast cancer patients. Asia-Pacific Journal of Oncology Nursing. 2017;4(3):p. 241. doi: 10.4103/apjon.apjon_15_17. http://www.apjon.org/text.asp?2017/4/3/241/207724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Öztürk R., Sevil Ü., Sargin A., Yücebilgin M. S. The effects of reflexology on anxiety and pain in patients after abdominal hysterectomy: a randomised controlled trial. Complementary Therapies in Medicine. 2018;36:107–112. doi: 10.1016/j.ctim.2017.12.005. https://linkinghub.elsevier.com/retrieve/pii/S0965229917305010. [DOI] [PubMed] [Google Scholar]
- 50.Rahimi Zarchi A., Hosseini M. A., Khankeh H. R., Salman Roghani R., Biglarian A. Evaluation of the effect of reflexology massage on pain severity after abdominal surgery. Medical-Surgical Nursing Journal. 2016;5(3):7–12. [Google Scholar]
- 51.Silverdale N., Wherry M., Roodhouse A. Massage and reflexology for post-operative cancer cystectomy patients: evaluation of a pilot service. Complementary Therapies in Clinical Practice. 2019;34:109–112. doi: 10.1016/j.ctcp.2018.11.010. https://linkinghub.elsevier.com/retrieve/pii/S1744388118304316. [DOI] [PubMed] [Google Scholar]
- 52.Mohammad Aliha J., Behroozi N., Peyrovi H., Mehran A. The effect of foot reflexology massage on incisional pain in abdominal and chest surgery patients admitted to intensive care unit. Iranian Journal of Cardiovascular Nursing. 2013;2(2):6–12. http://journal.icns.org.ir/article-1-172-en.html. [Google Scholar]
- 53.Shahriari M., Khalili A., Shamsizadeh M., Mardani D., Paymard A., Molavi Vardanjani M. Effects of foot reflexology on pain in patients after lower limb amputation. Journal of Mazandaran-University of Medical Sciences. 2016 Aug 1;26(139):18–26. http://jmums.mazums.ac.ir/article-1-8151-en.html. [Google Scholar]
- 54.Koraş K., Karabulut N. The effect of foot massage on postoperative pain and anxiety levels in laparoscopic cholecystectomy surgery: a randomized controlled experimental study. Journal of Perianesthesia Nursing : Official Journal of the American Society of PeriAnesthesia Nurses. 2019;34(3):551–558. doi: 10.1016/j.jopan.2018.07.006. https://linkinghub.elsevier.com/retrieve/pii/S1089947218302983. [DOI] [PubMed] [Google Scholar]
- 55.Mohammadi S., Pouladi S., Ostovar A., Ravanipour M. Effects of foot reflexology massage on pain and fatigue in patients undergoing coronary artery bypass graft. ATMPH. 2018;8(518) [Google Scholar]
- 56.Rigi F., Shahnavazi M., Feizi A., Adineh H., Malekraisi noushirvan S. The effect of reflexology massage on the fatigue severity in women with multiple sclerosis. UNMF. 2017;14(11):926–933. http://unmf.umsu.ac.ir/article-1-2989-en.html. [Google Scholar]
- 57.Unal K. S., Balci Akpinar R. The effect of foot reflexology and back massage on hemodialysis patients’ fatigue and sleep quality. Complementary Therapies in Clinical Practice. 2016;24:139–144. doi: 10.1016/j.ctcp.2016.06.004. https://linkinghub.elsevier.com/retrieve/pii/S1744388116300494. [DOI] [PubMed] [Google Scholar]
- 58.Abbasi Fakhravari A., Bastani F., Haghani H. The effect of foot reflexology massage on the sleep quality of elderly women with restless leg syndrome. Journal of Client-Centered Nursing Care. 2018;4(2):96–103. doi: 10.32598/jccnc.4.2.96. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


