Abstract
Background and Aims:
Removal of gastric button batteries (BBs) remains controversial. Our aim was to better define the spectrum of injury and to characterize clinical factors associated with injury from retained gastric BBs.
Methods:
Multicenter retrospective cohort study from January 2014 through May 2018. Pediatric gastroenterologists from 4 pediatric tertiary care centers identified patients, aged 0 to 18 years, who had a retained gastric BB on radiography and subsequently underwent endoscopic assessment. Demographic and clinical information were abstracted from electronic health records using a standard data collection form.
Results:
Sixty-eight patients with a median age of 2.5 years underwent endoscopic retrieval of a gastric BB. At presentation, 17 (25%) were symptomatic. Duration from ingestion to endoscopic removal was known for 65 patients (median [IQR]: 9 hours [5–19 hours]). Median time from ingestion to first radiographic evaluation was 2 hours. At endoscopic removal, 60% of cases had visual evidence of mucosal damage, which correlated with duration of BB retention (p=0.0018). Time to retrieval of the BB was not statistically significant between symptomatic and asymptomatic subjects (p=0.12). After adjusting for age and symptoms, the likelihood of visualizing gastric damage among patients who had BBs removed after 12 postingestion hours was 4.5 times that compared with those with BB removal within 12 hours of ingestion.
Conclusions:
In this study, swallowed BBs posed a risk of damage to the stomach, including a single case of impaction and perforation of the gastric wall. Clinicians may want to consider retrieval within 12 hours of ingestion of gastric BBs. Larger prospective studies to assess risk of injury are needed.
Introduction
Button battery ingestions (BBIs) are associated with significant morbidity and mortality in the pediatric population. Ingested button batteries (BBs) lodged in the upper airway or esophagus can cause significant harm including tracheoesophageal fistulas1, aortoesophageal fistulas,2,3 and death2. When lodged in the esophagus, tissue damage, which is the result of isothermic hydrolysis leading to tissue necrosis, can be noted within as little as 2 hours4,5. Per expert consensus and National Capital Poison Center guidelines, prompt evaluation and management of these ingestions is universally recommended2,6.Although BBIs are typically thought of as threatening to the esophagus and surrounding structures including the trachea and aorta, few case reports and studies have described gastric damage from BBIs. Gastric BBs are generally thought to be less damaging due to the larger stomach size, increased thickness, and decreased number of closely associated anatomic structures. Timing, urgency, and indication for removal of a BB beyond the lower esophageal sphincter have been controversial.
There is no universal recommendation for retained BBs beyond the lower esophageal sphincter, specifically in the stomach. A clinical report from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) recommends emergent removal of all esophageal BBs. However, per this report, removal of a gastric BB remains controversial and is left at the discretion of the treating physician. Observation alone is recommended for cases in which gastric BBIs present within 2 hours, if the battery is ≤20 mm, and when the child is ≥5 years of age6. The National Capital Poison Center has a published algorithm most recently revised in June 2018, which recommends observation alone for asymptomatic gastric BBIs regardless of the age of the patient or size of the battery. If the battery is ≤12 mm or the patient is >12 years of age, the patient can be managed at home and BB passage should be confirmed in the stool. Imaging can be repeated in 10 to 14 days if confirmation cannot be made. If patients become symptomatic later, then prompt endoscopic removal is recommended, even if symptoms are minor, unless it is beyond the reach of an endoscope, in which case surgical removal should be performed. If the battery is ≥15 mm and the child is <6 years old, then a repeat radiograph should be done 4 days after ingestion (sooner if symptomatic) and removed endoscopically4,7,8. In the United States, data from the Poison Control Center show that the incidence of moderate to severe morbidity and mortality from BBIs is on the rise8 Recent data evaluating foreign body ingestions of children treated in the United States from 1995 to 2015 reveal a 150-fold increase in rate of ingestion of batteries during the study period9. Of these battery ingestions, 85.9% were BBs. An increased incidence of fatality and debilitating injury secondary to BBI is likely due to the advent and increased use of inexpensive, high-voltage lithium batteries as power sources in electronics, toys, and commonly used household products4.
In this study, we describe a series of pediatric BBIs with gastric retention and subsequent removal or attempted removal after radiographic imaging revealing BB retention in the stomach. Through this data set from a large multicenter collaboration, we aim to better define the spectrum of injury associated with retained gastric BB and characterize clinical factors associated with gastric injury in BBI. We hypothesize that gastric BBIs do lead to gastric injury more than previously understood, which potentially can have an impact on future management of gastric BBIs.
Patients and Methods
We performed a multicenter retrospective study at 4 tertiary care centers from January 2014 through May 2018 with Institutional Review Board approval from each individual site. This time frame was determined based on the availability of electronic medical records at all the participating institutions. Chart review identified cases of endoscopic removal of gastric BBs in patients between 0 and 18 years of age. Cases were identified from the following tertiary care institutions: Children’s Hospital of Colorado (Aurora, Colorado, USA), Cincinnati Children’s Hospital Medical Center (Cincinnati, Ohio, USA), Johns Hopkins All Children’s Hospital Florida (St. Petersburg, Florida, USA) and Texas Children’s Hospital (Houston, Texas, USA). Study sites are all large referral centers with high capacity ranging from 250 to 800 pediatric beds. These sites were selected based on prior collaborative efforts. Patients were initially identified based on diagnosis codes and then further selected via chart review by gastroenterologists at participating institutions. Patients were included if they had a retained gastric BB on radiographic imaging and subsequently underwent endoscopic assessment by either pediatric gastroenterologists or surgeons at the participating institutions. To minimize selection bias, all cases discovered during chart review were included; no cases were excluded. Electronic Health Records (EHRs) and EHR-generated trauma databases were queried for pertinent real-language terms, CPT codes, or diagnosis codes to identify all patients, depending on the institution. Cases were subsequently confirmed by chart review. Demographic and clinical information were abstracted from electronic health records using a standard data collection form. Data gathered included age, sex, weight, comorbidities, and presenting symptoms at the time of evaluation. Data on timing of imaging studies and time to BB extraction as well as modality of extraction were also reported. Type and size of the battery were included in the data collection form along with analysis of adverse events after BB removal. Battery sizes were estimated based upon measurements of batteries after endoscopic retrieval if available; otherwise, they were estimated from measurements on radiographs.
Continuous variables were summarized using median and range or interquartile range (IQR) and compared between children with and those without gastric damage using the Wilcoxon Rank sum test. Categorical variables were summarized using percentage and compared between the groups using the Chi square test for association. To further explore factors associated with gastric damage, logistic regression analysis was conducted where time-to-endoscopy intervention and age of patient were treated either as continuous or dichotomous variables. Candidate factors entered into the multivariate analysis were determined based on their P valuesfrom univariate analysis (ie, P < .15) and clinical relevance. Backward selection method was used to determine the best multiple regression model with P < .05 as criterion for a predictor to stay in the final model. The P values for the univariate statistical tests are not corrected for multiple testing because those tests were taken as exploratory. The subsequent multivariable logistic regression analysis was considered the main definitive result as it determined those variables independently associated with the occurrence of gastric injury after adjusting for the contributions of the other variables in the model. Other statistical results are secondary, to be taken as descriptive only, and not requiring correction of their P values for multiple testing. As sensitivity analysis, institution as the dummy variable was adjusted in the above mention logistic regression analysis where Firth-type penalized likelihood was used. These sensitivity analyses produced consistent results with those analyses not adjusted for institution effect. A 2-tailed distribution with P < .05 was considered statistically significant. SAS 9.4 (SAS Institute Inc, Cary, NC, USA) was used for analysis.
Results
We identified 68 patients from 4 participating institutions who underwent endoscopic retrieval of gastric BBs (Table 1). Of these, 42 (65%) were male with a median age of 2.5 years (range 8 months to 16 years). Twenty-one (31%) had initial evaluation at an outlying facility before referral to 1 of the 4 tertiary care centers partaking in the study. Specifically, 27 cases were treated at Cincinnati Children’s Hospital, 26 at Texas Children’s Hospital, 8 at Children’s Hospital Colorado, and 7 at Johns Hopkins All Children’s Hospital (Table 2). Fifteen patients had at least one medical comorbidity, which are outlined in Table 1; the remaining 53 patients had no other reported medical history. At the time of presentation, 17 out of 68 (25%) were symptomatic. Symptoms were varied and are outlined in Table 1.
Table 1:
Patient characteristics across all sites
| Patient characteristics | Overall | Mucosal injury n=41 | No mucosal injury n=27 | P value | |
|---|---|---|---|---|---|
| Male, n (%) | 44 (65) | 26 (63) | 18 (67) | .78 | |
| Median age in years (range) | 2.5 (1–16) | 2.0 (0.7–11.0) | 4.0 (0.8–16) | .033 | |
| Age 5 year or older, n (%) | 22 (32) | 9 (22) | 13 (48) | .024 | |
| Median weight in Kg (range) | 15.2 (8–9) | 13.8 (8.0–56.4) | 19.4 (9.7–59.4) | .05 | |
| Comorbidities, n (%) | .23 | ||||
| ADHD*/Behavioral problems | 6 (8.9) | 3 (7.3) | 3 (11.1) | ||
| Seizure disorders | 2 (2.9) | 2 (4.9) | |||
| Anxiety and depression | 1 (1.5) | 1 (3.4) | |||
| Genetic abnormalities | 2 (2.9) | 1 (2.4) | 1 (3.4) | ||
| Asthma | 1 (1.5) | 1 (2.4) | |||
| Congenital hearing loss | 1 (1.5) | 1 (3.4) | |||
| Developmental delay | 1 (1.5) | 1 (3.4) | |||
| Food allergies | 1 (1.5) | 1 (3.4) | |||
| Iron deficiency anemia | 1 (1.5) | 1 (2.4) | |||
| Gastroesophageal reflux | 1 (1.5) | 1 (3.4) | |||
| Any syptoms, n (%) | 17 (25) | 13 (31.7) | 4 (14.8) | .12 | |
| Specific symptoms, n (%) | 18 (26.5) | 14 (34.1) | 4 (14.8) | .36 | |
| Abdominal pain | 7 (10.3) | 4 (9.8) | 3 (11.1) | ||
| Oropharyngeal symptoms | 4 (5.8) | 3 (7.3) | 1 (3.4) | ||
| Emesis, spit ups | 4 (5.8) | 4 (9.8) | |||
| Chest or back pain | 3 (4.4) | 3 (7.3) | |||
| Radiography | n (%) | Median hours (range) | n (%) | n (%) | |
| First | 62 (91.2) | 2.0 (1 to 27) | 36 (85.4) | 26 (96.3) | |
| Second | 40 (58.8) | 7.4 (3 to 113) | 30 (73.2) | 10 (37) | |
| Third | 11 (16.2) | 13 (5 to 42) | 8 (19.5) | 3 (14.3) | |
| Mean battery size in cm (SD) | 1.7 (0.5) | 1.6 (0.6) | 1.7 (0.5) | .37 | |
| Battery size ≥2 cm, n (%) | 18 (26.5) | 11 (26.8) | 7 (25.9) | .93 |
ADHD= attention deficit hyperactivity disorder
Table 2:
Patient characteristics by individual site
| Variable Name | Category | Texas Children’s Hospital | Cincinati Children’s Hospital | Johns Hopkins All Children’s Hospital | Children’s Hospital Colorado | P value |
|---|---|---|---|---|---|---|
| Counts (%) | ||||||
| Gastric damage | No | 10 (38.5%) | 15 (55.6%) | 2 (28.6%) | ||
| Yes | 16 (61.5%) | 12 (44.4%) | 5 (71.4%) | 8 (100%) | .029 | |
| Gender | F | 9 (34.6%) | 8 (29.6%) | 4 (57.1%) | 3 (37.5%) | |
| M | 17 (65.4%) | 19 (70.4%) | 3 (42.9%) | 5 (62.5%) | .639 | |
| Age 5 years or older | < 5 years | 20 (76.9%) | 15 (55.6%) | 5 (71.4%) | 6 (75.0%) | |
| ≥ 5 years | 6 (23.1%) | 12 (44.4%) | 2 (28.6%) | 2 (25.0%) | .401 | |
| Symptoms (None vs Yes) | Y | 6 (23.1%) | 5 (18.5%) | 2 (28.6%) | 4 (50.0%) | |
| N | 20 (76.9%) | 22 (81.5%) | 5 (71.4%) | 4 (50.0%) | .347 | |
| Battery size | ≤ 2 cm | 17 (65.4%) | 23 (85.2%) | 7 (100%) | 3 (37.5%) | |
| > 2 cm | 9 (34.6%) | 4 (14.8%) | 5 (62.5%) | .014 | ||
| Timing of imaging (hours) | > 2 hours | 11 (50.0%) | 12 (48.0%) | 6 (85.7%) | 1 (12.5%) | |
| Within 2 hours | 11 (50.0%) | 13 (52.0%) | 1 (14.3%) | 7 (87.5%) | .048 | |
| Timing of edoscopy (hours) | > 12 hours | 13 (54.2%) | 6 (23.1%) | 6 (85.7%) | 4 (50.0%) | |
| Within 12 hours | 11 (45.8%) | 20 (76.9%) | 1 (14.3%) | 4 (50.0%) | .012 | |
| Median (IQR) | ||||||
| Age (years) | 2.5 (1.0 – 4.0) | 2.0 (1.0 – 5.4) | 4.0 (1.7 – 7.0) | 2.3 (0.8 – 5.0) | .363 | |
| Weight (Kg) | 15.9 (10.9 – 22.0) | 12.5 (9.5 – 20.4) | 17.1 (12.0 – 25.3) | 12.2 (9.8 – 22.0) | .337 | |
| Size of battery in cm | 2.0 (1.3 – 2.1) | 2.2 (1.6 – 2.5) | 1.3 (1.0 – 1.5) | 1.9 (1.1 – 2.0) | .031 | |
| Hours from ingestion to removal | 14.6 (4.4 – 21.8) | 12.0 (6.5 – 20.5) | 5.9 (5.0 – 12.0) | 15.0 (13.5 – 21.0) | .14 | |
| Hours from ingestion at 1st xray | 2.1 (1.8 – 3.5) | 1.5 (1.0 – 2.0) | 2.0 (1.5 – 4.0) | 3.0 (2.5 – 6.0) | .095 | |
| Hours from ingestion at 2nd xray | 7.3 (5.5 – 12.8) | 5.0 (4.0 – 7.0) | 11.5 (6.5 – 12.8) | 12.5 (11.0 – 19.0) | .224 | |
| Length of stay | 4.5 (4.0 – 15.0) | 14.0 (5.0 – 17.0) | 0.0 (0.0 – 0.0) | 16.0 (12.0 – 16.0) | <.001 | |
Fisher exact test for categorical variables and Krusgal-Wallis test for continuous variables.
Duration from ingestion to endoscopic removal was estimated from historical information and endoscopy documentation in the electronic health record for 65 of the patients with known ingestion time (median [IQR]: 9 hours [5–19 hours], range 3–117 hours). Median time to first radiographic study was available for 62 patients and was 2 hours (range 1–27 hours) from ingestion. Of these, 25 patients (37%) had primary imaging performed at an outlying institution. A second set of radiographs was performed in 40 out of 68 cases (59%) at a median time of 7.4 hours (range 3–113 hours) from time of ingestion. A smaller number of patients had 3 to 5 sets of radiographs before endoscopy (Table 1). In one case, initial radiologic interpretation localized the BB in the small intestine, but repeat imaging and endoscopic evaluation confirmed erosion into and perforation of the gastric wall.
At the time of endoscopic removal, 41 out of 68 (60%) cases had reported visible gastric mucosal damage and 27 cases (40%) did not have visible gastric injury (Fig. 1). Duration of ingestion before removal of BBs was assessed for patients with and without gastric injury (median [IQR]: 14.75 [14.75] and 5.25 [6] hours, respectively, P = .003). Endoscopic mucosal injuries varied in severity and were described as ulcerations, necrosis, abrasions, gastric erythema, mucosal friability, and erosions at the site of the BB in the stomach. In 12 patients (18%) the batteries had cleared the stomach and the proximal duodenum by the time of endoscopic evaluation and thus were not removed. Of these patients, one patient had battery retention at the ileocolic region, which required removal via colonoscopy. Two (17%) of these patients had gastric mucosal injury at the time of endoscopy. The remainder of these patients had no known or documented adverse events. Of the 17 patients who were symptomatic at the time of presentation, 13 (76%) had gastric mucosal damage at the time of endoscopy. Twenty-eight out of 51 asymptomatic subjects (55%) at the time of presentation had visible damage. Median time to retrieval of BBs did not differ between symptomatic and asymptomatic subjects (12.75 [IQR 10.5] hours vs 7 [IQR 15.25] hours, P = .70).
Figure 1: Endoscopic images of patients with gastric button batteries pre and post endoscopic removal.

The upper panels reveal button batteries lodged in the antropyloric region in four separate patients. There are notable erosions, erythema and necrosis surrounding the button batteries in these images. The bottom four panels show the corresponding images following battery removal. Linear erosions, erythema, bleeding, edema and necrosis at the site of prior battery adhesion are seen in these images.
Logistic regression was used to explore factors that are associated with the gastric damage at the time of endoscopy. Univariate analysis revealed that age as a continuous variable was not significant (P = .0527) (Table 3); however, patients younger than 5 years of age had significantly lower likelihood of having gastric damage (OR, 0.3; P = .03) as compared with children of 5 years or older. When time from ingestion to endoscopy was treated as a continuous variable in the model, it was not significant (OR, 1.03; P = .22). However, when this predictor was dichotomized into less than 12 hours or longer than 12 hours, the binary predictor was very significant in the model (P = .006). The cutoff of 12 hours was selected based on likely timing of intervention and classification of urgent versus not urgent procedures. This observation in our patient population indicates that those who had BBs removed after 12 hours were 4.5 times more likely to have gastric damage than those whose BB was removed before 12 hours.
Table 3:
Univariate and multivariatelogistic regression analysis of gastric damage
| Univariate analysis | Multivariate analysis | ||||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | ||||||
| Predictor | Odds ratio description | Odds Ratio (95% CI) | P Value | Adj odds ratio (95% CI) | P Value | Adj odds ratio (95% CI) | P Value |
| Age (years) | Per 1 year older | 0.85 (0.72 – 1) | .0527 | 0.83 (0.68 – 1.01) | .0639 | ||
| Age 5 years or older | ≥5 years vs <5 years | 0.3 (0.11 – 0.87) | .0268 | 0.28 (0.08 – 0.93) | .0381* | ||
| Weight (kg) | Per 1 kg increase | 0.97 (0.92 – 1.01) | .1211 | ||||
| Size of battery (cm)-continuous | Per 1 cm increase | 1.52 (0.61 – 3.8) | .3674 | ||||
| Size of battery (cm)-dichotomous | ≤2 cm vs >2 cm | 0.96 (0.32 – 2.88) | .9343 | ||||
| Time from ingestion to removal (hours) | Per 1 hour longer | 1.03 (0.99 – 1.07) | .2229 | ||||
| Gender | F vs M | 1.15 (0.42 – 3.21) | .7837 | ||||
| Symptoms | None vs Yes | 0.38 (0.11 – 1.31) | .1234 | 0.29 (0.07 – 1.3) | .105 | 0.31 (0.07 – 1.35) | .118 |
| Timing of imaging (hours) | >2 hours vs within 2 hours | 1.52 (0.55 – 4.21) | .4166 | ||||
| Timing of endoscopy (hours) | >12 hours vs within 12 hours | 4.79 (1.57 – 14.59) | .006* | 4.54 (1.42 – 14.52) | .0108* | 4.44 (1.38 – 14.34) | .0127* |
P < .05
A multiple logistic regression analysis was then conducted with age, symptom at time of presentation, and endoscopic removal within 12 hours as candidate predictors (Table 3). Age was treated as either continuous or dichotomous predictors in separate analyses. In either model, age was a significant factor in the multivariate model; removal within 12 hours was the most significant (P = .01), whereas symptoms at time of presentation was not significant (P = .12). When backward selection was applied to these 2 models, removal within 12 hours was the only factor in the final model.
A severe adverse event of a retained lodged 2-cm battery in the antrum was reported in a 9-year-old patient who developed gastric perforation with pneumoperitoneum. Estimated time of gastric BB retention in this case was 117 hours (Fig. 2). Pneumoperitoneum self-resolved after patient was hospitalized overnight for observation. Another patient underwent endoscopy within 5.25 hours of ingestion of a 0.9 cm battery but did not have successful removal of the BB because it had already cleared the upper intestinal tract. However, this patient had a colonoscopy 1 week later due to battery retention at the level of the ileocecal valve. Four patients (6%) with endoscopic mucosal injury were admitted overnight for observation but were then discharged with no further adverse events. The remainder of the subjects were discharged after the procedure. Notably, 1 patient with necrotic tissue at the level of the pylorus at the time of BB removal had repeat endoscopy, which did not show pyloric stenosis or stricture.
Figure 2:
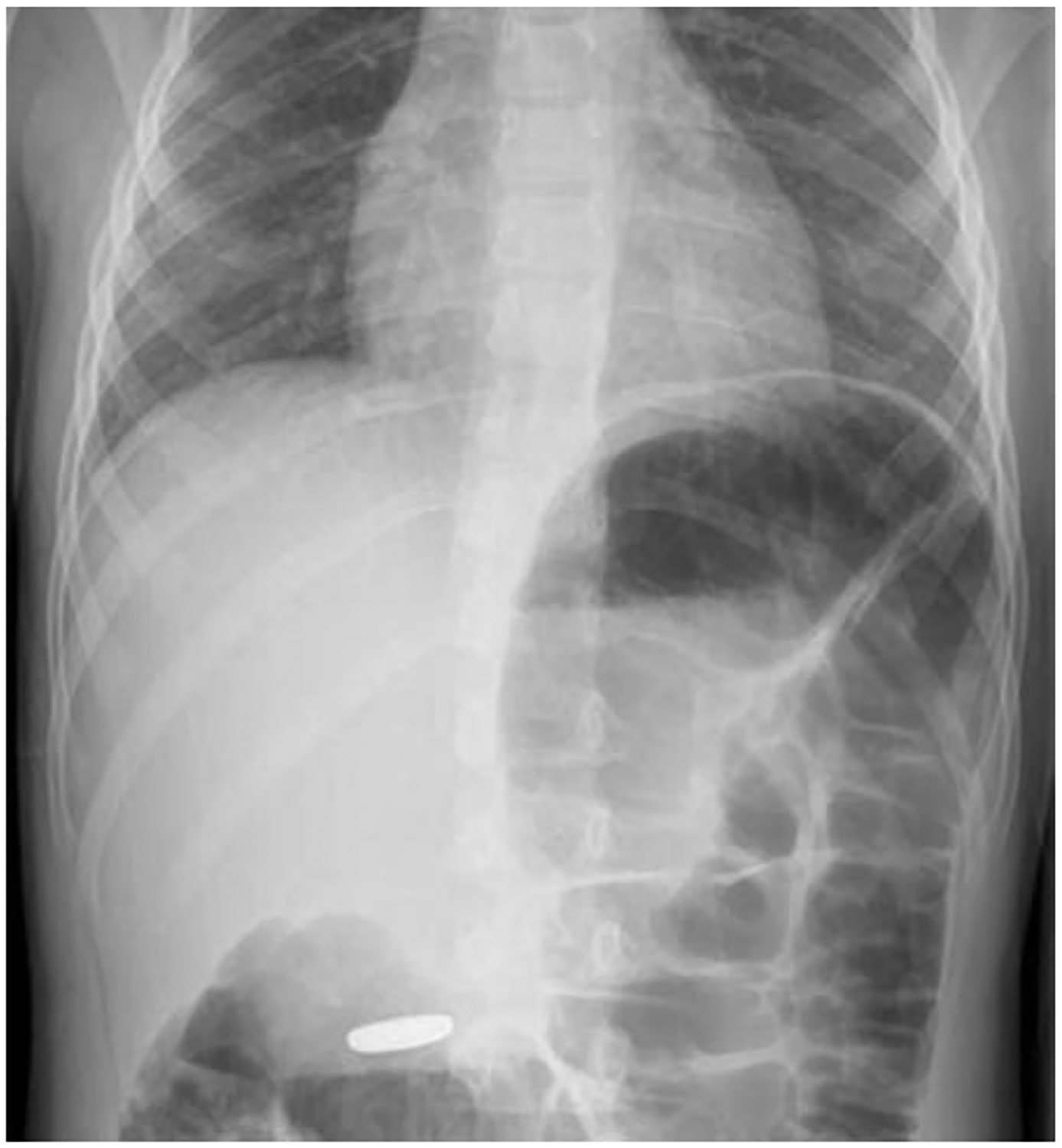

X-ray imaging of a patient’s retained gastric BBI that resulted in perforation. A, Foreign body in the antrum of the stomach interpreted as likely within the small bowel or colon by radiologist. Radiographic image obtained at 3 hours after ingestion. B, Radiography obtained 113 hours after ingestion showing retention and erosion of the button battery in the distal stomach.
In patients who underwent endoscopy, BBs were retrieved in 56 patients (82%). Of those, retrieval with a net was reported in 36 cases (64%), alligator forceps in 6 cases (11%), rat-tooth forceps in 4 cases (7%), and basket in 2 cases (4%). Six subjects (11%) required retrieval using a combination of instruments, and 4 cases (7%) did not describe the method of retrieval in the operative report.
The median diameter of ingested batteries was 1.67 cm (range 0.8–2.6cm). Among those with gastric injury, the median diameter was 1.9 cm (range 0.9 – 2.6), as opposed to a diameter of 1.4 cm (range 0.8–2.5) among those with no mucosal injury (P = .45). Eighteen patients ingested a BB greater or equal than 2 cm in diameter (26.5%). Of those, 11 had evidence of mucosal injury, and 7 did not have any visible mucosal injury (P = .93).
Discussion
This is the largest adult or pediatric case series investigating endoscopic findings and complications secondary to gastric retention of BBs to date. These data demonstrate that gastric retention of BBs poses a risk of serious injury. Prior published guidelines from the National Capital Poison Center, last revised in June of 2018, recommend immediate removal of a gastric BB only if coingested with a magnet or if the patient is symptomatic9. Otherwise, current guidelines from the Poison Control Center recommend repeating an imaging study 4 days after ingestion if the BB is ≥1.5 cm and the child is younger than 6 years9. The NASPGHAN Endoscopy Committee’s clinical recommendations, published in 2015, acknowledge the potential injury associated with gastric BBs and recommend removal within 48 hours only if the patient is symptomatic or electively if the BB remains static on repeat imaging studies6. Observation alone is recommended for cases in which the gastric BBI presents within 2 hours, the battery is ≤20 mm, and the child is ≥5 years of age6. This presents a dilemma to endoscopistsas: there is currently no clear single guideline in the management of gastric BBs. Our data are among the first to suggest that timely removal of gastric BBs is important.
In this case series, 60% of cases had gastric injury described at the time of endoscopic retrieval of the BB, and injury significantly correlated with duration of battery retention. Notably, 1 patient had substantial injury including gastric perforation and pneumoperitoneum. The presence of symptoms was not predictive of injury. In fact, the patient who sustained a severe adverse event had no symptoms at the time of endoscopic removal and presented for follow-up based on recommendations received at his initial emergency department visit. It is not known whether others with variable amounts of mucosal injury seen at the time of removal would have progressed to serious adverse events as a result of more prolonged gastric retention. Seventy-eight percent of symptomatic patients had visible erosive gastric damage, whereas 54% of the asymptomatic cohort at the time of presentation also had gastric mucosal damage. After adjusting for age and symptoms at time of presentation, the likelihood of visualizing gastric damage was 4.5 times higher among patients who had BBs removed after 12 hours following ingestion as compared with those with BB removal within 12 hours of ingestion. Our analysis suggests that early removal may prevent gastric injury, and symptoms are not sensitive for identifying damage. The difference in time to endoscopic removal between symptomatic and asymptomatic patients did not reach statistical significance. This is likely influenced by variation in institutions and provider to provider practice differences, which can be subject to institutional guidelines or prior experience with adverse events. For example, at Cincinnati Children’s Hospital, a local treatment algorithm suggests endoscopic removal within 24 to 48 hours for any gastric BB; however, the remainder of the participating centers in this study does not have local treatment algorithms for gastric BB.
Our data are consistent with and extend other published reports about injury secondary to gastric retention of BBs. A recent single-center retrospective study investigated BBI and reported 25 cases, of which 12 were located in the stomach. Rios et al10 advocated for extraction of button batteries from the stomach within 24 hours becaise they revealed that 50% of their patients with gastric BBs have visual mucosal damage, one of which had evidence of necrosis at the site of battery removal. In another series of 46 patients with BBIs, 13 had gastric BBs with a mean time of removal from the stomach of 27 hours11. This study identified endoscopic injury in 87.5% of children with BBs and subsequently recommend removal within 24 hours of ingestion if the BB was gastric in location. A third report by Lee et al12 urges prompt endoscopic removal even if the patient is asymptomatic and the battery is smaller than 2 cm in diameter. They report 5 cases with gastric button batteries with 3 having gastric adverse events, including mucosal ulceration and erosion. Numerous case reports have also been published describing injury to the gastric mucosa from BBs13–18. In a report of a BBI in a 3-month-old, a laparotomy was performed secondary to severe gastric wall injury due to battery adhesion to gastric mucosa after patient presented with significant emesis after BB retention for a speculated 48 hours14. In another account, an asymptomatic 18-month-old presented after known BBI and underwent emergent removal and was found to have multiple acute mucosal erosions in the stomach at the location of button battery contact despite intervention within 4 hours of ingestion15. In another report by Takagashi et al,16 a 3-month-old asymptomatic patient had ingestion of 3 cell batteries and, despite intervention within 48 hours, had adhesion of the button battery to the gastric wall requiring laparotomy.
These cases highlight the danger of gastric retention of BB, and they suggest that early intervention may be indicated; our case series is one of the largest to also support this. Our study reveals the wide practice variation in management of these ingestions across and within institutions, which is reflected by the wide range in timing from initial presentation to endoscopic removal of BBs (range 3–117 hours).
Our analysis suggests that early removal may prevent gastric injury, and symptoms are not sensitive for identifying damage. One case, in the current series, demonstrates that radiographic images can be misinterpreted, and numerous views may be needed to delineate the location of the foreign object. This patient initially had one lateral radiograph incorrectly interpreted by a radiologist as a BB distal to the stomach; however, follow-up images indicated a gastric location. A second case underscores the importance of follow-up imaging to ensure the passage of a BB. This patient had spontaneous passage of the BB at time of upper endoscopic evaluation; however, despite the small size of the BB (0.9 cm), the foreign body was retained at the ileocecal valve eventually requiring endoscopic removal.
As data in this study are solely collected from tertiary pediatric centers, there is likely a selection bias that may limit the generalizability of our data. Twenty-five (37%) of all included patients were initially assessed at outlying institutions before referral to one of the centers participating in this study. This pattern in referral may have led to some of the heterogeneity of duration from presentation to endoscopic intervention. Patients referred to other institutions that lack emergent endoscopic support may have been observed as opposed to undergoing endoscopic removal.
In this article, we did not have access to patients referred for a gastric BB and underwent observation alone. This is a limitation of this retrospective study because our databases track patients who underwent procedural interventions and do not track those who did not undergo upper endoscopy for a button battery.
Timely endoscopic removal of button batteries retained in the stomach may be considered based on this study because gastric injury in this cohort is common, there is poor correlation between symptoms and injury, and removal within 12 hours is associated with lower risk of injury. Early endoscopic removal regardless of the position of the battery at first presentation may prevent significant injury to the stomach despite lack of clinical symptoms.
Conclusion:
Although button battery injury is mainly thought of as harmful to the esophagus, the stomach may also be an anatomically susceptible region as demonstrated in this case series. Endoscopic removal within 12 hours of ingestion of gastric BBs may be considered regardless of symptoms or patient age. Gastric retention can offer risks of serious serosal injury and perforation. Imaging studies should be interpreted and carefully reviewed with an experienced radiologist in order to ascertain battery location within the intestinal tract. However, larger prospective studies aimed at understanding the risk of mucosal injury of gastric button batteries are needed.
Funding:
This work is partly supported by a Cystic Fibrosis Foundational Grant Award #Khalaf17B0 to RK, HAZLET15B0 and HAZLET18D0 to KH, National Institutes of Health Training Grant 5T32-DK067009-12 to KH and RK, National Institutes of Health Training Grant 5T32-DK7664-28 to WR, National Institutes of Health Training Grant NIH 5T32-DK0077-27 to SO, and Sondheimer Fellow Funds from Children’s Hospital Colorado.
Abbreviations:
- BB
Button battery
- BBI
button battery ingestion
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
COI: DSF is a paid contributor to UpToDate, “Caustic esophageal injury in children.”
Disclosures: Data from this manuscript has been presented previously at Digestive Disease Week and at the Annual Meeting for the North American Society for Pediatric Gastroenterology, Heaptology and Nutrition in the form of a poster.
References:
- 1.Ettyreddy AR, Georg MW, Chi DH, Gaines BA, Simons JP. Button battery injuries in the pediatric aerodigestive tract. Ear Nose Throat J. December 2015;94(12):486–493. [PubMed] [Google Scholar]
- 2.Leinwand K, Brumbaugh DE, Kramer RE. Button Battery Ingestion in Children: A Paradigm for Management of Severe Pediatric Foreign Body Ingestions. Gastrointest Endosc Clin N Am. January 2016;26(1):99–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brumbaugh DE, Colson SB, Sandoval JA, et al. Management of button battery-induced hemorrhage in children. J Pediatr Gastroenterol Nutr. May 2011;52(5):585–589. [DOI] [PubMed] [Google Scholar]
- 4.Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics. June 2010;125(6):1168–1177. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka J, Yamashita M, Yamashita M, Kajigaya H. Esophageal electrochemical burns due to button type lithium batteries in dogs. Veterinary and human toxicology. August 1998;40(4):193–196. [PubMed] [Google Scholar]
- 6.Kramer RE, Lerner DG, Lin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. Journal of pediatric gastroenterology and nutrition. April 2015;60(4):562–574. [DOI] [PubMed] [Google Scholar]
- 7.Litovitz T, Whitaker N, Clark L. Preventing battery ingestions: an analysis of 8648 cases. Pediatrics. June 2010;125(6):1178–1183. [DOI] [PubMed] [Google Scholar]
- 8.National Capital Poison Control Center. https://www.poison.org/battery/guideline. Accessed February 9. 2020, 2020.
- 9.Orsagh-Yentis D, McAdams RJ, Roberts KJ, McKenzie LB. Foreign-Body Ingestions of Young Children Treated in US Emergency Departments: 1995–2015. Pediatrics. May 2019;143(5). [DOI] [PubMed] [Google Scholar]
- 10.Rios G, Rodriguez L, Lucero Y, Miquel I, Arancibia ME, Alliende F. Endoscopic Findings Associated With Button Battery Ingestion in Children: Do We Need to Change the Protocol for Managing Gastric Location? Pediatric emergency care. January 23 2018. [DOI] [PubMed] [Google Scholar]
- 11.Al Lawati TT, Al Marhoobi RM. Timing of Button Battery Removal From the Upper Gastrointestinal System in Children. Pediatric emergency care. December 27 2018. [DOI] [PubMed] [Google Scholar]
- 12.Lee JH, Lee JH, Shim JO, Lee JH, Eun BL, Yoo KH. Foreign Body Ingestion in Children: Should Button Batteries in the Stomach Be Urgently Removed? Pediatr Gastroenterol Hepatol Nutr. March 2016;19(1):20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Temple DM, McNeese MC. Hazards of battery ingestion. Pediatrics. January 1983;71(1):100–103. [PubMed] [Google Scholar]
- 14.Honda S, Shinkai M, Usui Y, et al. Severe gastric damage caused by button battery ingestion in a 3-month-old infant. Journal of pediatric surgery. September 2010;45(9):e23–26. [DOI] [PubMed] [Google Scholar]
- 15.Patoulias I, Kaselas C, Patoulias D, et al. Multiple Gastric Erosion Early after a 3 V Lithium Battery (CR2025) Ingestion in an 18-Month-Old Male Patient: Consideration about the Proper Time of Intervention. Case Rep Pediatr. 2016;2016:3965393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takagaki K, Perito ER, Jose FA, Heyman MB. Gastric mucosal damage from ingestion of 3 button cell batteries. J Pediatr Gastroenterol Nutr. August 2011;53(2):222–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang YJ, Chao HC, Kong MS, Lai MW. Clinical analysis of disc battery ingestion in children. Chang Gung Med J. September 2004;27(9):673–677. [PubMed] [Google Scholar]
- 18.Huang T, Li WQ, Xia ZF, Li J, Rao KC, Xu EM. Characteristics and outcome of impacted button batteries among young children less than 7 years of age in China: a retrospective analysis of 116 cases. World journal of pediatrics : WJP. December 2018;14(6):570–575. [DOI] [PubMed] [Google Scholar]


