Abstract
There is increasing evidence for the role of environmental endocrine disrupting contaminants, coined obesogens, in exacerbating the rising obesity epidemic. Obesogens can be found in everyday items ranging from pesticides to food packaging. Although research shows that obesogens can have effects on adipocyte size, phenotype, metabolic activity, and hormone levels, much remains unknown about these chemicals. This review will discuss what is currently known about the mechanisms of obesogens, including expression of the PPARs, hormone interference, and inflammation. Strategies for identifying obesogenic chemicals and their mechanisms through chemical characteristics and model systems will also be discussed. Ultimately, research should focus on improving models to discern precise mechanisms of obesogenic action and to test therapeutics targeting these mechanisms.
Keywords: Obesogens, Endocrine disrupting chemicals, In vitro models, In vivo models, Obesogenic mechanisms, Hormone interference, Inflammation, Chemical characteristics, Model systems
Background
The economic impact of obesity worldwide is estimated to be 2.8% of the global gross domestic product [1]. While an imbalance in energy intake and expenditure is largely to blame, other factors contribute to this high economic burden. An analysis of obesity trends (the National Health and Nutrition Examination Study) found that from 1988 to 2006 for the same caloric intake and physical activity, the average BMI was higher [2]. Grun and Blumberg in 2006 [3] hypothesized that this increase in average BMI may be related to obesogens, a subset of endocrine disrupting chemicals (EDCs) that alter metabolism to favor lipid storage, leading to a predisposition to obesity. These chemicals can be found in pesticides, cleaning products, and food and beverage packaging [4]. Regular exposure to these contaminants can have long-term effects on adipose tissue, metabolic activity, hormones, and ultimately weight. Additionally, prenatal exposure may put people at risk for becoming obese later in life. As obesity care is a billion-dollar industry worldwide, identifying and understanding these obesogens is a crucial step in reforming worldwide health.
This review discusses possible mechanisms of obesogenic action including regulation of the PPAR genes, hormone interference, and inflammation. Insights into mechanisms of obesogens will allow for specific therapeutic targeting to minimize effects and aid in predicting potential obesogens from environmental contaminants. This review also discusses advantages and disadvantages of current model systems that are being used (both in vitro and in vivo as well as epidemiological studies) to study obesogens.
Main text
Chemical characteristics of obesogens
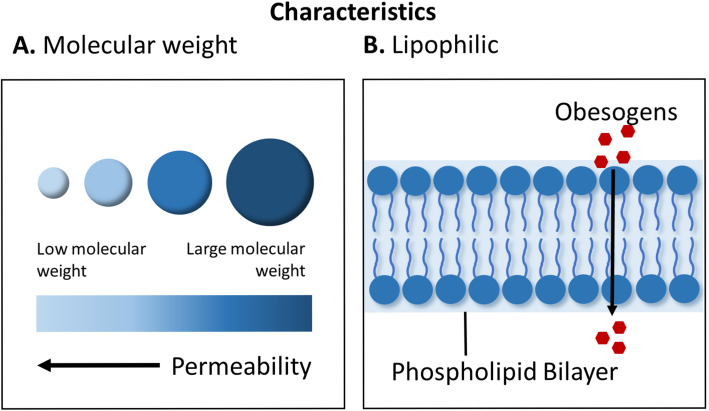
Obesogens work through a diverse set of mechanisms [5]. They have been known to mimic or partially mimic natural hormones, having undesired biological effects [6]. They can bind to receptors in the cell membrane, cytosol, or the nucleus affecting cellular responses, peptide hormones, or gene expression directly [6]. Their ability to do this depends on having chemical characteristics that resemble natural hormones including lipophilicity and small molecular weight (Fig. 1). Three key properties that may influence the ability of obesogens to act as xenohormones are the partition constant, half-life, and molecular weight. The partition constant is an equilibrium constant that measures how a compound distributes between two immiscible solvents. The octanol:water partition coefficient (Kow) is the ratio of a compound’s partition (divide) between organic matter and water [7]. The equation for KOW is defined as: concentration of chemical in octanol phase / concentration of chemical in aqueous phase [7]. The equation gives a measure of how a chemical will split between tissue and serum at equilibrium. As lipids are organic matter, it is thus an accepted measure of the lipophilicity of the compound. A higher KOW indicates a more lipophilic substance and a propensity to accumulate in adipose tissue [6, 7]. The biological half-life of a chemical is the time it takes for half of the amount of the chemical to be broken down or removed from the body. A longer biological half-life indicates longer persistence in the body. This is particularly relevant to obesogens as a longer biological half-life can mean even a brief exposure can have long-term effects [8]. Molecular weight is a measure of the size of the compound. This is important, since smaller molecules can diffuse into adipocytes more easily. Additionally, even high molecular weight chemicals can be broken down into low molecular weight metabolites in the body that can have obesogenic effects [7]. These three properties tend to have a profound effect on accumulation in the body and affinity for receptors [7, 9]. Lipophilic substances with low molecular weights cross cell membranes easily [6]. Those with long biological half-lives can reside in adipose tissue for months to years. Many well-studied obesogens fit these criteria. A short list of established obesogens and their molecular characteristics are given in Table 1. Lipophilic compounds are also more resistant to degradation, leading to many of them having a biphasic half-life such as 2,2′,4,4′-tetrabromodiphenyl ether (BDE-47) (Table 1) [6]. Substances that are biphasic have an elimination curve that is steep that describes the initial distribution of the drug in the body, followed by shallow curve that describes the final removal of drug, which is dependent on the release of the drug from tissue compartments such as adipose tissue into the blood [20]. Obesogens also have a strong affinity for receptors in the body, specifically nuclear receptors. This could be attributed to the lipophilic nature of the compounds that resemble steroid substances found heavily in adipose tissue [21]. However, more studies need to be done to find other physiochemical properties that control EDCs ability to utilize these receptors.
Fig. 1.
Obesogens have characteristics that make them well-suited to enter cells including small molecular weight (a) and lipophilicity (b). These properties allow obesogens to easily pass through cell membranes to influence cellular responses and gene expression
Table 1.
Sample list of a subset of well-established obesogens with their partitioning coefficients, half-life, and molecular weight (g/mol). The octanol/water partitioning coefficient is measured using the log Kow value, which indicates the partitioning of a chemical between octanol and water. In these experiments, octanol is used to mimic fat and other hydrophobic components in biological systems. A partitioning coefficient level greater than 1 indicates low solubility in water
| Obesogen Source | Obesogensa | Chemical Characteristics* | ||
|---|---|---|---|---|
| Partitioning (Log Kow) b | Half-life (hours)c | Size (g/mol) | ||
| Industrial Chemicals | Bisphenol A (BPA) | 3.32 | 5.3d [10, 11] | 228.291 |
| Bisphenol A diglycidyl ether (BADGE) | ~ 3.84 | 120e [12] | 340.419 | |
| Bisphenol S (BPS) | ~ 1.65 | 6.93 [13] | 250.268 | |
| Firemaster 550 (FM550) | 8.80–11.95f | Unknown [14] | 549.923 | |
| 2,2′,4,4′-Tetrabromodiphenyl ether (BDE-47) | 6.81 ± 0.08 [15] | 664 daysg | 485.795 | |
| 3,3′,4,4′-Tetrachlorobiphenyl (PCB-77) | 6.72 | 152–186 [16] | 291.980 | |
| Mono-(2-ethylhexyl) phthalate (MEHP) | 4.92h | 4.4–6.6i | 278.348 | |
| bis(2-ethylhexyl) phthalate (DEHP) | 7.60 | 5j | 390.564 | |
| Biocides | Dichlorodiphenyl-trichloroethane (DDT) | 6.91 | 10.6k | 354.476 |
| Tributyltin (TBT) | 3.90–4.90 [17] | 23–30 days [18] | 290.058 | |
| Triphenyltin (TPT) | 4.19l | 3 days | 385.478 | |
| Pharmaceuticals | Diethylstilbestrol (DES) | 5.07 | 2–3 days [19] | 268.350 |
| Estradiol (Estrogen steroid Hormone) | 4.01 | 3 days | 272.388 | |
| Pollutant | Dioxin | 6.80 | 5–8 years | 321.970 |
| Smoking | Nicotine | 1.17 | 1–4m | 162.236 |
Sources
*Values of partition coefficients and half-lives might differ from those in this table because of variations in the study such as the location the study was conducted, type of tissue, biphasic pattern, initial dosage, temperature, salinity and pH.
aThe obesogens discussed are well-established obesogens that have been used in various studies.
bAll values of log Kow were reported at 25°C and at a pH of 7 unless stated otherwise.
cAll estimated half-life values reported were conducted on studies in human based models unless stated otherwise.
dBPA data are not consistent with the current consensus that BPA exposures are both rapidly cleared and almost entirely related to food intake. Instead, it appears plausible that there is substantial nonfood exposure, accumulation in body compartments with long elimination times, or both [3].
eBisphenol A diglycidyl ether based on Hydrolysis in Water.
f2-ethyl-1-hexyl-2,3,4,5-tetrabromobenzoate (TBB) and bis (2-ethylhexyl) tetrabromophthalate (TBPH) are the two major additive Brominated flame retardants (BFRs) in Firemaster 550. [16].
gTetrabromodiphenyl ether (BDE-47) has two phases of elimination. The first phase of elimination is where the majority of the BDE-47 is eliminated from the body (67%), and the remaining BDE-47 is eliminated during the terminal phase. Additionally, elimination, both whole-body and from individual tissues, is biphasic due to varying initial and terminal phase lengths in different tissues. Since BDE-47 is highly lipophilic its terminal phase was primarily dictated by adipose tissue and skin [21].
hMEHP was estimated from n-octanol: water coefficient (Kow) by the algorithm from Poulin and Krishnan (1993). A log Kow of 4.92 was estimated based on the chemical structure for nonionized MEHP.
iSingle administration of MEHP in a rat (0.4 g/kg) resulted in plasma concentrations of 84.1 +/− 14.9 micrograms/ml 3 h after dosing; the half-life of MEHP was 5.5 +/− 1.1 h. [22].
jAfter an absorption and distribution phase of 4 to 8 h, half-life times of excretion in the first elimination phase were approximately 2 h; Half-life times in the second phase—beginning 14 to 18 h post dose—were 5 h for MEHP [23].
kFemale rats were dosed orally with (14) C-ring-labeled p,p’-DDT during pregnancy or lactation. Average half-life was 10.6 h in tissues and in the fetus.
lTriphentylin Chloride was used to find the log Kow.
mNicotine’s half-life in the initial phase is reportedly about 2–3 min and the half-life in the terminal phase averages about 2 h.
Note: All partitioning coefficient values > 1 indicate lipophilic properties (bold). Half-life with strong indication of biphasic pattern (bold). Non-asterisk and cited chemical characteristics were obtained from the U.S. National Library of Medicine Open Chemistry Database and the International Programme on Chemical Safety.
Mechanisms of action of obesogens
Definitive mechanisms for obesogens are still in the early stages of investigation. Current research points to a major role of peroxisome proliferator-activated receptor gamma (PPARγ), hormone interference, and inflammation in obesogenic outcomes (Fig. 2). While the role of these three mechanisms in obesogenic effects will be discussed in the following section, it should be noted that many potential mechanisms for obesogens exist, not all of which will be discussed here. It should also be noted that there are likely distinct pathways for developmental (in utero) and non-developmental exposures of obesogens, as well as persistent versus non-persistent exposures, with more research required to clearly define these differences. For more comprehensive reviews on what is currently known about mechanisms of obesogens see [22–24].
Fig. 2.
Obesogens can interfere with endocrine function by direct hormone interference or activation of peroxisome proliferator-activated receptor gamma (PPARγ) in adipocytes. Obesogens can also alter appetite and satiety through neuroendocrine mechanisms
Activation of peroxisome proliferator-activated receptor gamma (PPARγ)
Peroxisome proliferator activated receptors (PPARs) are a group of non-steroid nuclear hormone receptors [25, 26]. There are three known isoforms of PPAR: (1) PPARα; (2) PPARβ/δ; and (3) PPARγ. Each isoform is encoded by a separate gene [26, 27]. PPARs bind with the nuclear receptor 9-cis retinoic acid receptor (RXR) to form their own heterodimers. These heterodimers modulate expression of target genes [28–31]. The heterodimer binds to specific response sites called peroxisome proliferator response elements (PPRE) in the promoter region of target genes. Subsequent binding of a ligand to the receptor then alters the conformation of PPAR to induce recruitment of co-transcription factors. This results in an increase in mRNA expression of the target gene [28, 29, 31, 32]. PPARs target genes related to lipid storage, transport, and metabolism including fibroblast growth factor 1 (FGF1) (PPARγ) [33], G-protein-coupled receptor 81 (GPR81) (PPARγ) [34], adiponectin (PPARα), [35], and CPT-1 (PPARα) [36, 37] and so are common targets in the study of obesogenic mechanisms [28, 29, 31].
PPARγ is the most widely studied transcription factor in terms of adipose tissue development and is required for adipogenesis [38–40]. Thiazolidinedione drugs used to treat type 2 diabetes target PPARγ to increase insulin sensitivity with the side effect of inducing adipogenesis [41]. Many obesogens have already been shown to upregulate this gene. Tributyltin (TBT), one of the most widely studied obesogens, activates the PPARγ/RXR heterodimer in vitro [42, 43], in utero [44], and in vivo [43]. It is unclear if the effects are due to the activation of the PPARγ domain itself, the RXR domain, or both. It is likely that TBT activates the PPARγ/RXR complex through binding of the RXR domain since transfected Cos7 cells were activated by TBT in the presence of a PPARγ antagonist [42]. Additionally, commitment of mesenchymal stem cells to the adipogenic lineage has been shown to be dependent on RXR activation and not PPARγ activation [45]. However, further analysis needs to be done to affirm this conclusion. Other obesogens that have also been shown to act at least partially through PPARγ/RXR activation include bisphenol A (BPA, plastic monomer) [46–48], triflumizole (fungicide) [49], phthalate monoesters (plasticizers) [50], Firemaster 550 (flame retardant) [51], and dioctyl sodium sulfosuccinate (DOSS) (component of oil dispersant COREXIT) [52]. It is likely that different obesogens have different mechanisms for activating the PPARγ/RXR heterodimer and further research will be needed to determine specific molecular mechanisms. Understanding the specific effects of these obesogens on the PPARγ/RXR heterodimer may provide valuable insight for reversing obesogenic effects.
PPARα is another isoform of PPAR. It is found primarily in the liver, skeletal muscle, heart, and brown adipose tissue and plays a major role in fatty acid metabolism in the liver [53–55]. Natural ligands include oxidized phospholipids, lipoprotein lipolytic proteins, and fatty acids, among other natural ligands [54]. Although it is found primarily in liver and skeletal muscle, there is increasing evidence for its role in adipose tissue and as a target for obesogens. PPARα is known to improve insulin sensitivity and aid in body weight control in rodents [53, 54]. Agonists have also been shown to reduce insulin resistance and decrease body weight in male mice [53]. PPARα-deficient mice have been shown to have upregulated mRNA expression of adiponectin, but this is thought to be the result of increased adipose tissue mass or an attempt to counterbalance a concomitant increase in leptin expression [56]. PPARα is not as widely studied as PPARγ in terms of obesogens but current literature suggests there is an effect. Monosodium glutamate (MSG) and aspartame decreased gene expression of PPARα in mice [57]. TBT was shown to activate PPARα in transfected HeLa cells [58] and mice exposed to TBT in utero showed increased mRNA expression of PPARα [59]. Since PPARα is known to improve insulin sensitivity, the increased expression could be one of the mechanisms for obesogenic effects. However, the obesogen bis (2-ethylhexyl) phthalate (DEHP) increased mRNA expression of PPARα in liver tissue while decreasing expression in visceral fat in mice [60]. The mechanisms of obesogens are likely more complex than what is currently understood and further research will be required to draw conclusions.
Hormone interference
Exogenous chemicals that are capable of mimicking or interfering with hormonal action can have profound effects on the overall function of metabolic processes. Hormones such as androgens and estrogens are tightly regulated and play an important role in the function of adipose tissue. Increasing androgen levels are associated with lower BMIs in men [61]. Several phthalates are suspected antiandrogens [62] and have shown obesogenic effects in humans. BPA acts as a xenoestrogen. When mice are exposed perinatally to BPA, the offspring are significantly heavier [48]. Dichlorodiphenyldichloroethylene (DDE, a metabolite of the common pesticide dichlorodiphenyl-trichloroethane, DDT) has also been shown to exhibit estrogenic responses [63]. It leads to rapid weight gain in infants after prenatal exposure. BPA, phthalates and polybrominated diphenyl ethers (PBDEs) also have been shown to reduce circulating thyroid levels [64], a key regulator of basal metabolism. Decreased thyroid hormone levels result in an increased BMI [65]. Leptin and adiponectin are also influenced by obesogens. Leptin, discovered by Zhang et al., is responsible for satiety and increases glucose uptake by skeletal muscle and brown adipose tissue [66, 67]. Mutations in leptin result in obesity and hyperinsulinemia. However, hyperleptinemia, as is common in obesity, can lead to leptin resistance [66, 68]. Adiponectin, first discovered by Scherer et al., is known to increase insulin sensitivity [69, 70]. Multiple obesogens have been shown to have an effect on these hormones. TBT increases plasma leptin levels in mice, causing an overexpression of the leptin gene, and decreased serum adiponectin levels [71, 72]. DEHP decreases both adiponectin and leptin mRNA levels in mice [60]. DOSS increases plasma leptin levels in male mice exposed in utero [73]. Genistein, an isoflavone found in soy, induced adipose deposition in male mice, increased insulin resistance, and upregulated mRNA expression of leptin [74]. DEHP has also been shown to increase serum leptin levels [75]. Benzyl butyl phthalate (BBP, plasticizer) was shown to increase adiponectin protein expression in differentiated 3T3-L1 cells [76]. Additionally, glucocorticoid receptor signaling is crucial for adipocyte differentiation [77]. Sargis et al. [78] demonstrated increased adipogenic differentiation via glucocorticoid receptor activation with BPA, dicyclohexyl phthalate (DCHP), endrin, and tolylfluanid (TF). Hormones are a common target of obesogens but the exact effect of each obesogen and the mechanisms of hormone influence are yet to be determined. Moreover, there are likely other hormonal targets that are still unidentified.
Inflammation
Obesity is associated with chronic inflammation. While inflammation is associated with adipose tissue expansion, it may also be the result of epigenetic changes due to environmental and lifestyle factors [79]. DOSS has been shown to increase body mass, visceral fat mass, upregulate inflammatory gene expression (Cox2, Nox4), and increase plasma levels of IL-6 in male mice exposed in utero [73]. Likewise, TBT exposure in rats upregulated PPARγ, increased ovarian fat mass, and increased reproductive tract inflammation in rats [80]. A similar study in female rats showed increased body weight and uterine inflammation after TBT exposure [81]. Male mice exposed to BPA showed increased gene expression of IL-6, TNF-α, and IL-1β in white adipose tissue and increased fat mass on a chow-diet [82]. Differentiated 3T3-L1 preadipocytes also show increased expression of IL-6, TNF-α, MCP-1, and CXCL1 after exposure to either TBT, BPA, or mono-ethylhexyl phthalate (MEHP, metabolite of DEHP) [83]. Moreover, a study on male mice showed an Il-17 antibody was able to reduce inflammation and counter the obesogenic effects of BPA, suggesting inflammation plays a major role in the obesogenic effects of BPA [84]. Multiple obesogens have also been shown to increase the presence of immune cells in adipose tissue. Female sheep exposed to BPA show increased mRNA expression of CD68, a marker of macrophage infiltration [85]. Additionally, mice exposed to BPA perinatally showed increased presence of macrophages in gonadal white adipose tissue [86]. BPA has also been shown to increase macrophage self-renewal [87]. BPA is one of the most widely studied obesogens but it is likely that an influx of inflammatory cells plays a role in other obesogens as well. There is also evidence for a correlation between the PPAR genes and inflammation. While they are upregulated during inflammation they also act as negative feedback loops by being antagonists to transcription factors for proinflammatory genes [88–92]. Antidiabetic drugs, such as thiazolidinediones antagonize tumor necrosis factor-α (TNF-α) [93] and act as agonists for PPARγ [94]. This area is in early stages of research but suggests a role for inflammatory cells and gene expression in obesogenic modes of action.
Model systems
Currently, model systems are used to test mechanisms of obesogenic action including in vitro and in vivo systems as well as epidemiological studies. Each type poses unique benefits and drawbacks to establishing mechanisms. Common systems for each type are discussed below along with advantages and disadvantages.
In vitro models
In vitro models pose several benefits over other model systems. They can utilize human cell types to be more physiologically relevant. They are also generally simpler, faster, can be done in parallel (for medium to high throughput analyses), and are more cost-effective, making them a good screening mechanism for obesogens prior to in vivo studies. Currently, there are several in vitro models to screen potential obesogens that examine characteristics such as adipocyte maturation and lipid accumulation (Table 2). The vast majority of these models utilize mouse 3T3-L1 preadipocytes. These cultures have been integral in elucidating certain molecular mechanisms of adipogenesis. However, it is still unclear if the 3T3-L1 cell line is adequate for evaluating adipogenic responses, since they are fully committed to the adipocyte lineage [120, 121]. Additionally, the murine-derived 3T3-L1 cell line maintains species specificity, which may hinder application of results for human-based risk assessments. Use of human primary cell lines mitigates this risk but further limitations exist. Patient demographics and medical histories are unknown to researchers and contribute large variability in outcomes [122]. Sex specific differences are often not accounted for and gender is known to dictate body fat storage [123] and responses to obesogens [48]. Future work needs to work on validating these models using primary cells or tissues from a wide range of known patient demographics. There are also depot-specific effects of obesogens on adipose tissue. Cells derived from visceral versus subcutaneous or brown versus white adipose tissue may have varying responses to obesogens. As visceral adipose tissue is most closely linked to metabolic disease, understanding differential responses by adipose tissue depots is crucial for defining obesogenic effects.
Table 2.
2D and 3D in vitro models for studying obesogens. Note: -- under Matrix indicates a 2D cell culture study
| Matrix | Cell Type | Obesogen | Source |
|---|---|---|---|
| – | 3T3-L1 (murine preadipocyes) | Tributyltin (TBT) | [42, 43, 94–99] |
| Bisphenol A (BPA) | [97–99] | ||
| Bisphenol S (BPS) | [102] | ||
| Bisphenol A diglycidyl ether (BADGE) | [100] | ||
| Triphenyltin | [95] | ||
| Dioctyl sodium sulfosuccinate (DOSS) | [52] | ||
| Geneistein & naringenin | [103] | ||
| Phthalate monoesters | [32] | ||
| 4-nonylphenol (NP) | [101] | ||
| Mono-ethylhexyl phthalate (MEHP) | [50] | ||
| Flavanone | [104] | ||
| Bixin, norbixin | [105] | ||
| Emodin | [106] | ||
| C2C12 (murine) | Mono-ethylhexyl phthalate (MEHP) | [50] | |
| HELA (human) | Mono-ethylhexyl phthalate (MEHP) | [50] | |
| Human embryonic kidney cells (HEK293C) | Dioctyl sodium sulfosuccinate (DOSS) | [52] | |
| HepG2 (human liver carcinoma cells) | Bisphenol A (BPA), Bisphenol S (BPS) | [102] | |
| Human adipose-derived stem cells (hASCs) | Bisphenol A (BPA), Bisphenol A diglycidyl ether (BADGE) | [102] | |
| Tributyltin (TBT) | [44] | ||
| Murine adipose derived stem cells (mASCs) | Bisphenol A (BPA), Bisphenol A diglycidyl ether (BADGE) | [102] | |
| Tributyltin (TBT) | [44] | ||
| Fao (murine hepatoma cells) | Phthalate monoesters | [32] | |
| COS (monkey kidney-derived cells) | Bisphenol A (BPA), Bisphenol A diglycidyl ether (BADGE) | [102] | |
| MBzP, MBuP | [50] | ||
| Mono-ethylhexyl phthalate (MEHP) | [50, 107] | ||
| THP-1 macrophages (human) | Psi-baptigenin, hesperidin | [108] | |
| TARM-Luc (human, transfected T47-D epithelial cells) | Monosodium glutamate (MSG) | [109] | |
| KS483 (murine calvaria) | Soy phytoestrogen genistein | [110] | |
| C57BL/6 (murine–derived bone marrow stromal cells) | Firemaster 550 | [51] | |
| collagen embedded silk scaffolds | Human embryonic-derived stem cells (hESCs) | Tributyltin (TBT), Bisphenol A (BPA), Bisphenol S (BPS) | [111] |
| silk scaffolds | Human adipose-derived stem cells (hASCs), Human umbilical vein endothelial cells (HUVECs) | – | [112] |
| silk fibroin matrices | Human adipose-derived stem cells (hASCs) | – | [113] |
| collagen type 1 | OP9 (murine mesenchymal stromal pluripotent cells), HaCaT (human keratinocytes) | Super Hatomugi (SPH) | [114] |
| bacterial nanocellulose | Murine mesenchymal stem cells (mMSCs) | – | [115] |
| fibrous polyethylene teraphthalate scaffolds | 3T3-L1 (murine preadipocyes) | – | [116] |
| low-shear rotary bioreactor | Murine adipose-derived stem cells (mASCs) | – | [117] |
| polyglycolic acid fiber meshes | 3T3-L1 (murine preadipocyes) | – | [118] |
| adipospheres created via magnetic nanoparticle levitation system | 3T3-L1 (murine preadipocyes) | – | [119] |
To better understand the impact of obesogenic chemicals in more physiologically relevant environments, scientists have been examining 3D human tissue systems to model the effects of obesogens in vitro (Table 2). 3D adipose tissue systems recapitulate the in vivo adipose tissue microenvironment, can be extended for long term culture [122, 124] (months, to study chronic effects of obesogens) and can incorporate multiple cell types. They can be used to study the sequestration of obesogens in adipose tissue as well as cell migration. Obesogens are primarily lipophilic and thus prone to retention by adipose tissue [125]. 3D models can incorporate mature adipocytes which are non-adherent and cannot be cultured using standard 2D culture techniques. Similarly, they allow for long-term in vitro study of ASC differentiation which also become non-adherent over time [126]. The use of 3D models allows for more sophisticated co-culture systems. As multiple organs play a role in obesogenic actions including adipose tissue, pancreas, liver, thyroid, etc., systems integrating multiple cell types may provide more physiologically accurate data. They can also study paracrine signaling. However, 3D models increase cost and complexity over 2D systems, since they use natural or artificial extracellular matrices (ECM). This brings the added variables of cell binding domains, mechanical properties, pore size, etc. Perfusion cultures also pose issues related to flow rates, media, and fluid/cell ratios. Finally, most in vitro studies are currently 2D which limits the ability to compare results from 3D cultures to already-established models. Overall, both 2D and 3D in vitro models provide precise control of cellular interactions and boundary conditions, permitting quantitative analyses of mechanisms. They are ideally suited for high-throughput screening as they can test dose responses and mixture effects in parallel. While in vitro models have limitations that must be resolved, they provide strong screening potential for obesogens.
In vivo models
Animal models have the distinct and obvious disadvantage of not accurately replicating human physiology. However, animal models are an important and widely used tool for the study of obesogens because they are suited for studying whole body kinetics and systemic effects not possible in vitro. Metabolism and weight is regulated by complex interconnected pathways involving multiple organs including adipose tissue, liver, pancreas, muscle, brain, etc. [127]. Although in vitro cell culture techniques can use human cell lines, recapitulating the inter-dependency of these systems remains difficult. Long-term in vitro culture remains a challenge and multi-organ models pose unique problems such as scaling ratios, common mediums, and organ-specific ECMs. Thus, although more sophisticated in vitro models are being heavily researched, animal models still play an important role in identifying obesogens and understanding obesogenic mechanisms because they allow for the study of organ cross-talk and systemic effects. This is particularly relevant in understanding the role of chronic inflammation and hormone interference.
Rodents are the most commonly used animal model for studying obesogens. Multiple obesogens have been identified using murine models including: TBT [43], BPA [82], triphenyltin [43, 95], DEHP [128], DES [129], MEHP [130], polycyclic aromatic hydrocarbons [131, 132], DDT [133], and nicotine [134]. Mice are biologically and anatomically similar to humans and contract many of the same diseases [135]. This is particularly useful for diseases with an inflammatory component, such as obesity [136], as animal models can mimic complex inflammatory responses. Mice can also be genetically manipulated, inbred to yield genetically identical strains, can be grown under controlled conditions (i.e high-fat/western diet), and have an accelerated lifespan (minimizing the time required to do studies). Other common in vivo systems used to evaluate obesogens include: rats, [137–139] zebrafish, [140–142] and the Xenopus laevi [143]. Use of in vivo models to study endocrine disruption has provided many insights into potential obesogens and different modes of action. However, it is important to keep in mind the drawbacks of using animal models. As discussed, they do not necessarily recapitulate human physiology [144]. Moreover, the dose-response may not translate directly to humans. The window of exposure may also be unnatural. Mice exposed to a specified level of one particular chemical over the course of weeks may not represent chronic fluctuating exposure to multiple chemicals over the course of years in humans. Animal models play an important role in identifying obesogens and discerning mechanisms of action but should be combined with information from in vitro studies and epidemiological studies to draw the most accurate conclusions.
Epidemiological studies
Epidemiological studies are extremely important for correlating disease outcomes to concentrations of obesogens in humans. However, human studies linking EDCs and obesity are limited, inconsistent, and lack data to support the growing animal literature (for review see Hatch et al., 2010 [145]). Current studies are often cross-sectional and exploratory.
Since a significant amount of evidence suggests that prenatal exposures predispose patients towards obesity, measurements of obesogens during pregnancy is a large focus for epidemiological studies. A study revealed that increasing maternal urinary phthalate concentrations during pregnancy doubled the likelihood of the offspring being overweight or obese [146]. Likewise, cohort studies on the effects of prenatal exposures to BPA showed an association with an increased waist circumference, BMI, and risk of being obese [147]. Future work is necessary to compare results from developmental exposures to exposures later in life. Perspective long term studies are also necessary to track patients over time.
Some epidemiological studies examine single-spot urine or 24-h urine samples in order to assess exposure over a day [148]. This method allows investigators to directly measure individual chemical concentrations in a variety of biospecimens [149]. However, it is not possible to determine whether exposures were acute or long term. Although chemical exposure biomarkers have been advantageous in studying a variety of individual biospecimens, short half-lives in certain obesogens (such as BPA that persists as BPA-G) and reverse causality due to pharmacokinetic variables have limited their usefulness [150]. Additionally, given the lipophilic nature of obesogens, it is unlikely that urine samples are an accurate reading of exposure. Ideally, adipose tissue would be sampled directly.
Another important consideration brought up by Sharpe and Drake [151], is the influence of confounding factors in epidemiological studies. They warn that obesogenic exposures may not have a causal relationship with obesity, since a Western style diet increases exposure to these compounds, and thus the observed increase in levels would be reflective of greater food consumption. Another confounding factor is that many epidemiological studies are designed to assess the impact of a single chemical without accounting for the effects of mixtures [148]. Statistical models must be developed in order to elucidate the health outcomes associated with specific chemicals in the mixtures. These studies should account for the fact that some of these chemicals may operate by the same mechanism, while interfering with other mechanisms.
Conclusion
Abundant evidence supports the role of exogenous chemicals in rising obesity rates through regulation of gene expression (such as the PPARs), hormone changes, and inflammation. A greater understanding of obesogenic mechanisms will lead to better prophylactic and therapeutic strategies and identify other potential obesogens. In vitro models are useful screening tools for identifying and testing mechanisms of obesogens. Specifically, they can help discern changes to gene expression or molecular pathways that induce changes to adipocyte phenotype. Improvements to these models will also improve in vitro to in vivo extrapolation to humans. Still, animal models remain a useful and generally physiologically accurate tool for testing inter-organ obesogenic mechanisms including hormone interference and inflammation. To validate in vitro and in vivo animal models, more comparisons should be made to epidemiological studies. Epidemiological studies provide unparalleled insight into human obesogen exposures and effects. They can be used to identify exposure levels of potential obesogens and to analyze correlative effects between exposure level and BMI, adiposity, leptin/adiponectin levels, etc. This can help determine if there are safe levels of exposure to specific levels or whether drastic actions should be taken to remove a compound entirely. Integrating the information obtained from all three of these model systems will lead to better-informed choices of compounds that can be used in food processing, packaging, etc. to replace obesogens. Ultimately, this will decrease the economic burden of obesity.
Acknowledgements
Not applicable.
Abbreviations
- PPAR
Peroxisome proliferator-activated receptor
- PPARγ
Peroxisome proliferator-activated receptor gamma
- PPARβ/δ
Peroxisome proliferator-activated receptor beta/delta
- PPAR⍺
Peroxisome proliferator-activated receptor alpha
- EDC
Endocrine disrupting chemical
- KOW
Partition coefficient
- PPRE
Peroxisome proliferator response elements
- RXR
Retinoic acid receptor
- FGF1
Fibroblast growth factor 1
- GPR81
G-Protein-coupled receptor 81
- BDE-47
2,2′,4,4′-tetrabromodiphenyl ether
- BPA
Bisphenol A
- TBT
Tributyltin
- DOSS
Dioctyl sodium sulfosuccinate
- MSG
Monosodium glutamate
- DEHP
Di-2-ethylhexyl phthalate
- BMI
Body mass index
- DDE
Dichlorodiphenyldichloroethylene
- DDT
Dichlorodiphenyl-trichloroethane
- PBDEs
Polybrominated diphenyl ethers
- BBP
Benzyl butyl phthalate
- IL-6
Interleukin-6
- TNF-⍺
Tumor necrosis factor-alpha
- IL-1β
Interleukin-1 beta
- MCP-1
-
Monocyte chemoattractant protein-1
CXCL1:
C-X-C Motif Chemokine Ligand 1
- MEHP
-
Mono-(2-ethylhexyl) phthalate
IL-17:
Interleukin-17
- BPA-G
Bisphenol A β-D-glucuronide
- FM550
Firemaster 550
- DES
Diethylstilbestrol
- DCHP
Dicyclohexyl phthalate
- TF
Tolylfluanid
Authors’ contributions
MDG was a major contributor of the conception, design, and drafting of the manuscript. SRP did the literature review, table construction, and manuscript text for the section “Chemical Characteristics of Obesogens.” MKD was responsible for figure design and construction as well as critical editing for content. RDA was involved in the conception, design, and drafting of the manuscript. All authors revised the manuscript critically for important intellectual content; gave their final approval of the version to be published; and are accountable for the accuracy and integrity of the work.
Funding
No funding was obtained for this study.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mallory D. Griffin, Email: mdgriffi@andrew.cmu.edu
Sean R. Pereira, Email: sapereir@andrew.cmu.edu
Megan K. DeBari, Email: mdebari@andrew.cmu.edu
Rosalyn D. Abbott, Email: rabbott@andrew.cmu.edu
References
- 1.Tremmel Maximilian, Gerdtham Ulf-G., Nilsson Peter, Saha Sanjib. Economic Burden of Obesity: A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2017;14(4):435. doi: 10.3390/ijerph14040435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown RE, Sharma AM, Ardern CI, Mirdamadi P, Mirdamadi P, Kuk JL. Secular differences in the association between caloric intake, macronutrient intake, and physical activity with obesity. Obes Res Clin Pract. 2016;10:243–255. doi: 10.1016/j.orcp.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Grun F, Blumberg B. Environmental obesogens: organotins and endocrine disruption via nuclear receptor signaling. Endocrinology. 2006;147:S50–S55. doi: 10.1210/en.2005-1129. [DOI] [PubMed] [Google Scholar]
- 4.Sifakis S, Androutsopoulos VP, Tsatsakis AM, Spandidos DA. Human exposure to endocrine disrupting chemicals: effects on the male and female reproductive systems. Environ Toxicol Pharmacol. 2017;51:56–70. doi: 10.1016/j.etap.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 5.Kelishadi R, Poursafa P, Jamshidi F. Role of environmental chemicals in obesity: a systematic review on the current evidence. J Environ Public Health. 2013;2013:896789. doi: 10.1155/2013/896789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR, Jr, Lee DH, Shioda T, Soto AM, vom Saal FS, Welshons WV, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33:378–455. doi: 10.1210/er.2011-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jackson E, Shoemaker R, Larian N, Cassis L. Adipose tissue as a site of toxin accumulation. Comprehensive Physiology. 2017;7:1085–1135. doi: 10.1002/cphy.c160038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee YM, Kim KS, Jacobs DR, Lee DH. Persistent organic pollutants in adipose tissue should be considered in obesity research. Obes Rev. 2017;18:129–139. doi: 10.1111/obr.12481. [DOI] [PubMed] [Google Scholar]
- 9.Parker MA, Kurrasch DM, Nichols DE. The role of lipophilicity in determining binding affinity and functional activity for 5-HT2A receptor ligands. Bioorg Med Chem. 2008;16:4661–4669. doi: 10.1016/j.bmc.2008.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Genuis SJ, Beesoon S, Birkholz D, Lobo RA. Human excretion of bisphenol a: blood, urine, and sweat (BUS) study. J Environ Public Health. 2012;2012:185731. doi: 10.1155/2012/185731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stahlhut RW, Welshons WV, Swan SH. Bisphenol a data in NHANES suggest longer than expected half-life, substantial nonfood exposure, or both. Environ Health Perspect. 2009;117:784–789. doi: 10.1289/ehp.0800376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lane RF, Adams CD, Randtke SJ, Carter RE., Jr Bisphenol diglycidyl ethers and bisphenol a and their hydrolysis in drinking water. Water Res. 2015;72:331–339. doi: 10.1016/j.watres.2014.09.043. [DOI] [PubMed] [Google Scholar]
- 13.Oh J, Choi JW, Ahn YA, Kim S. Pharmacokinetics of bisphenol S in humans after single oral administration. Environ Int. 2018;112:127–133. doi: 10.1016/j.envint.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 14.Roberts SC, Macaulay LJ, Stapleton HM. In vitro metabolism of the brominated flame retardants 2-ethylhexyl-2,3,4,5-tetrabromobenzoate (TBB) and bis (2-ethylhexyl) 2,3,4,5-tetrabromophthalate (TBPH) in human and rat tissues. Chem Res Toxicol. 2012;25:1435–1441. doi: 10.1021/tx300086x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou SN, Buchar A, Siddique S, Takser L, Abdelouahab N, Zhu J. Measurements of selected brominated flame retardants in nursing women: implications for human exposure. Environ Sci Technol. 2014;48:8873–8880. doi: 10.1021/es5016839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saghir SA, Koritz GD, Hansen LG. Short-term distribution, metabolism, and excretion of 2,2′,5-tri-, 2, 2′,4,4′-tetra-, and 3,3′,4,4′-tetrachlorobiphenyls in prepubertal rats. Arch Environ Contam Toxicol. 1999;36:213–220. doi: 10.1007/s002449900463. [DOI] [PubMed] [Google Scholar]
- 17.Bangkedphol S, Keenan HE, Davidson C, Sakultantimetha A, Songsasen A. The partition behavior of tributyltin and prediction of environmental fate, persistence and toxicity in aquatic environments. Chemosphere. 2009;77:1326–1332. doi: 10.1016/j.chemosphere.2009.09.046. [DOI] [PubMed] [Google Scholar]
- 18.Ema M, Harazono A, Miyawaki E, Ogawa Y. Effect of the day of administration on the developmental toxicity of tributyltin chloride in rats. Arch Environ Contam Toxicol. 1997;33:90–96. doi: 10.1007/s002449900228. [DOI] [PubMed] [Google Scholar]
- 19.Reed CE, Fenton SE. Exposure to diethylstilbestrol during sensitive life stages: a legacy of heritable health effects. Birth Defects Research Part C-Embryo Today-Reviews. 2013;99:134–146. doi: 10.1002/bdrc.21035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oberg M, Sjodin A, Casabona H, Nordgren I, Klasson-Wehler E, Hakansson H. Tissue distribution and half-lives of individual polychlorinated biphenyls and serum levels of 4-hydroxy-2,3,3′,4′,5-pentachlorobiphenyl in the rat. Toxicol Sci. 2002;70:171–182. doi: 10.1093/toxsci/70.2.171. [DOI] [PubMed] [Google Scholar]
- 21.Janesick AS, Blumberg B. Obesogens: an emerging threat to public health. Am J Obstet Gynecol. 2016;214:559–565. doi: 10.1016/j.ajog.2016.01.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egusquiza RJ, Blumberg B. Environmental Obesogens and their impact on susceptibility to obesity: new mechanisms and chemicals. Endocrinology. 2020;161. [DOI] [PMC free article] [PubMed]
- 23.Heindel JJ, Blumberg B. Environmental Obesogens: mechanisms and controversies. Annu Rev Pharmacol Toxicol. 2019;59:89–106. doi: 10.1146/annurev-pharmtox-010818-021304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang O, Kim HL, Weon JI, Seo YR. Endocrine-disrupting chemicals: review of toxicological mechanisms using molecular pathway analysis. J Cancer Prev. 2015;20:12–24. doi: 10.15430/JCP.2015.20.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chandra V, Huang P, Hamuro Y, Raghuram S, Wang Y, Burris TP, Rastinejad F. Structure of the intact PPAR-γ-RXR-α nuclear receptor complex on DNA. Nature. 2008;456:350–356. doi: 10.1038/nature07413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berger Joel, Moller David E. The Mechanisms of Action of PPARs. Annual Review of Medicine. 2002;53(1):409–435. doi: 10.1146/annurev.med.53.082901.104018. [DOI] [PubMed] [Google Scholar]
- 27.Peters JM, Hollingshead HE, Gonzalez FJ. Role of peroxisome-proliferator-activated receptor β/δ (PPARβ/δ) in gastrointestinal tract function and disease. Clin Sci (Lond) 2008;115:107–127. doi: 10.1042/CS20080022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willson TMB, Peter J, Daniel D, Sternbach A, Henke BR. The PPARs: from orphan receptors to drug discovery†. 2000. [DOI] [PubMed] [Google Scholar]
- 29.Berger J, Moller DE. The Mechanisms of Action of PPARs. 2003. [DOI] [PubMed] [Google Scholar]
- 30.Chandra V, Huang P, Hamuro Y, Raghuram S, Wang Y, Burris TP, Rastinejad F. Structure of the intact PPAR-γ–RXR-α nuclear receptor complex on DNA. 2008. p. 456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kersten S, Desvergne B, Wahli W. Roles of PPARs in health and disease. 2000. p. 405. [DOI] [PubMed] [Google Scholar]
- 32.Bility M, Thompson J, McKee R, David R, Butala J, Vanden Heuvel J, Peters J. Activation of mouse and human peroxisome proliferator-activated receptors (PPARs) by phthalate monoesters. Toxicol Sci. 2004;82:170–182. doi: 10.1093/toxsci/kfh253. [DOI] [PubMed] [Google Scholar]
- 33.Jonker JW, Suh JM, Atkins AR, Ahmadian M, Li P, Whyte J, He M, Juguilon H, Yin Y-Q, Phillips CT, et al. A PPARγ–FGF1 axis is required for adaptive adipose remodelling and metabolic homeostasis. Nature. 2012;485:391. doi: 10.1038/nature10998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jeninga EH, Bugge A, Nielsen R, Kersten S, Hamers N, Dani C, Wabitsch M, Berger R, Stunnenberg HG, Mandrup S, Kalkhoven E. Peroxisome proliferator-activated receptor gamma regulates expression of the anti-lipolytic G-protein-coupled receptor 81 (GPR81/Gpr81) J Biol Chem. 2009;284:26385–26393. doi: 10.1074/jbc.M109.040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hiuge A, Tenenbaum A, Maeda N, Benderly M, Kumada M, Fisman Enrique Z, Tanne D, Matas Z, Hibuse T, Fujita K, et al. Effects of peroxisome proliferator-activated receptor ligands, Bezafibrate and Fenofibrate, on Adiponectin level. Arterioscler Thromb Vasc Biol. 2007;27:635–641. doi: 10.1161/01.ATV.0000256469.06782.d5. [DOI] [PubMed] [Google Scholar]
- 36.Lefebvre P, Chinetti G, Fruchart J-C, Staels B. Sorting out the roles of PPAR alpha in energy metabolism and vascular homeostasis. J Clin Invest. 2006;116:571–580. doi: 10.1172/JCI27989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brandt JM, Djouadi F, Kelly DP. Fatty acids activate transcription of the muscle Carnitine Palmitoyltransferase I gene in cardiac Myocytes via the peroxisome proliferator-activated receptor α. J Biol Chem. 1998;273:23786–23792. doi: 10.1074/jbc.273.37.23786. [DOI] [PubMed] [Google Scholar]
- 38.Tontonoz P, Hu E, Spiegelman BM. Stimulation of adipogenesis in fibroblasts by PPARγ2, a lipid-activated transcription factor. Cell. 1994;79:1147–1156. doi: 10.1016/0092-8674(94)90006-X. [DOI] [PubMed] [Google Scholar]
- 39.Rosen ED, Sarraf P, Troy AE, Bradwin G, Moore K, Milstone DS, Spiegelman BM, Mortensen RM. PPARγ is required for the differentiation of adipose tissue in vivo and in vitro. Mol Cell. 1999;4:611–617. doi: 10.1016/S1097-2765(00)80211-7. [DOI] [PubMed] [Google Scholar]
- 40.Barak Y, Nelson MC, Ong ES, Jones YZ, Ruiz-Lozano P, Chien KR, Koder A, Evans RM. PPARγ is required for placental, cardiac, and adipose tissue development. Mol Cell. 1999;4:585–595. doi: 10.1016/S1097-2765(00)80209-9. [DOI] [PubMed] [Google Scholar]
- 41.Straus D, Glass C. Cyclopentenone prostaglandins: new insights on biological activities and cellular targets. Med Res Rev. 2001;21:185–210. doi: 10.1002/med.1006. [DOI] [PubMed] [Google Scholar]
- 42.Li X, Ycaza J, Blumberg B. The environmental obesogen tributyltin chloride acts via peroxisome proliferator activated receptor gamma to induce adipogenesis in murine 3T3-L1 preadipocytes. J Steroid Biochem Mol Biol. 2011;127:9–15. doi: 10.1016/j.jsbmb.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grun F, Watanabe H, Zamanian Z, Maeda L, Arima K, Cubacha R, Gardiner DM, Kanno J, Iguchi T, Blumberg B. Endocrine-disrupting organotin compounds are potent inducers of adipogenesis in vertebrates. Mol Endocrinol. 2006;20:2141–2155. doi: 10.1210/me.2005-0367. [DOI] [PubMed] [Google Scholar]
- 44.Sv K, Kieu T, Chow C, Casey S, Blumberg B. Prenatal exposure to the environmental Obesogen Tributyltin predisposes multipotent stem cells to become adipocytes. Mol Endocrinol. 2010;24:526–539. doi: 10.1210/me.2009-0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shoucri BM, Martinez ES, Abreo TJ, Hung VT, Moosova Z, Shioda T, Blumberg B. Retinoid X receptor activation alters the chromatin landscape to commit Mesenchymal stem cells to the adipose lineage. Endocrinology. 2017;158:3109–3125. doi: 10.1210/en.2017-00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Directorate E. OECDD (organisation for economic cooperation and development) 2004. [Google Scholar]
- 47.Krishnan AV, Stathis P, Permuth SF, Tokes L, Feldman D. Bisphenol-a: an estrogenic substance is released from polycarbonate flasks during autoclaving. Endocrinology. 1993;132:2279–2286. doi: 10.1210/endo.132.6.8504731. [DOI] [PubMed] [Google Scholar]
- 48.Rubin BS, Soto AM. Bisphenol a: perinatal exposure and body weight. Mol Cell Endocrinol. 2009;304:55–62. doi: 10.1016/j.mce.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li X, Pham HT, Janesick AS, Blumberg B. Triflumizole is an Obesogen in mice that acts through peroxisome proliferator activated receptor gamma (PPARγ) Environ Health Perspect. 2012;120:1720–1726. doi: 10.1289/ehp.1205383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hurst CH, Waxman DJ. Activation of PPAR alpha and PPAR gamma by environmental phthalate monoesters. Toxicol Sci. 2003;74:297–308. doi: 10.1093/toxsci/kfg145. [DOI] [PubMed] [Google Scholar]
- 51.Pillai H, Fang M, Beglov D, Kozakov D, Vajda S, Stapleton H, Webster T, Schlezinger J. Ligand binding and activation of PPAR gamma by Firemaster (R) 550: effects on Adipogenesis and Osteogenesis in vitro. Environ Health Perspect. 2014;122:1225–1232. doi: 10.1289/ehp.1408111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Temkin A, Bowers R, Magaletta M, Holshouser S, Maggi A, Ciana P, Guillette L, Bowden J, Kucklick J, Baatz J, Spyropoulos D. Effects of crude oil/dispersant mixture and dispersant components on PPAR gamma activity in vitro and in vivo: identification of Dioctyl sodium Sulfosuccinate (DOSS; CAS #577-11-7) as a probable Obesogen. Environ Health Perspect. 2016;124:112–119. doi: 10.1289/ehp.1409672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Veiga FMS, Graus-Nunes F, Rachid TL, Barreto AB, Mandarim-de-Lacerda CA, Souza-Mello V. Anti-obesogenic effects of WY14643 (PPAR-alpha agonist): hepatic mitochondrial enhancement and suppressed lipogenic pathway in diet-induced obese mice. Biochimie. 2017;140:106–116. doi: 10.1016/j.biochi.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 54.Han L, Shen W-J, Bittner S, Kraemer FB, Azhar S. PPARs: regulators of metabolism and as therapeutic targets in cardiovascular disease. Part I: PPAR-α. Futur Cardiol. 2017;13:259–278. doi: 10.2217/fca-2016-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Azhar S. Peroxisome proliferator-activated receptors, metabolic syndrome and cardiovascular disease. Futur Cardiol. 2010;6:657–691. doi: 10.2217/fca.10.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yessoufou A, Atègbo J-M, Attakpa E, Hichami A, Moutairou K, Dramane KL, Khan NA. Peroxisome proliferator-activated receptor-α modulates insulin gene transcription factors and inflammation in adipose tissues in mice. Mol Cell Biochem. 2008;323:101. doi: 10.1007/s11010-008-9968-1. [DOI] [PubMed] [Google Scholar]
- 57.Collison KS, Makhoul NJ, Zaidi MZ, Inglis A, Andres BL, Ubungen R, Saleh S, Al-Mohanna FA. Prediabetic changes in gene expression induced by aspartame and monosodium glutamate in trans fat-fed C57Bl/6 J mice. Nutrition & metabolism. 2013;10:44. doi: 10.1186/1743-7075-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Al M, Grimaldi M, Roecklin D, Dagnino S, Vivat-Hannah V, Balaguer P, Bourguet W. Activation of RXR–PPAR heterodimers by organotin environmental endocrine disruptors. EMBO Rep. 2009;10:367–373. doi: 10.1038/embor.2009.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chamorro-García R, Sahu M, Abbey Rachelle J, Laude J, Pham N, Blumberg B. Transgenerational inheritance of increased fat depot size, stem cell reprogramming, and hepatic Steatosis elicited by prenatal exposure to the Obesogen Tributyltin in mice. Environ Health Perspect. 2013;121:359–366. doi: 10.1289/ehp.1205701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmidt J-S, Schaedlich K, Fiandanese N, Pocar P, Fischer B. Effects of Di (2-ethylhexyl) phthalate (DEHP) on female fertility and Adipogenesis in C3H/N mice. Environ Health Perspect. 2012;120:1123–1129. doi: 10.1289/ehp.1104016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gapstur SM, Gann PH, Kopp P, Colangelo L, Longcope C, Liu K. Serum androgen concentrations in young men: a longitudinal analysis of associations with age, obesity, and race. The CARDIA male hormone study. Cancer Epidemiol Biomark Prev. 2002;11:1041–1047. [PubMed] [Google Scholar]
- 62.Pan G, Hanaoka T, Yoshimura M, Zhang S, Wang P, Tsukino H, Inoue K, Nakazawa H, Tsugane S, Takahashi K. Decreased serum free testosterone in workers exposed to high levels of di-n-butyl phthalate (DBP) and di-2-ethylhexyl phthalate (DEHP): a cross-sectional study in China. Environ Health Perspect. 2006;114:1643–1648. doi: 10.1289/ehp.9016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heindel JJ. History of the Obesogen field: looking Back to look forward. Front Endocrinol. 2019;10:14. doi: 10.3389/fendo.2019.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zoeller RT. Environmental chemicals impacting the thyroid: targets and consequences. Thyroid. 2007;17:811–817. doi: 10.1089/thy.2007.0107. [DOI] [PubMed] [Google Scholar]
- 65.Knudsen N, Laurberg P, Rasmussen LB, Bulow I, Perrild H, Ovesen L, Jorgensen T. Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population. J Clin Endocrinol Metab. 2005;90:4019–4024. doi: 10.1210/jc.2004-2225. [DOI] [PubMed] [Google Scholar]
- 66.D'Souza AM, Neumann UH, Glavas MM, Kieffer TJ. The glucoregulatory actions of leptin. Mol Metab. 2017;6:1052–1065. doi: 10.1016/j.molmet.2017.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 68.Farr OM, Gavrieli A, Mantzoros CS. Leptin applications in 2015: what have we learned about leptin and obesity? Curr Opinion Endocrinol Diab Obesity. 2015;22:353–359. doi: 10.1097/MED.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Woodward L, Akoumianakis I, Antoniades C. Unravelling the adiponectin paradox: novel roles of adiponectin in the regulation of cardiovascular disease. Br J Pharmacol. 2017;174:4007–4020. doi: 10.1111/bph.13619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF. A novel serum protein similar to C1q, Produced Exclusively in Adipocytes. J Biol Chem. 1995;270:26746–26749. doi: 10.1074/jbc.270.45.26746. [DOI] [PubMed] [Google Scholar]
- 71.Chamorro-Garcia R, Diaz-Castillo C, Shoucri BM, Kach H, Leavitt R, Shioda T, Blumberg B. Ancestral perinatal obesogen exposure results in a transgenerational thrifty phenotype in mice. Nat Commun. 2017;8:2012. doi: 10.1038/s41467-017-01944-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yan H, Guo H, Cheng D, Kou R, Zhang C, Si J. Tributyltin reduces the levels of serum adiponectin and activity of AKT and induces metabolic syndrome in male mice. Environ Toxicol. 2018;33:752–758. doi: 10.1002/tox.22562. [DOI] [PubMed] [Google Scholar]
- 73.Temkin AM, Bowers RR, Ulmer CZ, Penta K, Bowden JA, Nyland J, Baatz JE, Spyropoulos DD. Increased adiposity, inflammation, metabolic disruption and dyslipidemia in adult male offspring of DOSS treated C57BL/6 dams. Sci Rep. 2019;9:1530. doi: 10.1038/s41598-018-38383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Penza M, Montani C, Romani A, Vignolini P, Pampaloni B, Tanini A, Brandi ML, Alonso-Magdalena P, Nadal A, Ottobrini L, et al. Genistein affects adipose tissue deposition in a dose-dependent and gender-specific manner. Endocrinology. 2006;147:5740–5751. doi: 10.1210/en.2006-0365. [DOI] [PubMed] [Google Scholar]
- 75.Gu H, Liu Y, Wang W, Ding L, Teng W, Liu L. In utero exposure to di-(2-ethylhexyl) phthalate induces metabolic disorder and increases fat accumulation in visceral depots of C57BL/6J mice offspring. Exp Therapeutic Med. 2016;12:3806–3812. doi: 10.3892/etm.2016.3820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yin L, Yu KS, Lu K, Yu X. Benzyl butyl phthalate promotes adipogenesis in 3T3-L1 preadipocytes: a high content Cellomics and metabolomic analysis. Toxicol in Vitro. 2016;32:297–309. doi: 10.1016/j.tiv.2016.01.010. [DOI] [PubMed] [Google Scholar]
- 77.Lee RA, Harris CA, Wang J-C. Glucocorticoid receptor and adipocyte biology. Nuclear Receptor Res. 2018;5:101373. doi: 10.32527/2018/101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sargis RM, Johnson DN, Choudhury RA, Brady MJ. Environmental endocrine disruptors promote adipogenesis in the 3T3-L1 cell line through glucocorticoid receptor activation. Obesity (Silver Spring) 2010;18(7):1283–8. doi: 10.1038/oby.2009.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Toubal A, Treuter E, Clément K, Venteclef N. Genomic and epigenomic regulation of adipose tissue inflammation in obesity. Trends in Endocrinol Metab. 2013;24:625–634. doi: 10.1016/j.tem.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 80.de Araújo JFP, Podratz PL, Sena GC, Merlo E, Freitas-Lima LC, Ayub JGM, Pereira AFZ, Santos-Silva AP, Miranda-Alves L, Silva IV, Graceli JB. The obesogen tributyltin induces abnormal ovarian adipogenesis in adult female rats. Toxicol Lett. 2018;295:99–114. doi: 10.1016/j.toxlet.2018.06.1068. [DOI] [PubMed] [Google Scholar]
- 81.Sena GC, Freitas-Lima LC, Merlo E, Podratz PL, de Araújo JFP, Brandão PAA, Carneiro MTWD, Zicker MC, Ferreira AVM, Takiya CM, et al. Environmental obesogen tributyltin chloride leads to abnormal hypothalamic-pituitary-gonadal axis function by disruption in kisspeptin/leptin signaling in female rats. Toxicol Appl Pharmacol. 2017;319:22–38. doi: 10.1016/j.taap.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 82.Yang M, Chen M, Wang J, Xu M, Sun J, Ding L, Lv X, Ma Q, Bi Y, Liu R, et al. Bisphenol a promotes adiposity and inflammation in a nonmonotonic dose-response way in 5-week-old male and female C57BL/6J mice fed a low-calorie diet. Endocrinology. 2016;157:2333–2345. doi: 10.1210/en.2015-1926. [DOI] [PubMed] [Google Scholar]
- 83.Manteiga S, Lee K. Monoethylhexyl phthalate elicits an inflammatory response in adipocytes characterized by alterations in lipid and cytokine pathways. Environ Health Perspect. 2017;125:615–622. doi: 10.1289/EHP464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lu X, Luo S, Li H, Zhang X, Wu M, Du Z, Zhu Q, Shen T. Effects of IL-17 antibody on inflammation of adipose tissue in obese mice induced by bisphenol A. Wei Sheng Yan Jiu. 2018;47:945–955. [PubMed] [Google Scholar]
- 85.Veiga-Lopez A, Moeller J, Sreedharan R, Singer K, Lumeng C, Ye W, Pease A, Padmanabhan V. Developmental programming: interaction between prenatal BPA exposure and postnatal adiposity on metabolic variables in female sheep. Am J Phys Endocrinol Metab. 2016;310:E238–E247. doi: 10.1152/ajpendo.00425.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Malaisé Y, Menard S, Cartier C, Gaultier E, Lasserre F, Lencina C, Harkat C, Geoffre N, Lakhal L, Castan I, et al. Gut dysbiosis and impairment of immune system homeostasis in perinatally-exposed mice to Bisphenol a precede obese phenotype development. Sci Rep. 2017;7:14472. doi: 10.1038/s41598-017-15196-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ampem G, Junginger A, Yu H, Balogh L, Thuróczy J, Schneider ME, Röszer T. The environmental obesogen bisphenol a increases macrophage self-renewal. Cell Tissue Res. 2019;378:81–96. doi: 10.1007/s00441-019-03019-5. [DOI] [PubMed] [Google Scholar]
- 88.Welch JS, Ricote M, Akiyama TE, Gonzalez FJ, Glass CK. PPARgamma and PPARdelta negatively regulate specific subsets of lipopolysaccharide and IFN-gamma target genes in macrophages. Proc Natl Acad Sci U S A. 2003;100:6712–6717. doi: 10.1073/pnas.1031789100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jiang C, Ting AT, Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998;391:82–86. doi: 10.1038/34184. [DOI] [PubMed] [Google Scholar]
- 90.Ricote M, Li AC, Willson TM, Kelly CJ, Glass CK. The peroxisome proliferator-activated receptor-γ is a negative regulator of macrophage activation. Nature. 1998;391:79–82. doi: 10.1038/34178. [DOI] [PubMed] [Google Scholar]
- 91.Ricote M, Glass C. PPARs and molecular mechanisms of transrepression. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2007;1771:926–935. doi: 10.1016/j.bbalip.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Devchand PR, Keller H, Peters JM, Vazquez M, Gonzalez FJ, Wahli W. The PPARα–leukotriene B4 pathway to inflammation control. Nature. 1996;384:39–43. doi: 10.1038/384039a0. [DOI] [PubMed] [Google Scholar]
- 93.Szalkowski D, White-Carrington S, Berger J, Zhang B. Antidiabetic thiazolidinediones block the inhibitory effect of tumor necrosis factor-alpha on differentiation, insulin-stimulated glucose uptake, and gene expression in 3T3-L1 cells. Endocrinology. 1995;136:1474–1481. doi: 10.1210/endo.136.4.7895657. [DOI] [PubMed] [Google Scholar]
- 94.Lehmann JM, Moore LB, Smith-Oliver TA, Wilkison WO, Willson TM, Kliewer SA. An Antidiabetic thiazolidinedione is a high affinity ligand for peroxisome proliferator-activated receptor γ (PPARγ) J Biol Chem. 1995;270:12953–12956. doi: 10.1074/jbc.270.22.12953. [DOI] [PubMed] [Google Scholar]
- 95.Kanayama T, Kobayashi N, Mamiya S, Nakanishi T, Nishikawa J. Organotin compounds promote adipocyte differentiation as agonists of the peroxisome proliferator-activated receptor gamma/retinoid X receptor pathway. Mol Pharmacol. 2005;67:766–774. doi: 10.1124/mol.104.008409. [DOI] [PubMed] [Google Scholar]
- 96.Inadera H, Shimomura A. Environmental chemical tributyltin augments adipocyte differentiation. Toxicol Lett. 2005;159:226–234. doi: 10.1016/j.toxlet.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 97.Pereira-Fernandes A, Vanparys C, Hectors T, Vergauwen L, Knapen D, Jorens P, Blust R. Unraveling the mode of action of an obesogen: mechanistic analysis of the model obesogen tributyltin in the 3T3-L1 cell line. Mol Cell Endocrinol. 2013;370:52–64. doi: 10.1016/j.mce.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 98.Pereira-Fernandes Anna, Demaegdt Heidi, Vandermeiren Karine, Hectors Tine L. M., Jorens Philippe G., Blust Ronny, Vanparys Caroline. Evaluation of a Screening System for Obesogenic Compounds: Screening of Endocrine Disrupting Compounds and Evaluation of the PPAR Dependency of the Effect. PLoS ONE. 2013;8(10):e77481. doi: 10.1371/journal.pone.0077481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bastos Sales L, Kamstra JH, Cenijn PH, van Rijt LS, Hamers T, Legler J. Effects of endocrine disrupting chemicals on in vitro global DNA methylation and adipocyte differentiation. Toxicol In Vitro. 2013;27:1634–1643. doi: 10.1016/j.tiv.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 100.Chamorro-Garcia R, Kirchner S, Li X, Janesick A, Casey S, Chow C, Blumberg B. Bisphenol A Diglycidyl ether induces Adipogenic differentiation of multipotent stromal stem cells through a peroxisome proliferator-activated receptor gamma-independent mechanism. Environ Health Perspect. 2012;120:984–989. doi: 10.1289/ehp.1205063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Masuno H, Okamoto S, Iwanami J, Honda K, Shiosaka T, Kidani T, Sakayama K, Yamamoto H. Effect of 4-Nonylphenol on cell proliferation and adipocyte formation in cultures of fully differentiated 3T3-L1 cells. Toxicol Sci. 2003;75:314–320. doi: 10.1093/toxsci/kfg203. [DOI] [PubMed] [Google Scholar]
- 102.Helies-Toussaint C, Peyre L, Costanzo C, Chagnon M, Rahmani R. Is bisphenol S a safe substitute for bisphenol a in terms of metabolic function? An in vitro study. Toxicol Appl Pharmacol. 2014;280:224–235. doi: 10.1016/j.taap.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 103.Harmon Anne W., Harp Joyce B. Differential effects of flavonoids on 3T3-L1 adipogenesis and lipolysis. American Journal of Physiology-Cell Physiology. 2001;280(4):C807–C813. doi: 10.1152/ajpcell.2001.280.4.C807. [DOI] [PubMed] [Google Scholar]
- 104.Saito T, Abe D, Sekiya K. Flavanone exhibits PPAR gamma ligand activity and enhances differentiation of 3T3-L1 adipocytes. Biochem Biophys Res Commun. 2009;380:281–285. doi: 10.1016/j.bbrc.2009.01.058. [DOI] [PubMed] [Google Scholar]
- 105.Takahashi N, Goto T, Taimatsu A, Egawa K, Katoh S, Kusudo T, Sakamoto T, Ohyane C, Lee J, Kim Y, et al. Bixin regulates mRNA expression involved in adipogenesis and enhances insulin sensitivity in 3T3-L1 adipocytes through PPAR gamma activation. Biochem Biophys Res Commun. 2009;390:1372–1376. doi: 10.1016/j.bbrc.2009.10.162. [DOI] [PubMed] [Google Scholar]
- 106.Yang Y, Shang W, Zhou L, Jiang B, Jin H, Chen M. Emodin with PPAR gamma ligand-binding activity promotes adipocyte differentiation and increases glucose uptake in 3T3-Ll cells. Biochem Biophys Res Commun. 2007;353:225–230. doi: 10.1016/j.bbrc.2006.11.134. [DOI] [PubMed] [Google Scholar]
- 107.Feige J, Gelman L, Rossi D, Zoete V, Metivier R, Tudor C, Anghel S, Grosdidier A, Lathion C, Engelborghs Y, et al. The endocrine disruptor monoethyl-hexyl-phthalate is a selective peroxisome proliferator-activated receptor gamma modulator that promotes adipogenesis. J Biol Chem. 2007;282:19152–19166. doi: 10.1074/jbc.M702724200. [DOI] [PubMed] [Google Scholar]
- 108.Salam NK, Huang THW, Kota BP, Kim MS, Li YH, Hibbs DE. Novel PPAR-gamma agonists identified from a natural product library: a virtual screening, induced-fit docking and biological assay study. Chem Biol Drug Des. 2008;71:57–70. doi: 10.1111/j.1747-0285.2007.00606.x. [DOI] [PubMed] [Google Scholar]
- 109.Shannon M, Wilson J, Xie Y, Connolly L. In vitro bioassay investigations of suspected obesogen monosodium glutamate at the level of nuclear receptor binding and steroidogenesis. Toxicol Lett. 2019;301:11–16. doi: 10.1016/j.toxlet.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 110.Dang Z, Audinot V, Papapoulos S, Boutin J, Lowik C. Peroxisome proliferator-activated receptor gamma (PPAR gamma) as a molecular target for the soy phytoestrogen genistein. J Biol Chem. 2003;278:962–967. doi: 10.1074/jbc.M209483200. [DOI] [PubMed] [Google Scholar]
- 111.Wang RY, Abbott RD, Zieba A, Borowsky FE, Kaplan DL. Development of a three-dimensional adipose tissue model for studying embryonic exposures to obesogenic chemicals. Ann Biomed Eng. 2017;45:1807–1818. doi: 10.1007/s10439-016-1752-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Choi J, Gimble J, Vunjak-Novakovic G, Kaplan D. Effects of Hyperinsulinemia on Lipolytic function of three-dimensional adipocyte/endothelial co-cultures. Tissue Engineering Part C-Methods. 2010;16:1157–1165. doi: 10.1089/ten.tec.2009.0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bellas E, Marra K, Kaplan D. Sustainable three-dimensional tissue model of human adipose tissue. Tissue Engineering Part C-Methods. 2013;19:745–754. doi: 10.1089/ten.tec.2012.0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kato S, Kato Y, Shibata H, Saitoh Y, Miwa N. Repressive effects of oat extracts on intracellular lipid-droplet formation in adipocytes and a three-dimensional subcutaneous adipose tissue model. Materials Sci Engineering C-Materials For Biol Appl. 2015;49:269–273. doi: 10.1016/j.msec.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 115.Krontiras P, Gatenholm P, Hagg D. Adipogenic differentiation of stem cells in three-dimensional porous bacterial nanocellulose scaffolds. J Biomed Materials Res Part B-Appl Biomaterials. 2015;103:195–203. doi: 10.1002/jbm.b.33198. [DOI] [PubMed] [Google Scholar]
- 116.Kang X, Xie Y, Kniss D. Adipose tissue model using three-dimensional cultivation of preadipocytes seeded onto fibrous polymer scaffolds. Tissue Eng. 2005;11:458–468. doi: 10.1089/ten.2005.11.458. [DOI] [PubMed] [Google Scholar]
- 117.Frye C, Patrick C. Three-dimensional adipose tissue model using low shear bioreactors. In Vitro Cellular & Dev Biol Animal. 2006;42:109–114. doi: 10.1290/0509055.1. [DOI] [PubMed] [Google Scholar]
- 118.Fischbach C, Seufert J, Staiger H, Hacker M, Neubauer M, Gopferich A, Blunk T. Three-dimensional in vitro model of adipogenesis: comparison of culture conditions. Tissue Eng. 2004;10:215–229. doi: 10.1089/107632704322791862. [DOI] [PubMed] [Google Scholar]
- 119.Daquinag A, Souza G, Kolonin M. Adipose tissue engineering in three-dimensional levitation tissue culture system based on magnetic nanoparticles. Tissue Engineering Part C-Methods. 2013;19:336–344. doi: 10.1089/ten.tec.2012.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hartman JK, Beames T, Parks B, Doheny D, Song G, Efremenko A, Yoon M, Foley B, Deisenroth C, McMullen PD, Clewell RA. An in vitro approach for prioritization and evaluation of chemical effects on glucocorticoid receptor mediated adipogenesis. Toxicol Appl Pharmacol. 2018;355:112–126. doi: 10.1016/j.taap.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 121.Foley B, Doheny DL, Black MB, Pendse SN, Wetmore BA, Clewell RA, Andersen ME, Deisenroth C. Screening ToxCast prioritized chemicals for PPARG function in a human adipose-derived stem cell model of Adipogenesis. Toxicol Sci. 2017;155:85–100. doi: 10.1093/toxsci/kfw186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Niedo J, Tanimoto S, Thompson RH, Abbott RD, Berninger VW. Computerized instruction in translation strategies for students in upper elementary and middle school grades with persisting learning disabilities in written language. Learn Disabil (Pittsbg) 2016;21:14–30. doi: 10.18666/LDMJ-2016-V21-I2-7751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shi H, Clegg DJ. Sex differences in the regulation of body weight. Physiol Behav. 2009;97:199–204. doi: 10.1016/j.physbeh.2009.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Abbott RD, Wang RY, Reagan MR, Chen Y, Borowsky FE, Zieba A, Marra KG, Rubin JP, Ghobrial IM, Kaplan DL. The use of silk as a scaffold for mature, sustainable Unilocular adipose 3D tissue engineered systems. Adv Healthc Mater. 2016;5:1667–1677. doi: 10.1002/adhm.201600211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Darbre PD. Endocrine disruptors and obesity. Curr Obes Rep. 2017;6:18–27. doi: 10.1007/s13679-017-0240-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bujalska IJ, Kumar S, Hewison M, Stewart PM. Differentiation of adipose stromal cells: the roles of glucocorticoids and 11 beta-hydroxysteroid dehydrogenase. Endocrinology. 1999;140:3188–3196. doi: 10.1210/endo.140.7.6868. [DOI] [PubMed] [Google Scholar]
- 127.Chamorro-Garcia R, Blumberg B. Current research approaches and challenges in the Obesogen field. Front Endocrinol. 2019;10:167. doi: 10.3389/fendo.2019.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hao C, Cheng X, Guo J, Xia H, Ma X. Perinatal exposure to diethyl-hexyl-phthalate induces obesity in mice. Front Biosci (Elite Ed) 2013;5:725–733. doi: 10.2741/E653. [DOI] [PubMed] [Google Scholar]
- 129.Newbold RR, Padilla-Banks E, Snyder RJ, Jefferson WN. Developmental exposure to estrogenic compounds and obesity. Birth Defects Res A Clin Mol Teratol. 2005;73:478–480. doi: 10.1002/bdra.20147. [DOI] [PubMed] [Google Scholar]
- 130.Hao C, Cheng X, Xia H, Ma X. The endocrine disruptor mono-(2-ethylhexyl) phthalate promotes adipocyte differentiation and induces obesity in mice. Biosci Rep. 2012;32:619–629. doi: 10.1042/BSR20120042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yan Z, Zhang H, Maher C, Arteaga-Solis E, Champagne FA, Wu L, McDonald JD, Yan B, Schwartz GJ, Miller RL. Prenatal polycyclic aromatic hydrocarbon, adiposity, peroxisome proliferator-activated receptor (PPAR) gamma methylation in offspring, grand-offspring mice. PLoS One. 2014;9:e110706. doi: 10.1371/journal.pone.0110706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bolton JL, Auten RL, Bilbo SD. Prenatal air pollution exposure induces sexually dimorphic fetal programming of metabolic and neuroinflammatory outcomes in adult offspring. Brain Behav Immun. 2014;37:30–44. doi: 10.1016/j.bbi.2013.10.029. [DOI] [PubMed] [Google Scholar]
- 133.La Merrill M, Karey E, Moshier E, Lindtner C, La Frano MR, Newman JW, Buettner C. Perinatal exposure of mice to the pesticide DDT impairs energy expenditure and metabolism in adult female offspring. PLoS One. 2014;9:e103337. doi: 10.1371/journal.pone.0103337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Maull EA, Ahsan H, Edwards J, Longnecker MP, Navas-Acien A, Pi JB, Silbergeld EK, Styblo M, Tseng CH, Thayer KA, Loomis D. Evaluation of the association between arsenic and diabetes: a National Toxicology Program Workshop Review. Environ Health Perspect. 2012;120:1658–1670. doi: 10.1289/ehp.1104579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nguyen TLA, Vieira-Silva S, Liston A, Raes J. How informative is the mouse for human gut microbiota research? Dis Model Mech. 2015;8:1–16. doi: 10.1242/dmm.017400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Monteiro R, Azevedo I. Chronic inflammation in obesity and the metabolic syndrome. Mediat Inflamm. 2010;2010. [DOI] [PMC free article] [PubMed]
- 137.Strakovsky RS, Lezmi S, Shkoda I, Flaws JA, Helferich WG, Pan YX. In utero growth restriction and catch-up adipogenesis after developmental di (2-ethylhexyl) phthalate exposure cause glucose intolerance in adult male rats following a high-fat dietary challenge. J Nutr Biochem. 2015;26:1208–1220. doi: 10.1016/j.jnutbio.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Somm E, Schwitzgebel VM, Toulotte A, Cederroth CR, Combescure C, Nef S, Aubert ML, Huppi PS. Perinatal exposure to bisphenol a alters early adipogenesis in the rat. Environ Health Perspect. 2009;117:1549–1555. doi: 10.1289/ehp.11342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Badr El Dine FMM, Nabil IM, Dwedar FI. The effect of Tributyltin on thyroid follicular cells of adult male albino rats and the possible protective role of green tea: a toxicological, histological and biochemical study. Egypt J Forensic Sci. 2017;7:7. doi: 10.1186/s41935-017-0012-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Green AJ, Hoyo C, Mattingly CJ, Luo Y, Tzeng JY, Murphy SK, Buchwalter DB, Planchart A. Cadmium exposure increases the risk of juvenile obesity: a human and zebrafish comparative study. Int J Obes. 2018;42:1285–1295. doi: 10.1038/s41366-018-0036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lyssimachou Angeliki, Santos Joana G., André Ana, Soares Joana, Lima Daniela, Guimarães Laura, Almeida C. Marisa R., Teixeira Catarina, Castro L. Filipe C., Santos Miguel M. The Mammalian “Obesogen” Tributyltin Targets Hepatic Triglyceride Accumulation and the Transcriptional Regulation of Lipid Metabolism in the Liver and Brain of Zebrafish. PLOS ONE. 2015;10(12):e0143911. doi: 10.1371/journal.pone.0143911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tingaud-Sequeira A, Ouadah N, Babin PJ. Zebrafish obesogenic test: a tool for screening molecules that target adiposity. J Lipid Res. 2011;52:1765–1772. doi: 10.1194/jlr.D017012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Punzon I, Latapie V, Le Mevel S, Hagneau A, Jolivet P, Palmier K, Fini JB, Demeneix BA. Towards a humanized PPAR gamma reporter system for in vivo screening of obesogens. Mol Cell Endocrinol. 2013;374:1–9. doi: 10.1016/j.mce.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 144.Rhrissorrakrai K, Belcastro V, Bilal E, Norel R, Poussin C, Mathis C, Dulize RH, Ivanov NV, Alexopoulos L, Rice JJ, et al. Understanding the limits of animal models as predictors of human biology: lessons learned from the sbv IMPROVER species translation challenge. Bioinformatics. 2015;31:471–483. doi: 10.1093/bioinformatics/btu611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hatch EE, Nelson JW, Stahlhut RW, Webster TF. Association of endocrine disruptors and obesity: perspectives from epidemiological studies. Int J Androl. 2010;33:324–332. doi: 10.1111/j.1365-2605.2009.01035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Buckley JP, Engel SM, Braun JM, Whyatt RM, Daniels JL, Mendez MA, Richardson DB, Xu YY, Calafat AM, Wolff MS, et al. Prenatal phthalate exposures and body mass index among 4-to 7-year-old children: a pooled analysis. Epidemiology. 2016;27:449–458. doi: 10.1097/EDE.0000000000000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Valvi D, Casas M, Mendez MA, Ballesteros-Gomez A, Luque N, Rubio S, Sunyer J, Vrijheid M. Prenatal Bisphenol a urine concentrations and early rapid growth and overweight risk in the offspring. Epidemiology. 2013;24:791–799. doi: 10.1097/EDE.0b013e3182a67822. [DOI] [PubMed] [Google Scholar]
- 148.Braun Joseph M, Gennings C, Hauser R, Webster Thomas F. What can epidemiological studies tell us about the impact of chemical mixtures on human health? Environ Health Perspect. 2016;124:A6–A9. doi: 10.1289/ehp.1509880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Needham LL, Calafat AM, Barr DB. Assessing developmental toxicant exposures via biomonitoring. Basic & clinical pharmacology & toxicology. 2008;102:100–108. doi: 10.1111/j.1742-7843.2007.00185.x. [DOI] [PubMed] [Google Scholar]
- 150.Savitz DA. Invited commentary: interpreting associations between exposure biomarkers and pregnancy outcome. Am J Epidemiol. 2014;179:545–547. doi: 10.1093/aje/kwt314. [DOI] [PubMed] [Google Scholar]
- 151.Sharpe RM, Drake AJ. Obesogens and obesity—an alternative view? Obesity. 2013;21:1081–1083. doi: 10.1002/oby.20373. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.