Abstract
Especially since the incorporation of swept laser sources, optical coherence tomography angiography (OCTA) has enabled quantification of choriocapillaris perfusion. A critical step in this process is binarization, which makes angiographic images quantifiable in terms of perfusion metrics. It remains challenging to have confidence that choriocapillaris perfusion metrics reflect the reality of pathophysiologic flow, largely because choice of binarization method can result in significantly different perfusion metric outcomes. This commentary discusses a proof-of-concept case involving comparative assessment of binarization methods for a set of dry age-related macular degeneration OCTA data. One of these methods was deemed preferable based on superior agreement with suspected physiologic and pathophysiologic characteristics, thus demonstrating the principle that, in the absence of gold standards for measurement of choriocapillaris perfusion, the best available approximations of pathophysiology may be used to guide choice of binarization method.
Keywords: binarization, quantification, choriocapillaris, OCTA, AMD
The Challenge of Binarizing Choriocapillaris Flow on OCTA
Optical coherence tomography angiography (OCTA) is an extension of the OCT imaging technology along the time dimension: When controlling for motion artifact, the only detectable difference between repeated B-scans at the same retinal location is due to movement of erythrocytes. By recording this decorrelation signal—the difference between a temporal sequence of B-scans—across lateral space, as in an OCT cube scan, it is possible to reconstruct blood flow in the various retinal plexuses. This has enabled the non-invasive, depth-resolved, in vivo exploration of retinal perfusion, a capability that has many research and clinical implications.1
The recent availability of longer wavelength, swept-source OCTA instruments has enabled enhanced signal penetration beneath scattering and/or attenuating structures, such as the retinal pigment epithelium or drusen, so that choriocapillaris (CC) perfusion may be better visualized.2 However, there remain a number of features that make CC perfusion uniquely difficult to quantify accurately in physiologic and pathologic conditions. One of these challenges occurs at the image processing step known as binarization, which uses a thresholding algorithm to convert 8-bit (grayscale pixel values coded on a scale of 0–255) OCTA images to black and white (binary pixel values) images representing non-flow and flow, respectively. There is currently no consensus on binarization practice, and choice of binarization method has been shown to result in significantly different flow deficit metrics.3–5 Thus, binarization could benefit from a more concerted effort at physiologic and pathophysiologic grounding.
This has not been a straightforward task, however. Unlike more superficial vasculature, the discontinuous appearance of the CC on en face images precludes the use of vessel continuity as a physiologic reference. Furthermore, established retinal imaging techniques (such as fluorescein angiography and fundus photography) are not available as accepted ground truths for comparison. Indeed, ground truths of any kind for CC flow measurement are absent.6 Although histology can be informative, it is limited to describing post mortem structure rather than in vivo function, meaning its use is restricted to judicious inference. Previous OCTA studies may also be informative, assuming these prior OCTA findings are robust and reproducible and when somewhat different methodologies arrive at similar conclusions. An example of this is the set of studies that found a positive association between advancing age and increasing CC flow deficit metrics.7–10 However, confirmation of previous OCTA findings in itself, without additional grounding in the reality of CC structure and function, may simply perpetuate erroneous conclusions due to, for example, a systematic error in image acquisition or processing.
There have been some commendable efforts that have worked toward physiologic grounding of CC perfusion as imaged with OCTA, typically in normal eyes. For example, the OCTA methodologies used by Spaide7 and Alten et al.10 suggested decreased macular perfusion with advancing age, a conclusion well supported by histology.11,12 Zhang et al.13 suggested the increased accuracy of applying a lower flow deficit area threshold to account for histologically anchored intercapillary distance. It has been observed that, to the extent possible, binarized CC images should make sense from a qualitative perspective, for example, by displaying peripheral macular lobularity and by gross resemblance to the pre-binarized angiogram.5,14 Selection of binarization method should make use of information from such attempts at physiologic grounding. More work must be done on accurate binarization, however, particularly in diseased eyes if studies involving diseased eyes are to make pathophysiologic claims. At the current stage of OCTA CC research, as ground truths and pathophysiologic reference characteristics are lacking or incomplete, the best that may be done with respect to selection of binarization method is a wariness of implausibility and argument for the reasonableness of a chosen method based on suspected pathophysiology. However, any conclusions about pathophysiology should be appropriately qualified. In particular, it should be clearly acknowledged that extent of confidence in choice of binarization method depends directly on extent of confidence that the hypothesized reality of CC flow conforms to the true reality of CC flow.
A Case
Recently, our group completed a study that suggested that dry age-related macular degeneration (AMD) stage had a statistically significant relationship with macular CC flow deficit metrics (Table 1).15 The Phansalkar local binarization method, based on the mean and standard deviation of grayscale values within a given radius (15 pixels in this study), was developed for effective binarization in low-contrast settings.3,5 It was used in this study because of the low-contrast character of the CC, its prevalence in the literature,8,16,17 its compatibility with the known structure of the CC,7 and reports of its reasonable approximation of average flow deficit size.3 Upon further analysis, there were at least five additional arguments that Phansalkar local binarization (radius, 15 pixels) was a reasonable method for our study, most of which can be elucidated by considering the summary statistics of the study (Table 2). For orientation, columns in Table 2 show flow deficit metrics (flow deficit percentage and average flow deficit size) and dry AMD stage for 6 × 6-mm, macula-centered en face images at the level of the CC. The rows show regions of analysis with sizes (e.g., 1 mm) representing the diameter of a circle centered on the fovea; rings exclude either a 1-mm-diameter central area (3-mm ring) or a 3-mm-diameter central area (5-mm ring). Staging was based on clinical trial criteria,18 with areas of geographic atrophy (GA) excluded from analysis to minimize detection of flow from inwardly displaced choroidal vessels.
-
1.
With rare exception, there is an increase in both flow deficit metrics from the early stage through the advanced stage. This might be expected based on OCTA and histology studies that have found flow or vessel impairment beneath drusen and around GA lesions17,19–22 and progressively by dry AMD stage.12,23 Even if stage is minimally contributory to flow deficit metrics, this trend is consistent with the findings of multiple studies of age in the CC,7–12 as there was a respective increase in the mean ages of early, intermediate, and advanced eyes in our cohort (early, intermediate, and advanced eye mean ages: 72, 77, and 81 years, respectively).
-
2.
There is a trend toward convergence of flow deficit metrics among stages in more peripheral regions. If advancing stage is indeed positively associated with increasing age, and age has less of an association with CC flow deficit in peripheral regions,8,9 then the diminished difference in flow deficit metrics among stages in these regions is not surprising.
-
3.
Within each stage there is a trend of decreasing flow deficit metrics from central to peripheral regions. This is logical if these trends are substantially influenced by age, which as noted above has a stronger association with flow deficit centrally versus peripherally. Such topographic influence is supported by modeling showing a strong correlation between age and macular CC flow deficit in eyes with dry AMD.15 Although this support is weakened by self-referentiality (this modeling relies upon the very binarization parameters whose reasonableness is being argued for here), we still think this argument worth making by a previously advocated principle—namely, the cautious utility of disparate methods converging on similar conclusions. A strong correlation between age and macular CC flow deficit in eyes with dry AMD was also affirmed with binarization parameters—Otsu global and Phansalkar local (3-pixel radius), both discussed below—other than the Phansalkar local (15-pixel radius) method used in the referenced modeling.
-
4.
Standard deviations are, without exception, smallest in the early stage to largest in the advanced stage. It is reasonable to think that there would be lower variation in patients with minimal disease (early) versus those with widely variable drusen burden (intermediate) versus those with disease that is phenotypically most diverse (advanced), ranging from barely hypertransmissive nascent GA to severe GA.
-
5.
Flow deficit percentage and average flow deficit size are positively correlated across stages and regions of analysis. Anatomically, this ought to be the case, because when flow deficit percentage increases, assumedly due to real or effective CC vessel loss, the space between areas of flow (average flow deficit size) should enlarge. This principle was recently demonstrated quantitatively by Shi et al.14
Table 1.
Summary of Case Study Used to Discuss an Approach to Binarization Method Selection
| Study question | Does dry AMD stage have a statistically significant relationship with macular choriocapillaris perfusion and, if so, how does this vary topographically? |
| Study findings | There is a statistically significant relationship between dry AMD stage and macular choriocapillaris perfusion that is most prominent in more peripheral macular regions. |
| Sample size | 56 eyes with dry AMD from 41 patients; 23 early, 12 intermediate, and 21 advanced |
| Image characteristics | 6 × 6-mm en face, macula-centered OCTA images composed of 500 B-scans at 500 A-scans per B-scan |
| Instrument | PLEX Elite 9000 (Carl Zeiss Meditec, Dublin, CA, USA) |
| Image analysis | ImageJ 1.52h |
| Binarization method | Phansalkar local (15-pixel radius) |
| Modeling | Linear (generalized estimating equations) |
Table 2.
Summary Statistics for All Dry AMD Stages and Regions of Analysis Using the Phansalkar Local Threshold (Radius, 15 Pixels)
| FD% | Average Flow Deficit Size (µm2) | |||||
|---|---|---|---|---|---|---|
| Early | Intermediate | Advanced | Early | Intermediate | Advanced | |
| 1-mm area | ||||||
| Mean (SD) | 26.9 (3.2) | 31.7 (7.4) | 33.9 (8.0) | 710.7 (230.0) | 944.1 (593.9) | 1349.2 (834.3) |
| [Range] | [22.0–35.5] | [23.9–45.0] | [20.0–46.6] | [381.1–1407.6] | [418.9–2053.1] | [326.2–3457.2] |
| 3-mm ring | ||||||
| Mean (SD) | 26.4 (3.2) | 29.8 (5.7) | 36.6 (11.6) | 700.4 (219.7) | 796.5 (394.8) | 1479.7 (1023.1) |
| [Range] | [22.1–32.7] | [22.5–38.6] | [18.7–58.1] | [370.8–1119.2] | [377.7–1606.7] | [315.9–3701.0] |
| 5-mm area | ||||||
| Mean (SD) | 25.6 (2.8) | 27.3 (4.4) | 32.1 (7.4) | 676.3 (192.3) | 672.9 (291.8) | 1239.4 (748.4) |
| [Range] | [20.7–31.8] | [20.8–34.2] | [18.4–43.4] | [384.5–1054.0] | [353.6–1263.4] | [309.0–2763.7] |
| 5-mm ring | ||||||
| Mean (SD) | 25.3 (2.9) | 25.8 (3.8) | 31.4 (7.4) | 655.7 (192.3) | 587.1 (240.3) | 1157.0 (676.3) |
| [Range] | [19.7–31.3] | [19.6–32.1] | [18.2–43.0] | [381.1–1005.9] | [329.6–1060.9] | [298.7–2396.4] |
| Whole image | ||||||
| Mean (SD) | 25.2 (2.9) | 25.9 (3.8) | 30.1 (6.4) | 66 9.5 (192.3) | 604.2 (247.2) | 1050.6 (535.6) |
| [Range] | [19.5–31.9] | [19.5–31.8] | [18.6–39.2] | [394.8–1084.9] | [336.5–1091.8] | [315.9–2087.4] |
Values in bold represent regions with a statistically significant relationship between dry AMD stage and flow deficit percentage or average flow deficit size—specifically in comparing intermediate versus advanced stages (5-mm ring for flow deficit percentage; 3-mm ring, 5-mm area, 5-mm ring, and whole image for average flow deficit size) and early versus intermediate stages (5-mm ring and whole image for average flow deficit size). Based on table © Braun et al. in Investigative Ophthalmology & Visual Science under CC BY-NC-ND 4.0 license.
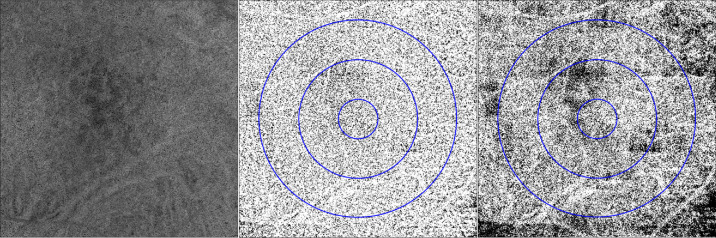
For contrast, the results of our study were compared with those that instead employed an Otsu global threshold, which is based on minimizing grayscale variance within above-threshold and below-threshold classes and which has also been used in analysis of OCTA metrics, including on CC angiograms.3,24,25 The study method was otherwise repeated exactly, and cohort characteristics remained the same. The Figure shows an example of the same angiogram after the binarization step in our study, using the Phansalkar local and Otsu methods. Use of the Otsu method, inferior for CC analysis from a theoretical standpoint due to the non-bimodal character of the en face CC histogram,26 resulted in notable departures from the five arguments above with respect to summary statistics (Table 3). For example, it is unlikely that, due to some combination of lowest age and least severity of the three stages, early eyes would have the highest flow deficit percentage among all stages (5-mm area, 5-mm ring, and whole image). Or, again, there are regions of analysis (average flow deficit size for the 5-mm ring and whole image) where the standard deviation for early eyes is greater than that for intermediate eyes. Importantly, the Otsu global threshold does not clearly seem to offer alternative arguments that would support its superiority with respect to pathophysiologic accuracy in this case, based on what is suspected about actual flow in dry AMD. It might well have done so if, for example, actual flow deficits were definitively determined to be closer to the larger values found with Otsu binarization, but because this pathophysiologic reality is not well understood, it cannot be used as a reference in selection of binarization method.
Figure.
Example of 6 × 6-mm, macula-centered choriocapillaris angiogram from eye with intermediate AMD (original, left) after binarization with the Phansalkar local method, radius 15 pixels (center), versus the Otsu global method (right). Per the analysis in our study investigating the relationship between dry AMD stage and CC flow deficit metrics, each image previously underwent compensation for signal attenuation beneath drusen. Flow is shown in white, and regions of analysis corresponding to those in Tables 2 and 3 are shown by the blue overlay.
Table 3.
Summary Statistics for All Dry AMD Stages and Regions of Analysis Using the Otsu Global Threshold
| FD% | Average Flow Deficit Size (µm2) | |||||
|---|---|---|---|---|---|---|
| Early | Intermediate | Advanced | Early | Intermediate | Advanced | |
| 1-mm area | ||||||
| Mean (SD) | 40.2 (6.6) | 45.6 (8.8) | 43.0 (10.2) | 2011.9 (1572.4) | 2599.0 (2262.5) | 2588.7 (2252.2) |
| [Range] | [28.9–58.7] | [36.6–63.0] | [19.6–63.2] | [731.3–8411.4] | [985.3–7875.8] | [367.4–1.0E5] |
| 3-mm ring | ||||||
| Mean (SD) | 43.5 (5.4) | 44.5 (5.6) | 48.4 (11.7) | 2595.5 (1287.5) | 2173.2 (1383.6) | 3488.2 (2767.2) |
| [Range] | [34.8–51.9] | [37.4–54.7] | [33.5–78.4] | [892.6–480.7] | [954.4–5352.4] | [803.4–1.2E5] |
| 5-mm area | ||||||
| Mean (SD) | 42.2 (3.6) | 40.8 (4.0) | 41.5 (8.9) | 2265.9 (824.0) | 1692.6 (878.9) | 2386.1 (1407.6) |
| [Range] | [35.2–47.1] | [35.4–48.7] | [17.7–54.2] | [937.3–3495.0] | [909.8–3481.3] | [309.0–5503.5] |
| 5-mm ring | ||||||
| Mean (SD) | 41.8 (3.6) | 38.4 (3.8) | 40.8 (8.8) | 2108.0 (786.2) | 1400.8 (679.8) | 2193.8 (1301.2) |
| [Range] | [34.3–47.4] | [34.2–45.7] | [17.7–53.3] | [858.3–3278.7] | [837.7–2746.6] | [309.0–4906.1] |
| Whole image | ||||||
| Mean (SD) | 41.5 (3.0) | 38.6 (3.4) | 38.4 (7.3) | 2152.6 (758.7) | 1442.0 (707.2) | 1850.5 (875.5) |
| [Range] | [36.3–46.3] | [34.5–46.2] | [19.6–49.7] | [1023.1–3337.1] | [878.9–2986.9] | [422.3–4095.8] |
Values in bold represent regions with a statistically significant relationship between dry AMD stage and flow deficit percentage or average flow deficit size—specifically in comparing early versus intermediate stages (5-mm area, 5-mm ring, and whole image for flow deficit percentage; 3-mm ring, 5-mm area, 5-mm ring, and whole image for average flow deficit size) and early versus advanced stages (whole image for average flow deficit size).
None of this is to argue that the Phansalkar local method with the parameters we used was the most accurate, but there is cause to think it was a reasonable technique to use for this study. Very recent work on the Phansalkar local method by Chu et al.,5,26 particularly as it relates to intercapillary distance, leads us to believe that, were we to repeat this study, a pixel radius of 2 to 4 would likely be more appropriate. Although re-analysis shows that use of this smaller radius instead of a 15-pixel radius does not radically alter the conclusions of the study—there remains a relationship between dry AMD stage and CC flow deficit that is most prominent in more peripheral macular regions—it is a good example of the iterative refinement critically needed in the field of CC flow quantification.
Conclusions
In the current absence of ground truths for OCTA studies of physiologic and pathophysiologic CC flow, choosing a binarization method can be a challenge; however, it seems reasonable to think that histology and prior OCTA studies can provide a useful reference for approaching the physiologic reality of CC flow. Only one example of this strategy has been discussed in this article, but a more expansive exploration of binarization in the context of a diversity of pathologies—alongside healthy CC anatomy and physiology—has the potential to make strides toward addressing the problem of accurate binarization. Effectively, the identification of an increasing number of anatomic and approximate physiologic CC characteristics in both health and disease could provide an increasingly refined set of criteria by which to judge the success of binarization methods with respect to physiologic fidelity.
Acknowledgments
Supported by the Macula Vision Research Foundation (West Conshohocken, PA), Massachusetts Lions Clubs (Belmont, MA), National Institutes of Health (grant no. 5-R01-EY011289-31), Air Force Office of Scientific Research (grant no. FA9550-15-1-0473), Champalimaud Vision Award (Lisbon, Portugal), Beckman–Argyros Award in Vision Research (Irvine, CA), Yale School of Medicine Medical Student Fellowship (New Haven, CT), National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Medical Student Research Fellowship, National Institutes of Health Clinical and Translational Science Award Multidisciplinary Pre-Doctoral Training Program in Translational Research (New Haven, CT), and Research to Prevent Blindness Challenge Grant (New York, NY). The funding organizations had no role in the design or conduct of this research.
Disclosure: P.X. Braun, None; N. Mehta, None; I. Gendelman, None; A.Y. Alibhai, None; C.R. Baumal, Genentech (C), Carl Zeiss Meditec, Inc. (S); J.S. Duker, Carl Zeiss Meditec, Inc. (F, C), Optovue, Inc. (F, C); N.K. Waheed, Topcon Medical Systems, Inc. (F), Nidek Medical Products, Inc. (F, S), Carl Zeiss Meditec, Inc. (F), Optovue, Inc. (C)
References
- 1. Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Prog Retin Eye Res. 2018; 64: 1–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moult EM, Waheed NK, Novais EA, et al.. Swept-source optical coherence tomography angiography reveals choriocapillaris alterations in eyes with nascent geographic atrophy and drusen-associated geographic atrophy. Retina. 2016; 36(suppl 1): S2–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mehta N, Liu K, Alibhai AY, et al.. Impact of binarization thresholding and brightness/contrast adjustment methodology on optical coherence tomography angiography image quantification. Am J Ophthalmol. 2019; 205: 54–65. [DOI] [PubMed] [Google Scholar]
- 4. Rabiolo A, Gelormini F, Sacconi R, et al.. Comparison of methods to quantify macular and peripapillary vessel density in optical coherence tomography angiography. PLoS One. 2018; 13: e0205773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chu Z, Cheng Y, Zhang Q, et al.. Quantification of choriocapillaris with Phansalkar's local thresholding: pitfalls to avoid. Am J Ophthalmol. 2020; 213: 161–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chu Z, Zhang Q, Zhou H, et al.. Quantifying choriocapillaris flow deficits using global and localized thresholding methods: a correlation study. Quant Imaging Med Surg. 2018; 8: 1102–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Spaide RF. Choriocapillaris flow features follow a power law distribution: implications for characterization and mechanisms of disease progression. Am J Ophthalmol. 2016; 170: 58–67. [DOI] [PubMed] [Google Scholar]
- 8. Nassisi M, Baghdasaryan E, Tepelus T, Asanad S, Borrelli E, Sadda SR. Topographic distribution of choriocapillaris flow deficits in healthy eyes. PLoS One. 2018; 13: e0207638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zheng F, Zhang Q, Shi Y, et al.. Age-dependent changes in the macular choriocapillaris of normal eyes imaged with swept-source optical coherence tomography angiography. Am J Ophthalmol. 2019; 200: 110–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alten F, Heiduschka P, Clemens CR, Eter N. Exploring choriocapillaris under reticular pseudodrusen using OCT-angiography. Graefes Arch Clin Exp Ophthalmol. 2016; 254: 2165–2173. [DOI] [PubMed] [Google Scholar]
- 11. Ramrattan RS, van der Schaft TL, Mooy CM, de Bruijn WC, Mulder PG, de Jong PT. Morphometric analysis of Bruch's membrane, the choriocapillaris, and the choroid in aging. Invest Ophthalmol Vis Sci. 1994; 35: 2857–2864. [PubMed] [Google Scholar]
- 12. Seddon JM, McLeod DS, Bhutto IA, et al.. Histopathological insights into choroidal vascular loss in clinically documented cases of age-related macular degeneration. JAMA Ophthalmol. 2016; 134: 1272–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang Q, Shi Y, Zhou H, et al.. Accurate estimation of choriocapillaris flow deficits beyond normal intercapillary spacing with swept source OCT angiography. Quant Imaging Med Surg. 2018; 8: 658–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shi Y, Zhang Q, Zheng F, et al.. Correlations between different choriocapillaris flow deficit parameters in normal eyes using swept source OCT angiography. Am J Ophthalmol. 2020; 209: 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Braun PX, Mehta N, Gendelman I, et al.. Global analysis of macular choriocapillaris perfusion in dry age-related macular degeneration using swept-source optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2019; 60: 4985–4990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nassisi M, Baghdasaryan E, Borrelli E, Ip M, Sadda SR. Choriocapillaris flow impairment surrounding geographic atrophy correlates with disease progression. PLoS One. 2019; 14: e0212563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Borrelli E, Shi Y, Uji A, et al.. Topographic analysis of the choriocapillaris in intermediate age-related macular degeneration. Am J Ophthalmol. 2018; 196: 34–43. [DOI] [PubMed] [Google Scholar]
- 18. National Institutes of Health. Non Exudative AMD Imaged with SS-OCT (BIRC-01). Available at: https://ClinicalTrials.gov/show/NCT03688243. Accessed March 21, 2019.
- 19. Borrelli E, Uji A, Sarraf D, Sadda SR. Alterations in the choriocapillaris in intermediate age-related macular degeneration. Invest Ophthalmol Vis Sci. 2017; 58: 4792–4798. [DOI] [PubMed] [Google Scholar]
- 20. Mullins RF, Johnson MN, Faidley EA, Skeie JM, Huang J. Choriocapillaris vascular dropout related to density of drusen in human eyes with early age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011; 52: 1606–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Choi W, Moult EM, Waheed NK, et al.. Ultrahigh-speed, swept-source optical coherence tomography angiography in nonexudative age-related macular degeneration with geographic atrophy. Ophthalmology. 2015; 122: 2532–2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nassisi M, Shi Y, Fan W, et al.. Choriocapillaris impairment around the atrophic lesions in patients with geographic atrophy: a swept-source optical coherence tomography angiography study. Br J Ophthalmol. 2019; 103: 911–917. [DOI] [PubMed] [Google Scholar]
- 23. Biesemeier A, Taubitz T, Julien S, Yoeruek E, Schraermeyer U. Choriocapillaris breakdown precedes retinal degeneration in age-related macular degeneration. Neurobiol Aging. 2014; 35: 2562–2573. [DOI] [PubMed] [Google Scholar]
- 24. Arya M, Rebhun CB, Alibhai AY, et al.. Parafoveal retinal vessel density assessment by optical coherence tomography angiography in healthy eyes. Ophthalmic Surg Lasers Imaging Retina. 2018; 49: S5–S17. [DOI] [PubMed] [Google Scholar]
- 25. Al-Sheikh M, Falavarjani KG, Pfau M, Uji A, Le PP, Sadda SR. Quantitative features of the choriocapillaris in healthy individuals using swept-source optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina. 2017; 48: 623–631. [DOI] [PubMed] [Google Scholar]
- 26. Chu Z, Gregori G, Rosenfeld PJ, Wang RK. Quantification of choriocapillaris with optical coherence tomography angiography: a comparison study. Am J Ophthalmol. 2019; 208: 111–123. [DOI] [PMC free article] [PubMed] [Google Scholar]