Abstract
Objectives
To investigate the feasibility and acceptability of telemedicine as a substitute for outpatient services in emergency situations such as the sudden surge of the COVID-19 pandemic in Italy.
Design
Observational cohort study with historical control.
Setting
Tertiary referral outpatient institute.
Participants
Consecutive services provided to patients with spinal disorders (N=1207).
Interventions
Telemedicine services included teleconsultations and telephysiotherapy, and lasted as long as usual interventions. They were delivered using free teleconference apps, caregivers were actively involved, and interviews and counseling were performed as usual. Teleconsultations included standard, but adapted, measurements and evaluations by video and from photographs and videos sent in advance according to specific tutorials. During telephysiotherapy, new sets of exercises were defined and recorded as usual.
Main Outcome Measures
We compared the number of services provided in 3 phases, including corresponding periods in 2018 and 2019. During the control (30 working d) and COVID-19 surge (13d) only usual consultations and physiotherapy were provided; during the telemed phase (15d), only teleconsultations and telephysiotherapy were provided. If a reliable medical decision was not possible during teleconsultations, usual face-to-face interventions were prescribed. Continuous quality improvement questionnaires were also evaluated.
Results
During telemed, 325 teleconsulations and 882 telephysiotherapy sessions were provided in 15 days. We found a rapid decrease (–39%) of outpatient services from the control to the COVID-19 phase (R2=0.85), which partially recovered in the telemed phase for telephysiotherapy (from –37% to –21%; P<.05) and stabilized for teleconsultation (from –55% to –60%) interventions. Usual face-to-face interventions were required for 0.5% of patients. Patients’ satisfaction with telemedicine was very high (2.8 out of 3).
Conclusions
Telemedicine is feasible and allows medical professionals to continue providing outpatient services with a high level of patient satisfaction. During the current pandemic, this experience can provide a viable alternative for many outpatient services while reducing the need for travel and face-to-face contact to a minimum.
Keywords: Epidemics, Outpatients, Rehabilitation, Telemedicine, Telerehabilitation
List of abbreviations: COVID-19, coronavirus disease 2019
With the spread of coronavirus disease 2019 (COVID-19) around the world, the World Health Organization declared it a pandemic.1 China responded with a total quarantine of the affected areas to eradicate the virus.2 Italy and most other countries adopted a partial quarantine to mitigate the epidemic.3 This strategy aimed to decrease the heavy effect on the health systems and allow hospitalization and intensive care of the large number of patients in need, reducing the overall mortality.4
The COVID-19 emergency has affected not only infected patients but also all others.5 In many countries, outpatient services have been fully closed owing to the need of physicians to treat COVID-19 patients and the need to reduce the risk of infection resulting from travels. Consequently, outpatients are on their own and mostly self-managing. This is not acceptable for diseases that can still have sudden, important progressions, even in a few months, and it is even less acceptable in children.6 These groups could become collateral damage of the COVID-19 emergency.
Telemedicine is defined as the exchange of medical information using electronic tools. It has multiple applications and can be used to provide different services, including consultations and physiotherapy. Telemedicine has been shown to be effective in specific areas of care, particularly where technology is involved or medical “hands-on” techniques are less important.7 To our knowledge, there are no published results regarding the application of telemedicine to patients with spinal deformities.
With the sudden COVID-19 emergency in Italy, and the subsequent mobility restrictions, we have been forced to convert completely to telemedicine and rapidly develop specific ad-hoc solutions to continue to provide our outpatient services, including hands-on physiotherapy and medical evaluations, to our patients. We are not aware of any studies reporting such a total conversion for either medical consultations (teleconsultations) or physiotherapy sessions (telephysiotherapy).
The aim of this study is to report the feasibility and acceptability of telemedicine as a substitute to the usual tertiary referral outpatient rehabilitation services. We evaluated the numeric effect on services of (1) the surge of COVID-19 in Italy and (2) the subsequent complete, immediate and enforced shift to telemedicine (teleconsultations and telephysiotherapy). This experience will inform present and future emergency situations resulting in total or partial lockdown, as well as other conditions precluding transportation.
Methods
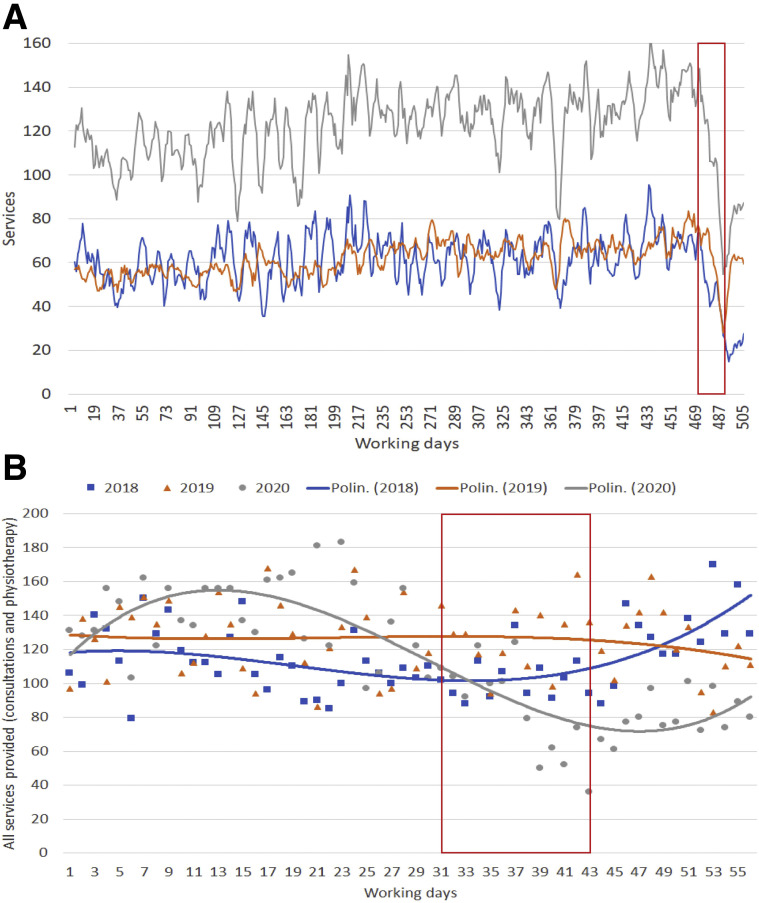
The COVID-19 epidemic in Italy was already underway on February 24, 2020 when immediate red zones (total quarantine) were imposed close to Milan. This did not reflect immediately on the services provided, but the partial quarantine throughout the country, with the closure of schools on March 2 and travel restrictions implemented on March 8, resulted in a clear drop of services (fig 1 A). This reduction, and the safety of patients and health professionals, urged the decision to move all activities of our institute to telemedicine on the same day of the Prime Minister’s decree to shut down all commercial activities (March 11). On March 16, all usual face-to-face services were stopped, unless required after telemedicine.
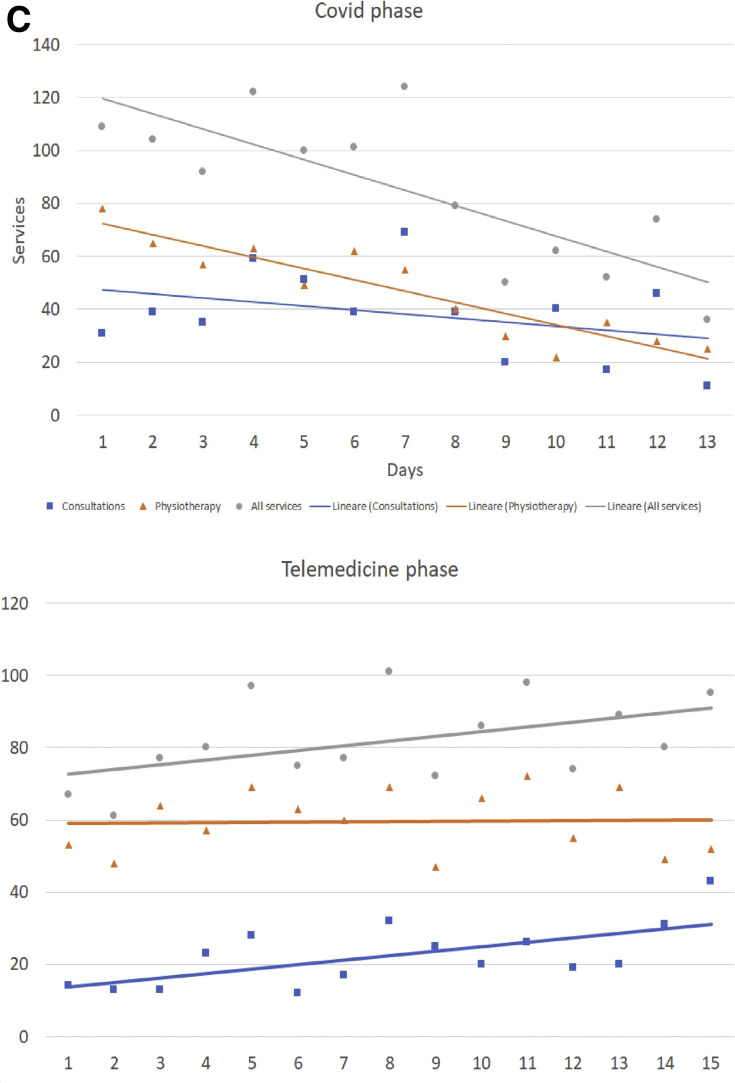
Fig 1.
(A) Evolution of outpatient services provided from January 7, 2018 to March 28, 2020. Vertical lines refer to the start of the observation periods: COVID-19 emergency (February 24) and the start of telemedicine services (March 16). Sudden and important changes (decrease and increase, respectively) can be seen, with a slight delay for consultations. Gray, total of services; blue, consultations; orange, physiotherapy. (B) Descriptive analysis of the observations performed through a polynomial function of the 3rd degree. (C) Evolution during the days of services (gray), consultations (blue), and physiotherapy (orange) in COVID-19 and telemedicine phases.
This study was conducted in a tertiary referral outpatient rehabilitation institute for spinal deformities, specializing in pediatric health conditions. The institute’s usual services include face-to-face consultations,8 physiotherapy (evaluation, teaching of exercises, cognitive-behavioral approaches, counseling),9 and psychological sessions; brace fitting is also provided in the orthotics facilities.10 Beginning with a few previous telephysiotherapy experiences, we developed and started brand new emergency protocols within a few days, with discussion and consensus among the institute’s most experienced physiotherapists and physicians. The protocols were discussed and agreed upon by all the other professionals in 2 meetings, which were repeated weekly during the study. Supervision was provided to all professionals. A few adaptations to the original protocol were performed in the first week.
The telemedicine service was offered to all patients between the ages of 3 and 18 years. For this analysis, we retrospectively included all services provided from January 7, 2018 to April 3, 2020. Telemedicine interventions (table 1 ) were delivered using free teleconference apps (Skype,a WhatsApp,b and Google Meetc software). We provided patients with written and video tutorials describing how to collect photographs and videos of clinical evaluations, imaging, or of exercises using home tools (ie, rulers, goniometers). These were received before the telemedicine sessions. All telemedicine sessions lasted as long as a usual face-to-face session. Clinical history, conclusions, and counseling were performed as usual. Teleconsultation innovations included measurements of the photographs and videos provided using the Surgimap software,d which were confirmed by the repetition of “live” measurements under direct medical guidance. Telephysiotherapy session innovations included the teaching of exercises using the parents’ hands under physiotherapist guidance along with the use of normal house furniture as treatment tools.
Table 1.
Differences between usual (consultations and physiotherapy) and telemedicine (teleconsultations and telephysiotherapy) interventions
| Phase of the Intervention | Usual |
Telemedicine |
||
|---|---|---|---|---|
| Consultation | Physiotherapy | Teleconsultation | Telephysiotherapy | |
| Preparation | General instructions as usual | |||
| — | — | Written/video tutorials sent to the patients | ||
| — | — | Patients’ collection of photos/videos of: | ||
| — | — | clinical evaluations or imaging | patients’ collection of exercises | |
| — | — | material sent to the secretariat in advance | ||
| — | — | trial of connection by secretariat | ||
| Setting | Office | Teleconference App | ||
| Intervention | Clinical history collection as usual | |||
| Measurements on the patient | Hands-on teaching of exercises | Measurements from videos/photos | Teaching exercises using the hands of parents under physiotherapist guidance | |
| Use of normal house furniture as treatment tools | Double check “live” with caregivers measuring patients | Use of normal house furniture as treatment tools | ||
| Conclusions as usual | ||||
| Counseling as usual | ||||
We considered 3 phases: (1) a control phase of 30 working days including the usual services before the spread of COVID-19 and the creation of “red zones” (January 7-February 23); (2) a COVID phase of 13 working days during which there was a surge of usual services before starting telemedicine (February 24-March 14); and (3) a telemed phase of 15 working days during which only telemedicine services were provided (starting March 16). During the control and COVID phases, the institute provided only usual consultations and physiotherapy, whereas only telemedicine services (telephysiotherapy and teleconsultations) were provided during the telemed phase. If a reliable medical decision was not possible during teleconsultations, physicians prescribed usual face-to-face interventions. Continuous quality improvement questionnaires were also evaluated.
Satisfaction with services provided was evaluated by the continuous quality improvement questionnaires, and all professionals were closely monitored throughout the period with supervision and email consultations. At the end of the study period, they were asked to provide their positive and negative comments on the experience.
The variation of the provided services in total and in the 2 groups (physiotherapy and consultations, with consultations divided into 3 subgroups [initial visits, follow-ups, and brace checks]) were compared during the 3 phases, as well as with the same periods in 2018 and 2019. We considered the explanatory categorical 3-level variables years and phases. We checked differences between and within the variables through a 2-way analysis of variance, a post hoc analysis with Scheffe correction for significant differences, and marginal means. We also performed a regression analysis within each phase to determine the influence of days on services provided. We used STATA 15e and Excel.a
Results
During the telemed phase, 12 physicians and 38 physiotherapists provided 1207 interventions (325 teleconsulations, 882 telephysiotherapy sessions) in 3 weeks (15 working days). We found a rapid decrease of outpatient services in the COVID phase (–39%) in both groups (–37% for physiotherapy sessions, –55% for consultations) in 2020, but not in 2018 and 2019. We also found differences among the other phases in 2020 (table 2 ). Compared with the great losses from the control phase to the COVID phase, physiotherapy recovered (from –37% to –21%; P<.05) during the telemed phase, but consultations did not. There were differences among subgroups for consultations: follow-up teleconsultations stabilized (from –55% to –60%), whereas first visits (from –34% to –89%) and brace checks (from –16% to –75%) decreased drastically (fig 1B). This regression describes well the day-by-day effects of COVID-19 and the use of telemedicine within the phases. All services and the physiotherapy subgroup decreased during the COVID phase (P<.01; R 2=0.85 and 0.62, respectively), and consultations increased during the telemed phase (P<.05; R 2=0.31) (fig 1C). During the telemed phase, 0.5% of patients were required by physicians, after the teleconsultation, to visit our institute for a usual face-to-face consultation.
Table 2.
Average variations (analysis of variance) in services provided in the study phases, including consultations and physiotherapy subgroup.
| Change Among Phases | Total Services |
Consultations |
Physiotherapy |
|||
|---|---|---|---|---|---|---|
| Variation | P Value | Variation | P Value | Variation | P Value | |
| Between control and COVID | –21.5% | <.01 | –12.8% | <.01 | –10.1% | <.01 |
| Between COVID and telemed | +4.2% | NS | –4.1% | NS | +8.3% | <.05 |
| Between control and telemed | –17.3% | <.01 | –16.9% | <.01 | –1.8% | NS |
| R2 | 0.46 | 0.35 | 0.38 | |||
NOTE. During the control and COVID phases, only usual consultations and physiotherapy were provided, whereas only teleconsultations and telephysiotherapy were provided during the telemed phase. See text for more details.
Abbreviation: NS, not significant.
Continuous quality improvement questionnaires (38% response rate) indicated a mean satisfaction of 2.8 out of 3. All physicians and therapists were very happy with their experiences, confirming that it was possible to work properly. Those who were less accustomed to technology declared surprise and great satisfaction with the services delivered.
Discussion
The sudden surge of COVID-19 in Italy created an ideal experimental setting for telemedicine. Our institute provided only face-to-face services until March 14. Beginning March 16, only telemedicine services were provided, with face-to-face consultations possible only if required by a physician after the teleconsultation. Consequently, the reduction in the number of services provided by the institute shows the difficulty of patients with usual outpatient services during the pandemic in Italy. Even before the total lockdown on March 11, there was a clear, progressive, and continuous reduction in services during the COVID phase. Conversely, when the institute moved completely to telemedicine, the recovery (even if not at the previous level) documents the value and feasibility of telemedicine for patients and professionals, particularly in emergency situations. Patients were satisfied according to the quality questionnaires, and all professionals were interviewed declaring their satisfaction. Physicians felt comfortable with the results of the teleconsultations, and required a face-to-face consultation for only 1 patient in every 200.
The COVID-19 pandemic started in China and currently has its epicenter in Europe and is spreading quickly. Italy was the first country heavily affected by COVID-19 after China, and the country’s public health system struggled to react.3 Outpatient services were shut down to shift the staff to COVID-19 services. A dramatic reduction of public services has also been documented in previous epidemic emergencies.9 Nevertheless, the COVID-19 pandemic is posing unique challenges to health systems worldwide. It is clear that there is a major need to guarantee a continuum of care to patients not affected by the virus, while protecting them from possible contact with it at the same time by avoiding travel and limiting access to health facilities.
Despite the unavoidable limits due to its observational nature and the use of a historical control, this study shows the possibility of completely transforming classic “hands-on” outpatient services to telemedicine during the COVID-19 emergency. In this way, we reduced the need for travels and access to health facilities for patients below 1% and eliminated the need of travel of these health professionals. This experience demonstrates a viable alternative for many outpatient services, avoiding closure and the subsequent effect not only on patients’ health, but also the economic effect on professionals and facilities.
Study limitations
The current study has limitations but also strengths. It has a high ecological validity in that we report a real-life, whole-institution experience with more than 1200 interventions. The unique situation during the COVID-19 pandemic allowed us to study emergency situations and the sudden and total change of all activities, offering insight on the feasibility and acceptability of telemedicine in these circumstances. There were risks of selection bias in this study. Patients feeling an urgent need for consultations or more severe cases could have accepted more easily to telemedicine. The digital divide (no available technology, internet connections, or digital knowledge) could also have precluded a specific population to access the services. Some patients cancelled the session because they did not feel comfortable in the preparation phase (see table 1). Moreover, patients accessing telemedicine could have been more inclined to technology or more worried for their clinical conditions, which could also have an effect on patients’ satisfaction. Future studies with a longer follow-up period will provide more complete data and will allow confirmation of the effectiveness of the services provided in telemedicine.
Conclusions
Telemedicine is feasible and allows health care providers to continue providing outpatient services with patient satisfaction. In the current pandemic, telemedicine can provide a viable alternative to closure for many outpatient services, while reducing to a minimum the need for travel and face-to-face contact.
Suppliers
-
a.
Microsoft Corp.
-
b.
WhatsApp; WhatsApp Inc.
-
c.
Google Meet; Google LLC.
-
d.
Surgimap; Nemaris, Inc.
-
e.
Stata 15; StataCorp LLC.
Acknowledgment
We thank our colleagues and patients at the Italian Scientific Spine Institute for their cooperation during this difficult time of emergency.
Footnotes
Disclosures: Stefano Negrini, Alberto Negrini, Alessandra Negrini, and Michele Romano hold stock in ISICO (Italian Scientific Spine Institute). The other authors have nothing to disclose.
References
- 1.Bedford J., Enria D., Giesecke J., et al. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020 Mar 13 doi: 10.1001/jama.2020.4031. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nacoti M., Ciocca A., Giupponi A., et al. At the epicenter of the COVID-19 pandemic and humanitarian crises in Italy: changing perspectives on preparation and mitigation. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0080 Available at: Accessed April 1, 2020.
- 6.Kerbl R., Sperl W., Strassburg H.M., Pettoello-Mantovani M., Ehrich J. Overview of habilitation and rehabilitation for children and adolescents in Europe. J Pediatr. 2016;172:233–235.e2. doi: 10.1016/j.jpeds.2015.12.078. [DOI] [PubMed] [Google Scholar]
- 7.Flodgren G., Rachas A., Farmer A.J., Inzitari M., Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015:CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotwicki T., Negrini S., Grivas T.B., et al. Methodology of evaluation of morphology of the spine and the trunk in idiopathic scoliosis and other spinal deformities - 6th SOSORT consensus paper. Scoliosis. 2009;4:26. doi: 10.1186/1748-7161-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romano M., Negrini A., Parzini S., et al. SEAS (Scientific Exercises Approach to Scoliosis): a modern and effective evidence based approach to physiotherapic specific scoliosis exercises. Scoliosis. 2015;10:3. doi: 10.1186/s13013-014-0027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Negrini S., Grivas T.B., Kotwicki T., Rigo M., Zaina F., international Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) Guidelines on "standards of management of idiopathic scoliosis with corrective braces in everyday clinics and in clinical research": SOSORT consensus 2008. Scoliosis. 2009;4:2. doi: 10.1186/1748-7161-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]