Abstract
Background
Leadership development programs (LDPs) are known to be educational and valuable, yet time consuming and costly for a healthcare organization and participants alike. This study is aimed to determine the impact that participation in a formal LDP has on hospital managers and leaders’ competencies, as well as to identify the positive organizational outcomes that can be achieved.
Materials and Methods
We conducted a literature review focusing on hospital managers and leaders who participated in formal LDPs. From there, we extracted data to determine the outcomes achieved by participating in LDPs.
Results
The search yielded 7420 articles, of which 23 articles were used for this literature review. Overall, there were a wide range of positive outcomes for participants of LDPs and some outcomes appeared more frequently than others. The beneficial outcome that appeared most frequently was that participants were able to gain knowledge of management and leadership roles and responsibilities which appeared 13 times. An increase in participant’s confidence and communication skills appeared 10 times, respectively. The ability to network with others within the organization and an increase in job positivity and satisfaction appeared 7 times each.
Discussion
LDPs provided an array of positive outcomes for hospital leaders who had participated. However, there was a lack of studies on the topic and more research is needed in order to have a better understanding of the correlation between LDPs and beneficial organizational outcomes.
Keywords: hospital manager, hospital leader, LDP, leadership development program, beneficial outcome, organizational outcomes
Introduction
Strong leadership is the foundation of successful healthcare organizations, and leaders are the driving force behind overcoming obstacles and achieving goals. One way to build more effective leaders is through leadership development programs (LDPs). LDPs are defined as educational interventions designed to address and improve the leadership capabilities of individuals.1 Leadership development is important for a healthcare organization as it promotes skills/competency development needed to effectively manage/lead the staff toward goal achievement. Early career leadership training has shown to be helpful in leadership competency enhancement and in building a foundation for those who choose to take on more advanced roles later in their career.2 New employees, particularly millennials, are looking for long-term career opportunities that place greater importance on leadership training than other benefits. A recent report on millennials at work found that they showed more interest in going to organizations that offer to develop their leadership skills.3 This report found that 52% of respondents said they would choose a job that would let them advance through the ranks quickly over one with a higher salary. Companies that provide leadership training programs give these and other individuals the opportunity to develop and improve on their leadership skills, which then gives them a better chance of getting promoted to a higher position over someone who has not developed those skills.
LDPs provide an important avenue through which both new and established leaders can receive education and training to meet their ongoing developmental needs.1 Organizations provide leadership development and training programs through various methods, such as classroom-based training, skills-based training, action learning, mentoring, coaching or online programs. When using LDPs, each organization utilizes their own method of teaching and therefore will differ from one another in how the program is taught. Approximately 50% of hospitals have a defined leadership development program, and of those programs, approximately 80% are developed in-house leadership development programs.4,5 There are many advantages to using a structured leadership program, especially if it is specific to an organization’s needs. A formal program that is developed in-house is more catered to a specific company’s strategic priorities, goals, and organizational culture. Participants can learn from situations and examples which are relevant to their company and engage in activities and projects that are related to the organization’s needs. Structured LDPs are a benefit to both the employee and the company, since the programs give participants the opportunity to improve on their leadership skills and gain valuable competencies. In turn, the company also benefits by educating and training more skilled and capable leaders to efficiently run their organization, which can also lead to better achievement of strategic initiatives including increased employee retention and satisfaction.
This study is an evidenced-based literature review on how individual competencies and organizational outcomes are influenced when hospital managers and leaders participate in a formal and structured leadership development program. A literature review format allowed for the exploration of a general question and related literature. In addition, this format provided flexibility and diversity for including literature depicting a wide range of different methodologies.6 This study seeks to determine if formal LDPs have an impact on hospital managers' competencies and if those programs have a positive influence on organizational outcomes.
Despite the potential benefits of LDPs, limited research currently exists on the impact of such programs. More specifically, little is known about the impact that LDPs have on both organizations and individuals and under which conditions the advantages of such programs can be maximized. The dearth of literature in this area provided much of the footer for this project. The data from this and other similar studies will help healthcare organizations to determine whether formal LDPs are beneficial for them, while identifying how specific LDPs affect organizational outcomes. It is not just potentially important to have healthcare managers participate in LDPs, but to also recognize why it is vital in improving healthcare overall. This understanding can only come from carrying out extensive studies on LDPs, which is something that is greatly lacking. If LDPs in fact yield positive outcomes, it will allow readers to determine how precisely healthcare managers are able to improve along with the organization. This literature review also explored the LDPs effects on healthcare manager’s competencies along with organizational outcomes.
The main goal of this review was to answer the following question: for hospital managers and leaders, how do formal and structured leadership development programs positively affect individual and organizational outcomes? The primary objective was to identify what type of benefits structured leadership development programs provide to individuals who undergo such programs, including the skills and competencies they may gain. The secondary objective was to understand how these programs benefit the organizations and add value to their overall success.
Materials and Methods
Though a literature review format was employed for this project, in lieu of a meta analysis or a scoping review, we have elected to utilize the PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) Checklist because it provides a thorough framework for conducting various types of literature reviews.7 The PRISMA-ScR is a checklist that contains 20 essential reporting items and 2 optional items and represents a widely recognized way of conducting a structured scoping review. It was created to help individuals develop a greater understanding of relevant terminology, core concepts, and key items to report, and to help ensure the consistency and scientific rigor of literature and other similar reviews.7
Before beginning this project, a protocol describing the research process was submitted to and approved by the Rutgers University-Rutgers Biomedical and Health Sciences-Newark Campus Institutional Review Board. Approval number for the IRB was Pro2019000518.
Research Question
The research question for this review was: “For hospital managers and leaders, how do formal and structured leadership development programs positively affect individual and organizational outcomes?”
Information Sources and Search Strategy
An initial hand search was done on the topic to determine if there was enough relevant information available online to carry out the research. Once the topic was determined, a PICO question was created with the main categories of search being the population, intervention, and outcomes. PICO (Population – Intervention – Comparison – Outcome) is a tool commonly used in medical and health research to help researchers formulate a researchable question using those terminologies.8 A search strategy combining the list of terminologies from these three categories was developed to retrieve articles of interest in the following databases: CINAHL, ERIC, Web of Science, OVID Medline, Academic Search Premier, Business Sources and Dissertations & Global Thesis. A sample search strategy from CINAHL database is provided (Appendix A). The search process for these databases was aided by the Rutgers University Librarian, who compiled the total results that were found and removed any duplicate articles before submitting the final list of articles for the reviewers to screen.
Searches were limited to English language studies and the time period between 2009 and 2019. Additionally, articles that were systematic or scoping reviews were excluded from this study.
Eligibility Criteria
Studies were included if they met the following conditions:
The searched publications were between January 2009 and December 2019.
Studies were published in English.
The study consisted of a structured and formal leadership development program with a minimum of three sessions of training.
The population undergoing the leadership training program consisted of hospital managers and leaders.
The result of the study consisted of at least one positive outcome.
Study Selection Process
The selection process began with three reviewers screening article titles and abstracts to check for relevancy to the topic. The remaining articles were screened for full text using the screening form (Appendix B) that was created for this literature review. Any articles that did not meet the three criteria for inclusion were excluded. The reasons for exclusion were recorded only at the full-text stage. Any disagreements between reviewers were resolved by consensus.
Data Extraction Process
A data extraction form was developed by the research team and included the following items:
article identifiers (author, title, date of publication)
selection criteria (population, study intervention, outcomes measures)
study identifiers (citation, country of origin)
study characteristics (aim, setting, inclusion and exclusion criteria)
participant characteristics (total participants, population description)
intervention (method used for LDP, duration and frequency of LDP)
outcome data (beneficial outcomes)
study conclusion
Collating, Summarizing, and Reporting the Results
A numerical summary of the beneficial outcomes of the included studies was performed. A table was created and was included as … to reflect the most common beneficial outcomes that were found overall in the combined number of studies. Additionally, the number of times an outcome was found in each of the studies was also documented on the table. Each outcome had to be present in a minimum of three studies in order to be listed on the table. A graph was created to display the results from the table.
Results
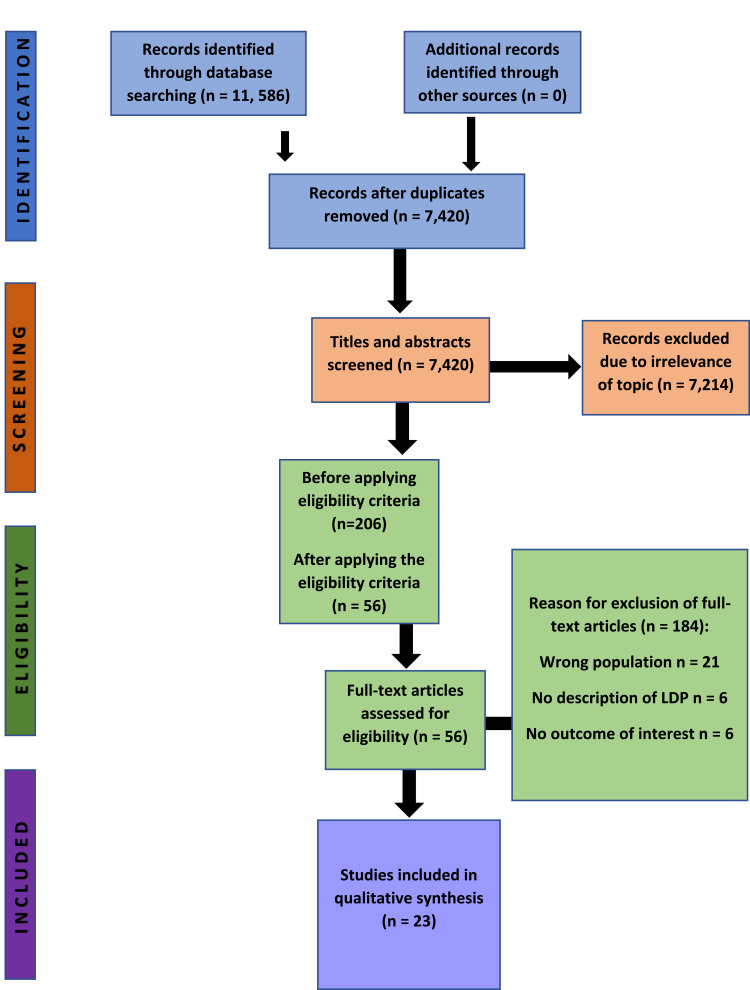
The initial database search yielded 7420 articles before title and abstract screening. Due to the nature of this topic, the majority of articles were not sufficiently relevant to our topic and were excluded, leaving 206 articles after this step in the screening process. An additional preliminary screening step left 56 which seemed to meet the eligibility criteria. Lastly, a comprehensive review of full-text articles left 23 articles that definitely met our inclusion criteria. A flow chart depicting the process of obtaining the 23 articles can be found in Figure 1. Table 1 was created using the data that was captured from those articles. Table 2 contains a summary of the chief characteristics of all articles included in this review. As such, it confirms that the selection criteria were met for the 23 articles included and describes such features as the types of research and our evaluation of the potential bias based on the Cochran tool.
Figure 1.
Flowchart of studies in the literature review and reasons for exclusion.
Table 1.
Beneficial Outcomes
| Beneficial Outcomes | Number of Studies in Which the Outcome Appears |
|---|---|
| Gained Knowledge of Management & Leadership Roles/Responsibilities | 13 |
| Increased Confidence | 10 |
| Improved Communication Skills | 10 |
| Gained Networking Opportunities | 7 |
| Increased Job Satisfaction/Positivity | 7 |
| Improved Career Planning Skills/Succession Planning | 6 |
| Increased Self-Awareness | 6 |
| Improved Teamwork Skills | 6 |
| Improved Problem Solving Skills | 6 |
| Gained Ability to Empower/Encourage Others | 6 |
| Increased Sense of Collective Vision Among Team | 5 |
| Gained Knowledge of Health Care Systems and Processes | 5 |
| Positive Impact on Organization (Patient Satisfaction, Outcomes, etc.) | 5 |
| Increased Motivation | 4 |
| Gained Ability to Become a Mentor/Role Model | 4 |
| Gained Knowledge on Financing/Budget Skills | 3 |
| Improved Networking Skills | 2 |
| Increased Leadership Presence | 1 |
| Increased Approachability | 1 |
| Increased Understanding of Diversity at the Workplace | 1 |
Table 2.
Summary Table
| Title | Author(s) | Citation | Selection Criteria 1: Was the Population Hospital Managers and Leaders? | Selection Criteria 2: Was the Intervention a Leadership Development Program? | Selection Criteria 3: Was There a Positive Influence from the Intervention? | Research or Study Design | Likelihood of Bias Using Cochrane Tool* | Use of Kirkpatrick Method** |
|---|---|---|---|---|---|---|---|---|
| 21 Developing capable quality improvement leaders | Geraldine M Kaminski, Maria T Britto, Pamela J Schoettker, Stacey L Farber, Stephen Muething, Uma R Kotagal | Kaminski, G. M., Britto, M. T., Schoettker, P. J., Farber, S. L., Muething, S., & Kotagal, U. R. (2012). Developing capable quality improvement leaders. BMJ Qual Saf, 21(11), 903–911. doi:10.1136/bmjqs-2012-000890 | Yes | Yes | Yes | Outcome Evaluation Study | Low Risk of Bias | Yes |
| 18 Impact of leadership development on emotional health in healthcare managers | How Lee, Janice Sharlow, Juditha. Spiers, Aslam Bhatti, Paula Germann, Ozden Yurtseven, Greta G. Cummings. | Lee, H., Spiers, J. A., Yurtseven, O., Cummings, G. G., Sharlow, J., Bhatti, A., & Germann, P. (2010). Impact of leadership development on emotional health in healthcare managers. J Nurs Manag, 18(8), 1027–1039. doi:10.1111/j.1365–2834.2010.01178.x | Yes | Yes | Yes | Mixed Method Study | Unclear- Did not mention if the managers were chosen at random or specifically chosen. | No |
| 19 Using the 7 Habits programme to develop effective leadership | David Leeson, Mark Miller | Leeson, D., & Millar, M. (2013). Using the 7 Habits programme to develop effective leadership. Nurs Manag (Harrow), 20(6), 31–37. doi:10.7748/nm2013.10.20.6.31.e1123 | Yes | Yes | Yes | Outcome Evaluation Study | Unclear- Does not mention a lot of details about population selection. | No |
| 22 Equipping clinical leaders for system and service improvements in quality and safety: an Australian experience | Sandra G. Leggat, Anne Smyth, Cathy Balding, Iain McAlpine | Leggat, S. G., Smyth, A., Balding, C., & McAlpine, I. (2016). Equipping clinical leaders for system and service improvements in quality and safety: an Australian experience. Aust N Z J Public Health, 40(2), 138–143. doi:10.1111/1753-6405.12462 | Yes | Yes | Yes | Longitudinal pre-post-intervention mixed methods study | Unclear- Did not mention if the managers were chosen at random or specifically chosen. | No |
| 23 A randomised study of leadership interventions for healthcare managers | Caroline Lornudd, David Bergman, Christer Sandahl and Ulrica von Thiele Schwarz | Lornudd, C., Bergman, D., Sandahl, C., & von Thiele Schwarz, U. (2016). A randomised study of leadership interventions for healthcare managers. Leadersh Health Serv (Bradf Engl), 29(4), 358–376. doi:10.1108/LHS-06-2015-0017 | Yes | Yes | Yes | Randomized Controlled Trial | Low Risk of Bias | No |
| 24 Evaluation of a clinical leadership programme for nurse leaders | Jacqueline S. Martin, Rebecca Spirig, Brendan Mccormack, Donna Fitzsimons | Martin, J. S., McCormack, B., Fitzsimons, D., & Spirig, R. (2012). Evaluation of a clinical leadership programme for nurse leaders. J Nurs Manag, 20(1), 72–80. doi:10.1111/j.1365–2834.2011.01271.x | Yes | Yes | Yes | Evaluation Design Study: Outcome Design | Low Risk of Bias | No |
| 9 Training evaluation: a case study of training Iranian health managers | Maye Omar, Nancy Gerein, Ehsanullah Tarin, Christopher Butcher, Stephen Pearson, and Gholamreza Heidari | Omar, M., Gerein, N., Tarin, E., Butcher, C., Pearson, S., & Heidari, G. (2009). Training evaluation: a case study of training Iranian health managers. Human Resources for Health, 7, 1–14. doi:10.1186/1478-4491-7-20 | Yes | Yes | Yes | Evaluation Design Study: Outcome Design | High Risk of Bias- Only 66% had turned in the questionnaire. | Yes |
| 10 A two-pronged quality improvement training program for leaders and frontline staff. | Kimberly J Rask, Richard S Gitomer, Nathan O Spell, Steven D Culler, Sarah C Blake, Susan S Kohler, Jonathan N Hawley, William A Bornstein | Rask, K. J., Gitomer, R. S., Spell Iii, N. O., Culler, S. D., Blake, S. C., Kohler, S. S.,. Bornstein, W. A. (2011). A two-pronged quality improvement training program for leaders and frontline staff. Joint Commission Journal on Quality & Patient Safety, 37(4), 147–153. | Yes | Yes | Yes | Evaluation Design Study: Outcome Design | Unclear | No |
| 16 A Case for Change: Assessment of an Evidenced-Based Leadership Development Program | Alexander, Bryan K. | Alexander, B. K. (2013). A Case for Change: Assessment of an Evidenced-Based Leadership Development Program. (3,570,370 D.M.), University of Phoenix, Ann Arbor. Retrieved from https://search.proquest.com/docview/1,399,157,970?accountid=13,626 https://rutgers.primo.exlibrisgroup.com/discovery/openurl?institution=01RUT_INST&vid=01RUT_INST:01RUT&genre=dissertations+%26+theses&atitle=&author=Alexander%2 |
Yes | Yes | Yes | Outcome Evaluation Study | Low Risk of Bias | No |
| 8 Characteristics of a Health System-Sponsored Leadership Development Program As They Relate To The Career Advancement of Physician Leaders. | Arsenault, Rebecca L. | Arsenault, R. L. (2017). Characteristics of a health system-sponsored leadership development program as they relate to the career advancement of physician leaders. (10,255,751 D.H.A.), Capella University, Ann Arbor. Retrieved from https://search.proquest.com/docview/1,873,501,837?accountid=13,626 https://rutgers.primo.exlibrisgroup.com/discovery/openurl?institution=01RUT_INST&vid=01RUT_INST:01RUT&genre=dissertations+%26+theses&atitle=&author=Arsenault%2C+Rebecca+L.&volume=&issue=&spage=&date=2017&rft.btitle=&rft.jtitle=&issn=&isbn=9,781,369,549,515&sid=ProQuest+Dissertations+%26+Theses+Global_ |
Yes | Yes | Yes | Qualitative Phenomenological Study | Low Risk of Bias | No |
| 25 Leadership, Inside and Out: The Tideswell-AGS-ADGAP Emerging Leaders in Aging Program. 67: 437–442. | Chang, A., Lundebjerg, N. E., Abrams, J., Barnes, D. E., Fain, M. J, Hal, W. J., Johnson, T. M., 2nd, Michael Harper, G., Williams, B., Ritchie, C. S. | Chang, A., Lundebjerg, N. E., Abrams, J., Barnes, D. E., Fain, M. J., Hall, W. J., Ritchie, C. S. (2019). Leadership, Inside and Out: The Tideswell-AGS-ADGAP Emerging Leaders in Aging Program. J Am Geriatr Soc, 67(3), 437–442. doi:10.1111/jgs.15702 | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | Yes |
| 11 A Physician LDP at an Academic Medical Center | Gagliano, N.J, Ferris, T., Colton, D., Dubitzky, A., Hefferman, J., Torchiana, D. | Gagliano, N. J., Ferris, T., Colton, D., Dubitzky, A., Hefferman, J., & Torchiana, D. (2010). A physician leadership development program at an academic medical center. Qual Manag Health Care, 19(3), 231–238. doi:10.1097/QMH.0b013e3181eb13ab | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | No |
| 26 Management and leadership development in healthcare and the challenges facing physician managers in clinical practice | Busari, Jamiu O. | Busari, J. O. (2012). Management and leadership development in healthcare and the challenges facing physician managers in clinical practice. International Journal of Clinical Leadership, 17(4), 211–216. | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | No |
| 15 Multi-professional Clinical Leadership Training in Healthcare: A Peer-led Evaluation of the experience and benefits of the “Darzi Fellowship” | Conn, R., Bali, A., Akers, E. | Conn, R., Bali, A., & Akers, E. (2016). Multi-professional clinical leadership training in healthcare A peer-led evaluation of the experience and benefits of the “Darzi Fellowship”. International Journal of Public Leadership, 12(4), 317–335. doi:10.1108/Ijpl-03-2016-0005 | Yes | Yes | Yes | Mixed Method Study | Possible Risk of Bias- Survey was undertaken with 8 weeks of the program left.? | No |
| 12 Strengthening the capacity of nursing leaders through multifaceted professional development initiatives: A mixed method evaluation of the ‘Take the lead’ program’ | Debono, D., Travaglia, J.F., Dunn, A.G., Thorns, D., Hinchcliff, R., Plumb, J., Milne, J., Erez-Rein, N., Wiley, J., Braithwaite, J. | Debono, D., Travaglia, J. F., Dunn, A. G., Thorns, D., Hinchcliff, R., Plumb, J.,Braithwaite, J. (2016). Strengthening the capacity of nursing leaders through multifaceted professional development initiatives: A mixed method evaluation of the ‘Take The Lead’ program. Collegian, 23(1), 19–28. doi:10.1016/j.colegn.2014.09.005 | Yes | Yes | Yes | Mixed Method Study | Unclear | No |
| 14 Reframing Leadership Development in Healthcare | Cocowitch, V., Orton, S., Daniels, J., & Kiser, D. | Reframing Leadership Development in Healthcare An OD Approach, 45, buh 10–18, OD Practitioner (2013). | Yes | Yes | Yes | Case Study | Low Risk of Bias | No |
| 27 Service impact of a national clinical leadership development programme: findings from a qualitative study | Fealy, G. M., McNamara, M. S., Casey, M., O’Connor, T., Patton, D., Doyle, L., & Quinlan, C. | Fealy, G. M., McNamara, M. S., Casey, M., O’Connor, T., Patton, D., Doyle, L., & Quinlan, C. (2015). Service impact of a national clinical leadership development programme: findings from a qualitative study. J Nurs Manag, 23(3), 324–332. doi:10.1111/jonm.12133 | Yes | Yes | Yes | Outcome Evaluation Study | High Risk of Bias- Participants were selected through purposive sampling. | No |
| 28 Physician-leader on-boarding: the Cleveland Clinic experience | K. Stoller, J., Barker, C., & FitzSimons, K. | K. Stoller, J., Barker, C., & FitzSimons, K. (2013). Physician-leader on-boarding: the Cleveland Clinic experience. Journal of Management Development, 32(9), 960–970. doi:10.1108/jmd-06-2011-0072 | Yes | Yes | Yes | Outcome Evaluation Study | High Risk of Bias- Possibility of Sampling Bias | No |
| 29 Growing Leaders in a Professional Membership Organization | Shekleton, M.E.; Preston, J.C.; Good, L.E. | Shekleton, M. E., Preston, J. C., & Good, L. E. (2010). Growing leaders in a professional membership organization. J Nurs Manag, 18(6), 662–668. doi:10.1111/j.1365–2834.2010.01152.x | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | No |
| 20 Development down under | Silverston, H. | Silverston, H. (2013). Development down under. Nurs Stand, 27(51), 24–25. doi:10.7748/ns2013.08.27.51.24.s28 | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | No |
| 13 The Leadership Practice Circle Program: An Evidence-Based Approach to Leadership Development in Healthcare | Taylor-Ford, R. L., Abell, D. | Taylor-Ford, R. L., & Abell, D. (2015). The Leadership Practice Circle Program: An Evidence-Based Approach to Leadership Development in Healthcare. Nurse Leader, 13(2), 63–68. doi:10.1016/j.mnl.2014.07.014 | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | No |
| 30 Influence of a Hospital-Based, Internal Leadership Development Program on Leadership Effectiveness | Welch-Carre, Elizabeth | Welch-Carre, E. (2017). Influence of a Hospital-Based, Internal Leadership Development Program on Leadership Effectiveness. ProQuest LLC. Retrieved from https://login.proxy.libraries.rutgers.edu/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=eric&AN=ED579917&site=ehost-livehttp://gateway.proquest.com/openurl?url_ver=Z39.88–2004&rft_val_fmt=info:ofi/fmt:kev:mtx:dissertation&res_dat=xri:pqm&rft_dat=xri:pqdiss:10,624,646 Available from EBSCOhost eric database. | Yes | Yes | Yes | Outcome Evaluation Study | Low Risk of Bias | Yes |
| 17 Evaluation of a nurse leadership development programme | West, M., Smithgall, L., Rosler, G., Winn, E. | West, M., Smithgall, L., Rosler, G., & Winn, E. (2016). Evaluation of a nurse leadership development programme. Nurs Manag (Harrow), 22(10), 26–31. doi:10.7748/nm.22.10.26.s29 | Yes | Yes | Yes | Outcome Evaluation Study | Unclear | No |
Notes: *Standardized technique for assessing the risk of bias. **The Kirkpatrick method is a standard and validated method for assessing training and education programs.
The aim of this study was to understand how individual competencies and organizational outcomes are influenced when hospital managers and leaders participate in a formal and structured leadership development program. From this frequency data, we discerned there is a wide range of individual benefits gained by hospital leaders who participated in a formal LDP, along with a few organizational outcomes that were found to a lesser extent. The individual beneficial outcome that appeared most frequently was that participants were able to gain knowledge of management and leadership roles and responsibilities which appeared 13 times. An increase in participant’s confidence and communication skills appeared 10 times, respectively. The ability to network with others within the organization and increase in job positivity and satisfaction appeared 7 times each. Participants were able to obtain an increase in improved career planning skills, succession planning, improved self-awareness, improved teamwork and problem-solving skills, and gained the ability to empower others, all of which appeared 6 times each. Additionally, 5 studies revealed that participants also showed an increased vision among their team, gained knowledge of healthcare systems and processes and increased patient satisfaction and outcomes. There was increased motivation within the participants along with a gained ability to be a mentor and role model, which appeared in 4 studies. A few studies also yielded in participants having gained knowledge on financing and budgeting skills.
A table was created that shows the percentage of times that the benefit appeared (Table 3).
Table 3.
Table of Beneficial Outcomes
| Beneficial Outcomes | Percentage of Studies Included in Which the Outcome Appears |
|---|---|
| Gained Knowledge of Management & Leadership Roles/Responsibilities | 57% |
| Increased Confidence | 43% |
| Improved Communication Skills | 43% |
| Gained Networking Opportunities | 30% |
| Increased Job Satisfaction/Positivity | 30% |
| Improved Career Planning Skills/Succession Planning | 26% |
| Increased Self-Awareness | 26% |
| Improved Teamwork Skills | 26% |
| Improved Problem Solving Skills | 26% |
| Gained Ability to Empower/Encourage Others | 26% |
| Increased Sense of Collective Vision Among Team | 22% |
| Gained Knowledge of Health Care Systems and Processes | 22% |
| Positive Impact on Organization (Patient Satisfaction, Outcomes, etc.) | 22% |
| Increased Motivation | 17% |
| Gained Ability to Become a Mentor/Role Model | 17% |
| Gained Knowledge on Financing/Budget Skills | 13% |
| Improved Networking Skills | 9% |
| Increased Leadership Presence | 4% |
| Increased Approachability | 4% |
| Increased Understanding of Diversity at the Workplace | 4% |
From this graph, it is evident that the majority of outcomes were found in less than 50% of the studies. Gaining knowledge of management and leadership roles and responsibilities was the most frequent beneficial outcome, and that appeared in 57% of the articles. Improved confidence and communication skills were next appearing in 43% of the articles. Gaining networking opportunities and increased job satisfaction was next just appearing in 30% of the articles.
Discussion
The purpose of our evidenced-based literature review was to understand how individual competencies and organizational outcomes are influenced when hospital managers and leaders participate in a formal and structured leadership development program. The data collected demonstrate the variety of beneficial outcomes for hospital managers and leaders who attended a formal LDP. The most common individual beneficial outcomes that appeared in the 23 articles were under the following categories: gaining knowledge of leadership roles/responsibilities, gaining confidence, and gaining communication skills. Gaining knowledge of leadership roles/responsibilities, which included skills on strategic planning, change management, and thinking strategically and critically had appeared in 13 out of the 23 articles. Arsenault (2017) stated that participants were able to expand their knowledge on being new leaders while developing skills on strategic planning and management.9 Omar et al (2009) stated that respondents claimed they could perform their jobs better because of new skills learned from the LDP along with attaining more in-depth understanding of health systems.10 Rask et al (2011) stated that pre- and post-test results showed a 30–40% improvement in the following categories: systems thinking, roles of leadership, management implications of process improvement, health outcome results from processes and tools for process management.11
From the literature review, we were able to find that the knowledge of management, leadership roles and responsibilities gained by formal LDPs helped in aiding participants in their roles in the organization by giving them knowledge and skills to lead their staff. For example, Gagliano et al (2010) stated that the pace and length of their LDP allowed participants to gradually incorporate their new skills learned within their own practices.12 Debono et al (2016) detailed that nursing and unit manager’s participation in the Take the Lead (TTL) LDP produced improvements in job performance and leadership skills.13 Taylor-Ford and Abell (2015) mentioned that the Leadership Practice Circle Program (LPCP) was effective in improving various aspects of leadership competency by building a sense of team and collective vision.14
The second most prominent beneficial outcome, appearing in 10 of the 23 articles, were that participants were able to gain a greater sense of confidence. In some instances, Arsenault (2017) identified that a significant experience reported by study participants was that they were able to develop improved confidence when functioning with key individuals at their organization after the LDP.9 Gagliano et al (2010) noted that participants were able to gain confidence in their skills throughout the 2 years, and by the end of the LDP participants were able to take on greater institution-wide challenges.12 In the article “Reframing Leadership Development in Healthcare”, it was stated that an impact of the Leadership Novant was participants felt more empowered to speak up and “push back”, as their CEO often implored them to do.15 Conn et al (2016) stated that through the experiential processes within the fellowship, fellows describe increasing confidence, a new way of thinking, and increased adaptability.16
Improvement of communication skills was the third most frequently mentioned beneficial outcome throughout the articles. Communication skills include receiving, understanding, and expressing information, feelings, and ideas. Alexander (2013) mentioned that participants were better informed and gained knowledge that helped them to communicate more effectively with employees thus helping them to foster a culture of excellence.17 Arsenault (2017) stated that physician leaders who participated in the health system-sponsored leadership development program were able to refine communication styles by creating meaningful presentations and becoming a better listener as both a physician and leader.9
There were several other beneficial outcomes that were not as frequent yet appeared throughout the literature. For example, one article stated that “diversity as a vehicle to wholeness” was one improvement that was recognized from those who had participated in the LDP.18 Using LDPs to teach the importance of diversity may not necessarily be common; however, the study showed that LDPs can possibly be used for that purpose. While this did not appear enough to be captured in the table, it should be noted as a beneficial outcome. Other beneficial outcomes that appeared less frequently were an increased leadership presence, approachability as a leader, and increased understanding of diversity at the workplace.
The variety of beneficial outcomes were to be expected, but what was surprising was the lack of consistency on them within the literature. Prior to this literature review, we had hypothesized that certain beneficial outcomes, such as gaining leadership skills or improving confidence, would have appeared in most of the studies. However, our data revealed that these benefits were only mentioned in about half of the studies or less. Only 13 out of the 23 (57%) of the literature stated that the leadership development program had helped the participants gain knowledge of management/leadership roles/responsibilities. Only 10 out of 23 (43%) of the literature said that the participants gained an increase in communication skills. This lack of consistency could have been due to the lessons themselves and what the goal for the course was with that particular LDP. It is hard to claim this as a fact however with the inconsistency and lack of data in the literature.
The most significant lesson learned from this evidence-based literature review was that formal LDPs have the potential to provide a variety of beneficial outcomes for hospital managers and leaders who participate. The likelihood of the leader gaining the beneficial outcome depends on several variables such as levels of engagement, attendance, and the efficiency of the lessons themselves. Leaders can ensure that they benefit by attending the LDPs with a high level of engagement and attention. The more active an individual is in the process of learning, the more likely he/she is of retaining the information and utilizing it in their job roles. Organizations can ensure that their leaders are gaining the desired beneficial outcomes by verifying that the LDPs cater to their specific needs, are applicable to their job roles, and that the leaders have the necessary time needed to fully engage in the LDP.
From the 23 articles reviewed, we found 16 different beneficial outcomes that appeared in at least three different articles. Organizations can organize and use an LDP to focus on any of the beneficial outcomes. The next lesson learned was that there is a gap in research to drive, support or anchor leadership practices in healthcare. As previously stated, we only had 23 studies that met our inclusion criteria. Each study was unique to a particular organization and some did not give any information regarding the method of the LDP itself. This gap of information makes it difficult to really correlate that participating in a LDP will lead to beneficial outcomes listed in the table.
For organizational outcomes, there were only two studies that mentioned that LDPs had a positive impact on the overall organization in terms of patient satisfaction and patient outcomes. Alexander (2013) stated that there was a positive correlation between the LDP and patient satisfaction and patient outcomes.17 Debono et al (2016) stated that participants of Take the Lead program (TTL) helped to improve patient experience while patient satisfaction was reported by the nursing unit to have increased by 40% subsequently after participating in the program.13 Another positive outcome of these LDPs was increased job satisfaction and positivity after participating in their respective LDP. Employee satisfaction is key for successful organizations while helping to promote the organization. Participants were able to increase job satisfaction which led them to perform better for the organization. Lee et al (2010) state that the participants of the program were able to better manage burnout while significantly improving their emotional health. This led to increased job satisfaction to continue their roles within their organization.19 Leeson et al (2013) mentioned that those who participated in the LDP were able to increase proactivity and positivity while decreasing stress.20 Due to this fact, the organization committed additional resources to continue the program.
Improved career planning and succession planning was also mentioned as a beneficial outcome by participating in LDPs. In the article “Reframing Leadership Development in Healthcare an OD Approach,” an organizational outcome mentioned was succession planning.15 Over half of the fellows in the first three cohorts of the LDP, Leadership Novant, had been promoted by 2011, including a full 70% of the initial class. All current senior leaders in the twelve hospital facilities participated in the LDP. Silverston (2013) states that those participants of the RCN Clinical Leadership Program were able to benefit from workshops that develop career planning skills for the present and future.21 West et al (2016) state that those who participated in the NEL program improved succession planning by developing leaders from within the Geisinger’s nursing teams, who are then well prepared for promotion when leadership positions become available.18 Emerging leaders will eventually replace them and continue the vital work being done to improve nursing environments and, most importantly patient outcomes. Arsenault (2017) mentioned that the majority of participants who completed the LDP believe that participating allowed them to develop a valuable network of other physician colleagues within the medical and health care field, which further supported their career advancement and success.9 Improvement in career planning and succession planning appeared in six occasions out of the 22 articles. This was not sufficient data to support the beneficial outcomes for organizations and will need further study to determine if there is a positive correlation between LDPs and organizational outcomes.
This evidence-based literature review has shown the different benefits that LDPs can offer hospital managers and leaders, however, we recognize that there were also negative outcomes, such as the high cost of implementation or the inconsistencies with improvement in certain areas such as obtaining leadership skills. Further exploration of these negative outcomes should be considered as a focus for future studies. Furthermore, literature relating to very specific leadership styles or limited to one discipline were excluded. For example, a study done by Senegal (2010) which focused only on Transformational Leadership competencies only in the clinical discipline of nursing was excluded. However, future studies could allow for the inclusion of projects which are aimed at one specific leadership style or clinical discipline to broaden the scope of the review.
In addition, future studies in this area could also focus on the average cost of creating and implementing the leadership development programs. Once a cost has been identified, it can help to determine if organizations will gain a return of investment. Additionally, due to the lack of studies on this topic, future literature reviews on this topic should also increase the population so that more studies meet the inclusion criteria.
With all of this said, perhaps the biggest class of limitations we faced stemmed from the inconsistencies and lack of data on the effects of formal leadership development programs. Our focus was on hospital managers and leaders who had participated in leadership programs, which ultimately left us with only 23 articles after screening. This may well not be enough evidence to conclude with certainty, that participating in the LDP will provide the participant with the beneficial outcomes listed in the table. Several of the studies did not detail the features of the LDP. Thus, we excluded certain studies and were unable to fully explore the characteristics of LDPs which may be more or less beneficial. Lastly, only four of the studies we included described used the Kirkpatrick method for evaluating their training program. As a benchmark standard for evaluating training programs, the fact that the Kirkpatrick method was not described in most of the articles included in this study left the research team concerned about the lack of consistency and relevance of program evaluation in the literature. Hence, we would also recommend future studies evaluating LDPs use the Kirkpatrick model to measure their data. This helps ensure a more rigorous and consistent evaluation of such programs that is currently lacking.
It should also be noted that given the limited amount of research in this area and the relatively few articles which met the inclusion criteria, a literature review format was selected over other review formats such as a meta-analysis and a scoping review. As a result, most but not all of the PRISMA guidelines were used to structure this project. In the future as the body of research in this area expands and matures, we would recommend that one or more formal meta-analysis be undertaken in this area to strictly adhere to the PRISMA criteria. This could include the use of highly rigorous statistical methods, perhaps including the kappa coefficient to demonstrate the degree to which there is an agreement between the two individuals assessing qualitative studies.
Conclusion
There are many advantages to using a structured leadership program, especially if it is specific to an organization’s needs. This study suggests that formal LDPs can provide a variety of beneficial outcomes for hospital managers and leaders who participate in them. However, these beneficial outcomes are dependent on the participant’s attendance and their level of engagement in the LDP. Executives should work to oversee the LDP material to verify that they are obtaining the desired beneficial outcome for their organization.
Most importantly, we cannot ignore the lack of studies on this topic. More studies will need to occur before strong inferences and conclusions can be made regarding the relationship between LDPs and beneficial outcomes. Additionally, organizations should also formally assess the impact that a LDP has on the organization and report on it so that wide spread data can be gathered and used for further studies. With this understanding, we may determine if the LDPs will successfully provide a return of investment for a healthcare organization.
Acknowledgment
We would like to thank Margaret Dreker for helping us develop the search strategy.
Funding Statement
No funding was received for this study.
Ethics Approval
Before beginning this project, a protocol describing the research process was submitted to and approved by the Rutgers University-Rutgers Biomedical and Health Sciences-Newark Campus Institutional Review Board. Approval number for the IRB was Pro2019000518.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work. All members of the research team contributed equally to this study.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.McAlearney SA. Using leadership development programs to improve quality and efficiency in healthcare. J Healthcare Manage. 2008;53(5, September/October):319–331. doi: 10.1097/00115514-200809000-00008 [DOI] [PubMed] [Google Scholar]
- 2.Sonnino ER. Healthcare leadership development and training: progress and pitfalls. J Healthcare Leadership. 2016;8:19–29. doi: 10.2147/JHL.S68068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.PWC PricewaterhouseCoopers. Millennials at work. Reshaping the workplace. 2011. Available from: http://www. pwc. ru/en_RU/ru/hr-consulting/publications/assets/millenials-survey. pdf (дата обращения. Accessed July27, 2020.
- 4.Thompson JM, Kim TH. A profile of hospitals with leadership development programs. Health Care Manag (Frederick). 2013;32:179–188. doi: 10.1097/HCM.0b013e31828ef677 [DOI] [PubMed] [Google Scholar]
- 5.Health Research & Educational Team. Building a leadership team for the health care organization of the future. 2014. Available from: http://www.hpoe.org/Reports-HPOE/leadership-team-future-2014.pdf. Accessed June10, 2015.
- 6.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for Scoping Reviews (PRISMA-ScR): checklist and explanation the PRISMA-ScR statement. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/m18-0850 [DOI] [PubMed] [Google Scholar]
- 7.Research guides: systematic reviews in the health sciences: strategy development. n.d.. Available from: https://libguides.rutgers.edu/c.php?g=337288&p=2269572.
- 8.Arsenault RL. Characteristics of a Health System-Sponsored Leadership Development Program as They Relate to the Career Advancement of Physician Leaders. (10255751 D.H.A.). Ann Arbor: Capella University; 2017. Available from: https://search.proquest.com/docview/1873501837?accountid=13626. Accessed July27, 2020. [Google Scholar]
- 9.Omar M, Gerein N, Tarin E, Butcher C, Pearson S, Heidari G. Training evaluation: a case study of training Iranian health managers. Hum Resour Health. 2009;7:1–14. doi: 10.1186/1478-4491-7-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rask KJ, Gitomer RS, Spell Iii NO, et al. A two-pronged quality improvement training program for leaders and frontline staff. Joint Commission J Qual Patient Saf. 2011;37(4):147–153. doi: 10.1016/S1553-7250(11)37018-3 [DOI] [PubMed] [Google Scholar]
- 11.Gagliano NJ, Ferris T, Colton D, Dubitzky A, Hefferman J, Torchiana D. A physician leadership development program at an academic medical center. Qual Manag Health Care. 2010;19(3):231–238. doi: 10.1097/QMH.0b013e3181eb13ab [DOI] [PubMed] [Google Scholar]
- 12.Debono D, Travaglia JF, Dunn AG, et al. Strengthening the capacity of nursing leaders through multifaceted professional development initiatives: a mixed method evaluation of the ‘Take The Lead’ program. Collegian. 2016;23(1):19–28. doi: 10.1016/j.colegn.2014.09.005 [DOI] [PubMed] [Google Scholar]
- 13.Taylor-Ford RL, Abell D. The leadership practice circle program: an evidence-based approach to leadership development in healthcare. Nurse Leader. 2015;13(2):63–68. doi: 10.1016/j.mnl.2014.07.014 [DOI] [Google Scholar]
- 14.Reframing Leadership Development in Healthcare An OD Approach, 45, buh 10-18, OD Practitioner (2013).
- 15.Conn R, Bali A, Akers E. Multi-professional clinical leadership training in healthcare a peer-led evaluation of the experience and benefits of the “Darzi Fellowship”. Int J Public Leadership. 2016;12(4):317–335. doi: 10.1108/Ijpl-03-2016-0005 [DOI] [Google Scholar]
- 16.Alexander BK (2013). A Case for Change: Assessment of an Evidenced-Based Leadership Development Program. (3570370 D.M.), University of Phoenix, Ann Arbor: Available from https://search.proquest.com/docview/1399157970?accountid=13626. Accessed July27, 2020. [Google Scholar]
- 17.West M, Smithgall L, Rosler G, Winn E. Evaluation of a nurse leadership development programme. Nurs Manag (Harrow). 2016;22(10):26–31. doi: 10.7748/nm.22.10.26.s29 [DOI] [PubMed] [Google Scholar]
- 18.Lee H, Spiers JA, Yurtseven O, et al. Impact of leadership development on emotional health in healthcare managers. J Nurs Manag. 2010;18(8):1027–1039. doi: 10.1111/j.1365-2834.2010.01178.x [DOI] [PubMed] [Google Scholar]
- 19.Leeson D, Millar M. Using the 7 Habits programme to develop effective leadership. Nurs Manag (Harrow). 2013;20(6):31–37. doi: 10.7748/nm2013.10.20.6.31.e1123 [DOI] [PubMed] [Google Scholar]
- 20.Silverston H. Development down under. Nurs Stand. 2013;27(51):24–25. doi: 10.7748/ns2013.08.27.51.24.s28 [DOI] [PubMed] [Google Scholar]
- 21.Kaminski GM, Britto MT, Schoettker PJ, Farber SL, Muething S, Kotagal UR. Developing capable quality improvement leaders. BMJ Qual Saf. 2012;21(11):903–911. doi: 10.1136/bmjqs-2012-000890 [DOI] [PubMed] [Google Scholar]
- 22.Leggat SG, Smyth A, Balding C, McAlpine I. Equipping clinical leaders for system and service improvements in quality and safety: an Australian experience. Aust N Z J Public Health. 2016;40(2):138–143. doi: 10.1111/1753-6405.12462 [DOI] [PubMed] [Google Scholar]
- 23.Lornudd C, Bergman D, Sandahl C, von Thiele Schwarz U. A randomised study of leadership interventions for healthcare managers. Leadersh Health Serv (Bradf Engl). 2016;29(4):358–376. doi: 10.1108/LHS-06-2015-0017 [DOI] [PubMed] [Google Scholar]
- 24.Martin JS, McCormack B, Fitzsimons D, Spirig R. Evaluation of a clinical leadership programme for nurse leaders. J Nurs Manag. 2012;20(1):72–80. doi: 10.1111/j.1365-2834.2011.01271.x [DOI] [PubMed] [Google Scholar]
- 25.Chang A, Lundebjerg NE, Abrams J, et al. Leadership, inside and out: the tideswell-AGS-ADGAP emerging leaders in aging program. J Am Geriatr Soc. 2019;67(3):437–442. doi: 10.1111/jgs.15702 [DOI] [PubMed] [Google Scholar]
- 26.Busari JO. Management and leadership development in healthcare and the challenges facing physician managers in clinical practice. Int J Clin Leadership. 2012;17(4):211–216. [Google Scholar]
- 27.Fealy GM, McNamara MS, Casey M, et al. Service impact of a national clinical leadership development programme: findings from a qualitative study. J Nurs Manag. 2015;23(3):324–332. doi: 10.1111/jonm.12133 [DOI] [PubMed] [Google Scholar]
- 28.Stoller K, Barker J, FitzSimons K. Physician-leader on-boarding: the Cleveland Clinic experience. J Manage Devel. 2013;32(9):960–970. doi: 10.1108/jmd-06-2011-0072 [DOI] [Google Scholar]
- 29.Shekleton ME, Preston JC, Good LE. Growing leaders in a professional membership organization. J Nurs Manag. 2010;18(6):662–668. doi: 10.1111/j.1365-2834.2010.01152.x [DOI] [PubMed] [Google Scholar]
- 30.Welch-Carre E (2017). Influence of a hospital-based, internal leadership development program on leadership effectiveness. ProQuest LLC. Available from https://login.proxy.libraries.rutgers.edu/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=eric&AN=ED579917&site=ehost-live. Accessed July27, 2020.