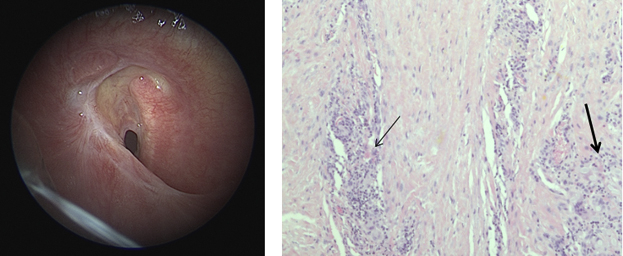
Preoperative laryngotracheal stenosis and postoperative pathologic findings.
Central Message.
In this case, we documented tracheal inflammation, vasculitis, and coagulative necrosis induced by SARS-CoV-2. Major airway healing after COVID-19 infection may not be a critical issue.
See Commentaries on pages 365 and 366.
Coronavirus disease 2019 (COVID-19) has quickly spread worldwide since the first reported case1, 2, 3 in Wuhan, China. Patients who need hospitalization for respiratory support require, in about 10% of cases, oro-tracheal intubation (OTI) for invasive ventilation and a tracheotomy whenever the patient is intubated for a long time and the prognosis is good.4
If a tracheotomy is deemed necessary in a patient with COVID-19, an open surgical tracheotomy is recommended over a percutaneous dilatation tracheotomy to minimize aerosol generation.5 Recently physicians at NYU Langone Health have developed a newer and perhaps safer approach to tracheotomy that, especially in patients with COVID-19, may reduce the risks of health care workers.6
The procedure should be performed at bedside, in a negative-pressure room, to minimize the risk of transmission during patient transport.5 However, the best strategy for tracheotomy in patients with COVID-19 is yet to be written in recommendations, and we continue to learn and evolve through experience.
Case Report
We present a case of a 53-year-old man who was admitted to a tertiary hospital complaining of fever (38.5°C), cough, and dyspnea. In his medical history, the patient reported systemic hypertension and 2 family members with COVID-19 infection. At the time of admission, oxygen saturation was 88%, and laboratory tests showed an enhanced C-reactive protein (4.58 mg/dL) and lymphopenia (740 cells per μL).
Chest radiograph showed multiple bilateral opacities and signs of interstitial pneumonia. A computed tomography (CT) scan was performed, which showed multiple ground-glass opacities extensively involving the lungs bilaterally, at the basis. A nasopharyngeal swab polymerase chain reaction test confirmed infection by severe acute respiratory syndrome coronavirus 2.
The patient was immediately isolated in a dedicated COVID-19 ward and was given supplemental oxygen and continuous positive airway pressure by helmet, antiviral (lopinavir/ritonavir), hydroxychloroquine, azithromycin, and dexamethasone. Ten hours later, the patient deteriorated, as well as the arterial oxygenation (partial pressure of oxygen 44 mm Hg and partial pressure of carbon dioxide 37 mm Hg). He was intubated (OTI) and transferred to an intensive care unit dedicated to COVID-19.
The patient slowly improved, and 15 days after OTI he underwent a bedside open surgical tracheotomy. It was described as a difficult operation because of a bleeding thyroid gland. The patient was progressively weaned from sedation and ventilation, 4 bronchoalveolar lavages in progressive days were negative for severe acute respiratory syndrome coronavirus 2, and 16 days later the tracheotomy was surgically closed. At that moment, bronchoscopy and/or laryngoscopy of the airway had not been performed.
When the patient was alert, collaborating, with a normal relaxed breathing, feeding with a free diet, he was transferred to a rehabilitation center. Twenty days after the closure of the tracheotomy, for the onset of mild inspiratory and expiratory dyspnea and on the suspicion of a tracheal stenosis, CT and tracheobronchoscopy were recommended.
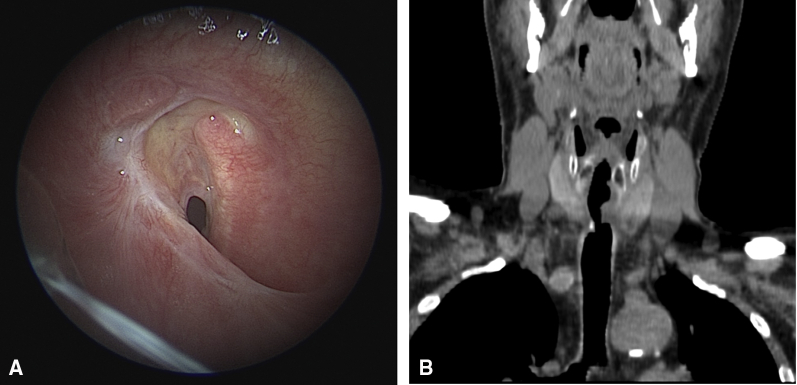
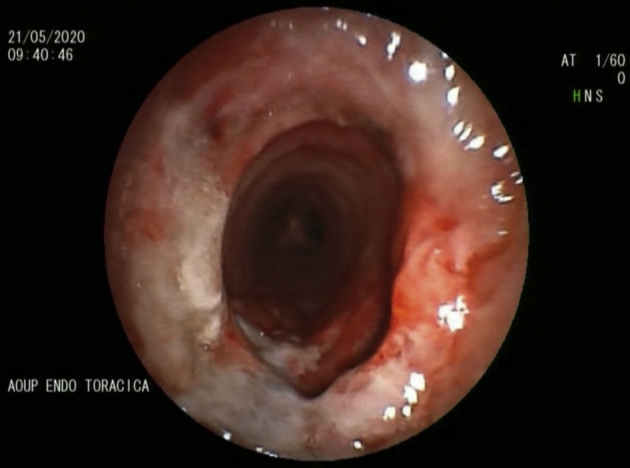
Bronchoscopy (Figure 1, A) revealed the result of a tracheotomy with cicatricial stenosis from probable ring fracture starting about 1.5 cm from the glottic plane (distal portion of the cricoid) and extending distally for about 2 cm, 25% residual tracheal caliber.
Figure 1.
Endoscopic view (A) and computed tomography scan of the neck (B) showing tracheal stenosis.
CT of the neck (Figure 1, B) showed the presence of a significant stenosis of the cervical trachea, with an hourglass morphology. It originated from the lower edge of the cricoid cartilage and extended longitudinally for about 1.5 cm, with a smaller caliber measurable in about 5 mm, within a framework of stenosis estimated at least 70% to 75% (tracheal diameter upstream and downstream of the stenosis of about 17-18 mm).
The pneumologist attempted a dilatation of the stenosis, which was not effective and then suggested a laryngotracheal resection. With the patient under general intravenous anesthesia, a transverse cervical incision of about 8 cm was performed (Video 1), removing the scar of the previous tracheotomy. Meticulous dissection of the cervical fascia, platysma, and pre-tracheal muscles allowed the visualization of the anterior tracheal wall.6
Video 1.
Diagnostic and surgical steps of the case. Video available at: https://www.jtcvs.org/article/S2666-2507(20)30398-9/fulltext.
The recurrent nerves having not been exposed, the distal resection begun by transection of the airway obliquely at the superior edge of the third tracheal ring. The distal trachea was intubated from the surgical field with a cuffed tracheal tube Bivona no. 6 (Smiths Medical, Dublin, Ohio), and the oral tracheal tube was retracted. We then resected the anterior cricoid arch, leaving a segment of the posterior plate of the cricoid above the posterolateral aspects of the mucous membrane in the subglottic region.
The membranous posterior part of the anastomosis was performed using a 4/0 absorbable running suture. The cartilaginous anterior part of the anastomosis was performed using a 3/0 absorbable single stiches suture. All the maneuvers of intubation from the field and then again through the oral tube were rapidly performed in apnea to reduce the aerosol contamination, with the anesthetist constantly monitoring the vital signs.
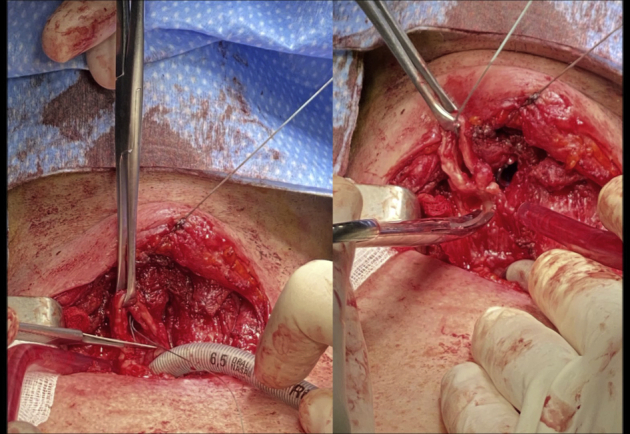
The postoperative course was characterized by a small dehiscence of a stich on the cartilaginous part of the anastomosis, which was treated conservatively, and healed in 7 days (Figure 2). We obtained informed consent of the patient for publication of his medical records.
Figure 2.
Postoperative laryngotracheal anastomosis.
Pathologic Examination
Macroscopic and Microscopic Findings
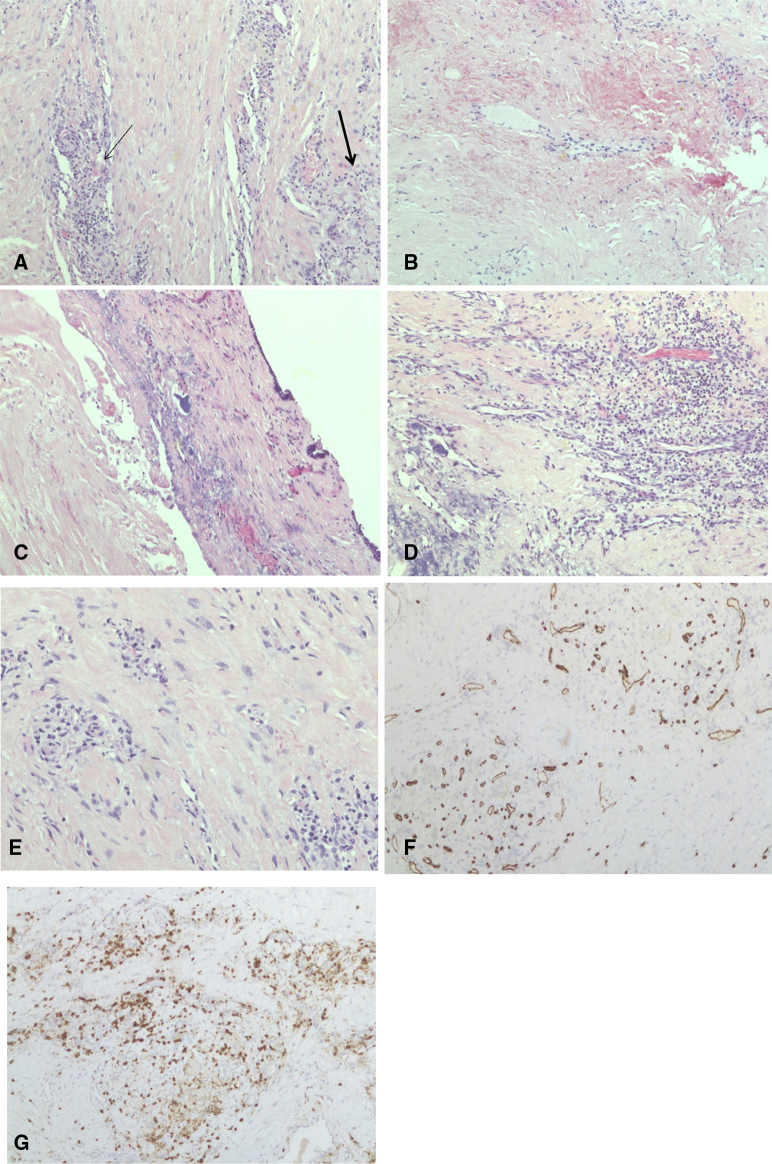
The sample of trachea showed small bleeding areas in the thickness of the mucosa of the cartilaginous portion. On microscopic examination, the mucosa sample displayed large areas of de-epithelization and microfoci of coagulative necrosis. Close to the pars membranacea, a rich vascular proliferation was present, with small- and medium-caliber vessels surrounded by a mix of lymphomonocytic and plasmacellular infiltrate. Some foci of granulocytic inflammation were also detected together with some occasional giant cell granulomas. Immunohistochemistry using CD3, CD4, CD8, CD20 PGM1 plasma cells, and CD31 and CD34 monoclonal antibodies was performed to evidence and characterize lympho-monocytic and plasma cellular infiltrate and to visualize the vessels wall (Figure 3).
Figure 3.
Pathologic findings in the tracheal specimen. A, Lymphomonocytic perivascular inflammatory infiltrate (thin arrow) and giant cell granulomas (thick arrow) (10×). B, Coagulative necrosis of the submucosal tissue with hemorrhage (10×). C, Coagulative necrosis of the submucosal tissue (10×). D, Coagulative necrosis with collateral dense perivascular inflammatory infiltrate (10×). E, Lymphomonocytic perivascular inflammatory infiltrate (20×). F, Neoangiogenesis of the submucosal tissue. Immunohistochemical stain with anti-CD34 antibody (10×). G, Perivascular lymphocytic infiltrate. Immunohistochemical stain with anti-CD3 antibody (10×).
Comment
Approximately 8% to 13% of patients admitted to modern intensive care units and requiring mechanical ventilation will undergo a tracheostomy.7 The major indication for tracheostomy is the possibility of mechanical ventilation for a long period of time without possible complications of a long-lasting OTI.4,5
Post-tracheotomy stenosis involving the cricoid cartilage is usually caused by high placement of a tracheotomy with rupture of the cricoid cartilage and of the first tracheal ring and infection at this level.8 Unfortunately, such injuries have become more frequent and present a more challenging technical problem as far as repair is concerned.9 The reasons for this increasing number of high airway lesions is uncertain, but we can assume that the placement of a tracheotomy in difficult scenario (such as an intensive care unit dedicated to COVID-19) or inflammation of the mayor airways (as it happens in patients with COVID-19 and it was confirmed in this case) may contribute to its further increase.9
It is reasonable to predict that the positive-pressure ventilation required in patients with COVID-19 with consequent intubation and later tracheotomy together with the inflammation of the airway for vasculitis phenomena may increase the rate of tracheal injuries and stenosis we may face in the near future.10
It appears that the COVID-19 pandemic presents an amazing challenge for surgical management of laryngotracheal stenosis because open airway access during laryngotracheal surgery create a high-risk situation for surgeons, anesthesiologists, and operating room personnel.11 While some surgical cases of laryngotracheal stenosis may be deferred, patients with significant airway obstruction or progressing symptoms often require urgent surgical intervention.11 Consequently, appropriate measures should be taken to prevent them and a discussion about their appropriate treatment and timing would be recommended.
Conclusions
In Italy,12 and worldwide, a high rate of patients affected by COVID-19 required, and are still requiring, tracheal intubation and tracheotomy for mechanical ventilation. The presence of platelet–fibrin thrombi in small arterial vessels caused by a coagulopathy appears to be common in patients with COVID-19, as detected in a series of autopsies in northern Italy.13 Inflammation, vasculitis, and coagulative necrosis of the major airways, induced by the virus, have been documented in this case. The fragility of the tracheal tissue, as well as difficult operative conditions, may be responsible of a high rate of tracheal injuries in the short term and will produce a high rate of tracheal sequelae in the long term.
Our case report emphasizes that:
-
1.
Meticulous surgical tracheostomy, either open or percutaneous, should be performed to mitigate the risk of post-tracheostomy stenosis, especially in patients with COVID-19.
-
2.
Intraoperative airway management to reduce aerosol-generating procedures and protect personnel while maintaining oxygenation and ventilation is critical, both during tracheotomy and tracheal resection; it requires teamwork and shared principles.
-
3.
As soon as the infection abates and the clinical conditions of the patient are adequate, surgical treatment of the tracheal or laryngotracheal stenosis is feasible.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Diagnostic and surgical steps of the case. Video available at: https://www.jtcvs.org/article/S2666-2507(20)30398-9/fulltext.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Ni Z.Y., Hu Y., Liang W., Ou C., He J., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Şentürk M., El Tahan M.R., Szegedi L.L., Marczin N., Karzai W., Shelley B., et al. Thoracic anesthesia of patients with suspected or confirmed 2019 novel coronavirus infection: preliminary recommendations for airway management by the European Association of Cardiothoracic Anaesthesiology Thoracic Subspecialty Committee. J Cardiothorac Vasc Anesth. 2020;34:2315–2327. doi: 10.1053/j.jvca.2020.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chao T.N., Braslow B.M., Martin N.D., Chalian A.A., Atkins J.H., Haas A.R., et al. Guidelines from the COVID-19 tracheostomy Task Force, a Working Group of the Airway Safety Committee of the University of Pennsylvania Health System. Tracheotomy in Ventilated Patients With COVID-19. Ann Surg. 2020;272:e30–e32. doi: 10.1097/SLA.0000000000003956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angel L., Kon Z.N., Chang S.H., Rafeq S., Shekar S.P., Mitzman B., et al. Novel percutaneous tracheostomy for critically ill patients with COVID-19. Ann Thorac Surg. 2020;110:1006–1011. doi: 10.1016/j.athoracsur.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tay J.K., Khoo M.L., Loh W.S. Surgical considerations for tracheostomy during the COVID-19 pandemic: lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg. March 31, 2020 doi: 10.1001/jamaoto.2020.0764. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Pearson F.G., Cooper J.D., Nelems J.M., Van Nostrand A.W. Primary tracheal anastomosis after resection of the cricoid cartilage with preservation of recurrent laryngeal nerves. J Thorac Cardiovasc Surg. 1975;70:806–816. [PubMed] [Google Scholar]
- 9.McGrath B.A., Brenner M.J., Warrillow S.J., Pandian V., Arora A., Cameron T.S., et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8:717–725. doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bassi M., Anile M., Pecoraro Y., Ruberto F., Martelli S., Piazzolla M., et al. Bedside transcervical transtracheal post-intubation injury repair in a Covid-19 patient. Ann Thorac Surg. April 22, 2020 doi: 10.1016/j.athoracsur.2020.04.009. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prince A.D.P., Cloyd B.H., Hogikyan N.D., Schechtman S.A., Kupfer R.A., Prince A.D.P., et al. Airway management for endoscopic laryngotracheal stenosis surgery during COVID-19. Otolaryngol Head Neck Surg. 2020;163:78–80. doi: 10.1177/0194599820927002. [DOI] [PubMed] [Google Scholar]
- 12.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carsana L., Sonzogni A., Nasr A., Roberta Rossi S., Pellegrinelli A., Zerbi P., et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis. June 8, 2020 doi: 10.1016/S1473-3099(20)30434-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagnostic and surgical steps of the case. Video available at: https://www.jtcvs.org/article/S2666-2507(20)30398-9/fulltext.