Highlights
-
•
Neurologic symptoms including headache are reported in COVID-19 patients.
-
•
Severe headache may be the sole presenting symptom of COVID-19 pneumonia.
-
•
Headache may precede respiratory symptoms for up to one week in COVID-19.
Keywords: COVID-19, SARS-CoV-2, Headache, Neurologic, Africa
Abstract
The spectrum of symptoms of COVID-19 continues to expand as more clinical observations are reported. Neurological manifestations including headache are increasingly described. However, headache as the sole presenting symptom of COVID-19 pneumonia has not been reported. We describe a patient in Tanzania who experienced severe headache for seven days before the onset of other symptoms of COVID-19 that led to her isolation, diagnosis, and treatment.
1. Introduction
COVID-19 is a global pandemic with cases reported in every World Health Organization (WHO) region [1]. The WHO African region has the lowest incidence rate with many countries reporting fewer than 1500 confirmed cases. The United Republic of Tanzania confirmed its first case on 16 March 2020 and to the date of this paper has reported 509 cases of COVID-19. The government has issued standard operating procedures for the screening, triaging, and isolation of suspected COVID-19 patients. We report the case of a woman with confirmed COVID-19 pneumonia who was admitted to Muhimbili National Hospital in Dar es Salaam, Tanzania, with the sole presenting symptom of severe headache. She was not suspected to have COVID-19 until she developed respiratory symptoms on the fifth day of admission.
2. Case report
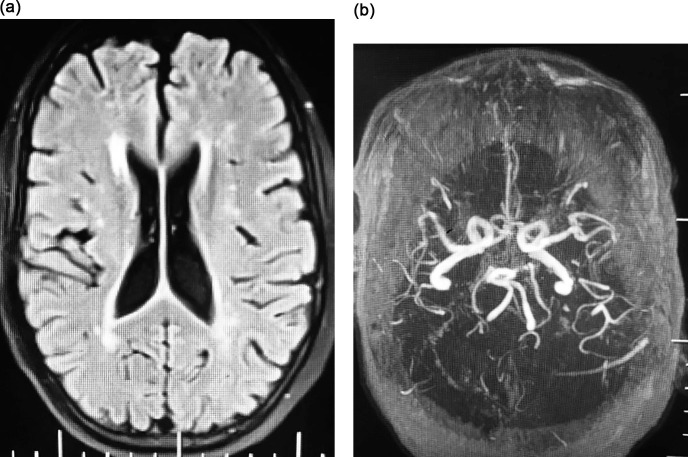
The patient is a 76-year-old female resident of a densely-populated area of Dar es Salaam. Her past medical history includes hypertension and chronic obstructive pulmonary disease. Her only complaint on presentation to the emergency department was severe generalized headache with pain extending to the neck for two days. She denied fever, cough, shortness of breath, sore throat, confusion, or seizure. On exam, she was afebrile, fully alert, and neurologically intact. Cranial nerve and motor exam were normal. She had no signs of meningeal irritation. She was admitted to the female general neurology ward. Brain CT could not be obtained because the scanner was under repair and consequently lumbar puncture was deferred. Brain MRI with contrast and MRA were requested and nimodipine was prescribed because of concern of aneurysmal subarachnoid hemorrhage. The MRI and MRA were completed on the fourth day of admission and did not show evidence for cerebral aneurysm, stroke, cerebral venous thrombosis, or meningitis (Fig. 1 ).
Fig. 1.
Brain MRI. A) axial FLAIR image showing nonspecific white matter hyperintensities. B) normal MRA at the level of the Circle of Willis.
On the fifth day of admission, the patient developed dry cough, shortness of breath, reduced appetite, and nausea with occasional vomiting. She was afebrile. Pulse oximetry showed an oxygen saturation of 90% on room air and chest X-ray revealed patchy bilateral lower lobe infiltrates (Fig. 2 ). The patient was transferred to the COVID-19 ward and placed on nasal cannula oxygen support. She was treated with intravenous amoxacllin/clavulanic acid, montelukast, salbutamol inhaler, and pantoprazole. A nasopharyngeal swab sample was obtained on the seventh day of admission and tested positive with SARS-CoV-2 Real-Time Reverse Transcriptase (rRT)-Polymerase Chain Reaction (PCR). Additional blood tests were ordered. Abnormal results included the following: C-reactive protein 124 mg/L, ESR 115 mm/hr, LDH 825 U/L, ferritin 538 ng/ml, hemoglobin 11.2 g/dL, and sodium 131 mmol/L. Normal results included the following: absolute lymphocyte count 2.12 × 109/L, platelet count 163 × 109/L, creatinine 79.5 µmol/L, and negative HIV 1/2 serology.
Fig. 2.

Chest X-ray showing bilateral lower lobe ground glass opacities.
On the ninth day of admission, she was transferred to a designated COVID-19 ward at another hospital in Dar es Salaam. She was treated with azithromycin 500 mg daily for six days and is receiving enoxaparin 60 mg twice daily. Her headache resolved completely in one week and she has not developed any other neurological symptoms. Her respiratory status is improving, and she no longer requires supplemental oxygen.
3. Discussion
In a meta-analysis of 38 retrospective studies involving 3062 COVID-19 patients in China, headache was recorded at a frequency of 15.4% [2]. In an observational study of mild to moderate COVID-19 patients treated in Europe, defined as not requiring intensive care, headache was reported by 70.3% of participants using a standardized questionnaire [3]. However, the severity of headache and the timing of headache symptoms in relation to respiratory symptoms were not described in these reports. Our patient presented with symptoms of severe generalized headache without respiratory symptoms or fever and was not suspected to have COVID-19 until she developed dry cough, shortness of breath, and hypoxia on the fifth day of admission. Except for holocephalic headache, she did not have clinical symptoms or signs of increased intracranial pressure. Since lumbar puncture was not done, we cannot exclude the possibility of meningitis due to SARS-CoV-2 infection. However, brain MRI did not show leptomeningeal enhancement or hydrocephalus. Her headache fulfilled criteria for acute headache attributed to systemic viral infection (9.2.2.1) according to the International Classification of Headache Disorders, 3rd edition [4]. The pathophysiology of headache associated with COVID-19 is not known. Acute neurologic conditions reported with COVID-19 include stroke and Guillain–Barré Syndrome [5], [6], [7].
4. Conclusion
Patients admitted with acute severe headache without identified intracranial pathology should be screened daily for at least one week for other COVID-19 symptoms and considered for early isolation and testing with SARS-CoV-2 rRT-PCR to prevent exposure of other patients and hospital staff.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
Dr. Chin is grateful to Muhimbili University of Health and Allied Sciences for the opportunity to support, teach, and mentor the physicians and students at Muhimbili National Hospital.
Study Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.inat.2020.100882.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Coronavirus Resource Center at Johns Hopkins University & Medicine, https://coronavirus.jhu.edu.
- 2.Zhu J., Ji P., Pang J. Clinical characteristics of 3,062 COVID‐19 patients: a meta‐analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lechien J.R., Chiesa-Estomba C., Place S. Clinical and epidemiological characteristics of 1,420 European patients with mild-to-moderate coronavirus disease 2019. J. Intern. Med. 2020 doi: 10.1111/JOIM.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. Cephalalgia. 2018;38(1):1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 5.Li Y., Li M., Wang M. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc. Neurol. 2020 doi: 10.1136/svn-2020-000431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oxley T.J., Mocco J., Majidi S. Large Vessel Stroke as a Presenting Feature of COVID-19 in the Young. N. Engl. J. Med. 2020;382 doi: 10.1056/NEJMc200978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toscano G., Palmerini F., Ravaglia S. Guillain-Barré Syndrome Associated with SARS-CoV-2. N. Engl. J. Med. 2020;382:2574–2576. doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.