Abstract
Background:
Cocaine-involved overdose mortality has recently risen in the United States (US), yet it is unclear to what extent patterns in cocaine-involved overdose mortality parallel patterns in cocaine use. This study: examined time trends (2002–2018) in past-year cocaine use and cocaine-involved overdose mortality in the US; and compared demographics and drug involvement of adults who reported past-year cocaine use versus adults who died of a cocaine-involved overdose.
Methods:
Data from two sources were utilized: (1) the National Survey on Drug Use and Health (n=1,334 adults self-reporting cocaine use in 2018); and (2) the Multiple Cause of Death dataset of the National Center for Health Statistics (N=14,630 adults who died of a cocaine-involved overdose in 2018). The study examined prevalence of past-year cocaine use, mortality rates for cocaine-involved overdose, 2002–2018 trends, demographic characteristics, and involvement of other drugs.
Results:
Results of Joinpoint Regression indicated that the prevalence of past-year cocaine use increased after 2011, with an annual percent change of 5.13, while age-adjusted cocaine-involved overdose mortality rates escalated after 2012, with an annual percent change of 26.54. In 2018, prevalence of past-year cocaine use did not significantly differ (p=0.09) by racial/ethnic group, yet Non-Hispanic Blacks had an age-adjusted cocaine-involved overdose mortality rate more than double the rate in Non-Hispanic Whites and significantly higher (p<0.001) than in any other group.
Conclusions:
While the prevalence of cocaine use has increased modestly, cocaine-involved overdose mortality has risen dramatically. Cocaine-involved overdose mortality is disproportionately affecting individuals who are Black, older, or with lower educational attainment.
Keywords: cocaine use, drug overdose, overdose mortality
1. Introduction
In 2018, more than one in five fatal drug overdoses in the United States (US) involved cocaine, representing 14,666 deaths (Centers for Disease Control and Prevention [CDC], 2020). Cocaine-involved overdose mortality has recently surged in the US, with mortality rates more than tripling from 2012 to 2018 (Hedegaard et al., 2020). Cocaine-involved overdose mortality is projected to continue escalating, with the potential to approach levels comparable to recent rates of opioid overdose deaths (Drug Enforcement Administration [DEA], 2019a).
The recent increase in cocaine-involved overdose mortality in the US has accompanied record-high cocaine purity, availability, and affordability, largely attributed to increased levels of Colombian coca cultivation (DEA, 2019a). It is unclear, however, whether recent increases in cocaine-involved overdose mortality parallel increases in the number of Americans using cocaine. An analysis of two population surveys of non-institutionalized US adults revealed increases in the prevalence of past-year cocaine use between the time periods of 2001–2002 and 2012–2013 for nearly all sociodemographic groups (Kerridge et al., 2019). However, a study using survey data from non-institutionalized individuals ages 12 and older reported increases in prevalence of past-year cocaine use between 2011 and 2015 in a few demographic groups only (e.g., women, individuals aged 18–25 or 50+, and non-Hispanic Blacks; John and Wu, 2017). Overall, trends in past-year cocaine use in the US have fluctuated over the course of the past 15 years (Substance Abuse and Mental Health Services Administration, 2019).
Increases in cocaine-involved overdose mortality rates may be partially explained by improvements in postmortem toxicology testing and drug-reporting in mortality data (Hedegaard et al, 2020), as well as increased risk associated with using cocaine, often related to polysubstance use (Jones et al., 2017) and exposure to the synthetic opioid fentanyl, which is highly potent and lethal even in miniscule quantities (DEA, 2019b). Some individuals who use cocaine are exposed to fentanyl through co-use of cocaine and heroin (when heroin is adulterated or substituted with fentanyl); laboratory submissions of “speedballs” (cocaine and heroin) with and without fentanyl have recently increased (DEA, 2019a). At the same time, fentanyl has also been detected in samples of cocaine, as a result of contamination or drug adulteration (DEA, 2019a). Data on drug seizures (DEA, 2019a), an analysis of a sample of one million urine drug tests (LaRue et al., 2019), and reports of clustered overdose outbreaks (Armenian et al., 2019; Khatri et al., 2018) indicate a disconcerting and rising risk of exposure to fentanyl among individuals who use cocaine.
Given this confluence of factors, research is needed to better characterize recent trends and risk factors for cocaine-involved overdose mortality. An understanding of the differences between risk profiles for cocaine use versus cocaine-involved overdose mortality is key in informing interventions targeting those at high risk of overdose death. The present study first examined the demographic characteristics of adults who reported past-year cocaine use in 2018 (in the civilian, non-institutionalized National Survey on Drug Use and Health [NSDUH] sample) and adults who died of a cocaine-involved overdose during 2018 (using national mortality data). Prevalence estimates for past-year cocaine use, and cocaine-involved overdose mortality rates, were computed by sex, age, and race/ethnicity, in order to identify and compare the groups most affected by cocaine use versus cocaine-involved overdose mortality. Next, the study examined the co-use of various drugs among adults using cocaine, as well as the co-involvement of other drugs in cocaine-involved overdose deaths. Finally, trends from 2002–2018 were tested for: the prevalence of past-year cocaine use (in the civilian, non-institutionalized adult NSDUH sample); and age-adjusted cocaine-involved overdose mortality rates among US adults.
2. Methods
2.1. Data
The study utilized two data sources: (1) public-use data from the NSDUH dataset from the Substance Abuse and Mental Health Services Administration; and (2) mortality data from the public-access Multiple Cause of Death (MCD) dataset of the National Center for Health Statistics. The NSDUH gathers data on substance use and health behaviors among the US civilian, non-institutionalized population age 12 or older, utilizing stratified multistage area probability sampling. The analytic sample of the present study consisted of the 1,334 adults (ages 18 and older) who responded affirmatively to questions regarding use of “cocaine in any form” during the prior 12 months, in the 2018 survey. NSDUH data from 2002 to 2018 were also utilized to obtain prevalence estimates of past-year cocaine use among adults each year.
The MCD dataset contains death certificate information from all deaths in the United States. The present study was restricted to deaths of adult US residents, occurring in the 50 states or District of Columbia, for which the underlying cause of death was specified as drug overdose (International Classification of Diseases [ICD]-10 codes X40-X44, X60–64, X85, or Y10-Y14) and for which cocaine (ICD-10 code T40.5) was listed as a “multiple cause of death.” On the death certificate, demographics of the decedent are provided by the funeral director, generally with assistance from the decedent’s next of kin (Arias et al., 2016), while death-related information is supplied by the medical certifier (e.g., a coroner or medical examiner; Brooks and Reed, 2015). After excluding seven decedents for whom age was not reported, the present study focused on the 14,630 adults who died of a cocaine-involved overdose in 2018. Data from the years 2002 to 2018 were also utilized to compute age-adjusted cocaine-involved overdose mortality rates among adults for each year.
2.2. Measures
2.2.1. Demographics
Sex, age, race/ethnicity, educational attainment, and marital status were included as demographic variables. Demographics were based on self-report in NSDUH and based on the report of a funeral director (often informed by a next of kin) in mortality data. In the present study, sex was categorized as male or female. The following age categories were utilized: 18–25, 26–34, 35–49, 50–64, and 65 and older. Race/ethnic group was classified as Non-Hispanic (NH) White, NH Black, Hispanic, NH American Indian/Alaska Native, NH Asian or Pacific Islander, or “other.” “Other” was utilized for cases in which data were insufficient to classify an individual into one of the aforementioned racial/ethnic categories, that is, individuals who identified with “two or more races” in NSDUH (2.97%, weighted estimate) and individuals with missing race/ethnicity data on the death certificate (0.74%). For educational attainment, the following categories were utilized: less than a high school diploma; high school diploma or General Education Diploma (GED); some college or associate’s degree; and a college degree or higher. “Unknown” educational attainment applied to mortality data only (3.10%). In the present study, marital status was categorized as either “never married” or “married, widowed, divorced, or separated,” in order to accommodate differences in the categories utilized in NSDUH versus death certificate data. The marital status of “unknown” applied to mortality data only (2.19%).
2.2.2. Other drug involvement
The study examined the percentage of adults reporting past-year cocaine use who also reported past-year use of other drugs, as well as the percentage of cocaine-involved overdose deaths that also involved another drug. In NSDUH, data were based on self-report of drugs used within the past year; for mortality data, drug involvement was indicated via ICD codes in the death certificate’s multiple cause of death section. Drug categories examined in the present study included: any opioid; heroin; prescription opioids (excluding methadone); methadone; synthetic opioids (e.g., fentanyl) excluding methadone; benzodiazepines; and psychostimulants with abuse potential (e.g., methamphetamine). Table 1 details the criteria utilized to define involvement of these drug categories in the NSDUH data and mortality data.
Table 1.
Criteria utilized for defining involvement of specified drugs, for NSDUH data and mortality data (Multiple Cause of Death dataset)
| Drug | ||
|---|---|---|
| Any opioid | Heroin, hydrocodone, oxycodone, oxymorphone, hydromorphone, morphine, or codeine products, methadone, buprenorphine, pharmaceutical fentanyl, Demerol, or Tramadol | T40.0-T40.4 or T40.6 (opium, heroin, natural/semisynthetic prescription opioids, methadone, or synthetic opioids) |
| Heroin | Heroin | T40.1 (heroin) |
| Prescription opioida | Hydrocodone, oxycodone, oxymorphone, hydromorphone, morphine, or codeine products | T40.2 (natural and semisynthetic “other opioids,” e.g., codeine, hydromorphone, morphine, and oxycodone) |
| Methadone | Methadone | T40.3 (methadone) |
| Synthetic opioid | n.a. (NSDUH does not include questions about all drugs in the synthetic opioids category, and some synthetic opioids are often consumed unknowingly, unlikely to be accurately identified by self-report) | T40.4 (“other synthetic narcotics excluding methadone;” e.g., pharmaceutical or illicitlymanufactured fentanyl, fentanyl analogs, other novel synthetic opioids, Tramadol, and buprenorphine) |
| Benzodiazepine | Benzodiazepine tranquilizer or benzodiazepine sedative | T42.4 (benzodiazepine) |
| Psychostimulant with abuse potential | Methamphetamine, amphetamine or methylphenidate (e.g., Ritalin) products, or 3,4-Methylenedioxymethamphetamine (MDMA/Ecstasy) | T43.6 (“psychostimulant with abuse potential, excluding cocaine;” e.g., methamphetamine, amphetamine, methylphenidate, MDMA, caffeine; T43.6 overdose deaths most frequently involve methamphetamine; Ossiander, 2014) |
Notes.
Other prescribed opioids that correspond to different ICD-10 categories (e.g., methadone) were not included in this category. Abbreviations. NSDUH: National Survey on Drug Use and Health; ICD: International Classification of Diseases; n.a.: not applicable.
2.3. Statistical analysis
Descriptive analyses were conducted to examine relative frequencies of demographic characteristics, as well as other drug involvement, for: individuals reporting past-year cocaine use in NSDUH; and cocaine-involved overdose decedents from mortality data. For NSDUH data, survey weights were utilized and 95% confidence intervals (CIs) were computed. No CIs were necessary for the descriptive analyses using mortality data, as these data represent a census, rather than a sample, of all deaths reported as cocaine-involved overdoses.
Past-year prevalence of cocaine use among adults in NSDUH was computed using survey weights, for each year from 2002 to 2018, and stratified by demographic group for 2018. Age-specific cocaine-involved overdose rates were obtained through the online platform for mortality data, CDC WONDER, which utilizes bridged-race intercensal estimates for population denominators (CDC, 2020). Age-adjusted cocaine-involved overdose mortality rates (for the years 2002–2018, and by sex and racial/ethnic group for 2018) were also computed using US Census Bureau bridged-race intercensal estimates for population denominators. These rates were age-adjusted via the direct method, using age distribution #9 of the 2000 US standard population (Klein and Schoenborn, 2001), with 95% CIs calculated via the gamma method with the user-written program distrate (Consonni et al., 2012). Analyses were conducted in Stata/MP 16.0.
For prevalence estimates from NSDUH data, a chi-square test was utilized to test for significant differences within each group. For mortality rates, non-overlapping 95% CIs were considered evidence of a statistically significant difference between groups, while post-hoc z-tests (two-tailed, α = 0.05) were conducted to obtain specific p values and to test the significance of differences with overlapping confidence intervals, considering that a difference may be significant even if confidence intervals overlap (Schenker and Gentleman, 2001).
Lastly, Joinpoint Regression (version 4.7.0.0; National Cancer Institute, 2019) was utilized to characterize time trends between 2002 and 2018 for prevalence of past-year cocaine use and age-adjusted cocaine-involved overdose mortality rates. Also known as piecewise, segmented, or broken line regression (Kim et al., 2000), Joinpoint Regression examines a range of data and uses various methods (e.g., permutation tests or the Bayes information criterion) to identify the model with the best-fitting set of joinpoints (i.e., points indicating significant trend changes along line segments). In the present study, permutation tests were utilized in selection of the optimal joinpoint regression model, using Monte Carlo simulations (α = 0.05, with Bonferroni correction; Kim et al., 2000).
The Joinpoint Regression software provided annual percent change (APC) to characterize trends over time, assuming change at a constant percentage of the value in the previous year, in a log-linear model (National Cancer Institute, 2019). A significance test for annual percent change, and average annual percent change for the entire time period, were also computed by Joinpoint Regression. In order to depict 95% confidence intervals of prevalence estimates and mortality rates, results of Joinpoint Regression analyses were plotted using Microsoft Excel.
3. Results
3.1. Demographics
Table 2 presents the demographic characteristics of civilian non-institutionalized adults who reported cocaine use within the past year in the 2018 NSDUH (hereafter referred to as “cocaine users”). Demographic characteristics from mortality data are also presented for adults who died of a cocaine-involved overdose in the US in 2018 (hereafter referred to as “cocaine overdose decedents”). Table 3 provides prevalence estimates for past-year cocaine use, and cocaine-involved overdose mortality rates, by sex, age, and racial/ethnic group. Education and marital status are not included in Table 3 because bridged-race intercensal estimates by education or marital status were unavailable for rate calculation.
Table 2.
Demographic characteristics of adults reporting past-year cocaine use (civilian, non-institutionalized; n=1,334, from NSDUH) and adults who died of a cocaine-involved overdose (N=14,630, from Multiple Cause of Death [MCD] Dataset) in the United States in 2018
| Characteristic | NSDUH Past-year Cocaine Users,a % (95% CI) | MCD Mortality Data Past-year Cocaine Decedents,b % |
|---|---|---|
| Sex | ||
| Male | 63.78 (59.33–68.00) | 71.18 |
| Female | 36.22 (32.00–40.67) | 28.82 |
| Age, years | ||
| 18–25 | 35.96 (32.53–39.53) | 7.58 |
| 26–34 | 33.07 (29.85–36.46) | 22.56 |
| 35–49 | 18.63 (15.87–21.76) | 35.80 |
| 50–64 | 11.72 (8.68–15.64) | 30.29 |
| 65+ | 0.62 (0.24–1.61) | 3.78 |
| Race/Ethnicity | ||
| White (Non-Hispanic) | 65.73 (62.51–68.82) | 59.13 |
| Black (Non-Hispanic) | 11.37 (8.37–15.27) | 27.04 |
| Hispanic | 14.89 (12.53–17.61) | 11.66 |
| AI/AN (Non-Hispanic) | 0.63 (0.32–1.24) | 0.59 |
| Asian/PI (Non-Hispanic) | 4.41 (2.96–6.51) | 0.84 |
| Other | 2.97 (2.12–4.13) | 0.74 |
| Education | ||
| Less than High School Diploma | 9.97 (7.72–12.78) | 20.94 |
| High School Diploma or GED | 22.05 (19.01–25.43) | 50.83 |
| Some College/Associate’s Degree | 35.83 (32.07–39.78) | 18.89 |
| College Degree or Higher | 32.15 (27.50–37.18) | 6.23 |
| Unknown | n.a. | 3.10 |
| Marital Status | ||
| Married/Widowed/Divorced/Separated | 27.47 (24.36–30.82) | 39.88 |
| Never Married | 72.53 (69.18–75.64) | 57.92 |
| Unknown | n.a. | 2.19 |
Notes.
Weighted results from the National Survey on Drug Use and Health (NSDUH) for the civilian, non-institutionalized US population, for adults who self-reported past-year use of cocaine in the 2018 survey.
Results from death certificates of all US adult resident deaths in 2018 with “drug overdose” specified as an underlying cause of death and cocaine listed as an involved drug. No 95% CIs were included as mortality data represent a census, rather than a sample. Abbreviations. CI, confidence interval; n.a., not applicable; AI/AN, American Indian/Alaska Native; PI, Pacific Islander; GED, General Education Diploma.
Table 3.
Past-year prevalence of cocaine use for civilian, non-institutionalized adults (from NSDUH), and cocaine-involved overdose mortality rates for adults (from Multiple Cause of Death [MCD] dataset), in the United States in 2018, by sex, age, and race/ethnicity
| Characteristic | NSDUH Prevalence of past-year cocaine use,a % (95% CI) | MCD Mortality Data Cocaine overdose mortality rate,b per 100,000 (95% CI) |
|---|---|---|
| Sex | ||
| Male | 2.87 (2.56–3.22) | 8.63 (8.47–8.80) |
| Female | 1.52 (1.33–1.74) | 3.48 (3.38–3.59) |
| Age, years | ||
| 18–25 | 5.72 (5.19–6.30) | 3.16 (2.98–3.35) |
| 26–34 | 4.47 (3.95–5.07) | 8.03 (7.76–8.30) |
| 35–49 | 1.65 (1.36–2.00) | 8.44 (8.21–8.67) |
| 50–64 | 1.02 (0.73–1.42) | 7.02 (6.81–7.22) |
| 65+ | 0.01 (0.01–0.17) | 1.05 (0.97–1.14) |
| Race/Ethnicityc | ||
| White (Non-Hispanic) | 2.26 (2.08–2.45) | 6.08 (5.95–6.21) |
| Black (Non-Hispanic) | 2.08 (1.51–2.86) | 12.40 (12.02–12.80) |
| Hispanic | 1.99 (1.65–2.40) | 3.97 (3.78–4.17) |
| AI/AN (Non-Hispanic) | 2.35 (1.14–4.79) | 4.32 (3.44–5.35) |
| Asian/PI (Non-Hispanic) | 1.58 (1.07–2.34) | 0.74 (0.61–0.88) |
Notes.
Weighted results from the National Survey on Drug Use and Health (NSDUH) for the civilian, non-institutionalized US population, for adults in the 2018 survey; n=43,026.
Results for drug overdose deaths involving cocaine among adults in the US in 2018; rates by sex and race/ethnicity are age-adjusted, while rates for specific age categories are crude rates.
Data for “other” race/ethnicity not available. Abbreviations. CI, confidence interval; AI/AN, American Indian/Alaska Native; PI, Pacific Islander.
Men were over-represented both among cocaine users and cocaine overdose decedents; the prevalence of past-year cocaine use was nearly double in men compared to women, and the age-adjusted cocaine-involved overdose mortality rate was more than twice as high in men than in women. Age distributions differed between cocaine users and cocaine overdose decedents, with cocaine users concentrated in younger ages (with the highest proportion in age categories 18–25 and 26–34) compared to cocaine overdose decedents (with the highest proportion in age categories 35–49 and 50–64). Prevalence of past-year cocaine use was highest among those 18–25 years, while the cocaine-involved overdose mortality rate was highest in the age group 35–49.
Differences in race/ethnicity between cocaine users and cocaine overdose decedents were also observed. While NH Blacks constituted 11.37% (95% CI, 8.37–15.27) of cocaine users, they represented 27.04% of the cocaine overdose decedents. Although past-year prevalence of cocaine use was relatively similar (and did not significantly differ; p=0.09) across all racial/ethnic groups, NH Blacks had an age-adjusted cocaine-overdose mortality rate more than double the rate in NH Whites, more than triple the rate in Hispanics, and significantly higher (p<0.001) than in any other group.
Educational attainment also differed between cocaine users and cocaine overdose decedents. The largest percentages of cocaine users reported attaining some college, an associate’s degree, or a college degree or higher, while nearly three in four (71.77%) cocaine overdose decedents had an educational attainment less than or equal to a high school diploma or GED. Almost three in four (72.53% [95% CI, 69.18–75.64]) cocaine users had never been married, compared to 57.92% of cocaine overdose decedents.
3.2. Involvement of other drugs
Table 4 presents the percentage of cocaine users who also reported use of another drug, as well as the percentage of cocaine-involved overdose deaths also involving another drug. Half (50.10% [95% CI, 46.58–53.62]) of cocaine users reported using some type of opioid in the past year; 45.48% (95% CI 42.14–48.87) reported use of a prescription opioid excluding methadone. Nearly three of every four (74.22%) cocaine-involved overdose deaths also involved an opioid, with 59.06% involving a synthetic opioid. More than half (54.56% [95% CI, 50.52–58.54]) of cocaine users reported past-year use of a “psychostimulant with abuse potential” (a category including methamphetamine, amphetamine products, and MDMA), while approximately one in ten (9.97%) cocaine-involved overdose deaths included “psychostimulants with abuse potential” as a cause of death.
Table 4.
Use of other drugs in addition to cocaine (among civilian, non-institutionalized adults, from NSDUH), and involvement of other drugs in cocaine-involved overdose deaths among US adults (from Multiple Cause of Death [MCD] Dataset), 2018
| Other drug involved | NSDUH Cocaine users reporting use of another drug, past year,a % (95% CI) | MCD Mortality Data Cocaine overdose deaths also involving another drug,b % |
|---|---|---|
| Any opioidc | 50.10 (46.58–53.62) | 74.22 |
| Heroin | 8.81 (6.27–12.24) | 26.71 |
| Prescription opioidd | 45.48 (42.14–48.87) | 12.52 |
| Methadone | 4.56 (3.15–6.56) | 3.25 |
| Synthetic opioide | n.a. | 59.06 |
| Benzodiazepine | 39.83 (36.58–43.18) | 13.84 |
| Psychostimulant with abuse potentialf | 54.56 (50.52–58.54) | 9.97 |
Notes.
Weighted results from the 2018 National Survey on Drug Use and Health (NSDUH) for adults who self-reported past-year use of cocaine.
Data for drug overdose deaths involving cocaine among adults in the US in 2018. No 95% CIs were included as mortality data represent a census, rather than a sample.
Including opium, heroin, prescription opioids, methadone, and synthetic opioids.
Hydrocodone, oxycodone, oxymorphone, hydromorphone, morphine, or codeine products; excludes methadone.
Excluding methadone; n.a. for NSDUH, as NSDUH does not report on all drugs in the synthetic opioid category.
Methamphetamine, amphetamine or methylphenidate products, or 3,4-Methylenedioxymethamphetamine (MDMA); deaths involving psychostimulants with abuse potential most frequently involve methamphetamine (Ossiander, 2014). Abbreviations. CI, confidence interval; n.a., Not applicable.
3.3. Time trends
Figure 1 depicts time trends in prevalence of past-year cocaine use, and age-adjusted cocaine-involved overdose mortality rates, among adults in the US. For prevalence of past-year cocaine use, two joinpoints were identified in the trend from 2002–2018. The annual percent change (APC) of −1.42 for 2002–2008 and −11.71 for 2008–2011 did not significantly differ from zero (p=0.30 and p=0.23, respectively). From 2011 to 2018, a significant (p<0.01) increasing trend in prevalence was observed, with an APC of 5.13. The average annual percent change over the entire time period (2002–2018), however, did not significantly differ from zero (p=0.72). In sensitivity analyses, the mean number of days of cocaine use each year (for adults reporting past-year use), did not significantly differ between 2002 (43.00 [95% CI, 37.23–48.78]) and 2018 (35.95 [95% CI, 28.76–43.15]).
Figure 1.
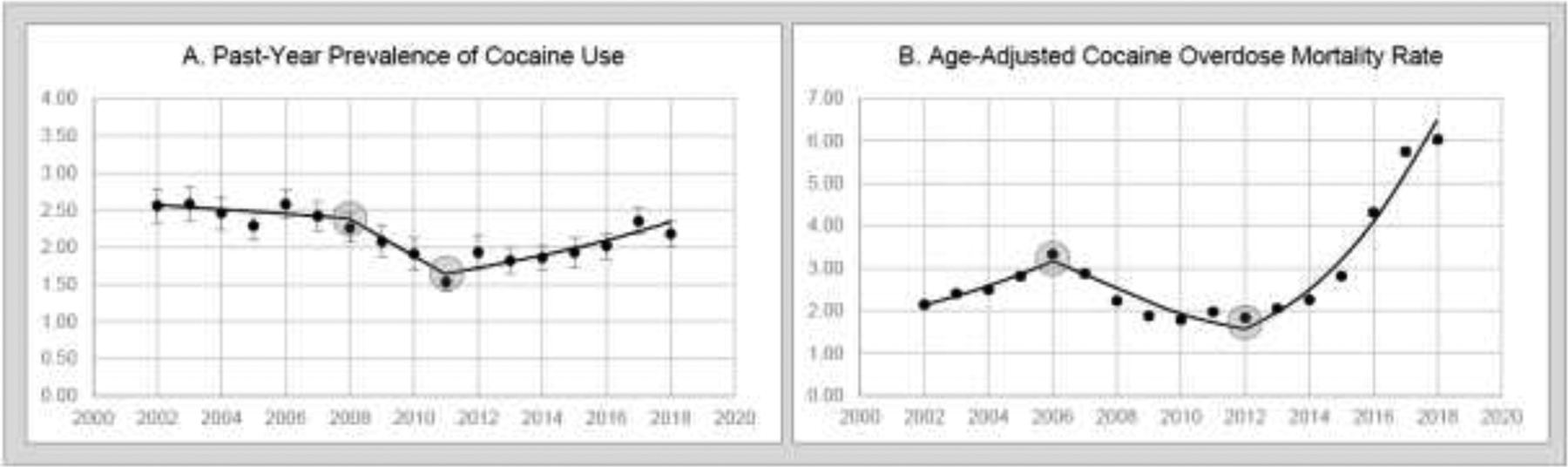
A. Past-year prevalence (and 95% confidence intervals) of cocaine use among U.S. civilian non-institutionalized adults, 2002–2018 (weighted results from NSDUH). B. Age-adjusted cocaine overdose mortality rates (and 95% confidence intervals) for U.S. adults, 2002–2018 (source: Multiple Cause of Death Dataset)
Notes. Joinpoints are represented by circles, and lines connecting joinpoints are fitted via Joinpoint Regression (National Cancer Institute, 2019).
For trends in age-adjusted cocaine-involved overdose mortality rates among adults from 2002 to 2018, two joinpoints were identified. From 2002–2006, the APC of 9.46 was not significantly different from zero (p=0.13). From 2006–2012, a significant (p<0.05) decrease was observed with an APC of −10.50, and from 2012–2018, a significant (p<0.001) increase was observed with an APC of 26.54. The average annual percent change over the entire time period (2002–2018) was 7.17 (p<0.01), with the age-adjusted cocaine-involved overdose mortality rate rising from 2.14 (95% CI, 2.08–2.20) in 2002 to 6.03 (95% CI, 5.93–6.13) in 2018.
4. Discussion
Results of the study highlighted similarities and contrasts in the demographic profiles of civilian, non-institutionalized US adults reporting past-year cocaine use and US adults who died of a cocaine-involved overdose. Consistent with documented sex differences in drug use (Salas-Wright et al., 2016), males were overrepresented among adults reporting past-year cocaine use, and even more so among adults who died of a cocaine-involved overdose. The prevalence of past-year cocaine use was highest for young adults, while cocaine-involved overdose deaths were concentrated in relatively older, or middle-aged, groups. Although prevalence of past-year cocaine use did not significantly differ by race/ethnicity, the age-adjusted cocaine-involved overdose mortality rate among NH Blacks was significantly higher than in any other racial/ethnic group and was double the rate in NH Whites.
Disproportionately high rates of cocaine-involved overdose mortality in NH Blacks have been previously documented (Shiels et al., 2018), yet findings of the present study suggest that the difference in cocaine-involved overdose mortality rates between NH Blacks and NH Whites may not be simply explained by rates of past-year cocaine use in each group. Other drug use-related factors may play a role, such as frequency, quantity, history, or route of cocaine use, use of crack instead of powder cocaine (Palamar et al., 2015), or polysubstance use. At the same time, the high mortality burden in NH Blacks may be symptomatic of disparities in socioeconomic disadvantage (Palamar et al., 2015), exposure to adversity (Fothergill et al., 2016), underlying medical conditions (Han et al., 2019), comorbidity (Huang et al., 2006), rates of substance use disorder treatment completion (Saloner et al., 2013), marginalization, use of drugs while alone, or fear of calling 911 when witnessing an overdose (Wagner et al., 2019). The overrepresentation of NH Blacks among the cocaine-involved overdose decedents, relative to the civilian, non-institutionalized adults reporting past-year cocaine use, mirrors the history of disparities related to drug use in Blacks in the US, including criminal justice involvement and incarceration (Iguchi et al., 2005), crack versus powder cocaine sentencing (Palamar et al., 2015), and the contrasting responses to the crack-cocaine epidemic of the 1980s versus the opioid epidemic of the 2000s (Netherland and Hansen, 2017).
The older age distribution of cocaine-involved overdose decedents, compared to individuals reporting past-year cocaine use, may also be connected to race/ethnicity, as suggested by the previously documented older ages of NH Black overdose decedents compared to NH White and Hispanic decedents (Shiels et al., 2018) and the cohort aging effect for cocaine-involved overdose mortality in Black individuals (Jalal et al., 2018). Relatively older cocaine-involved overdose decedents may include populations of individuals who initiated cocaine use during the crack-cocaine epidemic of the 1980s, as well as aging baby-boomers (Wu and Blazer, 2011). The use of cocaine throughout the life course may have cumulative effects, as cocaine has both acute and chronic impacts on functioning and health (Kloner et al., 1992), and older adults are often more vulnerable to the cardiovascular effects of cocaine (Egred and Davis, 2005).
Findings of the present study indicated that the time trends in age-adjusted cocaine-involved overdose mortality did not closely mirror the trends in past-year prevalence of cocaine use. Although both indicators increased over the past few years (with prevalence rising after 2011 and mortality rising after 2012), the rate of increase was far more pronounced for overdose mortality. Moreover, the prevalence of past-year cocaine use in 2018 did not significantly differ from the prevalence in 2002, while the age-adjusted cocaine-involved overdose mortality rate in 2018 was nearly triple the 2002 rate. Recent analyses suggest that the dramatic increases in cocaine-involved overdose mortality may be largely attributed to the involvement of opioids, especially synthetic opioids such as fentanyl (Jones et al., 2017).
The central role of opioids in both cocaine use and cocaine-involved overdose mortality is supported by the present study’s findings, as approximately half of adults reporting past-year cocaine use reported use of an opioid, and opioids were involved in nearly three of four cocaine-involved overdose deaths. These findings suggest the need for strategies that acknowledge and address polysubstance use, rather than focusing on opioid misuse alone. The risk of fentanyl exposure among cocaine users necessitates the dissemination of fentanyl education and naloxone training for at-risk individuals using cocaine (Nolan et al., 2019). The relatively older age distribution of cocaine-involved overdose decedents supports the need for screening, intervention, and treatment targeting older age groups, informed by recognition of drug addiction as a chronic disease which requires management throughout the life course (Hser et al., 2007). Finally, the disproportionate cocaine-involved overdose mortality burden in NH Blacks requires initiatives employing culturally-appropriate approaches spearheaded by Black communities, with consideration of socioeconomic factors, cumulative effects of inequity, and adversities throughout the life course.
4.1. Limitations
When comparing results from the two data sources in the study, it is important to consider that NSDUH does not include incarcerated, institutionalized, or unsheltered homeless individuals or active duty military personnel, while mortality data encompass all US resident deaths. NSDUH data are based on self-report, while mortality data are based on death certificate information provided by funeral directors and medical certifiers. The accuracy of demographic information on each death certificate may hinge on the existence of a reliable informant or next-of-kin to provide information to the funeral director, and death certificate data have historically undercounted American Indian/Alaska Native race (Arias et al., 2016). Postmortem toxicology procedures, and the accuracy of drug reporting on death certificates, vary between jurisdictions in the US (Hedegaard et al., 2020). In sensitivity analyses, however, results of decedent demographics and drug involvement were comparable when computed using data from all states and using data limited to states with death reporting classified as excellent, very good, or good (by CDC standards; 38 states and DC; Wilson et al., 2020). Approximately 8% of drug overdoses in 2018 lacked mention of a specific drug (Hedegaard et al., 2020), and some of these “unclassified” drug overdoses may have involved cocaine yet were not included in the present study. Finally, the inclusion of various drug codes on a death certificate does not provide information about the route of drug administration, whether drugs were used simultaneously, and what drugs the individual typically used or believed they were using prior to overdose.
5. Conclusions
The rising cocaine-involved overdose mortality in the US requires a coordinated public health response that extends beyond a focus on opioids and addresses polysubstance use, the unique risk profiles of individuals using cocaine, and underlying social and economic determinants of substance use (Dasgupta et al., 2018). Initiatives centered on preventing cocaine use among youth and adults must be accompanied by efforts related to screening, treatment, and harm reduction for those at elevated risk of a cocaine-involved overdose, with attention to middle-aged and older adults and disadvantaged populations experiencing disparate impact.
Highlights.
The prevalence of past-year cocaine use among US adults was similar in 2002 and 2018, yet rates of cocaine-involved overdose mortality in 2018 were nearly three times as high as in 2002.
While Non-Hispanic Blacks accounted for 11.37% of the adults reporting past-year cocaine use, they represented 27.04% of the adults who died of cocaine-involved overdose.
Half of adults reporting past-year cocaine use also reported past-year use of an opioid, and nearly three of every four cocaine-involved overdose deaths also involved an opioid.
Role of Funding Source
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health [Award Number K01AA026645; Christopher P. Salas-Wright]. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
No conflict declared.
References
- Arias E, Heron MP, Hakes JK, 2016. The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. Vital Health Stat. 2, 1–21. [PubMed] [Google Scholar]
- Armenian P, Whitman JD, Badea A, Johnson W, Drake C, Dhillon SS, Rivera M, Brandehoff N, Lynch KL, 2019. Notes from the field: unintentional fentanyl overdoses among persons who thought they were snorting cocaine — Fresno, California, January 7, 2019. Morb. Mortal. Wkly. Rep 68, 687–688. doi: 10.15585/mmwr.mm6831a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks EG, Reed KD, 2015. Principles and pitfalls: a guide to death certification. Clin. Med. Res 13, 74–82. doi: 10.3121/cmr.2015.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2020. Multiple cause of death 1999–2018. https://wonder.cdc.gov/wonder/help/mcd.html
- Consonni D, Coviello E, Buzzoni C, Mensi C, 2012. A command to calculate age-standardized rates with efficient interval estimation. The Stata Journal 12, 688–701. [Google Scholar]
- Dasgupta N, Beletsky L, Ciccarone D., 2018. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health 108, 182–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Enforcement Administration, 2019a. 2019 Drug Enforcement Administration national drug threat assessment. https://www.dea.gov/sites/default/files/2020-02/DIR-007-20%202019%20National%20Drug%20Threat%20Assessment%20%20low%20res210.pdf
- Drug Enforcement Administration, 2019b. Fentanyl signature profiling program report. https://www.dea.gov/sites/default/files/2019-10/DEA_Fentanyl_Signature_Profiling_Program_Report-Oct-2019.pdf
- Egred M, Davis GK, 2005. Cocaine and the heart. Postgrad. Med. J 81, 568–571. doi: 10.1136/pgmj.2004.028571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fothergill K, Ensminger ME, Doherty EE, Juon HS, Green KM, 2016. Pathways from early childhood adversity to later adult drug use and psychological distress: a prospective study of a cohort of African Americans. J. Health Soc. Behav 57, 223–239. doi: 10.1177/0022146516646808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han BH, Tuazon E, Kunins HV, Mantha S, Paone D, 2019. Unintentional drug overdose deaths involving cocaine among middle-aged and older adults in New York City. Drug Alcohol Depend. 198, 121–125. 10.1016/j.drugalcdep.2019.01.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Warner M, 2020. Drug overdose deaths in the United States, 1999–2018 NCHS Data Brief, no 356. National Center for Health Statistics, Maryland. [Google Scholar]
- Hser YI, Longshore D, Anglin MD, 2007. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval. Rev 31, 515–547. 10.1177/0193841X07307316 [DOI] [PubMed] [Google Scholar]
- Huang B, Grant BF, Dawson DA, Stinson FS, Chou SP, Saha TD, Goldstein RB, Smith SM, Ruan WJ, Pickering RP, 2006. Race-ethnicity and the prevalence and co-occurrence of Diagnostic and Statistical Manual of Mental Disorders, alcohol and drug use disorders and Axis I and II disorders: United States, 2001 to 2002. Compr. Psychiatry 47, 252–257. 10.1016/j.comppsych.2005.11.001 [DOI] [PubMed] [Google Scholar]
- Iguchi MY, Bell J, Ramchand RN, Fain T, 2005. How criminal system racial disparities may translate into health disparities. J. Health Care Poor Underserved 16, 48–56. 10.1353/hpu.2005.0114 [DOI] [PubMed] [Google Scholar]
- Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS, 2018. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science 361, 1–6. doi: 10.1126/science.aau1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John WS, Wu LT, 2017. Trends and correlates of cocaine use and cocaine use disorder in the United States from 2011 to 2015. Drug Alcohol Depend. 180, 376–384. doi: 10.1016/j.drugalcdep.2017.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Baldwin GT, Compton WM, 2017. Recent increases in cocaine-related overdose deaths and the role of opioids. Am. J. Public Health 107, 430–432. doi: 10.2105/AJPH.2016.303627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerridge BT, Chou SP, Pickering RP, Ruan WJ, Huang B, Jung J, Zhang H, Fan AZ, Saha TD, Grant BF, Hasin DS, 2019. Changes in the prevalence and correlates of cocaine use and cocaine use disorder in the United States, 2001–2002 and 2012–2013. Addict. Behav 90, 250–257. doi: 10.1016/j.addbeh.2018.11.005 [DOI] [PubMed] [Google Scholar]
- Khatri UG, Viner K, Perrone J, 2018. Lethal fentanyl and cocaine intoxication. N. Engl. J. Med 379, 1782–1782. doi: 10.1056/NEJMc1809521 [DOI] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN, 2000. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med 19, 335–351. [DOI] [PubMed] [Google Scholar]
- Klein RJ, Schoenborn CA, 2001. Age adjustment using the 2000 projected U.S. population Healthy People statistical notes, no. 20. National Center for Health Statistics, Maryland. [PubMed] [Google Scholar]
- Kloner RA, Hale S, Alker K, Rezkalla S, 1992. The effects of acute and chronic cocaine use on the heart. Circulation 85, 407–419. doi: 10.1016/1053-0770(92)90125-Q [DOI] [PubMed] [Google Scholar]
- LaRue L, Twillman RK, Dawson E, Whitley P, Frasco MA, Huskey A, Guevara MG, 2019. Rate of fentanyl positivity among urine drug test results positive for cocaine or methamphetamine. JAMA Netw. Open 2, e192851–e192851.doi: 10.1001/jamanetworkopen.2019.2851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute, 2019. Joinpoint regression program, version 4.7.0.0. https://surveillance.cancer.gov/help/joinpoint
- Netherland J, Hansen H, 2017. White opioids: pharmaceutical race and the war on drugs that wasn’t. BioSocieties 12, 217–238. doi: 10.1057/biosoc.2015.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan ML, Shamasunder S, Colon-Berezin C, Kunins HV, Paone D, 2019. Increased presence of fentanyl in cocaine-involved fatal overdoses: implications for prevention. J. Urban Health 96, 49–54. doi: 10.1007/s11524-018-00343-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ossiander EM, 2014. Using textual cause-of-death data to study drug poisoning deaths. Am. J. Epidemiol 179, 884–894. doi: 10.1093/aje/kwt333 [DOI] [PubMed] [Google Scholar]
- Palamar JJ, Davies S, Ompad DC, Cleland CM, Weitzman M, 2015. Powder cocaine and crack use in the United States: an examination of risk for arrest and socioeconomic disparities in use. Drug Alcohol Depend. 149, 108–116. doi: 10.1016/j.drugalcdep.2015.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Reingle Gonzalez JM, 2016. Drug Abuse and Antisocial Behavior: a Biosocial Life Course Approach. Palgrave Macmillan, New York. [Google Scholar]
- Saloner B, Cook BL, 2013. Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Aff. 32, 135–145. doi: 10.1377/hlthaff.2011.0983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenker N, Gentleman JF, 2001. On judging the significance of differences by examining the overlap between confidence intervals. American Stat. 55, 182–186. doi: 10.1198/000313001317097960 [DOI] [Google Scholar]
- Shiels MS, Freedman ND, Thomas D, Berrington de Gonzalez A, 2018. Trends in U.S. drug overdose deaths in non-Hispanic black, Hispanic, and non-Hispanic white persons, 2000–2015. Ann. Intern. Med 168, 453–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Maryland. [Google Scholar]
- Wagner KD, Harding RW, Kelley R, Labus B, Verdugo SR, Copulsky E, Bowles JM, Mittal ML, Davidson PJ, 2019. Post-overdose interventions triggered by calling 911: centering the perspectives of people who use drugs (PWUDs). PLoS One 14, e0223823. doi: 10.1371/journal.pone.0223823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N, Kariisa M, Seth P, Smith H, Davis NL, 2020. Drug and opioid-involved overdose deaths—United States, 2017–2018. Morb. Mortal. Wkly. Rep, 69, 290–297. doi: 10.15585/mmwr.mm6911a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, 2011. Illicit and nonmedical drug use among older adults: a review. J. Aging Health 23, 481–504. doi: 10.1177/0898264310386224 [DOI] [PMC free article] [PubMed] [Google Scholar]


