Abstract
Background:
The prevalence of cigarette smoking is more than two times higher among individuals with versus without opioid misuse and/or opioid use disorders (OUD). Overall, smoking cessation has increased over time although it is unknown whether it has similarly increased for those with opioid misuse or OUD. The current study examined cigarette quit ratios from 2002–2018 among US individuals with and without opioid misuse or OUD.
Methods:
Data came from the National Survey on Drug Use and Health, a yearly cross-sectional survey of US civilians 12 years or older. Annual quit ratios (i.e., proportion of former smokers among lifetime-smokers) were estimated from 2002–2018. Logistic regression tested time trends in quit ratios by opioid misuse/OUD.
Results:
Past-month smoking prevalence was much higher for persons with versus without opioid misuse (64.6% versus 25.7%) and OUD (73.3% versus 26.0%). In 2018, quit ratios for individuals with opioid misuse (18.0%) or OUD (10.0%) were less than half of those without opioid misuse (48.3%) or OUD (48.1%). After adjusting for background characteristics, the quit ratio did not change over time among individuals with opioid misuse or OUD in contrast to an increase in quit ratios for those without opioid misuse or OUD. For those without opioid misuse or OUD, males had higher quit ratios than females.
Conclusions:
Cigarette quit ratios remain dramatically lower among those with opioid misuse or OUD. Public health and clinical attention are needed to increase cessation and reduce smoking consequences for individuals with opioid misuse and OUD.
Keywords: quit ratios, tobacco, epidemiology, opioid use disorder, smoking
1. Introduction
Tobacco use remains a critical public health problem in the United States (US) and globally (World Health Organization, 2012). While the prevalence of smoking has decreased over the past several decades (Reitsma et al., 2017), this decline has not been seen equally in all groups. The prevalence of cigarette smoking is more than two times higher among individuals who misuse opioids and/or have an opioid use disorder (OUD) compared to those who do not (Zale et al., 2015). Conversely, individuals who use cigarettes are more likely to use opioids and meet criteria for OUDs (Rajabi et al., 2019) and there are overlaps in the neurobiological brain systems related to nicotine and opiates (Berrendero et al., 2010; Hadjiconstantinou and Neff, 2011; Kishioka et al., 2014). Recently, there has been a dramatic increase in OUD related to opioid misuse and the opioid epidemic (Assistant Secretary of Public Affairs (ASPA), 2017; Dart et al., 2015; Jones, 2017) and concurrent increases in the negative consequences of opioid misuse (e.g., overdose deaths; Rudd et al., 2016).
While smoking cessation has increased over time in the general US population (U.S. Department of Health and Human Services et al., 2020), it remains significantly lower in those who use drugs or have mental illness (Streck et al., 2020; Weinberger et al., 2019). The mortality of smokers with concurrent drug use disorders is more attributable to smoking than other causes (Rogers et al., 2005). Compared to persons with other psychiatric diagnoses, persons with drug use disorders are more likely to smoke (Parker et al., 2019), and of those who attempt smoking cessation, few are successful (Ferron et al., 2011). Based on the strong relationship between cigarette smoking, opioid misuse, and OUDs, reducing the prevalence and negative consequences of smoking through quitting cigarettes has become increasingly important. Existing studies using national data have estimated the prevalence of smoking or quitting among those with a drug use disorder at a single point in time (Smith et al., 2018), but there is still the need to estimate trends in smoking cessation among those with opioid misuse and OUD over the time frame in which opioid related deaths have risen rapidly (Compton et al., 2016).
The current study used cross-sectional waves of national US data to examine trends in quit ratios over time among individuals with and without opioid misuse and OUDs. The first aim was to examine cigarette quit ratios from 2002 to 2018 among individuals with and without opioid misuse and with and without OUD. Given mixed findings on the prevalence of opioid misuse and OUD among males versus females (Grant et al., 2016; John et al., 2019; Parsells et al., 2008; Zale et al., 2015), but clearer findings that males and females differ on a number of cigarette use behavior (e.g., greater difficulty quitting for females versus males (Smith et al., 2016); the second aim was to examine sex differences in the prevalence of cigarette smoking quit ratios by opioid status using the same national data.
2. Methods
2.1. Data Source & Sample
Data came from the National Survey on Drug Use and Health (NSDUH), a yearly cross-sectional survey of US civilians 12 years or older. Datasets for each year from 2002–2018 were concatenated, and a variable was added for the survey year (total analytic sample, n=949,285). For examining smoking prevalence, the combined sample of responses for who had ever smoked was 504,726; in 2018, the analytic sample was n=56,313. Respondents who were 12 years old or older with lifetime and former cigarette smoking (i.e., at least 100 cigarettes) were included in the analyses of quit ratios (2018: n=15,087 lifetime cigarette smokers, n=5,619 former cigarette smokers; 2002 to 2018 combined: n=283,684 lifetime cigarette smokers, n=79,352 former cigarette smokers).
2.2. Measures
2.2.1. Opioid misuse and Opioid Use Disorder
Respondents were classified into two categories based on their past-month opioid misuse. Respondents were considered to have opioid misuse if they used prescription pain relievers extra-medically (Parker and Anthony, 2015) and/or used heroin at least once in the past 30 days. They were not considered opioid misusers if they did not have extra-medical prescription pain reliever use or use heroin in the past month.
Respondents were also classified into two categories based on their past-year OUD, assessed using the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (American Psychiatric Association, 1994). Individuals were classified as having OUD if they meet criteria for opioid abuse or dependence in the past 12 months and as not having OUD if they did not meet criteria for opioid abuse or dependence in the past 12 months. Methodological details can be found in the NSDUH 2016 Codebook (Substance Abuse and Mental Health Services Administration, 2017). Due to survey changes in 2015 surrounding time period and definition of use, two variables [2002–2014 and 2015–2018] were combined to identify both opioid misuse and OUD over the survey years 2002–2018 (see Supplemental Information from Cheng et al., 2019).
2.2.2. Smoking Prevalence and Quit Ratios
Lifetime smokers had smoked at least 100 cigarettes in their lifetime. Former smokers were lifetime smokers who had not smoked cigarettes in the past year. Current smokers met criteria for lifetime smoking and had smoked at least one cigarette in the past 30 days. Daily smokers had smoked 30 days in the past month. The quit ratio was calculated as the proportion of former smokers among the full sample of lifetime smokers consistent with other research (e.g., Weinberger et al., 2019). This measure was estimated separately for those with and without opioid misuse and those with and without OUD.
2.2.3. Background Characteristics
Age (12–17 years, 18–25 years, 26–34 years, 35+ years), sex (male/female), race/ethnicity (Non-Hispanic (NH) White, NH Black, Hispanic, Other [NH Native American/Alaskan Native, NH Hawaiian/Pacific Islander, NH Asian, NH more than one race), and annual income (<$20,000, $20,000–$49,999, $50,000–$74,999, ≥$75,000) were included in analyses as covariates.
Past-month alcohol and cannabis use, alcohol use disorder, and cannabis use disorder were additional covariates. Past-month alcohol and cannabis misuse and alcohol use disorder/cannabis use disorder were defined similar to opioid misuse and opioid use disorder, respectively. These substances were included as covariates due to strong associations with opioid misuse and OUD with lower cigarette quit ratios (Weinberger et al., 2019).
2.3. Statistical Analyses
First, past-month smoking was estimated for the most recent data year, 2018, by opioid status (i.e., past-month misuse, OUD). For smoking quit ratios, the prevalence of former smoking was estimated each year from 2002 to 2018. Logistic regression tested linear time trends in quit ratios by opioid misuse/OUD by using year as a continuous predictor (Weinberger et al., 2019). Stratified models were run by sex for both opioid misuse and OUD. First, unadjusted models were run followed by models with a priori covariates: year, age, sex, race/ethnicity, income, alcohol use, cannabis use, alcohol use disorder, and cannabis use disorder. Next, the adjusted stratified models examined differences in quit ratios by sex while adjusting for all other background characteristics. Last, models that included two-way interaction terms of year by opioid misuse/OUD were estimated to explore differential time trends in quit ratios by opioid status over the study time period.
Analyses were completed using Stata Version 14 (Stata Corp, 2015), which accounts for NSDUH sampling weights and complex clustered sampling. It also produces accurate standard errors using Taylor series estimation. Survey weights were divided by the number of years to provide nationally representative estimates.
3. Results
For 2018, past-month prevalences of smoking and daily smoking were much higher for persons with, compared to without, opioid misuse (smoking: 64.6% versus 25.7%; daily smoking: 34.9% versus 12.8%) or OUD (smoking: 73.3% versus 26.0%; daily smoking: 43.6% versus 13.0%). In the same year, quit ratios for individuals with opioid misuse (18.0%) or OUD (10.0%) were less than half the quit ratios of those without opioid misuse (48.2%) or OUD (48.1%). The relative difference in quit ratios between those with and without opioid misuse and OUD remained consistent across all years (See Supplemental Table 1).
After adjusting for background characteristics including other drug use/drug use disorders, the quit ratio did not change over time among individuals with opioid misuse (Figure 1) or OUD (Figure 2). In contrast, there was an increase in quit ratios for those without opioid misuse or OUD (p <0.05; see Figures 1 and 2). For all years, females without opioid misuse or OUD were less likely to be former smokers than males. There were no differences in quit ratios by sex for individuals with opioid misuse/OUD (see Supplemental Table 2).
Figure 1.
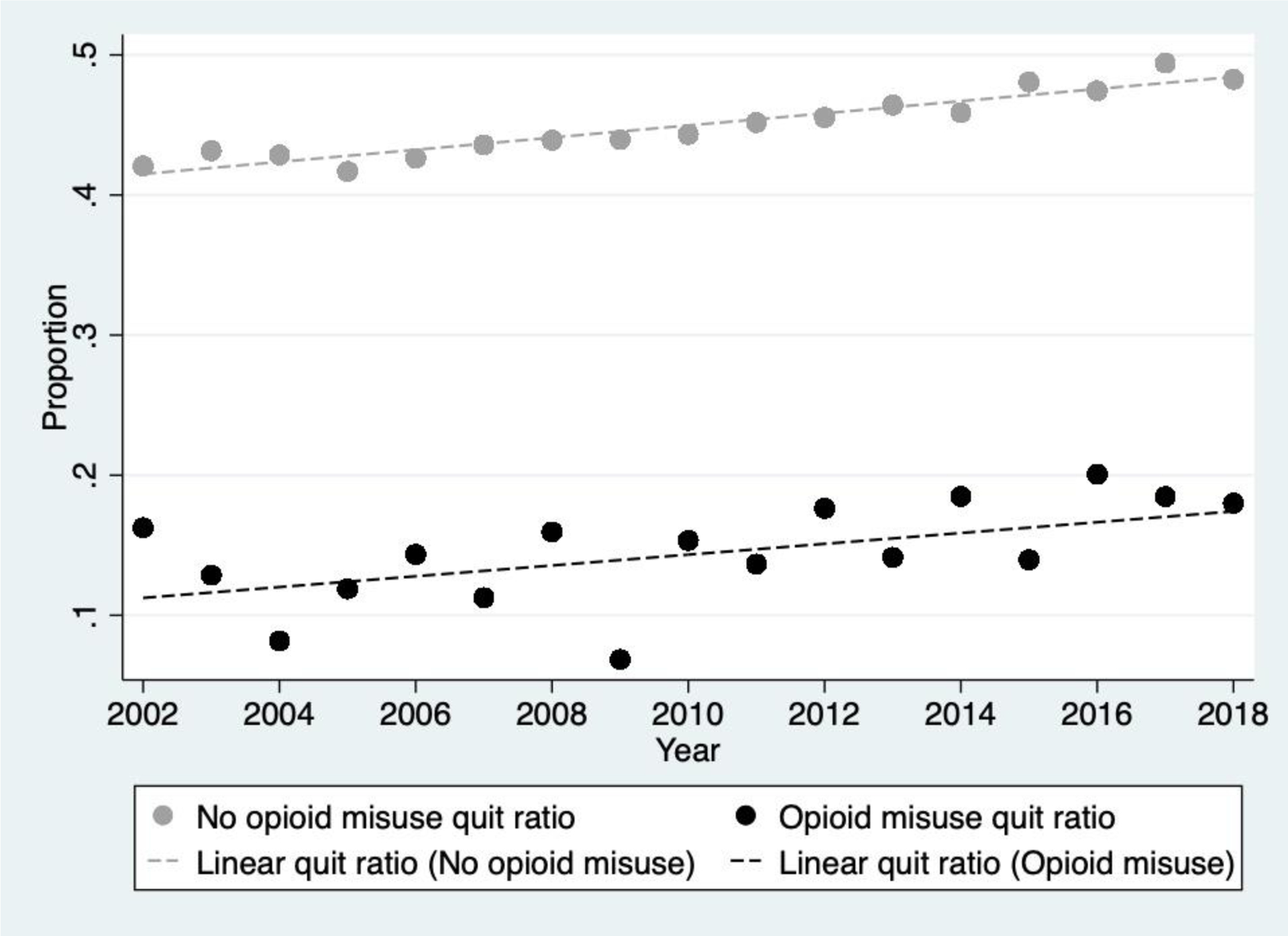
Smoking quit ratios for individuals with and without past-month opioid misuse. Data from the National Surveys on Drug Use and Health, 2002–2018.
Figure 2.
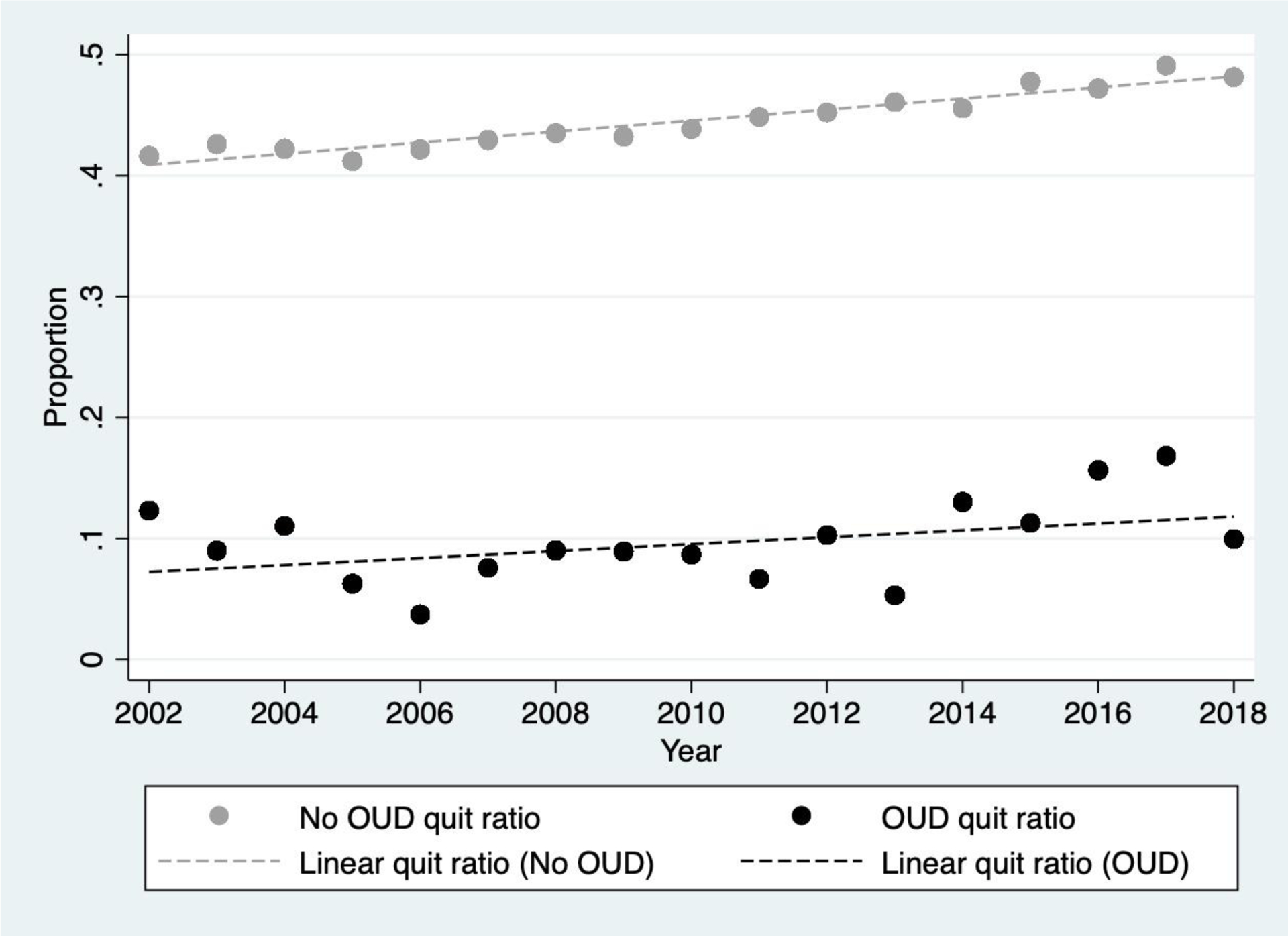
Smoking quit ratios for individuals with and without opioid use disorder (OUD). Data from the National Surveys on Drug Use and Health, 2002–2018.
4. Discussion
Using nationally representative data of US individuals age 12 and older, we found that cigarette quit ratios remained dramatically lower among individuals with opioid misuse or OUD compared to those without opioid misuse or OUD from 2002–2018. In addition, quit ratios increased from 2002–2018 for persons without opioid misuse or OUD, but did not change for those with opioid misuse or OUD. These findings were consistent with those related to cannabis use and cannabis use disorder using a similar approach (Weinberger et al., 2019). In addition, for individuals with no opioid misuse or OUD, quit ratios were higher for males over time. This is in contrast to a sample of primary care patients who smoke where opioid misuse and OUD was overrepresented among males and the unemployed (John et al., 2019).
Importantly, in 2018, past-month smoking prevalence and daily smoking prevalence persons with versus with opioid misuse or OUD remained more than double for persons without opioid misuse or OUD. Our findings demonstrate that cigarette smoking has persisted among persons with either opioid misuse or OUD, which contrasts with declines in smoking seen in the general US population (U.S. Department of Health and Human Services et al., 2020). It may be that those with a history of opioid misuse or OUD have a more difficult time quitting due to more severe nicotine/tobacco dependence (Parker et al., 2018) and/or more severe tobacco withdrawal (Streck et al., 2018). Developing a better understanding of which FDA-approved smoking treatments work best for individuals with opioid misuse and OUD would be useful due to the small number of treatment studies among this group of smokers. For example, individuals with OUD and individuals receiving methadone-maintenance treatment for OUD may have greater success with transdermal nicotine patches than with varenicline or bupropion (Martin et al., 2019; Yee et al., 2018) potentially due to greater adherence to transdermal nicotine patches than varenicline (Martin et al., 2019). In addition, testing novel smoking treatments for this vulnerable population may aid in increasing the quit ratio. For example, electronic cigarettes have been effective in pilot studies for reducing cigarettes per day among opioid dependent smokers (Felicione et al., 2019).
Several study strengths are worth noting including the generalizability of findings to the US population 12 years or older and the ability to examine quit ratios over time by opioid status. With regard to limitations, both cigarette use and opioid misuse were self-reported measures and opioid variables were subject to methodological changes during the study period. Still, we did not find inconsistencies in opioid misuse/OUD estimates prior to versus after 2015. Also, there was some overlap among opioid misusers and persons with OUD, but chose these two categories to facilitate comparisons with other studies that have a similar approach (e.g., Weinberger et al., 2019). In addition, focus was solely on cigarette use and not other tobacco products. Former smokers were defined as not smoking in the past year as the survey does not provide more granularity. The data were cross-sectional samples and we could not follow trajectories of opioid or cigarette use longitudinally for individual respondents.
This study reports two-fold to three-fold lower quit ratios in people with opioid misuse or OUD compared to those without opioid misuse or OUD and the stability of this difference over time. Disparities in quit ratios for persons with and without opioid misuse or OUD highlight the need for public health and clinical efforts to increase cessation and reduce smoking-related consequences in these subgroups. Building on these findings, next steps should be to explore variables related to cessation (e.g., tobacco use disorder), time to cessation, treatment efficacy, patterns of smoking (e.g., topography), and longitudinal trajectories for persons based on their opioid status and experience with substance use treatment.
Supplementary Material
HIGHLIGHTS.
We examined smoking quit ratios by opioid misuse and opioid use disorder (OUD).
Smoking prevalence was higher for persons with OUD and opioid misuse vs. without.
Smoking quit ratios were lower for persons with OUD and opioid misuse vs. without.
Quit ratios increased for persons without opioid misuse or OUD over time.
Quit ratios did not change for those with opioid misuse or OUD over time.
Role of Funding Source
ACV was supported by the Tobacco Centers of Regulatory Science (TCORS) award from the National Institute on Drug Abuse and Food and Drug Administration (FDA) [U54DA036114], and the National Institute of General Medical Sciences (NIGMS) of the NIH [P20GM103644]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, FDA, or the US Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared.
References
- American Psychiatric Association, 1994. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, 4th edition ed. American Psychiatric Association, Washington, DC. [Google Scholar]
- Assistant Secretary of Public Affairs (ASPA), 2017. What is the U.S. Opioid Epidemic? [WWW Document]. HHS.gov. URL https://www.hhs.gov/opioids/about-the-epidemic/index.html (accessed 4.27.20). [Google Scholar]
- Berrendero F, Robledo P, Trigo JM, Martín-García E, Maldonado R, 2010. Neurobiological mechanisms involved in nicotine dependence and reward: Participation of the endogenous opioid system. Neurosci. Biobehav. Rev., Novel Perspectives on Drug Addiction and Reward 35, 220–231. 10.1016/j.neubiorev.2010.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng HG, Parker MA, Anthony JC, 2019. Female-male differences in prescription pain reliever dependence levels: Evidence on newly incident adolescent and young adult users in the United States, 2002–2014. Drug Alcohol Depend. 204, 107466 10.1016/j.drugalcdep.2019.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT, 2016. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. N. Engl. J. Med 374, 154–163. 10.1056/NEJMra1508490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, Green JL, 2015. Trends in Opioid Analgesic Abuse and Mortality in the United States. N. Engl. J. Med 372, 241–248. 10.1056/NEJMsa1406143 [DOI] [PubMed] [Google Scholar]
- Felicione NJ, Enlow P, Elswick D, Long D, Sullivan CR, Blank MD, 2019. A pilot investigation of the effect of electronic cigarettes on smoking behavior among opioid-dependent smokers. Addict. Behav., E-cigarettes and Non-combustible Tobacco Products 91, 45–50. 10.1016/j.addbeh.2018.07.003 [DOI] [PubMed] [Google Scholar]
- Ferron JC, Brunette MF, He X, Xie H, McHugo GJ, Drake RE, 2011. Course of Smoking and Quit Attempts Among Clients With Co-occurring Severe Mental Illness and Substance Use Disorders. Psychiatr. Serv 62, 353–359. 10.1176/ps.62.4.pss6204_0353 [DOI] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, Zhang H, Smith SM, Pickering RP, Huang B, Hasin DS, 2016. Epidemiology of DSM-5 Drug Use Disorder. JAMA Psychiatry 73, 39–47. 10.1001/jamapsychiatry.2015.2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjiconstantinou M, Neff NH, 2011. Nicotine and endogenous opioids: Neurochemical and pharmacological evidence. Neuropharmacology, Trends in Neuropharmacology: In Memory of Erminio Costa 60, 1209–1220. 10.1016/j.neuropharm.2010.11.010 [DOI] [PubMed] [Google Scholar]
- John WS, Zhu H, Mannelli P, Subramaniam GA, Schwartz RP, McNeely J, Wu L-T, 2019. Prevalence and patterns of opioid misuse and opioid use disorder among primary care patients who use tobacco. Drug Alcohol Depend. 194, 468–475. 10.1016/j.drugalcdep.2018.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, 2017. The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence — An assessment of demographic and substance use trends, United States, 2003–2014. Addict. Behav 65, 229–235. 10.1016/j.addbeh.2016.08.027 [DOI] [PubMed] [Google Scholar]
- Kishioka S, Kiguchi N, Kobayashi Y, Saika F, 2014. Nicotine Effects and the Endogenous Opioid System. J. Pharmacol. Sci 125, 117–124. 10.1254/jphs.14R03CP [DOI] [PubMed] [Google Scholar]
- Martin RA, Rohsenow DJ, Tidey JW, 2019. Smokers with opioid use disorder may have worse drug use outcomes after varenicline than nicotine replacement. J. Subst. Abuse Treat 104, 22–27. 10.1016/j.jsat.2019.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Anthony JC, 2015. Epidemiological evidence on extra-medical use of prescription pain relievers: transitions from newly incident use to dependence among 12–21 year olds in the United States using meta-analysis, 2002–13. PeerJ 3 10.7717/peerj.1340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Sigmon SC, Villanti AC, 2019. Higher smoking prevalence among United States adults with co-occurring affective and drug use diagnoses. Addict Behav. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Streck JM, Sigmon SC, 2018. Associations between opioid and nicotine dependence in nationally representative samples of United States adult daily smokers. Drug Alcohol Depend. 186, 167–170. 10.1016/j.drugalcdep.2018.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsells K, Cook S, Kaufman D, Anderson T, Rosenberg L, Mitchell A, 2008. Prevalence and characteristics of opioid use in the US adult population. Pain 138, 507–513. 10.1016/j.pain.2008.01.027 [DOI] [PubMed] [Google Scholar]
- Rajabi A, Dehghani M, Shojaei A, Farjam M, Motevalian SA, 2019. Association between tobacco smoking and opioid use: A meta-analysis. Addict. Behav 92, 225–235. 10.1016/j.addbeh.2018.11.043 [DOI] [PubMed] [Google Scholar]
- Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH, Abbafati C, Abera SF, Abraham B, Abyu GY, Adebiyi AO, Al-Aly Z, Aleman AV, Ali R, Al Alkerwi A, Allebeck P, Al-Raddadi RM, Amare AT, Amberbir A, Ammar W, Amrock SM, Antonio CAT, Asayesh H, Atnafu NT, Azzopardi P, Banerjee A, Barac A, Barrientos-Gutierrez T, Basto-Abreu AC, Bazargan-Hejazi S, Bedi N, Bell B, Bello AK, Bensenor IM, Beyene AS, Bhala N, Biryukov S, Bolt K, Brenner H, Butt Z, Cavalleri F, Cercy K, Chen H, Christopher DJ, Ciobanu LG, Colistro V, Colomar M, Cornaby L, Dai X, Damtew SA, Dandona L, Dandona R, Dansereau E, Davletov K, Dayama A, Degfie TT, Deribew A, Dharmaratne SD, Dimtsu BD, Doyle KE, Endries AY, Ermakov SP, Estep K, Faraon EJA, Farzadfar F, Feigin VL, Feigl AB, Fischer F, Friedman J, G/hiwot TT, Gall SL, Gao W, Gillum RF, Gold AL, Gopalani SV, Gotay CC, Gupta Rahul, Gupta Rajeev, Gupta V, Hamadeh RR, Hankey G, Harb HL, Hay SI, Horino M, Horita N, Hosgood HD, Husseini A, Ileanu BV, Islami F, Jiang G, Jiang Y, Jonas JB, Kabir Z, Kamal R, Kasaeian A, Kesavachandran CN, Khader YS, Khalil I, Khang Y-H, Khera S, Khubchandani J, Kim D, Kim YJ, Kimokoti RW, Kinfu Y, Knibbs LD, Kokubo Y, Kolte D, Kopec J, Kosen S, Kotsakis GA, Koul PA, Koyanagi A, Krohn KJ, Krueger H, Defo BK, Bicer BK, Kulkarni C, Kumar GA, Leasher JL, Lee A, Leinsalu M, Li T, Linn S, Liu P, Liu S, Lo L-T, Lopez AD, Ma S, El Razek HMA, Majeed A, Malekzadeh R, Malta DC, Manamo WA, Martinez-Raga J, Mekonnen AB, Mendoza W, Miller TR, Mohammad KA, Morawska L, Musa KI, Nagel G, Neupane SP, Nguyen Q, Nguyen G, Oh I-H, Oyekale AS, Pa M, Pana A, Park E-K, Patil ST, Patton GC, Pedro J, Qorbani M, Rafay A, Rahman M, Rai RK, Ram U, Ranabhat CL, Refaat AH, Reinig N, Roba HS, Rodriguez A, Roman Y, Roth G, Roy A, Sagar R, Salomon JA, Sanabria J, de Souza Santos I, Sartorius B, Satpathy M, Sawhney M, Sawyer S, Saylan M, Schaub MP, Schluger N, Schutte AE, Sepanlou SG, Serdar B, Shaikh MA, She J, Shin M-J, Shiri R, Shishani K, Shiue I, Sigfusdottir ID, Silverberg JI, Singh J, Singh V, Slepak EL, Soneji S, Soriano JB, Soshnikov S, Sreeramareddy CT, Stein DJ, Stranges S, Subart ML, Swaminathan S, Szoeke CEI, Tefera WM, Topor-Madry R, Tran B, Tsilimparis N, Tymeson H, Ukwaja KN, Updike R, Uthman OA, Violante FS, Vladimirov SK, Vlassov V, Vollset SE, Vos T, Weiderpass E, Wen C-P, Werdecker A, Wilson S, Wubshet M, Xiao L, Yakob B, Yano Y, Ye P, Yonemoto N, Yoon S-J, Younis MZ, Yu C, Zaidi Z, El Sayed Zaki M, Zhang AL, Zipkin B, Murray CJL, Forouzanfar MH, Gakidou E, 2017. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. The Lancet 389, 1885–1906. 10.1016/S0140-6736(17)30819-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RG, Hummer RA, Krueger PM, Pampel FC, 2005. Mortality attributable to cigarette smoking in the United States. Popul. Dev. Rev 31, 259–292. 10.1111/j.1728-4457.2005.00065.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM, 2016. Increases in Drug and Opioid Overdose Deaths - United States, 2000–2014. MMWR Morb. Mortal. Wkly. Rep 64, 1378–1382. 10.15585/mmwr.mm6450a3 [DOI] [PubMed] [Google Scholar]
- Smith PH, Bessette AJ, Weinberger AH, Sheffer CE, McKee SA, 2016. Sex/gender differences in smoking cessation: A review. Prev. Med., Special Issue: behavior change, health, and health disparities 2016 92, 135–140. 10.1016/j.ypmed.2016.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PH, Chhipa M, Bystrik J, Roy J, Goodwin RD, Sherry A McKee, 2018. Cigarette smoking among those with mental disorders in the US population: 2012–2013 update. Tob. Control tobaccocontrol-2018–054268. 10.1136/tobaccocontrol-2018-054268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corp Stata, 2015. Stata Statistical Software: Release 14. Stata Corp LP, College Station, TX. [Google Scholar]
- Streck JM, Heil SH, Higgins ST, Bunn JY, Sigmon SC, 2018. Tobacco withdrawal among opioid-dependent smokers. Exp Clin Psychopharmacol 26, 119–124. 10.1037/pha0000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streck JM, Weinberger AH, Pacek LR, Gbedemah M, Goodwin RD, 2020. Cigarette Smoking Quit Rates Among Persons With Serious Psychological Distress in the United States From 2008 to 2016: Are Mental Health Disparities in Cigarette Use Increasing? Nicotine Tob. Res 22, 130–134. 10.1093/ntr/nty227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2017. National Survey on Drug Use and Health 2016 (NSDUH-2016-DS0001). SAMHDA, Rockville, MD. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health, Office on Smoking and Health, 2020. Smoking Cessation: A Report of the Surgeon General - Executive Summary. Atlanta, GA. [Google Scholar]
- Weinberger AH, Pacek LR, Wall MM, Gbedemah M, Lee J, Goodwin RD, 2019. Cigarette smoking quit ratios among adults in the USA with cannabis use and cannabis use disorders, 2002–2016. Tob. Control 10.1136/tobaccocontrol-2018-054590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2012. Mortality Attributable to Tobacco, WHO Global Report. WHO Press, Geneva, Switzerland. [Google Scholar]
- Yee A, Hoong MC, Joyce YC, Loh HS, 2018. Smoking Cessation Among Methadone-Maintained Patients: A Meta-Analysis. Subst. Use Misuse 53, 276–285. [DOI] [PubMed] [Google Scholar]
- Zale EL, Dorfman ML, Hooten WM, Warner DO, Zvolensky MJ, Ditre JW, 2015. Tobacco smoking, nicotine dependence, and patterns of prescription opioid misuse: Results from a nationally representative sample. Nicotine Tob. Res 17, 1096–1103. 10.1093/ntr/ntu227 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


