Structured Abstract
Objectives
(1) To compare the prevalence of antenatal admissions and mean length of stay among women with opioid-affected and non-opioid-affected deliveries; (2) examine predictors of admission; and (3) describe the most common discharge diagnoses in each group.
Methods
Using data from seven states in the State Inpatient Databases for varying years between 2009 and 2014, delivery hospitalizations among women >18 years old were identified and classified as opioid-affected or non-opioid-affected. Antenatal admissions were linked to deliveries. The antenatal admission ratio and mean length of stay for each group were calculated; the percentage of deliveries in each group with no, any, one, two, or three or more antenatal admissions were compared with t-tests. Logistic regression models estimated odds of any antenatal admission, stratified by opioid-affected and non-opioid-affected deliveries. Frequencies were tabulated for the ten most common discharge diagnoses in each group.
Results
Of 2,684,970 deliveries, 14,765 were opioid-affected. Admissions among women with opioid-affected deliveries were more prevalent (26.4 per 100 deliveries) compared to 6.7 among women with non-opioid-affected deliveries and were associated with a 1.5-day longer mean length of stay. The presence of a behavioral health condition was associated with higher odds of antenatal admission in both groups, with a particularly strong association among women with opioid-affected deliveries. Six of the ten most common diagnoses for admissions prior to opioid-affected deliveries were behavioral health-related.
Conclusions for Practice
These results highlight the importance of addressing the large burden of behavioral health conditions among pregnant women, especially those with opioid dependence and abuse.
Keywords: Antenatal admission, Behavioral health, Mental health, Opioid use disorder, Substance use disorder
Introduction
Antenatal admission, or an inpatient hospital stay during pregnancy, may be a marker of a high-risk pregnancy and a signal for maternal morbidity.(Bacak, Callaghan, Dietz, & Crouse, 2005; Martin et al., 2016) Recent attention to increasing maternal mortality rates in the United States has led to efforts to better identify and address underlying causes of this trend.(Molina & Pace, 2017) A 2018 report(Moniz, Spector-Bagdady, Heisler, & Harris, 2017) from nine maternal mortality review committees concluded that behavioral health conditions, including substance use disorders, were a leading cause of pregnancy-related deaths, accounting for 7% of deaths among non-Hispanic white women, and were a contributing factor to many more.
Opioid use in pregnancy is a growing public health challenge. Rates of opioid use disorder (OUD) diagnosis at the time of delivery more than quadrupled in the United States from 1999 to 2014,(Haight SC, 2018) and the incidence of neonatal opioid withdrawal syndrome (NOWS) due to prenatal opioid exposure increased nearly seven-fold over the same period.(Patrick et al., 2012; Winkelman, Villapiano, Kozhimannil, Davis, & Patrick, 2018) Women with OUD are a vulnerable population, with significantly increased risk of pregnancy-related death and adverse obstetrical outcomes.(Maeda, Bateman, Clancy, Creanga, & Leffert, 2014) A better understanding of the patterns of antenatal admission among women with opioid-affected deliveries (OADs) more generally could offer opportunities for improved patient education; more targeted resources and support; and improved screening and care delivery across the care continuum for pregnant women who may not consistently interface with the healthcare system. Importantly, modifiable factors could be identified and intervened upon to prevent antenatal admissions and adverse maternal and infant outcomes. Little is known about antenatal admissions among women with OAD and how they compare to antenatal admissions among women with non-OAD.
To address this gap in the literature, we (1) compare the prevalence of non-delivery antenatal admissions and mean length of stay per admission among women with OAD and non-OAD; (2) examine sociodemographic and clinical predictors of antenatal admission; and (3) describe the most common discharge diagnoses for antenatal admissions among women with OAD compared to non-OAD. We hypothesized that antenatal admissions among women with OADs would be more prevalent than among women with non-OADs, would have longer lengths of stay, and would be associated with the presence of co-occurring behavioral health conditions.
Methods
Study Design and Data Source
This retrospective, population-based cross-sectional study of antenatal admissions of women in seven states used data from the State Inpatient Databases (SID) of the Healthcare Cost and Utilization Project (HCUP), compiled by the Agency for Healthcare research and Quality. The SID contains the universe of inpatient discharge records from hospitals in participating states and includes all patients, regardless of payer. A convenience sample of states and years were selected for the presence of verified patient-level identifiers that permit linkage of multiple admissions over time and across hospitals for the same patient: Florida (2009–2014), Iowa (2013–2014), Maryland (2013–2014), Massachusetts (2010–2014), Nebraska (2012–2014), New York (2009–2014), Utah (2012–2014). The study was approved by the corresponding author’s Institutional Review Board.
Identification of Sample
Delivery hospitalizations for women 18 years of age and older (n=3,376,671) were identified using a previously developed algorithm.(Kuklina et al., 2008) The 6% of deliveries missing the longitudinal patient-level identifier were excluded from analysis (n=204,656). To allow for an adequate period in which to observe antenatal admissions, delivery hospitalizations in the first three quarters of the first year of each state’s data were excluded (n=487,045). As the SID is at the discharge rather than patient level, individuals with multiple deliveries during the study period are included more than once in the study sample.
Outcome
The primary outcome of interest was antenatal admission. Consistent with Martin et al.,(Martin et al., 2016) we defined antenatal admissions as those with an admission date within 260 days (37 weeks of gestation) and >4 days before the admission date of the delivery hospitalization, allowing us to capture the majority of antenatal admissions, exclude pre-pregnancy admissions, and exclude prolonged hospitalizations near the end of pregnancy that resulted in delivery. We defined an admission as having a length of stay greater than or equal to 24 hours. We calculated the number of antenatal admissions (none, any, one, two, and three or more) per delivery and the mean length of stay for each antenatal admission.
Predictors
The main predictor of interest was whether or not a delivery was affected by opioids. Applying a definition of opioid-related hospital admissions used by the Centers for Disease Control and Prevention,(Haight SC, 2018) the sample was stratified into two groups: opioid-affected deliveries (OAD), which included any of the following International Classification of Disease, 9th Clinical Modification (ICD-9-CM) diagnosis codes: 304.00–304.03, 304.70–304.73, 305.50–305.53, and non-opioid-affected deliveries.
To examine other potential predictors of antenatal admission from the literature, (Bacak et al., 2005; Gazmararian et al., 2002; Martin et al., 2016) we identified maternal race/ethnicity, age at time of delivery (categorized as 18–34 years and >=35 years) and primary payer for the delivery hospitalization (categorized as public coverage, which included Medicaid and Medicare; commercial insurance; and uninsured/self-pay). For other predictors hypothesized to have a relationship with the primary outcome, we identified deliveries resulting in multiple births (“multiple gestation”) and preterm deliveries and created indicators for co-occurring behavioral and physical health conditions appearing in any of 15 diagnosis fields on the discharge record for the delivery hospitalization or any antenatal admission (see Appendix A). Behavioral health conditions were defined as mental health conditions and non-opioid-related substance dependence or abuse. Physical health conditions are common chronic conditions not directly associated with pregnancy, including chronic respiratory disease, chronic hypertension, pre-existing diabetes, chronic heart disease, chronic renal disease, chronic liver disease, and human immunodeficiency virus (HIV).(Admon et al., 2017)
Analysis
Frequencies and percentages describe the demographic and clinical characteristics of the study sample. Descriptive statistics are reported for OAD and non-OAD, and we compared the distribution of each variable using chi-square tests. We calculated the number of antenatal admissions per 100 deliveries for women with OAD versus non-OAD and compared the percentage of deliveries in each group with no, any, one, two, or three or more antenatal admissions with t-tests. We calculated the mean length of stay for antenatal admissions for women with OAD compared to non-OAD.
Next, we used logistic regression models to estimate the odds of having any antenatal admission, stratified to examine the OAD and non-OAD samples separately and adjusting for the sociodemographic and clinical covariates shown in Table 1. Models were adjusted for age, race, primary payer, multiple gestation, preterm delivery, the presence of a behavioral health condition, and the presence of a chronic physical health condition. As a secondary analysis, we also modeled the odds of multiple (two or more) antenatal admissions for each group. All models included state and year fixed effects and accounted for clustering at the woman level when determining variance estimates, given the possibility of multiple deliveries for the same individual during the study period. A significance level of 0.05 was used.
Table 1.
Characteristics of the sample: all deliveries, opioid-affected deliveries, and non-opioid-affected deliveries
| All deliveries N (%) N=2,684,970 | OADs N (%) N=14,765 | Non-OADs N (%) N=2,670,205 | P-valuea | |
|---|---|---|---|---|
| Age | <0.001 | |||
| 18–34 | 2,189,895 (81.6) | 13,258 (89.8) | 2,176,637 (81.5) | |
| >=35 | 495,075 (18.4) | 1,507 (10.2) | 493,568 (18.5) | |
| Race/ethnicityb | <0.001 | |||
| White, non-Hispanic | 1,292,063 (50.9) | 12,318 (86.1) | 1,279,745 (50.7) | |
| Black, non-Hispanic | 451,821 (17.8) | 689 (4.8) | 451,132 (17.9) | |
| Hispanic | 457,340 (18.0) | 830 (5.8) | 456,510 (18.1) | |
| Other | 334,902 (13.2) | 474 (3.3) | 334,428 (13.3) | |
| Primary Payerc | <0.001 | |||
| Public coverage | 1,218,566 (45.4) | 12,152 (82.3) | 1,206,414 (45.2) | |
| Commercially insured | 1,346,605 (50.2) | 1,911 (12.9) | 1,344,694 (50.4) | |
| Uninsured/self-pay | 119,757 (4.5) | 700 (4.7) | 119,057 (4.5) | |
| Multiple gestation | 55,482 (2.1) | 205 (1.4) | 55,277 (2.1) | <0.001 |
| Preterm delivery | 177,126 (6.6) | 2,154 (14.6) | 174,972 (6.6) | <0.001 |
| Behavioral health condition present | 101,596 (3.8) | 4,975 (33.7) | 96,621 (3.6) | <0.001 |
| Anxiety disorders | 24,301 (0.9) | 579 (3.9) | 23,722 (0.9) | |
| Mood disorders | 48,922 (1.8) | 1,336 (9.0) | 47,586 (1.8) | |
| Personality disorders | 861 (0.0) | 53 (0.4) | 808 (0.0) | |
| Schizophrenia/psychotic disorders | 2,367 (0.1) | 41 (0.3) | 2,326 (0.1) | |
| Substance dependence or abused | 38,576 (1.4) | 3,966 (26.9) | 34,610 (1.3) | |
| Physical health condition present | 218,039 (8.1) | 2,068 (14.0) | 215,971 (8.1) | <0.001 |
| Chronic respiratory disease | 118,426 (4.4) | 1,457 (9.9) | 116,969 (4.4) | |
| Chronic Hypertension | 64,338 (2.4) | 423 (2.9) | 63,915 (2.4) | |
| Pre-existing diabetes | 26,341 (1.0) | 125 (0.8) | 26,216 (1.0) | |
| Chronic heart disease | 12,081 (0.4) | 100 (0.7) | 11,981 (0.4) | |
| Chronic renal disease | 11,731 (0.4) | 108 (0.7) | 11,623 (0.4) | |
| Chronic liver disease | 1,171 (0.0) | 20 (0.1) | 1,151 (0.0) | |
| HIV | 3,172 (0.1) | 52 (0.4) | 3,120 (0.1) |
P-values obtained from chi-square tests comparing the distribution of each variable between OADs and non-OADs.
Race was missing in 3% of OADs and 5.5% of non-OADs.
Primary payer was missing in 0.01% of OADs and <0.01% of non-OADs.
This variable includes alcohol, cocaine, cannabis, sedative-hypnotics, anxiolytics, hallucinogens, amphetamines and other psychostimulants, and “other” substances not otherwise classified. It excludes opioid-related diagnoses.
Abbreviations: OADs, opioid-affected deliveries; HIV, human immunodeficiency virus
Lastly, we tabulated frequencies of the ten most common discharge diagnoses in any diagnosis field for antenatal admissions prior to OADs and non-OADs. Analyses were conducted using STATA v14.2 (StataCorp LP, College Station, TX).
Results
Descriptive Results
There were 2,684,970 deliveries in the sample, of which 14,765 were OADs. The majority of deliveries were to women 18–34 years old (81.6%), white, non-Hispanic (50.9%), and commercially insured (50.2%) (Table 1). Multiple gestations accounted for 2.1% of deliveries, 6.6% of deliveries were preterm, behavioral health conditions were present in 3.8% of all deliveries, and chronic physical health conditions were present in 8.1%. Compared to non-OADs, woman with OADs were significantly more likely to be age 18–34 years old (89.8% versus 81.5%); white, non-Hispanic (86.1% versus 50.7%); and have public coverage (82.3% versus 45.2%); to have a preterm delivery (14.6% versus 6.6%); a behavioral health condition (33.7% versus 3.6%); or a physical health condition (14.0% versus 8.1%), P<0.001 for all comparisons. Multiple gestations occurred in 1.4% of OADs and 2.1% of non-OADs.
There were 26.4 antenatal admissions per 100 deliveries among women with OADs compared to 6.7 among women with non-OADs. The range of total antenatal admissions was similar: 0 to 19 for OADs and 0 to 21 for non-OADs. Figure 1 shows the proportion of OADs and non-OADs with any antenatal admission (17% versus 5%), one admission (12% versus 4%), two admissions (3% versus 0.7%), and three or more (2% versus 0.2%), P<0.001 for all comparisons. Mean length of stay for antenatal admissions prior to OADs was 4.9 days compared to 3.5 days for those prior to non-OADs.
Figure 1. Percent of opioid-affected deliveries and non-opioid-affected deliveries with any, 1, 2, or 3 or more antenatal admissions*.
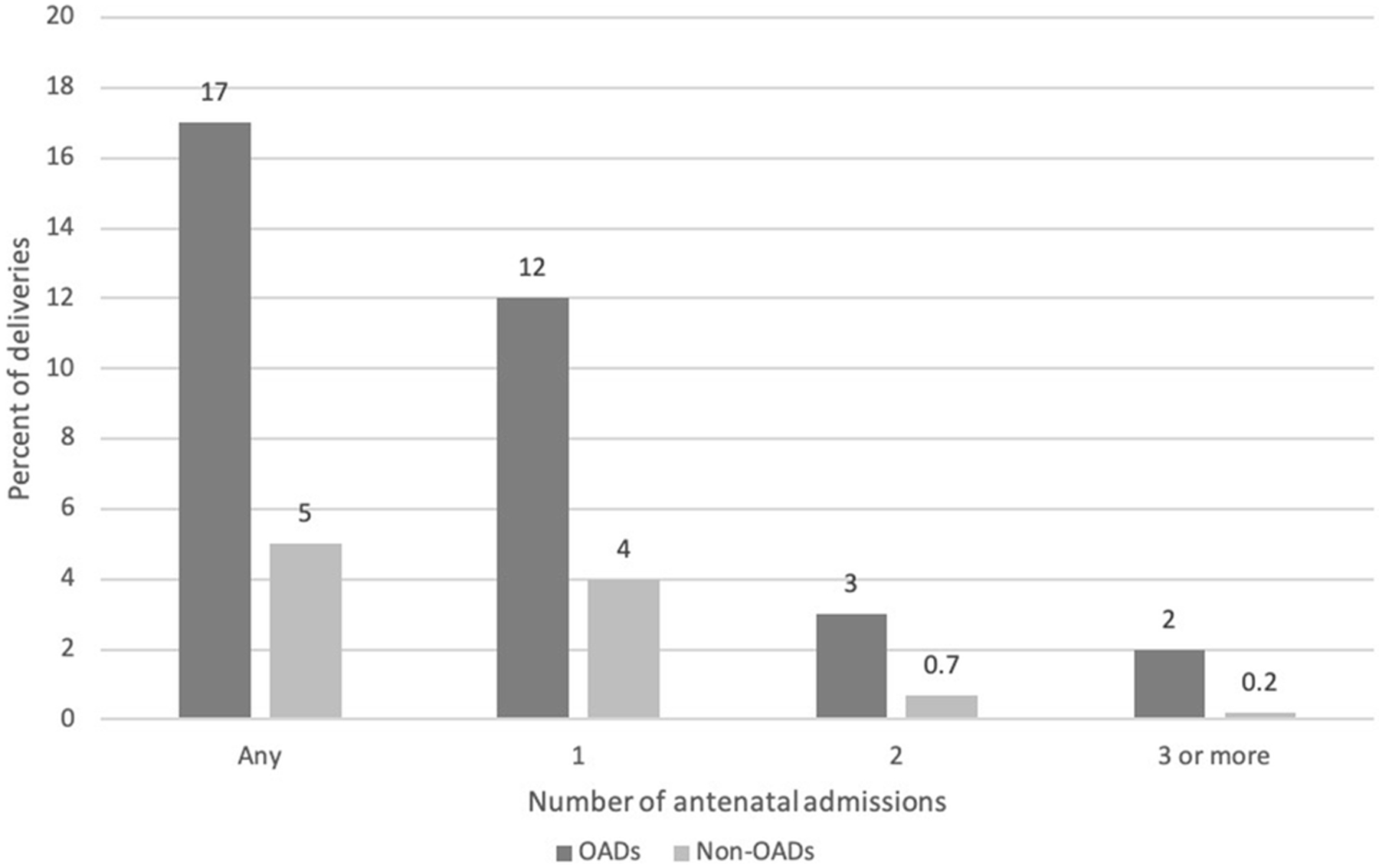
* T-tests comparing proportions of deliveries among OADs versus non-OADs with any, 1, 2, and 3 or more antenatal admissions yielded P-values of <0.001 for each comparison.
Abbreviations: OADs, opioid-affected deliveries
Regression Results
As shown in Table 2, among women with non-OADs, those who were 35 years or older had lower odds of antenatal admission, while Black, non-Hispanic women; Hispanic women; those with public coverage; and those who were uninsured/self-pay had significantly greater odds of antenatal admission. Those with multiple gestation (aOR, 2.86, [95% CI=2.78–2.94]); preterm delivery (aOR=2.93, 95% CI=2.89–2.98); a behavioral health condition (aOR, 3.71, [95% CI=3.63–3.78]); or a chronic physical health condition (aOR 4.03, [95% CI=3.98–4.09]) had significantly greater odds of any antenatal admission.
Table 2.
Models estimating odds of any antenatal admission among women with opioid-affected deliveries and among women with non-opioid-affected deliveriesa
| Odds of any antenatal admission among women with OADs (n=14,310 deliveries)b | Odds of any antenatal admission among women with non-OADs (n=2,521,783 deliveries)b | |||
|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | |
| Age (ref: 18–34 years) | ||||
| >=35 years | 1.02 | 0.87 – 1.18 | 0.98**c | 0.96 – 0.99 |
| Race/ethnicity (ref: White, non-Hispanic) | ||||
| Black, non-Hispanic | 1.01 | 0.82 – 1.25 | 1.73*** | 1.71 – 1.76 |
| Hispanic | 1.08 | 0.90 – 1.31 | 1.38*** | 1.36 – 1.40 |
| Other | 0.83 | 0.64 – 1.08 | 1.00 | 0.98 – 1.02 |
| Primary payer (ref: commercially insured) | ||||
| Public coverage | 1.16 | 1.00 – 1.36 | 1.35*** | 1.33 – 1.36 |
| Uninsured/self-pay | 0.93 | 0.71 – 1.21 | 1.04* | 1.01 – 1.07 |
| Multiple gestation | 2.24*** | 1.62 – 3.11 | 2.86*** | 2.78 – 2.94 |
| Preterm delivery | 1.59*** | 1.41 – 1.79 | 2.93*** | 2.89 – 2.98 |
| Behavioral health condition present | 5.44*** | 4.94 – 5.99 | 3.71*** | 3.63 – 3.78 |
| Physical health condition present | 2.86*** | 2.55 – 3.20 | 4.03*** | 3.98 – 4.09 |
All logistic regression models adjusted for variables listed in the table and included state and year fixed effects.
Observations missing race and payer were excluded from the models.
*P<0.05; **P<0.01, ***P<0.001
Abbreviations: OADs: opioid-affected deliveries; ref: reference; aOR, adjusted odds ratio; CI, confidence interval.
Among women with OADs, age, race/ethnicity, and payer were not associated with higher odds of antenatal admission. However, similar to women with non-OADs, those with multiple gestation (aOR 2.24, [95% confidence interval [CI]=1.62–3.11]); preterm delivery (aOR 1.59, [95% CI=1.41–1.79]); a behavioral health condition (aOR 5.44, [95% CI=4.94–5.99]); or a chronic physical health condition (aOR 2.86, [95% CI=2.55–3.20]) had significantly higher odds of any antenatal admission than women without these conditions.
Overall, results for models predicting multiple antenatal admissions in each group were similar in magnitude, direction, and significance to those predicting any admission (Appendix B, Table B1), with the exception of the associations between behavioral health and physical health conditions and multiple antenatal admissions. These associations were greater in magnitude for women with OADs and non-OADs.
Discharge Diagnoses for Antenatal Admissions Prior to OADs and non-OADs
Table 3 shows the ten most frequently documented discharge diagnoses for antenatal admissions prior to OADs and non-OADs, ranked in descending order of frequency. Among non-OADs, threatened premature labor was the most common specified discharge diagnosis (n=37,725 of a total of 848,815 diagnoses in any diagnosis field), followed by infections of the genitourinary tract (n=27,386). Two different ICD-9-CM codes for anemia (n=21,336 and n=12,101) appeared in the top ten most frequent diagnoses in this group, and “mental disorders” was ranked fifth. In contrast, the six most common specified diagnoses for antenatal admissions prior to OADs were related to behavioral health conditions, with drug dependence, mental health disorders, and tobacco use disorder being the three most frequently documented. Infections of the genitourinary tract was ranked ninth and anemia tenth in this group.
Table 3.
Ten most common discharge diagnoses for antenatal admissions prior to opioid-affected deliveries and non-opioid-affected deliveries
| Antenatal admissions prior to OADsa | Antenatal admissions prior to non-OADsb | ||||
|---|---|---|---|---|---|
| Rank | Discharge Diagnosis | Frequency | Rank | Discharge Diagnosis | Frequency |
| 1 | Drug dependence | 2,106 | 1 | Other condition, not specified | 66,920 |
| 2 | Mental disorders | 1,821 | 2 | Threatened premature labor | 37,725 |
| 3 | Tobacco use disorder | 1,622 | 3 | Infections of genitourinary tract | 27,386 |
| 4 | Other condition, not specified | 1,537 | 4 | Anemiac | 21,336 |
| 5 | Opioid type dependence, continuous | 1,176 | 5 | Mental disorders | 16,921 |
| 6 | Opioid type dependence, unspecified | 836 | 6 | Elderly multigravida | 15,068 |
| 7 | Drug withdrawal | 796 | 7 | Previous cesarean delivery | 13,118 |
| 8 | Other viral diseases | 620 | 8 | Cervical shortening | 12,673 |
| 9 | Infections of genitourinary tract | 605 | 9 | Asthma | 12,468 |
| 10 | Anemia | 547 | 10 | Anemia, unspecified‡ | 12,101 |
There were a total of 33,126 diagnoses found in any diagnosis field on discharge records for antenatal admissions prior to OADs. Each delivery could have multiple antenatal admissions and each discharge record could list up to 15 diagnoses.
There were a total of 848,815 diagnoses found on discharge records for antenatal admissions prior to non-OADs.
There were two ICD-9-CM codes for anemia among the 10 most commonly-listed discharge diagnoses for antenatal admissions prior to non-OADs, the first corresponding to “anemia of mother, antepartum condition or complication” and the second, “anemia, unspecified.”
Abbreviations: OADs: opioid-affected deliveries
Discussion
Principal Findings
This study, the first to our knowledge to examine antenatal admissions among women with and without opioid-affected deliveries, found that admissions among women with OADs were more prevalent and were associated with a longer mean length of stay than admissions among women with non-OADs. The presence of a non-opioid behavioral health condition was associated with higher odds of antenatal admission in both women with OADs and non-OADs, with a particularly strong association among women with OADs.
Results and Implications
There is limited literature on antenatal admission, with much of the research occurring prior to the current opioid crisis.(Adams, Harlass, Sarno, Read, & Rawlings, 1994; Bacak et al., 2005; Bennett, Kotelchuck, Cox, Tucker, & Nadeau, 1998; Franks et al., 1992; Gazmararian et al., 2002; Martin et al., 2016; Scott et al., 1997) We found an antenatal admission ratio of 26.4 per 100 among women with OADs, over four-fold higher than for non-OADs, and a mean length of stay of a day and a half longer, providing further evidence that pregnant women with opioid dependence or abuse are a high-risk group with significant morbidity. While elective admissions for induction onto methadone or buprenorphine, which we were unable to identify, may have contributed to this higher ratio, given significant barriers to receipt of medication treatment for opioid use disorders by pregnant women,(Patrick et al., 2018; Short, Hand, MacAfee, Abatemarco, & Terplan, 2018) we would expect the impact of inpatient induction to be modest. In contrast, for women with non-OADs, we found a ratio of 6.7 per 100 deliveries, lower than a previously-reported ratio of 12.8 per 100 deliveries from 1999 to 2000.(Bacak et al., 2005) While recent studies show that the prevalence of chronic conditions among pregnant women is increasing, particularly driven by substance use disorders,(Admon, Winkelman, Heisler, & Dalton, 2018; Admon et al., 2017; Admon, Winkelman, Zivin, et al., 2018) the lower admission rate we observed perhaps reflects an encouraging change over time in management of pregnancy complications among women without an OAD,(Bacak et al., 2005; Bennett et al., 1998) a trend that has not yet been observed in the management of women with OADs.
While there has been some progress made in recent years, the delivery of medical, mental health, and substance use disorder services to those affected by OADs, and to pregnant women in particular, remains quite siloed. In this study, the higher prevalence of antenatal admissions among women with OADs highlights the need to improve the often-fragmented outpatient care women with opioid use disorder often receive in the perinatal period.(Clemans-Cope et al., 2019) Preventing antenatal admissions will require comprehensive and coordinated care across multiple dimensions addressing opioid dependence or abuse, general primary care needs, reproductive health, and critically, behavioral health concerns and social factors that may serve as barriers to treatment. A 2019 Cochrane review found that social support during pregnancies at high risk for preterm delivery or a low birthweight infant by professionals or trained lay persons (e.g., emotional support; direct assistance including home visits and transportation; information and counseling) was associated with a reduction in the number of antenatal admissions per participant.(East, Biro, Fredericks, & Lau, 2019) Better understanding how to adapt and implement similar programs for women whose pregnancies are impacted by opioids, as well as rigorously evaluate their effectiveness in this population, is a critical need.
Prior work has found that younger women, women of color, and those without commercial insurance have higher odds of antenatal admission,(Bacak et al., 2005; Gazmararian et al., 2002; Martin et al., 2016) and are most commonly hospitalized in the antenatal period for preterm labor, hyperemesis gravidarum, hypertension, kidney disorders, and prolonged premature rupture of membranes.(Bacak et al., 2005; Gazmararian et al., 2002) Our results for admissions prior to non-OADs are consistent with these findings. In contrast, among women with OADs, sociodemographic characteristics were not significantly associated with odds of antenatal admission, and behavioral health conditions comprised the majority of the ten most commonly-documented discharge diagnoses for antenatal admissions prior to OADs. Many inpatient settings that are accustomed to managing the physical health conditions commonly seen in the antenatal period such as preterm labor and hyperemesis gravidarum may be challenged to provide adequate inpatient psychosocial support, facilitate safe discharges, and arrange necessary outpatient follow-up for women with predominantly behavioral health comorbidities.
Not only did behavioral health conditions dominate the list of common diagnoses for antenatal admissions among women with OADs, those with a behavioral health condition had nearly five times higher odds of being admitted in the antenatal period. Furthermore, there was a significant association between behavioral health conditions and antenatal admission among women with non-OADs. The high prevalence of co-occurring mental health conditions among pregnant women with opioid use disorder has been described, with estimates ranging from approximately 25–33%, (Arnaudo, Andraka-Christou, & Allgood, 2017; Faherty, Matone, Passarella, & Lorch, 2018; Holbrook & Kaltenbach, 2012) and they have been associated with poorer maternal, neonatal, and treatment outcomes.(Fitzsimons, Tuten, Vaidya, & Jones, 2007; Tuten et al., 2009) Co-occurring substance use disorders in addition to opioid use disorder are also common. (Clemans-Cope et al., 2019). We find these co-occurring behavioral health conditions are associated with significantly higher odds of antenatal admission in both women with OADs and non-OADs. Given the association between untreated maternal behavioral health conditions and multiple downstream effects on the child, including decreased attachment, cognitive delays, and depression,(O’Hara & McCabe, 2013; Pearson et al., 2013; Tronick & Reck, 2009) these findings reinforce the need to screen for and address mental health conditions and co-occurring substance use at key opportunities when all pregnant women, particularly those with opioid dependence or abuse, interface with the healthcare system. Such interventions should be aimed not only at preventing admissions in the antenatal period, but more broadly at supporting the health and wellbeing of the mother-infant dyad in the short, medium, and long terms.
Strengths and Limitations
Our findings must be considered within the context of the study’s limitations. We attempted to exclude admissions occurring prior to the start of pregnancy and prolonged admissions leading to delivery but may have included pre-pregnancy admissions (particularly for preterm deliveries), missed early pregnancy admissions (particularly for post-term deliveries) or excluded non-delivery admissions in the four days prior to delivery. We were unable to examine certain sociodemographic variables such as educational attainment and marital status, or clinical covariates such as obesity, smoking status, or type of opioid use in pregnancy (e.g., medication treatment for opioid use disorder, heroin, prescription opioid misuse). Misclassification may have affected the ICD-9-CM codes used to identify opioid-affected deliveries, as well as the discharge diagnosis codes for antenatal admissions. We were unable to observe admissions for induction onto medication treatment for opioid use disorder, nor could we distinguish the primary reason for admission from co-occurring conditions documented on the discharge record. Finally, in this observational study, we report associations and are unable to make causal claims. These limitations are balanced by the following strengths: we examined a large sample of deliveries from geographically diverse states, we analyzed an all-payer database with minimal data missingness, we leveraged a unique longitudinal patient-level identifier that allowed us to link multiple admissions for the same individual, and we contribute to a literature that has not been updated since the beginning of the ongoing opioid crisis.
Conclusions for Practice
There is a growing recognition that mental health conditions and substance use disorders are a significant contributor to maternal morbidity and mortality in the United States. This study found that antenatal admissions were more common and resulted in longer lengths of stays for women with OADs compared to women with non-OADs and among both groups, behavioral health conditions were significantly associated with odds of admission. These results highlight the importance of identifying and addressing the large burden of behavioral health conditions among pregnant women overall, especially those with opioid dependence and abuse. Specifically, efforts to implement standardized screening and referral processes for behavioral health conditions, co-locate and integrate behavioral health and prenatal care, and increase Medicaid reimbursement rates for behavioral health services are critically needed. Building capacity among perinatal providers to identify and treat behavioral health conditions such as opioid use disorder and expanding the use of tele-mental health are other potential strategies to address the unmet need for behavioral health care in the perinatal period. Finally, strengthening social supports during pregnancy such as home visiting, direct assistance (e.g., transportation, childcare), and group prenatal care with strong peer support components are also approaches worthy of greater consideration. Complex interactions of biopsychosocial factors influence antenatal admission, as well as postpartum outcomes, among women with and without OADs. An effective public health approach to preventing maternal morbidity and mortality will require a variety of interventions tailored to individual needs and rigorous evaluation of their effectiveness in different populations.
Significance:
Little is known about antenatal admissions among women with opioid-affected deliveries and how they compare to women with non-opioid-affected deliveries. We found the antenatal admission ratio among women with opioid-affected deliveries to be over four-fold higher than among those with non-opioid-affected deliveries. The presence of a non-opioid behavioral health condition was associated with higher odds of antenatal admission in both groups, with a particularly strong association among women with opioid-affected deliveries. Our results highlight the importance of addressing the large burden of behavioral health conditions among pregnant women overall, especially those with opioid dependence and abuse.
Acknowledgements:
R21DA045212 “An Exploratory Analysis of the Association of State Policies and Neonatal Abstinence Syndrome” (PI: Faherty) and P50DA046351 “Opioid Policy Tools and Information Center for Research Excellence” (PI: Stein). The authors wish to thank Hilary Peterson of the RAND Corporation (supported by R21DA045212) for preparing the paper for submission.
Appendix A.
Clinical Classification System (CCS) codes and International Classification of Diseases, Ninth Revision, Clinical Modification, (ICD-9-CM) codes Used to Identify Co-occurring Clinical Conditions Present at Antenatal Admissions and/or the Delivery Hospitalization
| Multiple gestation | ICD-9-CM codes |
| 651, V27.2-V27.7 | |
| Preterm delivery | ICD-9-CM codes |
| 644.20, 644.21 | |
| Behavioral Health Conditions | CCS codes or ICD-9-CM codes |
| Anxiety disorders | 651 |
| Mood disorders | 657 |
| Personality disorders | 658 |
| Schizophrenia/other psychotic disorders | 659 |
| Substance dependence of abuse (non-opioid) | 30300–30303; 30390–30393; 30420–30423; 30560–30563; 30430–30433; 30520–30523; 30410–30413; 30440–30443; 30450–30453; 30460–30463; 30530–30533; 30540–30543; 30570–30573; 30580–30583; 30480–30483; 30490–30493; 30590–30593 |
| Chronic Physical Health Conditions | ICD-9-CM codes |
| Chronic respiratory disease | 491.x-496.x |
| Chronic hypertension | 401.x-405.x, 642.0x, 642.1x, 642.2x, 642.7x |
| Pre-existing diabetes | 249.x, 250.x, 648.0x |
| Chronic heart disease | 412.x-414.x, 394.x-397.x, 424.x, 428.22, 428.23, 428.32, 428.33, 428.42, 428.43, 648.5x, 745.0x-747.4x, |
| Chronic renal disease | 581.x-583.x, 585.x, 587.x, 588.x, 646.2x |
| Chronic liver disease | 571.x, 572.x |
| HIV | 042.x, V08.x |
Appendix B.
Table B1.
Models estimating odds of multiple antenatal admissions among women with opioid-affected deliveries and multiple antenatal admissions among women with non-opioid-affected deliveriesa,b
| Odds of multiple antenatal admissions among women with OAD (n=14,310 deliveries)c | Odds of multiple antenatal admissions among women with non-OAD (n=2,521,783 deliveries) | |||
|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | |
| Age (ref: 18–34 years) | ||||
| >=35 years | 1.06 | 0.83 – 1.34 | 0.93***d | 0.89 – 0.96 |
| Race/ethnicity (ref: White, non-Hispanic) | ||||
| Black, non-Hispanic | 1.21 | 0.90 – 1.62 | 1.99*** | 1.93 – 2.06 |
| Hispanic | 1.08 | 0.81 – 1.46 | 1.43*** | 1.38 – 1.48 |
| Other | 0.80 | 0.54 – 1.20 | 1.00 | 0.95 – 1.05 |
| Primary payer (ref: commercially insured) | ||||
| Public coverage | 1.33* | 1.01 – 1.74 | 1.44*** | 1.40 – 1.49 |
| Uninsured/self-pay | 1.09 | 0.71 – 1.70 | 1.06 | 0.99 – 1.14 |
| Multiple gestation | 2.05** | 1.24 – 3.39 | 2.80*** | 2.65 – 2.95 |
| Preterm delivery | 1.61*** | 1.34 – 1.94 | 3.37*** | 3.25 – 3.48 |
| Behavioral health condition present | 9.00*** | 7.46 – 10.86 | 5.50*** | 5.30 – 5.70 |
| Physical health condition present | 3.07*** | 2.59 – 3.63 | 5.54*** | 5.39 – 5.71 |
“Multiple” is defined as two or more antenatal admissions.
All logistic regression models adjusted for variables listed in the table and included state and year fixed effects.
Observations missing race and payer were excluded from the models.
*P<0.05; **P<0.01, ***P<0.001
Abbreviations: OAD: opioid-affected deliveries; ref: reference; aOR, adjusted odds ratio; CI, confidence interval.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Contributor Information
Laura J. FAHERTY, RAND Corporation, Boston, MA;; School of Medicine, Boston University, Boston, MA
Ashley M. KRANZ, RAND Corporation, Arlington, VA.
Mr. Joshua RUSSELL-FRITCH, RAND Corporation, Santa Monica, CA.
Mr. Teague RUDER, RAND Corporation, Santa Monica, CA.
Stephen W. PATRICK, Department of Pediatrics, Vanderbilt University, Nashville, Tennessee; Mildred Stahlman Division of Neonatology, Vanderbilt University, Nashville, Tennessee; Vanderbilt Center for Child Health Policy, Nashville, Tennessee; Department of Health Policy, Vanderbilt University, Nashville, Tennessee; RAND Corporation, Pittsburgh, Pennsylvania.
Bradley D. STEIN, RAND Corporation, Pittsburgh, PA; School of Medicine, University of Pittsburgh, Pittsburgh, PA.
References
- Adams MM, Harlass FE, Sarno AP, Read JA, & Rawlings JS (1994). Antenatal hospitalization among enlisted servicewomen, 1987–1990. Obstet Gynecol, 84(1), 35–39. [PubMed] [Google Scholar]
- Admon LK, Winkelman TNA, Heisler M, & Dalton VK (2018). Obstetric Outcomes and Delivery-Related Health Care Utilization and Costs Among Pregnant Women With Multiple Chronic Conditions. Prev Chronic Dis, 15, E21. doi: 10.5888/pcd15.170397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Admon LK, Winkelman TNA, Moniz MH, Davis MM, Heisler M, & Dalton VK (2017). Disparities in Chronic Conditions Among Women Hospitalized for Delivery in the United States, 2005–2014. Obstet Gynecol, 130(6), 1319–1326. doi: 10.1097/AOG.0000000000002357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, & Dalton VK (2018). Racial and Ethnic Disparities in the Incidence of Severe Maternal Morbidity in the United States, 2012–2015. Obstet Gynecol, 132(5), 1158–1166. doi: 10.1097/AOG.0000000000002937 [DOI] [PubMed] [Google Scholar]
- Arnaudo CL, Andraka-Christou B, & Allgood K (2017). Psychiatric Co-Morbidities in Pregnant Women with Opioid Use Disorders: Prevalence, Impact, and Implications for Treatment. Curr Addict Rep, 4(1), 1–13. doi: 10.1007/s40429-017-0132-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacak SJ, Callaghan WM, Dietz PM, & Crouse C (2005). Pregnancy-associated hospitalizations in the United States, 1999–2000. Am J Obstet Gynecol, 192(2), 592–597. doi: 10.1016/j.ajog.2004.10.638 [DOI] [PubMed] [Google Scholar]
- Bennett TA, Kotelchuck M, Cox CE, Tucker MJ, & Nadeau DA (1998). Pregnancy-associated hospitalizations in the United States in 1991 and 1992: a comprehensive view of maternal morbidity. Am J Obstet Gynecol, 178(2), 346–354. [DOI] [PubMed] [Google Scholar]
- Clemans-Cope L, Lynch V, Howell E, Hill I, Holla N, Morgan J, … Thompson JA (2019). Pregnant women with opioid use disorder and their infants in three state Medicaid programs in 2013–2016. Drug Alcohol Depend, 195, 156–163. doi: 10.1016/j.drugalcdep.2018.12.005 [DOI] [PubMed] [Google Scholar]
- East CE, Biro MA, Fredericks S, & Lau R (2019). Support during pregnancy for women at increased risk of low birthweight babies. Cochrane Database Syst Rev, 4, CD000198. doi: 10.1002/14651858.CD000198.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faherty LJ, Matone M, Passarella M, & Lorch S (2018). Mental Health of Mothers of Infants with Neonatal Abstinence Syndrome and Prenatal Opioid Exposure. Matern Child Health J, 22(6), 841–848. doi: 10.1007/s10995-018-2457-6 [DOI] [PubMed] [Google Scholar]
- Fitzsimons HE, Tuten M, Vaidya V, & Jones HE (2007). Mood disorders affect drug treatment success of drug-dependent pregnant women. Journal of Substance Abuse Treatment, 32(1), 19–25. doi: 10.1016/j.jsat.2006.06.015 [DOI] [PubMed] [Google Scholar]
- Franks AL, Kendrick JS, Olson DR, Atrash HK, Saftlas AF, & Moien M (1992). Hospitalization for pregnancy complications, United States, 1986 and 1987. Am J Obstet Gynecol, 166(5), 1339–1344. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Petersen R, Jamieson DJ, Schild L, Adams MM, Deshpande AD, & Franks AL (2002). Hospitalizations during pregnancy among managed care enrollees. Obstet Gynecol, 100(1), 94–100. [DOI] [PubMed] [Google Scholar]
- Haight SC, K. J, Tong VT, Bohm MK, Callaghan WM. (2018). Opioid Use Disorder Documented at Delivery Hospitalization -- United States, 1999–2014. MMWR Morb Mortal Wkly Rep(67), 845–849. doi: 10.15585/mmwr.mm6731a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook A, & Kaltenbach K (2012). Co-occurring psychiatric symptoms in opioid-dependent women: the prevalence of antenatal and postnatal depression. Am J Drug Alcohol Abuse, 38(6), 575–579. doi: 10.3109/00952990.2012.696168 [DOI] [PubMed] [Google Scholar]
- Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, & Marchbanks PA (2008). An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J, 12(4), 469–477. doi: 10.1007/s10995-007-0256-6 [DOI] [PubMed] [Google Scholar]
- Maeda A, Bateman BT, Clancy CR, Creanga AA, & Leffert LR (2014). Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology, 121(6), 1158–1165. doi: 10.1097/ALN.0000000000000472 [DOI] [PubMed] [Google Scholar]
- Martin AS, Zhang Y, Crawford S, Boulet SL, McKane P, Kissin DM, … States Monitoring Assisted Reproductive Technology, C. (2016). Antenatal Hospitalizations Among Pregnancies Conceived With and Without Assisted Reproductive Technology. Obstet Gynecol, 127(5), 941–950. doi: 10.1097/AOG.0000000000001392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina RL, & Pace LE (2017). A Renewed Focus on Maternal Health in the United States. N Engl J Med, 377(18), 1705–1707. doi: 10.1056/NEJMp1709473 [DOI] [PubMed] [Google Scholar]
- Moniz MH, Spector-Bagdady K, Heisler M, & Harris LH (2017). Inpatient Postpartum Long-Acting Reversible Contraception: Care That Promotes Reproductive Justice. Obstet Gynecol, 130(4), 783–787. doi: 10.1097/AOG.0000000000002262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara MW, & McCabe JE (2013). Postpartum depression: current status and future directions. Annu Rev Clin Psychol, 9, 379–407. doi: 10.1146/annurev-clinpsy-050212-185612 [DOI] [PubMed] [Google Scholar]
- Patrick SW, Buntin MB, Martin PR, Scott TA, Dupont W, Richards M, & Cooper WO (2018). Barriers to Accessing Treatment for Pregnant Women with Opioid Use Disorder in Appalachian States. Subst Abus, 1–18. doi: 10.1080/08897077.2018.1488336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, & Davis MM (2012). Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA, 307(18), 1934–1940. doi: 10.1001/jama.2012.3951 [DOI] [PubMed] [Google Scholar]
- Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, … Stein A (2013). Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry, 70(12), 1312–1319. doi: 10.1001/jamapsychiatry.2013.2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CL, Chavez GF, Atrash HK, Taylor DJ, Shah RS, & Rowley D (1997). Hospitalizations for severe complications of pregnancy, 1987–1992. Obstet Gynecol, 90(2), 225–229. doi: 10.1016/S0029-7844(97)00230-5 [DOI] [PubMed] [Google Scholar]
- Short VL, Hand DJ, MacAfee L, Abatemarco DJ, & Terplan M (2018). Trends and disparities in receipt of pharmacotherapy among pregnant women in publically funded treatment programs for opioid use disorder in the United States. J Subst Abuse Treat, 89, 67–74. doi: 10.1016/j.jsat.2018.04.003 [DOI] [PubMed] [Google Scholar]
- Tronick E, & Reck C (2009). Infants of depressed mothers. Harv Rev Psychiatry, 17(2), 147–156. doi: 10.1080/10673220902899714 [DOI] [PubMed] [Google Scholar]
- Tuten M, Fitzsimons H, Chisolm MS, Jones HE, Heil SH, & O’Grady KE (2009). The Impact of Mood Disorders on the Delivery and Neonatal Outcomes of Methadone-Maintained Pregnant Patients. American Journal of Drug and Alcohol Abuse, 35(5), 358363. doi: 10.1080/00952990903108231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, & Patrick SW (2018). Incidence and Costs of Neonatal Abstinence Syndrome Among Infants With Medicaid: 2004–2014. Pediatrics, 141(4). doi: 10.1542/peds.2017-3520 [DOI] [PMC free article] [PubMed] [Google Scholar]


