Abstract
As more nurses embrace precision science, there is a tendency to utilize theoretical frameworks from other disciplines thus, placing nursing at risk of losing its autonomy and independence. The discipline has fallen prey to internal binary opposition, eliminating opportunities to engage in civil discourse. To explore how the roles nurses select might fit together in a theoretical framework and help nurses understand how the roles they choose to support their identity as nurses, this paper introduced a model of nursing that includes the bench scientists, the policy activists, and bedside nurses, using the Neuman Systems Model (NSM). The Nurse Role Integration Model (NRIM) espouses the basic tenets of NSM: prevention counteracts stressors from penetrating the client’s lines of defense thus, reducing stress response. Primary prevention reflects the work of the nurse bench scientists, investigating the underlying mechanisms behind pathophysiology; secondary prevention is applied nurse scientists who build upon nurse researchers’ work, identifying and testing potential interventions; tertiary prevention is nurse policy activists, the fulcrum, who leverage primary and secondary findings to argue policy change at all levels. Once policy change is adopted, bedside nurses are educated and implement the change. This lens provides an opportunity to create greater solidarity, strengthening the unity and autonomy of the discipline.
Keywords: Neuman systems model, Nurse’s role, Nursing theory, Pre-clinical models, Theoretical models
What is known?
-
•
As precision science takes a greater role in nursing, many nurses have chosen to adopt conceptual and theoretical frameworks from non-nursing disciplines thus, the profession risks losing its identify as an independent discipline with its own science and knowledge base.
What is new?
-
•
The Nurse Role Integration Model (NRIM), based on the Neuman Systems Model (NSM), may have the potential to change the way we look at different roles in nursing.
As a nursing PhD student and neonatal intensive care unit (NICU) nurse, my research focused on the neurodevelopmental outcomes of repeated painful or stressful procedures on preterm infants. Preterm infants often face seemingly insurmountable odds for survival, compounded by a stressful, unnatural environment with prolonged parent-infant separation and painful procedures or treatments that are a part of routine-lifesaving care. These types of early adverse life experiences have demonstrated a negative impact on infant development. Sequelae of parent-infant separation and repeated tissue injury include epigenetic alterations that affect neurotransmitter function, can affect the hypothalamic-pituitary-adrenal axis leading to dysregulation and even decreased neuronal myelination and white matter [[1], [2], [3], [4], [5], [6], [7]]. Building on previous research, I chose to investigate how repeated painful procedures combined with alterations in serotonin expression might affect behavior and neuroanatomy. Since the tissue of origin (brain tissue) is required, my only option was to use a rodent model to give us an inside look into these effects.
Early on, I had the opportunity to share my dissertation proposal with colleagues at the Robert Wood Johnson Foundation Future of Nursing Scholars Summer Institute. I responded to many questions regarding my proposal, however, the question for which I was not prepared to answer was: “How does this translate? It does not seem like nursing to me”. This caused quite a bit of angst and much reflection. Is my researchnursingresearch? Is it nursing science? Do I belong in another discipline? This identity crisis led me on a journey of self-reflection, theory research and ultimately to a new understanding of the many varied roles in nursing including mine.
Almost twenty years ago, Johnson (1991) stated “controversy is the starting point for all philosophic enterprises” (p.9) [8]. In 2020, nurse scientists have access to instrumentation that offers greater insight into basic sciences such as bio-behavioral science, symptom science, precision science and omics [9]. These instruments offer a bench research method to investigate the underlying pathophysiology of diseases that have influenced patients and nurses who care for them. However, as nurses pursue bench research, it has reignited a long-standing concern among many nurse scholars that without a firm commitment to, and engagement with, nursing conceptual and theoretical frameworks, we risk losing the very thing that makes the discipline unique –our holistic perspective – the meta-paradigm of interaction between human, environment, and health [9,10]. Do all roles that nurses espouse and all research questions within nursing require grounding in nursing theoretical or conceptual frameworks? Is our identity intrinsically tied to our science? I began to investigate the literature, to explore how the roles and questions nurses select might somehow fit together in a theoretical framework. I was hoping to find the answers that could help me and other nurses understand how the roles they choose support their identity as nurses.
The question that I was unable to answer was asked by Fawcett 20 years ago, “Where is the nursing in the science” [11]? One potential answer to that question requires a closer examination of nursing conceptual and theoretical frameworks and their role in maintaining our identity as an independent discipline. If nurses only adopt conceptual and theoretical frameworks from related but non-nursing disciplines, the profession risks losing its identity as an independent discipline with its own science and knowledge base. Indeed, Parse (2016) questioned whether nursing science was “being sacrificed on the altar of other disciplines’ needs” (p. 101) [12]? While nurses may choose to conduct bench science, sometimes overlapping into other disciplines, nursing knowledge serves as a unifying force, a foundation from which to maintain our identity and independence which allows us to evolve and flourish as a discipline.
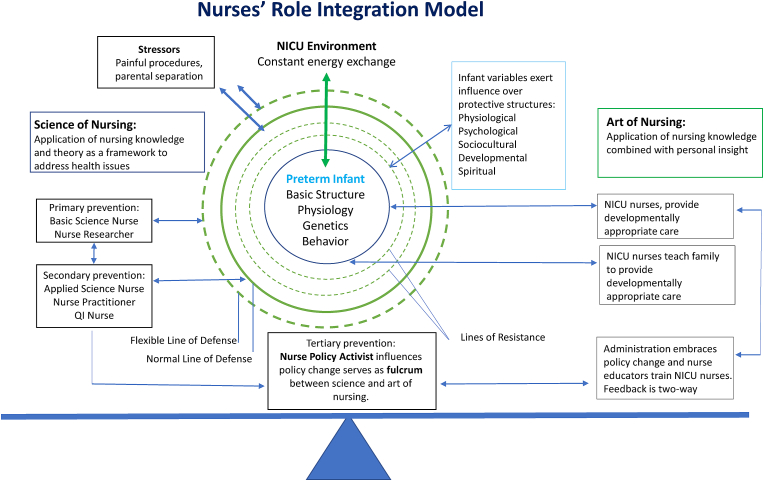
Whether to include nursing theory in undergraduate curricula has been vigorously debated over the years with many nursing programs deciding against inclusion. However, as Amankwaa noted in 2018, if “we expect some semblance of connectedness around the topic of nursing science” (p. 185) we must at least expose all nurses to nursing science based on nursing theory [13]. Exploring the richness of nursing science is often excluded particularly in undergraduate curricula where the focus is on teaching the tasks and techniques needed to become a practicing registered nurse. In addition, there is an increasing emphasis on NCLEX initial pass rates with schools that have higher pass rates being determined as superior. Yet a curriculum rich in theory is a valuable contributor to disciplinary identity. Thus, the purpose of this paper is to describe how the role that a nurse chooses to embrace (using animal models or not) works synergistically with other nurse roles. This concept is elucidated in the “Nurses’ Role Integration Model” (NRIM) based on Neuman Systems Model [9]. In the model, the Science of Nursing is the preventative side of nursing represented by roles in primary, secondary, or tertiary prevention. On the other side of the model is the Art of Nursing where a nurse applies nursing knowledge combined with personal insight to improve health and comfort at the bedside.
During my education on theory and nursing science, I immediately identified with Neuman Systems Model (NSM). Its focus on the interactions between clients and environments and the prevention of negative stressors on clients worked well with my passion for reducing harm to preterm infants [5]. As I began to think more about the NSM and how my research fit into nursing, I had an “aha” moment. Suddenly, I began to see how all roles, through to and including the nurse policy activists, had a place in our discipline. The NRIM demonstrates how conceptual and theoretical frameworks, in this case the NSM, can be used to create new knowledge with a holistic framework that integrates a wide variety of nursing roles. Theoretical and conceptual frameworks provide a basis for our identity as a discipline and thus, this model has the potential to increase solidarity across the discipline for all roles. The NRIM embraces the basic tenet of the NSM: prevention counteracts negative stressors from penetrating the client’s flexible line of defense, thereby, reducing the need to mount a stress response. In this case, the “client” represents the patient population to whom a nurse is either researching or providing care.
In this adaptation of the NSM, the client (infant), along with lines of defense and interaction with the environment (NICU, separation from parents, etc.), remains the central focus, as everything we endeavor to do in NICU nursing relates to protecting the infant in order to ensure optimal outcomes. We accomplish this by protecting the client from negative stressors through prevention. Stressors represent any threat to wellness in an individual nurse’s specific patient population, and prevention represents the roles of nurses within the discipline.
This model has the potential to change the way we look at different roles in nursing. In the model, three boxes are larger than the others, science of nursing, tertiary prevention (nurse policy activist) and the art of nursing. These three are all equal in importance. The science of nursing includes primary and secondary prevention. For example, primary prevention reflects the work of nurse research scientists. This can occur at the bench investigating underlying cellular mechanisms behind pathophysiology in an animal model. It can happen in a clinical setting, collecting human biomarkers to better understand the effect of the environment on behavior. It can take place in a hospital setting using chart review methods to make associations between methods of treatment and patient outcomes. It can arise over the internet where the researcher asks post-partum mothers about their symptoms of depression to gain a richer understanding of the challenges in caring for and preventing the disease. Each of these methods represents primary prevention, the base understanding of the human condition and giving rise to secondary inquiry leading to secondary prevention (see Fig. 1.).
Fig. 1.
Nurses’ Role Integration Model (an adaption of Neuman Systems Model, reproduced with the permission of Betty Neuman and Jacqueline Fawcett).
The findings of primary prevention promote secondary prevention. This represents applied nurse scientists or nurse practitioners who use the primary findings to develop innovative treatments or interventions to prevent or heal diseases of human conditions. For example, now that we know skin-to-skin care reduces infant cortisol levels and increases oxytocin, secondary prevention nurses might suggest that the neonatal intensive care unit that s/he works in implement skin-to-skin care during all painful procedures [14]. However, changing practice in a hospital is challenging. This is where the tertiary prevention nurse’s role becomes critical, that of the policy activist.
Without the nurse policy activist, science would simply exist in a vacuum. The nurse policy activist argues the validity and importance of science to influence policy change. That person is the fulcrum, balancing the scale between the science of nursing and the art of nursing. The nurse policy activist has the opportunity to create healthier outcomes by leveraging primary and secondary findings to argue policy change that influences change at local, state, national and global levels.
Please note that the primary prevention, secondary prevention, administration and NICU nurse boxes are all smaller but equal in size indicating there is no hierarchical nature, yet without each of them, there would be no innovation in nursing. Once policy change is approved legislatively, it can then be adopted by hospital administration. Once the administration has adopted the policy, unit directors and managers are educated on the benefit of adopting this policy. Directors and managers then advise educators on the benefits and educators then teach bedside or advance practice nurses on implementation of the intervention representing the practical application of nursing. Those nurses further educate clients and families on the benefit of the intervention and how best to implement the intervention. This application of nursing knowledge combined with each individual nurse’s personal insight constitutes the Art of Nursing (see Fig. 1.).
While this paper specifies NSM it is important to acknowledge that interaction with the environment is a concept adopted by many nurse theorists including Johnson, King, Roy, and Parse [15]. There are also biological aspects in many theories such as Roy, Orem, and Watson. In fact, any theory that focuses on holism, by its very nature must account for physical and biological factors.
This model is inclusive of many roles in nursing, whether they be the science of nursing, policy nurse activist, or art of nursing. This model constitutes new nursing knowledge however, it uses a nursing framework with historical utility. By creating new nursing knowledge based on the science of today, we have the ability to unify and strengthen the autonomy of the discipline. While the question posed during my presentation created an intellectual and professional crisis of sorts, it provided an opportunity for me to reflect upon and further explore the discipline, roles within the discipline as well as theoretical frameworks serving as the bedrock of the discipline. This exploration led me to find my own place in nursing and better understand how the many roles in nursing fit together. Barret pondered how nursing research will distinguish itself from the efforts of biological, bio-behavioral and other sciences [9]? My answer is that nursing will distinguish ourselves by using conceptual models and theoretical frameworks that provide a foundation on which to construct, disseminate and implement the findings of our science. It is the use of conceptual and theoretical frameworks that will allow us to ensure that our research is structured in a way that furthers the discipline’s growth. As research priorities change at our own and others’ tables our perspective is best heard when there is a foundation for our words and actions. Conceptual and theoretical frameworks are that foundation. While many nurses may not agree that my science is nursing, the NRIM demonstrates there is a place for animal models in nursing when the ultimate purpose of these studies is to improve outcomes for some of the most vulnerable in our society. In today’s age of precision science, it behooves our discipline to be more inclusive of all nursing research. If we do not, precision science nurses will continue to use frameworks that are outside the discipline of nursing.
The author put forward questions for contemplation and hopes these questions will provoke discussion either via direct communication with the author or via response to the journal.
-
1)
If a nurse chooses to study pre-clinical models (animal studies) does that mean s/he is not a nurse? Is the nursing paradigm relevant to them?
-
2)
Should nurses have the opportunity to discover underlying mechanisms of pathology just as other scientists? Is it possible that their findings might support the development of novel interventions that could then be applied to their population of interest and change practice for the better?
-
3)
Does nursing theory only apply to the art of nursing? What about science?
-
4)
Why do precision science nurses turn to theoretical frameworks outside of nursing? Could it be that other nurses have told them their work is not nursing?
Declaration of competing interest
No conflicts of interest to report.
Acknowledgements
Research reported in this discussion paper was supported by the National Institute for Nursing Research of the National Institutes of Health under award number [1 F32 NR018591 01]. Special thanks to Dr. E. Carol Polifroni, EdD, NEA-BC, CNE RN, ANEF for her unwavering support, guidance, and encouragement to see this discussion published.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.06.005.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Brummelte S., Chau C.M.Y., Cepeda I.L., Degenhardt A., Weinberg J., Synnes A.R., Grunau R.E. Cortisol levels in former preterm children at school age are predicted by neonatal procedural pain-related stress. Psychoneuroendocrinology. 2015;51:151–163. doi: 10.1016/j.psyneuen.2014.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chau C.M.Y., Ranger M., Sulistyoningrum D., Devlin A.M., Oberlander T.F., Grunau R.E. Neonatal pain and COMT Val158Met genotype in relation to serotonin transporter (SLC6A4) promoter methylation in very preterm infants at school age. Front Behav Neurosci. 2014;8(409):1–12. doi: 10.3389/fnbeh.2014.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D’Agata A.L., Wash S., Vittner D., Cong X., McGrath J.M., Young E.E. FKBP5 genotype and early life stress exposure predict neurobehavioral outcomes for preterm infants. Dev Psychobiol. 2016;59:410–418. doi: 10.1002/dev.21507. [DOI] [PubMed] [Google Scholar]
- 4.Montirosso R., Provenzi L., Fumagalli M., Sirgiovanni I., Giorda R., Pozzoli U. Serotonin transporter gene (SLC6A4) methylation associates with neonatal intensive care unit stay and 3-month-old termperment in preterm infants. Child Dev. 2016;87(1):38–48. doi: 10.1111/cdev.12492. [DOI] [PubMed] [Google Scholar]
- 5.Provenzi L., Fumagalli M., Sirgiovanni I., Giorda R., Pozzoli U., Morandi F., Beri S., Menozzi G., Mosca F., Borgatti R., Montirosso R. Pain-related stress during the Neonatal Intensive Care Unit stay and SLC6A4 methylation in very preterm infants. Front Behav Neurosci. 2015;9(99):1–9. doi: 10.3389/fnbeh.2015.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rohan A.J. Pain-associated stressor exposure and neuroendocrine values for premature infants in neonatal intensive care. Dev Psychobiol. 2015:60–70. doi: 10.1002/dev.21346. [DOI] [PubMed] [Google Scholar]
- 7.Kurinczuk J.J., White-Koning M., Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev. 2010;86:329–338. doi: 10.1016/j.earlhumdev.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Johnson J.L. Nursing science: basic, applied or practical? Implications for the art of nursing. Adv Nurs Sci. 1991;14(1):7–16. doi: 10.1097/00012272-199109000-00003. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=ovfta&NEWS=N&AN=00012272-199109000-00003 Retrieved from: Retrieved from. [DOI] [PubMed] [Google Scholar]
- 9.Barrett E. Again, what is nursing science? Nurs Sci Q. 2017;30(2):129–133. doi: 10.1177/0894318417693313. [DOI] [PubMed] [Google Scholar]
- 10.Turkel M., Fawcett J., Chinn P.L., Eustace R., Hansell P.S., Smith M.C. Thoughts about advancement of the discipline: dark clouds and bright lights. Nurs Sci Q. 2018;31(1):82–85. doi: 10.1177/0894318417741121. [DOI] [PubMed] [Google Scholar]
- 11.Fawcett J. The state of nursing science: where is the nursing in science? Theoria: J. Nurs. Theory. 2000;9:3–10. https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106917115&site=ehost-live Available from: [Google Scholar]
- 12.Parse R. Where have all the nursing theories gone? Nurs Sci Q. 2016;29:101–102. doi: 10.1177/0894318416636392. [DOI] [PubMed] [Google Scholar]
- 13.Turkel M.C., Fawcett J., Amankwaa L., Clarke P.N., Dee V., Eustace R. Thoughts about nursing curricula: dark clouds and bright lights. Nurs Sci Q. 2018;31(2):185–189. doi: 10.1177/0894318418755734. [DOI] [PubMed] [Google Scholar]
- 14.Cong Xiaomei, Luddington-Hoe Susan, Walsh Stephen. Randomized Crossover Trial of Kangaroo Care to Reduce Biobehavioral Pain Responses in Preterm Infants: A Pilot StudyApril 2011, Vol.13(2), pp.204-216. Biological Research For Nursing. 2011;13(2):204–216. doi: 10.1177/1099800410385839. [DOI] [PubMed] [Google Scholar]
- 15.Szanton S.L., Gill J.M. Facilitating resilience using a society-to-cells framework: a theory of nursing essentials applied to research and practice. Adv Nurs Sci. 2010;33(4):329–343. doi: 10.1097/ANS.0b013e3181fb2ea2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.