Abstract
Objective
To identify self-care actions for the maintenance of arteriovenous fistula of renal patients.
Method
An integrative review study was conducted and literature were searched in Medline/PubMed, Scopus, CINAHL, LILACS, BDENF and SciELO Library databases using the descriptors chronic renal insufficiency, arteriovenous fistula, self-care, and knowledge. The inclusion criteria were that the documents be written in Portuguese, English, and Spanish, full text available, published in the last five years, and that they address the research question. Reflection articles, theses, dissertations, editorials of non-scientific journals, and research studies that did not follow the necessary methodological rigor were excluded. Data were analyzed with the IRAMUTEQ software.
Results
Fifteen articles were selected and comprised the final sample. Seven classes of self-care actions emerged from the text segments analysis and grouped into three categories: 1) Self-care actions that maintain the arteriovenous fistula; 2) Self-care actions for the prevention and the monitoring of complications with arteriovenous fistula; 3) Self-care actions directed at the perioperative period of arteriovenous fistula preparation.
Conclusion
The results allowed us to identify important care for the maintenance of arteriovenous fistula functionality. The self-care actions identified in this study can guide a nursing care policy for implementation with protocols that help identify problems related to self-care actions and, thus, subsidize the development of actions aimed at the renal patient. However, more studies with high levels of evidence that identify self-care actions with arteriovenous fistula and the factors involved in its implementation are needed.
Keywords: Arteriovenous fistula, Chronic renal insufficiency, Health education, Renal dialysis, Self care
What is known?
-
•
An arteriovenous fistula is the best access for hemodialysis and, therefore, self-care actions to maintain its functionality should be followed by chronic renal patients.
-
•
An integrative review was published in 2013 about self-care with the arteriovenous fistula; however, the article focused on the identification of ‘teaching’ interventions that promote self-care of the access.
What is new?
-
•
The self-care actions described in this review are important to the preservation of an arteriovenous fistula, which was made possible by the methodological quality of the studies that composed the sample. The presence of experimental, quasi-experimental and studies that aimed to construct and validate scales in the sample contributed to the emergence of important self-care actions necessary to preserve an arteriovenous fistula.
-
•
The self-care actions identified in this study can guide a nursing care policy and subsidize the development of actions aimed at the renal patient, favoring the maintenance of adequate practices about the access.
1. Introduction
Chronic Kidney Disease (CKD) is a major global health challenge, especially in low and middle-income countries. In high-income countries, the overall prevalence of CKD in adults over 20 years old is 8.6% among males and 9.6% in females. In low-income countries, this rate increases to 10.6% in men and 12.5% in women [1]. In Brazil, according to the Brazilian Society of Nephrology, about 126,583 individuals underwent treatment for CKD in July 2017, with an average annual increase of 4960 patients between 2002 and 2017 [2].
Among the Substitutive Renal Therapy (SRT) modalities, hemodialysis is the therapy used by 92.1% of patients in Brazil [2]. To perform this treatment, however, the patient must have vascular access [3]. Hence, the access choice represents one of the most important factors associated with a patient’s health outcomes [4].
The arteriovenous fistula (AVF) is considered the most adequate access for hemodialysis therapy, because it has longer durability, allows a safe and continuous vascular system approach, and is associated with a lower morbidity and mortality in comparison with arteriovenous grafts and catheters. Patients undergoing central venous catheter therapy usually present higher infection rates, cardiovascular events, and hospitalization [5].
Despite the lower complication rates related to AVF, complications may be present in access. A systematic review identified that, on average, the complication rate per 1000 patient-days was 0.04 for aneurysms (14 single cohorts, n = 1827 fistulas), 0.11 for infections (16 cohorts, n = 6439 fistulae), 0.05 considering the theft syndrome (15 cohorts; n > 2543 fistulas), 0.24 for thrombosis (26 cohorts, n = 4232 fistulas), and 0.03 for venous hypertension (1 cohort, n = 350 fistulas) [6].
To reduce complication rates with AVF, chronic renal patients perform self-care actions directed at the access. Dorothea Orem defines self-care as the maintenance of practices developed by an individual for his benefit to maintain life, health, and well-being. Correctly performed activities assist in structural and functional maintenance [7].
Despite that, many patients are unaware of the care that the AVF needs and, therefore, they don’t practice it correctly. In this context, the nurses’ educational interventions with renal patients may be a resource for the maintenance of self-care behaviors with the fistula [8,9].
One research study identified ‘teaching’ interventions that promote self-care (behavior) with AVF. However, other studies that explore the self-care actions required to maintain AVF are needed. It is important to know the AVF maintenance care that is required to plan educational actions directed at the renal patient audience, one that addresses correct self-care actions the patients should implement. Thus, this study aims to identify self-care actions for the maintenance of AVF of renal patients.
2. Method
2.1. Design
The study used the integrative review method. This type of study is a broad literature review aimed to subsidize discussions about the methods and results of research in a systematic and organized way [10].
Following PRISMA guidelines, the study adhered to the steps described by Whittemore and Knafl (2005) [10] in its development: 1) identification of the problem or a well-specified review purpose; 2) identification of a well-defined search strategy and actual literature search; 3) evaluation of the data’s collected quality; 4) data analysis through unbiased interpretation or synthesis of the evidence, and 5) data presentation.
2.2. Search strategy
The following guiding question was formulated based on the PICO strategy: What are the self-care actions necessary to maintain the AVF? The PICO strategy stands for Population, Intervention, Comparison, and Outcomes and can be used to construct research questions of different natures, enabling the researcher to find the best available scientific evidence accurately and quickly [11]. In this study, the population is represented by the renal patient, the intervention is the self-care actions with AVF and the outcome is the maintenance of the fistula. It is noteworthy that the presence of Comparison is not mandatory in the PICO strategy.
The data collection occurred in August and September 2018. An online indexed article search was conducted on the following databases: Medline/PubMed, Scopus, CINAHL, LILACS, BDENF and SciELO Library. To that end, we used Descriptors in Health Sciences -- DeCS/MeSH and their respective translations in Portuguese and Spanish: Renal insufficiency, Chronic/Insuficiência Renal Crônica/Insuficiencia Renal Crónica; Arteriovenous Fistula/Fístula Arteriovenosa/Fístula Arteriovenosa; Self Care/Autocuidado/Autocuidado/Knowledge/Conhecimento/Conocimiento. Crosses were performed using the Boolean operator “AND” as follows: 1) Renal insufficiency, chronic AND Arteriovenous fistula, AND Selfcare AND Knowledge; 2) Renal insufficiency, chronic AND Arteriovenous fistula, AND Selfcare; 3) Renal insufficiency, chronic AND Arteriovenous fistula; 4) Arteriovenous fistula AND Selfcare; 5) Arteriovenous fistula AND Knowledge.
To guarantee the uniform search of the databases, the search was carried out by two researchers independently, after defining the standard sequence for use of the descriptors and their combinations.
2.3. Inclusion criteria
Criteria for articles to be included in this study were that they be full text available free of charge, written in the Portuguese, English, or Spanish language, published in the last five years, and that they answer the research question. The temporal cut was defined to enable the search for updated evidence about the actions of self-care with the AVF. We excluded reflection articles, theses, dissertations, non-scientific newspaper editorials, and research studies that did not follow the methodological rigor.
2.4. Data extraction
A validated instrument [12] was used to retrieve data contained in the sample, which defined the following data collection: research authors, location of study, year and country where conducted, level of evidence, objective, results and main conclusions of the study.
2.5. Validity assessment
The methodological rigor was verified in the third stage of this study, through the application of the Critical Appraise Skills Program (CASP) [13], adapted to fit all the study designs of the articles in the final sample. This checklist consists of ten questions, so that, when evaluated, the study acquires a score of 0–10 points and is classified in two categories: 1) level A (6–10 points), which represents studies with good methodological quality reduced bias, and 2) level B (up to 5 points), that includes studies with satisfactory methodological quality, but present increased bias risk. Articles classified in level B were excluded from the sample.
The evidence level of the articles was evaluated according to the classification proposed by Fineout-Overholt et al. (2010) [14], which establishes seven categories, according to the article’s methodological approach. They are: level I - Evidence from systematic reviews or relevant clinical trials meta-analysis; Level II - Evidence derived from at least one well-delineated randomized controlled trial, moderate evidence; level III - Well delineated clinical trials without randomization; Level IV - well-delineated cohort and case-control studies; level V - Systematic review of descriptive and qualitative studies, weak evidence; level VI - Evidence derived from a single descriptive or qualitative study; level VII - Authorities’ opinion or expert committees report [14].
2.6. Data analysis
The data analysis was conducted using the software IRAMUTEQ (Interface R pour lês Analyses Multidimensionnelles de Textes et de Questionnaires). The IRAMUTEZ is free of charge and enables textual analysis [15].
The software analysis allowed the text compilation of the results and conclusions of the selected articles, their codification by command lines, the gathering and organization in a single corpus for submission to IRAMUTEQ. This stage allowed the thematic classification of the results according to the evaluation and comparison of the studies that composed the sample, performed through CHD.
3. Results
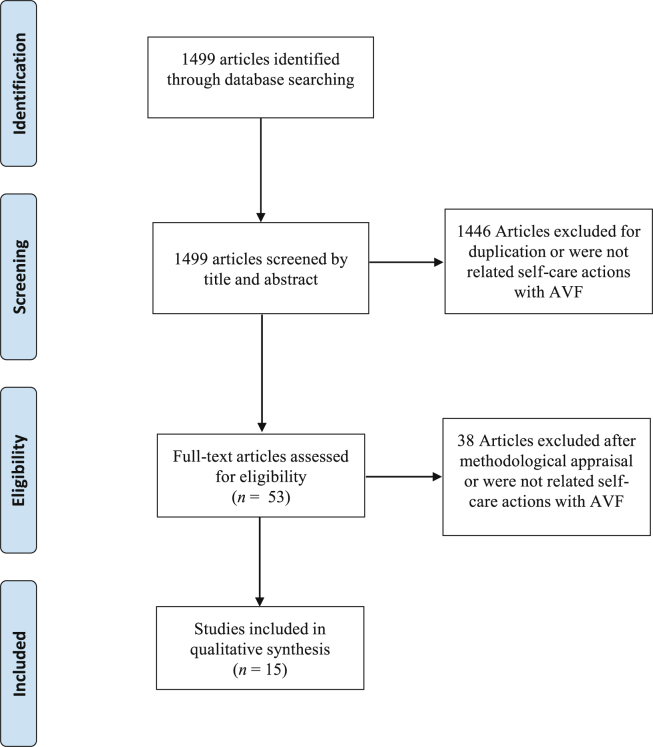
The initial databases search identified 1499 articles, of which 1428 were ruled out after careful reading of the titles and abstracts. This resulted in the selection of 71 articles. Among these, 16 were duplicates, leaving 53 articles to be fully read. After reading the articles, 17 were identified as complying with the inclusion and exclusion criteria. After the CASP application, 2 articles were excluded from the final sample because they were classified as Level B studies; that is, they presented satisfactory methodological quality but have increased bias risk. The selection process is described in Fig. 1.
Fig. 1.
Flow chart of studies selection process.
The 15 articles that comprised the final sample were published between 2013 and 2018. Most of them were conducted in Brazil [9,[16], [17], [18], [19]] and were available in English [8,[19], [20], [21], [22], [23], [24], [25], [26], [27], [28]] and in medical journals [8,19,[21], [22], [23], [24], [25], [26], [27], [28]].
Characterization of the sample articles, regarding the objective, study design, sample, evidence level and main results is described in Table 1, Table 2, Table 3.
Table 1.
Intervention studies included in the review.
| Author/year | Purpose | Sample/Intervention | Self-care actions with AVF | Results | Evidence level |
|---|---|---|---|---|---|
| Fontseré et al., 2016 [21] | To determine whether a postoperative ambulatory controlled exercise program can increase AVF maturation at 1 month | 31 patients in exercise group (elbow flexion-extension and wrist and open-closed hand) and 38 in control group |
|
The exercise group showed greater clinical, but not ultrasonographic significance, maturation (OR 5.861, 95% CI: 1.006–34.146 and OR 2.403, 0.66–8.754) | II |
| Kong; Lee; Jang, 2014 [22] | To compare the effect of two different hand exercises on hand strength and vascular maturation in patients who underwent AVF surgery | 10 patients in the first group (manual grip for exercise with GD Grip) and 8 in the second group (soft-ball exercises) |
|
Cephalic vein size and blood flow volume were also significantly increased in both groups (P = 0.005 and 0.017 for the GD Grip/P = 0.024 and 0.018 for the soft-ball). | II |
| Barbosa et al., 2018 [19] | To evaluate the efficacy of blood flow restriction training on vessel diameter and flow, muscular strength and forearm circumference in chronic renal patients before AVF creation | 12 patients in blood flow restriction training group and 14 in group without blood flow restriction training |
|
An increase in the diameter of the cephalic vein in the 2 cm (P = 0.008) and 10 cm segments (P = 0.001) was observed in the control group. | II |
| Liu et al., 2016 [26] | To investigate the effects of a knowledge-attitude-behaviour health education model on acquisition of disease-related knowledge and self-management behavior by patients undergoing maintenance hemodialysis | 43 patients in control group (usual care and general education models) and 43 in intervention group (health education model based on attitude, knowledge and behavior) |
|
Self-management behavior scores (correct fistula care) for intervention group were also higher than those for control group (P < 0.001). | II |
| Salimi et al., 2013 [27] | To compare simple exercise to the supervised structured isometric exercise with tourniquet programme on the maturation of brachiocephalic fistulas | 25 patients in first group (simple exercises with hands) and 25 patients in second (structured isometric exercises program) |
|
The number of patients who had clinically mature AVFs in case group was significantly more than control group (13 vs. 5; P = 0.008). | II |
| Uy et al., 2013 [28] | To assess whether or not an exercise intervention may increase venous size and allow AVF placement in patients who were not AVF candidates because of small vein size | 15 renal patients, performed daily gripping exercises on chosen access arm for fistula and the arm not exercised as control |
|
Isometric handgrip exercises resulted in a significant increase in proximal (P = 0.031) and distal (P = 0.011) cephalic vein diameter after four weeks in access arm. In non-exercised arm, an increase was also observed increase in the proximal (P = 0.004) and distal (P = 0.002) cephalic vein diameter in the same period. | III |
Note: AVF, arteriovenous fistula.
Table 2.
Observational studies included in the review.
| Author/year | Purpose | Study Design/Sample | Self-care actions with AVF | Results | Evidence level |
|---|---|---|---|---|---|
| Clementino et al., 2018 [16] | To investigate the knowledge of patients with chronic renal disease on self-care with AVF | Quantitative, cross-sectional, descriptive-exploratory study/32 patients |
|
Of the 24 questions, the score of correct answers varied between 15 (62.5%) and 24 (100%) and 81.2% of the patients had a score greater than or equal to 20 correct answers | VI |
| Roso et al., 2015 [17] | To describe the limits and possibilities of self-care for people who are in conservative treatment of chronic renal failure | Qualitative, descriptive and exploratory study/15 people on conservative treatment |
|
The study showed the following categories: the progress of the disease and its repercussions; the expression of autonomy; the support of family members to take care of themselves. | VI |
| Moreira et al., 2013 [18] | To Identify the customer care on hemodialysis treatment with the puncture site for the preservation of AVF | Qualitative, descriptive-exploratory study/17 clients with chronic kidney disease |
|
The study showed that patients claim to know the care for the AVF preservation. However, not all extensive home care is followed by the majority. | VI |
| Pessoa et al., 2015 [9] | To identify the knowledge, attitude and practice in self-care patients receiving dialysis with AVF | Descriptive, cross-sectional and quantitative study/30 renal patients on hemodialysis |
|
97.7% of patients had inadequate knowledge; The attitude was adequate in 70% of those who responded the survey; The self-care practice with the fistula was inadequate in 97.7% of patients. | VI |
| Sousa et al., 2018 [23] | To compare self-care behaviors for vein preservation by patients followed-up or not by the nephrologist in predialysis | Prospective, observational and comparative study/145 renal disease patients |
|
Patients who were not followed-up by the nephrologist exhibited a higher frequency of self-care behaviors than those who were followed-up (59.2% vs. 29.4%, P = 0.000) | VI |
| Adib-Hajbagheri et al., 2014 [25] | To investigate the factors correlated to the complications of vascular access site in hemodialysis patients in Isfahan Aliasghar | Cross-sectional study/110 patients undergoing hemodialysis |
|
There was a significant association between some nursing techniques including cannulation technique, being aware of the pump speed at the beginning of dialysis, and some patients’ self-care techniques including doing fistula exercising and not sleeping on the limb with fistula, and the dimensions of aneurysm. | VI |
| Ozen et al., 2017 [8] | To compare self-care behaviors for vein preservation by patients followed-up or not by the nephrologist in predialysis. | Quantitative and descriptive study/335 chronic renal patients |
|
-The rules most known and implemented self-care actions: not to measure blood pressure and draw blood from arms with fistula. -The least known and implemented self-care actions: to use blood vessels on the hands in arms without fistula for intravenous intervention and to know which situations cause hypotension. |
VI |
Note: AVF, arteriovenous fistula.
Table 3.
Methodological studies included in the review.
| Author/year | Purpose | Study Design/Sample | Self-care actions with AVF | Results | Evidence level |
|---|---|---|---|---|---|
| Sousa et al., 2015b [24] | To describe the process of building a rating scale of self-care behaviors anticipatory to creation of AVF and its validation in patients with renal disease | Methodological study/12 judges (content validation) and 90 patients with end-stage renal disease (construct validation) |
|
A principal component analysis confirmed the univariate structure of the scale (KMO = 0.759, Bartlett’s sphericity test-approximate v2 142.201, P < 0.000). Cronbach’s α is 0.831, varying between 0.711 and 0.879. | VI |
| Sousa et al., 2015a [20] | To describe the process of building a scale of assessment of self-care behaviors with AVF in hemodialysis | Methodological study/12 judges (content validation) and 218 end-stage renal disease patients (construct validation) |
|
The scale revealed properties that allow its use to assess the self-care behaviors of patients on hemodialysis in the maintenance and upkeep of AVF (Cronbach’sαvalue of 0.722). | VI |
Note: AVF, arteriovenous fistula.
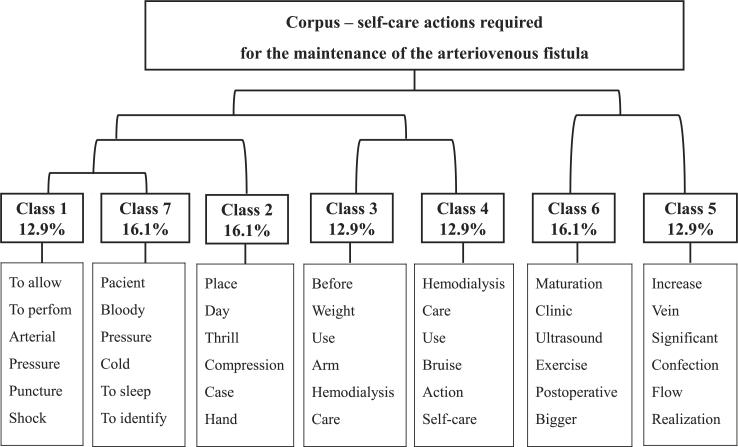
After organizing the information that addressed the guiding question of this research in a textual corpus titled “self-care actions necessary for AVF maintenance” and its analysis by the IRAMUTEQ software, 7 classes of self-care actions emerged.
Initially, the corpus was divided into two subcorpus: left and right corpus. Afterward, the right subcorpus was subdivided, giving rise to classes 6 and 5. The left subcorpus presented/displayed four new divisions giving origin to the other classes. The representation of these divisions and class formation from descending hierarchical classification (DHC) is demonstrated in a dendrogram shown in Fig. 2.
Fig. 2.
Dendogram resulting from descending hierarchical classification corpus “self-care actions required for the maintenance of the arteriovenous fistula".
It should be noted that, upon reading the text sequences assigned to each class, the need to perform some groupings emerged because of the similarity of themes among the different classes. Classes 1, 3 and 7 refer to the care needed to maintain the AVF functionality and, therefore, were grouped to form the category named “Self-care actions aimed at preserving AVF.” Classes 2 and 4 addressed self-care actions that should be performed to prevent or monitor AVF-related complications and were grouped in the category “self-care actions for prevention and monitoring of complications with AVF” category. Classes 5 and 6 are related to actions taken during the pre, trans and postoperative periods of AVF construction and were grouped in the category “self-care actions directed to the perioperative period of AVF construction".
4. Discussion
Self-care is part of the human being’s activities, regardless of whether the person is sick or healthy. However, for sick people, disease management becomes a priority. When the illness is chronic, the management of self-care is even more important since the patient’s involvement in self-care makes him/her an active agent in his/her illness management [29].
Despite the importance of maintaining self-care actions in patients with chronic disease, studies show that renal patients develop these actions poorly [9,30,31]. Yang and co-workers [30] found that 69.9% of hemodialysis patients had a low or moderate self-care behavior with low-grade AVF, suggesting that although patients remain attentive to AVF, self-care behavior with access still needs to be improved.
Therefore, it is important to present information about AVF care to the patient in a structured and systematic way. Also, it is necessary to understand the importance of maintaining adequate self-care behavior to verify, maintain and preserve vascular access functionality [8].
The important care that the patient on AVF maintenance needs to develop was identified in this study. This care will be discussed according to the classes identified as a result of the research analysis.
4.1. Self-care actions aimed at AVF preservation
Class 1 presented 42% of the text segments analyzed and it refers to actions that should not be developed or allowed by the client in order to avoid compromising access functionality. These actions were evidenced in several articles [8,9,16,17,25,26,28].
Venous punctures on the arm with AVF for blood collection or drug infusion are actions to avoid [8,9,25,26,28]. It is important that these procedures not be performed on the arm with AVF because of the risk of local hematoma formation. However, if it occurs, even while on access use during dialysis, the patient should be taught to administer cold compresses on the first 24 h of hematoma formation and warm ones after that period [32].
Blood pressure checking and carrying excess weight on the arm with AVF [8,9,17,25,26,28] were also cited as actions to be avoided by the patient. Ozen et al. (2017) [8] identified that such care was among the actions most known to HD renal patients (96.4% and 93.1%, respectively).
Another caution is to not lie down over the arm with AVF [17,25]. A study in Iran with 110 hemodialysis patients demonstrated that the aneurysm size of those patients that did not sleep on the fistula limb was significantly smaller than those that did. This fact emphasizes the association between quality of self-care and the aggravation of complications such as aneurysm [25].
To maintain AVF functionality, avoiding excessive fluid intake between hemodialysis sessions was a caution mentioned in two studies [9,16]. This approach aims to reduce episodes of intradialytic hypotension, which may be related to vascular access failure. Hypotension diagnosis in hemodialysis is based on the patient’s clinical history of systolic blood pressure lower than 90 mmHg during dialysis [33].
4.2. Self-care actions for prevention and monitoring of complications with AVF
In class 2, which presented 29% of the text sequences, the objective of access care was to prevent or identify complications with the AVF [9,16,18,20,26]. Therefore, the fistula limb must be examined regularly through an approach that allows the patient to “see, hear and feel” the arteriovenous access [34].
Among the complications that can be signaled from an AVF examination is thrombosis. It should be noted that, often, its first signs of erythema and tenderness are not specific. Early identification is essential since thrombosis is a medical emergency which requires an immediate physical and ultrasound AVF examination with the objective of saving arteriovenous access and avoiding catheters use [34].
One care action cited was the observation for bleeding in the AVF [16,20]. Hemorrhage, in this case, is a complication for the renal patients. In case of hemorrhage, the AVF site must be compressed and emergency assistance should be requested immediately. Besides, it is important to consider situations that represent risks for access rupture and consequent hemorrhage such as aneurysms presence in fistula, which should be monitored by periodically measuring its dimensions. Another factor that requires monitoring is necrotic skin presence at puncture sites associated with infection [34].
About AVF infection monitoring, Sousa and collaborators (2015) [20] identified the need to observe for the presence of redness and swelling at puncture sites. Although AVF is associated with lower infection rates when related to prostheses or catheters [35], a high incidence of this event is still observed. A systematic review reported a median rate of total infections of 0.11 per 1000 patient-days [6]. This fact reinforces the importance of patient monitoring for signs that show the presence of this complication.
Furthermore, regarding AVF care, it has been observed that infection control rules are little known and implemented by hemodialysis patients [8]. In addition to monitoring, the patient should perform self-care actions to prevent infection, such as washing the fistula arm with soap and water before the HD session, an action that can be neglected by the patient. The study of Pessoa et al. (2015) identified that 73.3% of patients knew this care and only 20% of them did it [9].
It is important to point out that adequate maintenance of self-care actions occurs along with the presentation of information in a structured and systematic way that enables patients to understand the importance of developing these actions [8].
As for hematoma care, it is recommended that cold compresses be applied in the first 24 h after the intercurrence, and warm compresses from that period onward [9,18,20]. Carrying out this care correctly is essential, as it assists in the reduction of the hematoma which may promote thrombus formation at the AVF site [36].
Surveillance for signs of the Steal Syndrome was another care cited in articles [8,20]. The clinical symptoms of BSS due to the AVF presence result from the arterial ischemia, causing pallor, fatigue, and cooling of the arm with AVF extremities. Also, limb pain may be present, which may appear only during the HD session or when the access is not in use. When pain reports occur during AVF resting and when trophic lesions are evident, surgical treatments are necessary [37].
Still, in complications monitoring, three studies identified the skin thrill check as a self-care activity with fistula [9,16,20]. The tremor evaluation consists of an important sign indicating AVF functioning and should be continuous and palpable along the vein, with more intensity in the anastomosis region [38].
Despite the importance of all self-care actions for the prevention and monitoring of AVF complications, a study that applied a scale of self-care behaviors with fistula showed that only 63.9% of patients developed these behaviors [31].
4.3. Self-care actions in the perioperative period of AVF preparation
This class presented 29% of the follow-up texts, and included the care needed before the construction of the vascular access and in the post-surgical phase [9,19,[21], [22], [23], [24],27,28]. During the preoperative AVF preparation, the aim of self-care is to preserve vascular network. For this purpose, the patient should be instructed not to allow venous punctures or blood pressure measurement on the arm where the access will be produced, and to protect the limb from blows and shocks [23,24].
Also, two studies demonstrate the benefits of exercises of the arm with AVF during this preoperative period [19,28]. One study reported that individuals with advanced chronic kidney disease that conducted four weeks of manual gripping exercises of the arm to have the AVF had a significant increase of the vein size which enabled an increase in the number of sites eligible for the construction of the vascular access [28].
Barbosa and collaborators [19] developed an exercise program and applied it to two groups (control and intervention). The patients in the intervention group performed the activities with the proposed arm with AVF under blood flow restriction. The patients in the control group performed the same exercises. However, the arm proposed for the AVF did not have the blood flow restriction. An increase in cephalic vein diameters was found in both groups, and no significant differences were found between the groups. However, the study reported that flow restriction promoted a significant increase in radial artery diameters compared to the unrestricted group.
Renal patients should continue the exercises with the arm with AVF because of its benefits observed during fistula maturation [21,22,27]. The use of regular exercise programs can significantly increase cephalic vein size and blood flow volume [22]. In addition, it is significantly related to greater clinical maturation when compared to patients who do not follow a regular exercise program [21].
Additionally, hand exercises using an arm tourniquet during the postoperative period of AVF production affect most of the ultrasound parameters associated with its maturity and may be beneficial for accelerating its clinical maturation [27].
Besides the practice of exercises during the maturation period, the patient must be attentive to care of the surgical dressing. In the Pessoa and Linhares’ (2015) [9] study, the care “to observe if the coverage is too tight” was not mentioned by any patient, while the need to keep the coverage clean and dry was mentioned by only 23.3% of participants [9].
It should be emphasized that preoperative evaluation of AVF confection should be a routine tool and the continuing education process of all those involved in AVF care, including patients and their families, is considered essential [39]. Thus, this moment could be a space for guidance about care during the postoperative period of fistula construction.
The self-care actions to maintain the FAV functionality identified in this study can guide a care policy to be implemented by nurses. The creation of protocols that help to identify problems related to self-care actions subsidize the development of educational actions aimed at the renal patient, favoring the maintenance of adequate practices with their access.
The usefulness of self-care actions for the preservation of AVF described in this review was made possible by the methodological quality of the studies that composed it and by the presence of experimental and quasi-experimental studies in the sample [19,21,22,[26], [27], [28]]. The studies provided data of significantly effective self-care actions to maintain the fistula. Moreover, in two studies that aimed to construct and validate scales to assess self-care with AVF [20,24], the items were based on extensive research, which contributed to the emergence of important self-care actions for the AVF preservation.
4.4. Limitation and implication for future study
The studies that made up this review were mostly descriptive. The only level II research found verified the effectiveness of exercises with the fistula arm at the pre- and postoperative periods of preparation. Because of that, further studies with high levels of evidence that identify self-care actions with AVF and factors involved in its implementation need to be performed.
5. Conclusion
The results of this review allowed us to identify important care for the maintenance of the AVF functionality, which were categorized in three situations. First, we identified actions that should be avoided in the preservation of the AVF, such as checking blood pressure, performing punctures, sleeping over the arm, carrying excessive weight, and drinking excess fluids. Then, attitudes for the prevention and monitoring of complications with AVF were identified, where the care involved the steal syndrome surveillance, and the observation for hemorrhage, thrombosis, and infections. Also, measures for infection prevention and treatment of hematomas were discussed.
Finally, self-care actions at the pre- and postoperative periods of AVF construction included vascular network preservation and fistula arm exercises before and after vascular access. Also addressed in this category, was the care with the surgical dressing.
Funding
This work was supported by the National Council for Scientific and Technological Development in Brazil.
CRediT authorship contribution statement
Natália Ramos Costa Pessoa: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing, Visualization. Laís Helena de Souza Soares Lima: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing. Gutembergue Aragão dos Santos: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Cecília Maria Farias de Queiroz Frazão: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Funding acquisition. Clemente Neves Sousa: Conceptualization, Methodology, Writing - review & editing, Supervision. Vânia Pinheiro Ramos: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing, Supervision.
Declaration of competing interest
No conflict of interest is declared by the authors.
Acknowledgments
We thank the Federal University of Pernambuco for the subsidies that allowed the broad search in the literature carried out in this research.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.06.007.
Contributor Information
Natália Ramos Costa Pessoa, Email: nataliarcpessoa@gmail.com.
Cecília Maria Farias de Queiroz Frazão, Email: ceciliamfqueiroz@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Mills K.T., Xu Y., Zhang W., Bundy J.D., Chen C.S., Kelly T.N. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88(5):950–957. doi: 10.1038/ki.2015.230. https://www.ncbi.nlm.nih.gov/pubmed/26221752 Available in: Access in 3 Out. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomé F.S., Sesso R.C., Lopes A.A., Lugon J.R., Martins C.T. Brazilian chronic dialysis survey 2017. Brazilian Journal of Nephrology. 2019;41(2):208–214. doi: 10.1590/2175-8239-jbn-2018-0178. Epub 2019/03/28. Available in: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lok C.E. KDOQI Clinical practice guideline for vascular access: 2019 update. Am J Kidney Dis. 2020;75(4):S1–S164. doi: 10.1053/j.ajkd.2019.12.001. https://www.ajkd.org/article/S0272-6386(19)31137-0/fulltext suppl 2. Available in: Access in: 10 Jan 2020. [DOI] [PubMed] [Google Scholar]
- 4.Robinson B.M., Akizawa T., Jager K.J., Kerr P.G., Saran R., Pisoni R.L. Factors affecting outcomes in patients reaching end-stage kidney disease worldwide: differences in access to renal replacement therapy, modality use, and haemodialysis practices. Lancet. 2016;388(10041):294–306. doi: 10.1016/S0140-6736(16)30448-2. https://www.sciencedirect.com/science/article/pii/S0140673616304482 Available in: Access in 26 Jul. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ravani P., Palmer S.C., Oliver M.J., Quinn R.R., MacRae J.M., Tai D.J. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol. 2013;24(3):465–473. doi: 10.1681/ASN.2012070643. https://jasn.asnjournals.org/content/24/3/465.short Available in: Access in: 30 Jul. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Jaishi A.A., Liu A.R., Lok C.E., Zhang J.C., Moist L.M., Al-Jaishi A.A. Complications of the arteriovenous fistula: a systematic review. J Am Soc Nephrol. 2016;28(6):1839–1850. doi: 10.1681/ASN.2016040412. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5461784/ Available in: Access in 3 Out. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orem D.E. 6 th. Mosby Year Book Inc; St Louis (USA): 2001. Nursing: concepts of practice. [Google Scholar]
- 8.Ozen N., Tosun N., Cinar F.I., Bagcivan G., Yilmaz M.I., Askin D. Investigation of the knowledge and attitudes of patients who are undergoing hemodialysis treatment regarding their arteriovenous fistula. J Vasc Access. 2017;18(1):64–68. doi: 10.5301/jva.5000618. http://journals.sagepub.com/doi/abs/10.5301/jva.5000618 Available in: Access in 8 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 9.Pessoa N.R.C., Linhares F.M.P. Hemodialysis patients with arteriovenous fistula: knowledge, attitude and practice. Escola Anna Nery. 2015;19(1):73–79. https://www.ingentaconnect.com/content/doaj/14148145/2015/00000019/00000001/art00012 Available in: Access in 05 Jul. 2018. [Google Scholar]
- 10.Whittemore R., Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2648.2005.03621.x Available in: Access in: 04 Set. 2018. [DOI] [PubMed] [Google Scholar]
- 11.Santos C.M.C., Pimenta C.A.M., Nobre M.R.C. The PICO strategy for the research question construction and evidence search. Rev. Lat. Am. Enfermagem. 2007;15(3):508–511. doi: 10.1590/s0104-11692007000300023. http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext Available in: Access in: 05 Out. 2018. [DOI] [PubMed] [Google Scholar]
- 12.Ursi E.S., Galvão C.M. Perioperative prevention of skin injury: an integrative literature review. Rev. Lat. Am. Enfermagem. 2006;14(1):124–131. doi: 10.1590/s0104-11692006000100017. http://www.scielo.br/pdf/rlae/v14n1/v14n1a17.pdf Available in: Access in 30 Set. 2018. [DOI] [PubMed] [Google Scholar]
- 13.Programme C.A.S.P. 2013. Critical appraisal Skills (CASP). 10 quest. To help you make sense a rev.http://media.wix.com/ugd/dded87_ebad01cd736c4b868 Access in 28 Set. 2018. [Google Scholar]
- 14.Fineout-Overholt E., Melnyk B.M., Stillwell S.B., Williamson K.M. Evidence-based practice step by step: critical appraisal of the evidence: part I. AJN The American Journal of Nursing. 2010;110(7):47–52. doi: 10.1097/01.NAJ.0000383935.22721.9c. https://journals.lww.com/ajnonline/Fulltext/2010/07000/Evidence_Based_Practice_Step_by_Step__Critical.26.aspx Available in. Access in: 12 Set. 2018. [DOI] [PubMed] [Google Scholar]
- 15.Camargo B.V., Justo A.M. IRAMUTEQ: a free software for analysis of textual data. Temas em psicologia. 2013;21(2):513–518. http://pepsic.bvsalud.org/scielo.php?pid=S1413-389X2013000200016&script=sci_abstract&tlng=es Available in: Access in: 22 Dez 2018. [Google Scholar]
- 16.Clementino D.C., Souza A.M.Q., Barros D.C.C., Carvalho D.M.A., Santos C.R., Fraga S.N. Hemodialysis patients: the importance of self-Care with the arteriovenous fistula. Journal of Nursing UFPE on line. 2018;12(7):1841–1852. https://periodicos.ufpe.br/revistas/revistaenfermagem/article/view/234970 Available in: Access in: 10 Ago. 2018. [Google Scholar]
- 17.Roso C.C., Beuter M., Jacobi C.S., Pauletto M.R., Timm A.M.B., Silva C.T. Taking care of yourself: limits and possibilities in the conservative treatment of chronic renal failure. Journal of Nursing UFPE on line. 2015;9(2):617–623. https://periodicos.ufpe.br/revistas/revistaenfermagem/article/view/10380 Available in: Access in 12 Ago. 2018. [Google Scholar]
- 18.Moreira A.G.M., Araújo S.T.C., Torchi T.S. Preservation of arteriovenous fistula: conjunct actions from nursing and client. Escola Anna Nery Revista de Enfermagem. 2013;17(2):256–262. http://www.redalyc.org/pdf/1277/127728367008.pdf Available in: Access in 10 Ago. 2018. [Google Scholar]
- 19.Barbosa J.B., Maia T.O., Alves P.S., Bezerra S.D., Moura E.C., Medeiros A.I.C. Does blood flow restriction training increase the diameter of forearm vessels in chronic kidney disease patients? A randomized clinical trial. J Vasc Access. 2018;19(6):626–633. doi: 10.1177/1129729818768179. http://journals.sagepub.com/doi/abs/10.1177/1129729818768179 Available in: Access in 12 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 20.Sousa C.N., Apóstolo J.L.A., Figueiredo M.H.J.S., Dias V.F.F., Teles P., Martins M.M. Construction and validation of a scale of assessment of self-care behaviors with arteriovenous fistula in hemodialysis. Hemodial Int. 2015;19(2):306–313. doi: 10.1111/hdi.12249. https://onlinelibrary.wiley.com/doi/abs/10.1111/hdi.12249 Available in: Access in 17 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 21.Fontseré N., Mestres G., Yugueros X., López T., Yuguero A., Bermudez P. Effect of a postoperative exercise program on arteriovenous fistula maturation: a randomized controlled trial. Hemodial Int. 2016;20(2):306–314. doi: 10.1111/hdi.12376. https://onlinelibrary.wiley.com/doi/abs/10.1111/hdi.12376 Available in: Access in: 15 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 22.Kong S., Lee K.S., Kim J., Jang S.H. The effect of two different hand exercises on grip strength, forearm circumference, and vascular maturation in patients who underwent arteriovenous fistula surgery. Ann Rehabil Med. 2014;38(5):648–657. doi: 10.5535/arm.2014.38.5.648. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4221393/ Available in: Access in: 11 Ago. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sousa C.N., Ligeiro I., Teles P., Paixão L., Dias V.F., Cristovão A.F. Self-care in preserving the vascular network: old problem, new challenge for the medical staff. Ther Apher Dial. 2018;22(4):332–336. doi: 10.1111/1744-9987.12664. https://onlinelibrary.wiley.com/doi/abs/10.1111/1744-9987.12664 Available in: Access in: 13 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 24.Sousa C.N., Figueiredo M.H., Dias V.F., Teles P., Apóstolo J.L. Construction and validation of a scale of assessment of Self care behaviours anticipatory to creation of arteriovenous fistula. J Clin Nurs. Jan. 2019;2015(24) doi: 10.1111/jocn.12970. https://onlinelibrary.wiley.com/doi/abs/10.1111/jocn.12970 23-24), 3674–80. Available in. Access in: 13 Ago. 2018. 28;issue=2;spage=313;epage=317;aulast=Manne. Access in: 15 de. [DOI] [PubMed] [Google Scholar]
- 25.Adib-hajbagheri M., Molavizadeh N., Alavi N.M., Abadi M.H.M. Factors associated with complications of vascular access site in hemodialysis patients in Isfahan Aliasghar hospital. Iran J Nurs Midwifery Res. 2014;19(2):208–215. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4020033/ Available in: Access in 19 Ago. 2018. [PMC free article] [PubMed] [Google Scholar]
- 26.Liu L., Liu Y.P., Wang J., An L.W., Jiao J.M. Use of a knowledge-attitude-behaviour education programme for Chinese adults undergoing maintenance haemodialysis: randomized controlled trial. J Int Med Res. 2016;44(3):557–568. doi: 10.1177/0300060515604980. http://journals.sagepub.com/doi/abs/10.1177/0300060515604980 Available in: Access in: 6 Ago. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salimi F., Nassiri G.M., Moradi M., Keshavarzian A., Farajzadegan Z., Saleki M. Assessment of effects of upper extremity exercise with arm tourniquet on maturity of arteriovenous fistula in hemodialysis patients. J Vasc Access. 2013;14(3):239–244. doi: 10.5301/jva.5000123. http://journals.sagepub.com/doi/abs/10.5301/jva.5000123 Available in. Access in: 16 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 28.Uy A.L., Jindal R.M., Herndon T.W., Yuan C.M., Abbott K.C., Hurst F.P. Impact of isometric handgrip exercises on cephalic vein diameter in non-AVF candidates, a pilot study. J Vasc Access. 2013;14(2):157–163. doi: 10.5301/jva.5000116. http://journals.sagepub.com/doi/abs/10.5301/jva.5000116 Available in: Access in: 18 Ago. 2018. [DOI] [PubMed] [Google Scholar]
- 29.Riegel B., Jaarsma T., Strömberg A. A middle-range theory of self care of chronic illness. Adv Nurs Sci. 2012;35(3):194–204. doi: 10.1097/ANS.0b013e318261b1ba. https://journals.lww.com/advancesinnursingscience/Abstract/2012/07000/A_Middle_Range_Theory_of_Self_Care_of_Chronic.3.aspx Available in: Access in: 11 Jan. 2019. [DOI] [PubMed] [Google Scholar]
- 30.Yang M.M., Zhao H.H., Ding X.Q., Zhu G.H., Yang Z.H., Ding L. Self-care behavior of hemodialysis patients with arteriovenous fistula in China: a multicenter, cross-sectional study. Ther Apher Dial. 2019;23(2):167–172. doi: 10.1111/1744-9987.12770. https://onlinelibrary.wiley.com/doi/full/10.1111/1744-9987.12770 Available in: Access in: 12 Jan. 2019. [DOI] [PubMed] [Google Scholar]
- 31.Sousa C.N., Marujo P., Teles P., Lira M.N., Novais M.E.L.M. Self-care on hemodialysis: behaviors with the arteriovenous fistula. Ther Apher Dial. 2017;21(2):195–199. doi: 10.1111/1744-9987.12522. https://onlinelibrary.wiley.com/doi/full/10.1111/1744-987.12522 Disponível em: Access in: 11 Jan.2019. [DOI] [PubMed] [Google Scholar]
- 32.Ramalho Neto J.M., Rocha E.R.S., Almeida A.R.M., Nóbrega M.M.L. Arteriovenous fistula in chronic renal patients perspective. Enferm. Foco. 2016;7(1):37–41. http://revista.portalcofen.gov.br/index.php/enfermagem/article/viewFile/663/282 Available in: Access in:13 Jan. 2019. [Google Scholar]
- 33.Manne V., Vaddi S.P., Reddy V.B., Dayapule S. Factors influencing patency of Brescia-Cimino arteriovenous fistulas in hemodialysis patients. Saudi J Kidney Dis Transpl. 2017;28(2):313–317. doi: 10.4103/1319-2442.202759. http://www.sjkdt.org/article.asp?issn=1319-2442 Available in: year=2017;volume= [DOI] [PubMed] [Google Scholar]
- 34.Almasri J., Alsawas M., Mainou M., Mustafa R.A., Wang Z., Woo K. Outcomes of vascular access for hemodialysis: a systematic review and meta-analysis. J Vasc Surg. 2016;64(1):236–243. doi: 10.1016/j.jvs.2016.01.053. https://www.sciencedirect.com/science/article/pii/S0741521416002160 Available in: Access in 14 Jan. 2019. [DOI] [PubMed] [Google Scholar]
- 35.Neves Junior M.A., Petnys A., Melo R.C., Rabboniu E. Acesso vascular para hemodiálise: O que há de novo? J Vasc Bras. 2013;12(3):221–225. http://www.scielo.br/pdf/jvb/v12n3/1677-5449-jvb-12-03-00221.pdf Available in: Access in:23 Dez. 2018. [Google Scholar]
- 36.González-Fajardo J.A., Sanz J.B., del Río Solá L., Pedrosa M.M., Calavia Á.R., Puerta C.V. Síndrome isquémico de la mano secundario a Acceso vascular para hemodiálisis. Estrategias terapéuticas. Angiologia. 2016;68(4):311–321. https://www.sciencedirect.com/science/article/pii/S0003317015000279 Available in: Access in 10 Dez. 2018. [Google Scholar]
- 37.Sousa C.N., Apóstolo J.L., Figueiredo M.H., Martins M.M., Dias V.F. Physical examination: how to examine the arm with arteriovenous fistula. Hemodial Int. 2013;17(2):300–306. doi: 10.1111/j.1542-4758.2012.00714.x. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1542- 8.2012.00714.x Available in: Access in 13 Jan. 2019. [DOI] [PubMed] [Google Scholar]
- 38.Fila B., Ibeas J., Tey R.R., Lovčić V., Zibar L. Arteriovenous fistula for haemodialysis: the role of surgical experience and vascular access education. Nefrología (Madrid) 2016;36(2):89–94. doi: 10.1016/j.nefro.2015.07.003. http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S021169952016000200089 Available in: Access in: 22 Jan. 2019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.