Abstract
Aim
Previous research has mainly focused on the advantages of PCC and less on its disadvantages. Hence, there is a need to further explore the recent research regarding PCC from both sides. Therefore, the aim of this paper is to elucidate the advantages and disadvantages of PCC.
Design
Discussion paper.
Methods
We searched relevant literature published January 2000–March 2018 in PubMed, Medline, CHINAL, Scopus and Web of Science.
Results
The results showed that PCC can contribute to improved health and well‐being, improved mutual interaction in relationships, improved cost‐effectiveness and improved work environment, while the disadvantages can involve increased personal and financial costs, exclusion of certain groups, increased personal and financial costs, exclusion of staff's personhood and unfairness due to empathy. An analysis of the existing literature on PCC showed paradoxes, which call for further investigation.
Keywords: clinical practice, concept, evidence, healthcare, person‐centred care
1. INTRODUCTION
As a way to strengthen individual participation in health care, approaches such as family‐, child‐, patient‐ and person‐centred care have been advocated in recent decades (Coyne, Holmström, & Söderbäck, 2018). One of these, person‐centred care (PCC), has been equated with high‐quality care (Ekman et al., 2011; McCormack & McCance, 2006). PCC places the person receiving care in the centre and focuses on their needs, strengths and weaknesses. It also respects the individual's context, history and family circumstances. Instead of viewing the patient as a passive target of care, PCC views the patient as an active part in the care and decision‐making (Ekman et al., 2011; Holmström & Röing, 2010; Leplege et al., 2007). While it shares many similarities with patient‐centred care, the goal of PCC is different: rather than aiming for a functional life, it has a meaningful life as its goal (Håkansson Eklund et al., 2018). However, different contexts require different types of centredness (Hughes, Bamford, & May, 2008). As noted by Leplege et al. (2007), PCC is a diverse and multidimensional concept.
Person‐centred care is advancing internationally. During the period 2000–2011, the number of published papers employing a PCC perspective increased from three to seven per month (Olsson, Ung, Swedberg, & Ekman, 2013). However, a literature review shows that the concepts of person‐centredness and patient‐centredness are blended and applied interchangeably (Håkansson Eklund et al., 2018).
However, the trend of advocating PCC as inherently good and as a quality goal to strive for is strong. Previous research has mainly focused on the advantages of PCC and less on its disadvantages. Hence, there is a need to further explore the recent research regarding PCC from both sides. Therefore, the aim of the present discussion paper is to elucidate the advantages and disadvantages of PCC.
2. DESIGN AND METHODS
For this discussion paper, we searched for empirical studies from a PCC perspective in PubMed, Medline, CHINAL, Scopus and Web of Science, (a) peer reviewed, (b) in English and (c) published January 2000–March 2018 using the term “person‐centred/ered care” in the title. The search was extended with a citation search and footnote chasing (Kacem & Mayr, 2017). Selected literature in this paper presents PCC studies with empirical evidence (i.e. inductively) for most of the reported advantages of PCC. However, disadvantages are additionally explored using other theoretical literature (i.e. abductively). The overview of findings is shown in Table 1.
Table 1.
The outline of the advantages and disadvantages of person‐centred care in clinical settings
| Advantages of person‐centred care | Items | References |
|---|---|---|
| Improved health and well‐being |
|
Alharbi, Carlström et al. (2014); Beauchamp & Childress (2009); Edvardsson, Winblad, & Sandman (2008); Edvardsson et al. (2011); Edvardsson, Petersson, et al. (2014); Edvardsson, Sandman, et al. (2014); Ekman et al. (2011, 2012); Feldthusen et al. (2016); Fletcher (2015); Fors et al. (2015); Fors et al. (2016); Fossey et al. (2014); Halpern et al. (2004); Hansson, Olsson et al. (2016); Holburn, Jacobson, et al. (2004); Li & Porock, (2014); Parley, (2001); Ricoeur, (1992); Sharp, McAllister, & Broadbent (2016); Sloane et al., ( 2004); Wigham et al., (2008); Rosher & Robinson (2005) |
| Improved mutual interaction in the relationships |
|
Bolster & Manias, (2010); Dewing, (2004); Ekman et al., (2011); Fors et al. (2015, 2017, 2018); Gabrielsson et al. (2015); Hansson et al. (2016), Jansson et al. (2018); McCormack (2004); Ulin, Olsson, Wolf, & Ekman, (2016); Wilberforce et al. (2017); Wallström & Ekman, (2018); Wildevuur and Simonse (2015); Zoffmann et al. (2008) |
| Improved cost‐effectiveness |
|
Ekman et al., (2012); Hansson et al. (2016); Ulin et al. (2016); Wildevuur & Simonse (2015) |
| Improved work environment |
|
Barbosa, Sousa, Nolan, & Figueiredo, (2015); Brownie & Nancarrow, (2013); Edvardsson, Fetherstonhaugh, McAuliffe, Nay, & Chenco (2011); Edvardsson, Sandman, Sandman, & Borell (2014); Sjögren, Lindkvist, Sandman, Zingmark, & Edvardsson, (2014); Lehuluante et al. (2012); Vassbø et al., (2018) |
| Disadvantages of person‐centred care | ||
|
Increased personal and financial costs |
|
Blom et al. (2016); Chenoweth et al. (2009); Coleman et al. (2003); Leeuwen et al. (2015); Makai et al. (2015); Metzelthin et al. (2015); Uittenbroek et al., (2018) |
| Exclusion of certain groups |
|
O’Dwyer (2013); Britten et al. (2017). |
| Exclusion of the personhood of staff |
|
Buber, (1971); Buber & Kaufmann, (1970); Mead & Bower (2000); Kadri et al. (2018). |
| Risk for compassion fatigue |
|
Håkansson Eklund et al., (2018); Coetzee & Klopper (2010); Hansen et al., (2018); Joison, (1992). Leplege et al., (2007) |
| Unfairness due to empathy |
|
Håkansson Eklund et al., (2018); Leplege et al. (2007); Batson, (2011); Batson, Klein, Highberger & Shaw (1995); Batson, Eklund, Chermok, Hoyt, & Ortiz, (2007); Krebs, (1975) |
2.1. Ethics
Ethics approval was not required for this manuscript.
3. DISCUSSION
3.1. Advantages of PCC
Numerous studies have described the advantages of PCC, summarized as: Improved health and well‐being, Improved mutual interaction in relationships, Improved cost‐effectiveness and Improved work environment.
3.1.1. Improved health and well‐being
The ethics of PCC entail reinforcing the person's resources and retaining their independence regarding their values, freedom of choice and self‐determination. These aspects are fundamental for increasing self‐esteem and quality of life. As a result, the person will experience physical and mental well‐being, increased self‐efficacy and empowerment.
Person‐centred care highlights the importance of seeing and respecting the patient as a person – a capable human being with resources and needs (Edvardsson, Winblad, & Sandman, 2008; Ricoeur, 1992). A person has been described as someone who has the capacity for self‐consciousness (Fletcher, 2015; Ricoeur, 1992). Furthermore, PCC involves considering the person's desires, values (Halpern, Johnson, Miranda, & Wells, 2004), family and social circumstances, as well as lifestyle. The purpose is to provide better health and well‐being for patients, which is in line with ethics goals (Beauchamp & Childress, 2009).
Other positive aspects for older persons, specifically, concern freedom of choice, self‐determination and purposeful living (Li & Porock, 2014). Previous research using both qualitative (Parley, 2001) and quantitative methods (Edvardsson, Petersson, Petersson, Sjogren, Lindkvist, & Sandman, 2014; Hansson, Carlström, Olsson, Nyman, & Koinberg, 2017; Holburn, Jacobson, Schwartz, Flory, & Vietze, 2004) indicated that PCC improves quality of life, life satisfaction, (Wigham et al., 2008) and well‐being (Sharp, McAllister, & Broadbent, 2016). Other effects include patients experiencing their lives differently and having more self‐confidence (Olsson, Hansson, & Ekman, 2016). Some patients showed to be more determined in their choice and decision‐making (Rosher & Robinson, 2005; Wigham et al., 2008), while others experienced reduced fatigue and anxiety (Feldthusen, Dean, Forsblad‐d’Elia, & Mannerkorpi, 2016). Patients expressed feelings of respect and recognition of personhood (Alharbi, Carlström, Ekman, Jarneborn, & Olsson, 2014), and better functional performance was observed (Ekman et al., 2012). Inpatients described that PCC had helped them boost their self‐efficacy in controlling their chronic disease (Fors, Taft, Ulin, & Ekman, 2016) and significant improvement to their empowerment and self‐efficacy was observed (Fors et al., 2015). In patients with dementia or depression, symptoms seemed to be reduced (Fossey et al., 2014; Li & Porock, 2014; Robertson & Rosher, 2006; Sloane et al., 2004). Finally, the PCC approach seemed to reduce medication use (Fossey et al., 2014).
3.1.2. Improved mutual interaction in relationships
Person‐centred care has shown advantages in terms of improved mutual interactions. Previous studies stress the importance of interpersonal relationships in PCC for patients to thrive through equability and mutuality. A mutual relationship can lead to the development of a partnership, which includes shared decision‐making.
Caring relationships are described as essential in PCC, where interpersonal nursing takes place between patients and healthcare professionals (Gabrielsson, Sävenstedt, & Zingmark, 2015) who are authentic and present (McCormack, 2004). Consequently, the importance of partnership is emphasized (Ekman et al., 2011; Fors et al., 2015; Jansson, Fors, Ekman, & Ulin, 2018; Wallström & Ekman, 2018) and may be established even without face‐to‐face conversations and with vulnerable patient groups (Fors et al., 2018). For instance, in a literature concept synthesis Wilberforce et al. (Wilberforce et al., 2017) found that PCC encourages the caring relationship in the care of older persons. In addition, participation in PCC means that control is given back to the patient, who needs to be involved and to actively participate in their own care and treatment (Fors, Swedberg, Ulin, Wolf, & Ekman, 2017). The discharge process improved when the persons themselves were involved (Ulin, Olsson, Wolf, & Ekman, 2016) and had an opportunity to participate (Bolster & Manias, 2010). Furthermore, shared decision‐making strengthens the opportunity for persons to participate in a partnership (Dewing, 2004; Ekman et al., 2011) (Fors et al., 2017) and empowers them to solve problems (Zoffmann, Harder, & Kirkevold, 2008). PCC and treatment require a partnership approach to the patient and family members (Ekman et al., 2011) and could raise the understanding in clinical practice to create collaboration among institutions (Wallström & Ekman, 2018). PCC also helps patients improve their relationships and expand their social networks (Hansson et al., 2016; Wildevuur & Simonse, 2015).
3.1.3. Improved cost‐effectiveness
Another advantage of PCC is cost‐effectiveness. One hospital goal is to discharge patients as early as possible. Therefore, cost reduction for patients’ hospital stays and efficient time use might be a preference for healthcare organizations. A scoping review by Wildevuur and Simonse (Wildevuur & Simonse, 2015) showed that PCC information and communication technology management had an impact on five chronic diseases through decreased hospitalization and increased cost‐effectiveness. Time efficiency was another reviewed indicator, where the impact appeared to be positive but less conclusive (Wildevuur & Simonse, 2015).
Hansson et al. (2016) reported that costs for patients receiving PCC were significantly lower than for those in the conventional care group. At workplaces where PCC was fully implemented, the outcomes showed that the length of hospital stay was reduced by 2.5 days (Ekman et al., 2012). Furthermore, the improvement involved the discharge process, with increased notifications to the institution of discharge and a confirmed discharge planning conference starting sooner than in the usual care group (Ulin et al., 2016).
3.1.4. Improved work environment
Person‐centred care results in a better working environment for staff. Research indicates that burnout is highly associated with long‐term workload and stress of conscience. PCC seems to relieve staff's stress of conscience, as they are enabled to provide appropriate care.
An association has been found between person‐centredness and job satisfaction in elderly care (Barbosa, Sousa, Nolan, & Figueiredo, 2015; Brownie & Nancarrow, 2013; Edvardsson, Fetherstonhaugh, McAuliffe, Nay, & Chenco, 2011; Edvardsson, Sandman, Sandman, & Borell, 2014; Lehuluante, Nilsson, & Edvardsson, 2012; Sjögren, Lindkvist, Sandman, Zingmark, & Edvardsson, 2014; Vassbø et al., 2018) and with elderly care in an acute setting (Lehuluante et al., 2012). This could induce the importance of shifting from merely doing tasks and following organizational routines to providing PCC that promotes a good life for residents in elderly care (Edvardsson et al., 2011; Sjögren et al., 2014). Further, PCC has been shown to have a positive impact on nurses’ capacity to meet individual needs of residents in aged care (Brownie & Nancarrow, 2013).
Teamwork facilitates PCC and increases healthcare professionals’ instrumental and relational resources such as time, support and safety (Edvardsson, Sandman, et al., 2014; Sjögren et al., 2014). Working with PCC resulted in a significant reduction in healthcare professionals’ stress of conscience (Edvardsson, Sandman, et al., 2014). The effectiveness of working with PCC has shown a tendency to benefit care workers in terms of avoiding stress and burnout (Barbosa et al., 2015; Sjögren et al., 2014). PCC has further been associated with higher levels of supportive psychosocial unit climate and a higher proportion of staff with continuing education in dementia care (Sjögren et al., 2014).
3.2. Disadvantages of person‐centred care
There is less written regarding the disadvantages of PCC. A likely reason for this is that most researchers who publish in this field have a positive attitude towards PCC, with it being been stressed as ethically just and “the right thing to do” (Edvardsson, Watt, & Pearce, 2017; Ekman et al., 2011; Leplege et al., 2007; McCormack, 2004). Therefore, we had to dig deeper into the literature to find possible disadvantages. Due to this, we have used more cautious language, such as “might” and more theoretical reasoning as mentioned earlier. The possible disadvantages of PCC are as follows: Increased personal and financial costs; Exclusion of certain groups; Exclusion of staff's personhood; Risk for compassion fatigue; and Unfairness due to empathy.
3.2.1. Increased personal and financial costs
Most of the existing literature sheds light on the positive sides of the PCC approach. However, alongside the advantages, PCC is one of the reasons for patient falls in clinical settings. Implementing PCC in practice demands careful thought, especially for persons with cognitive impairment. The obvious results of falls are the “costs” generated by injuries, fractures and pain. These costs not only include suffering on the patient's part and risks to patient safety but are also felt in economic terms through increased expenses for hospital care and rehabilitation.
The increased risk of falls has been shown by Chenoweth et al. (2009) and Coleman (2003). Chenoweth et al. (2009) performed a randomized control trial where urban residential sites were randomized to PCC, dementia‐care mapping or usual care. The proportions of residents with falls were significantly higher in the PCC and usual care groups than in the dementia‐care group. Furthermore, there were also significantly more falls in the PCC group than in usual care, which was in accordance with Coleman (2003). This was due to environmental enhancements such as plants and animals. Furthermore, increased costs but no statistically significant differences in health‐associated outcomes were shown (Metzelthin et al., 2015; Uittenbroek et al., 2018). Other studies have shown no significant differences in costs and outcome between PCC and usual care (Blom et al., 2016; Leeuwen et al., 2015; Makai et al., 2015).
3.2.2. Exclusion of certain groups
There is no consensus regarding which group of patients PCC is best suited for. There is, however, a risk that it might be “too beneficial” for some but not for others. If one of the ideas is to involve those who are able to make informed decisions and actively participate in their care, there is a risk that some persons will take advantage of the situation, using their strong voice while others with weaker voices might be disadvantaged. There are also persons who do not wish to be involved in their care, regardless of the reason.
It might be difficult to operationalize and provide PCC in a consistent way; as O’Dwyer (2013) points out, PCC has been equated with a consumer‐based approach in elderly care. Investigating policy documents for Irish residential care standards, she found that PCC was portrayed as a hotel‐like service. Residents were seen as consumers with a right to autonomy and choice. This might be unsuitable for those older persons with a limited capacity to make informed decisions. Many older persons become dependent on others due to age‐related illnesses and/or impaired cognitive functions; this way of conceptualizing PCC does not account for the complexities involved in decision‐making for such older persons. Another example is found in the rehabilitation context, where the person must be an active partner in their rehabilitation. Not everyone wants, or is able, to be active in their rehabilitation (Britten et al., 2017).
3.2.3. Exclusion of staff's personhood
Usually, the focus of PCC is on the patient/person and their rights and staff and their personhood has often been neglected. This might diminish the value of the staff as autonomous persons, which in turn might result in poor working conditions and high turnover rates.
There might hence be a risk that only patients/clients are considered persons, while staff are not. Kadri et al. (2018) found that many among the care staff in dementia care were not identified by their employing institutions as persons in their own right and that there was a general lack of acknowledgement of the moral work of caring. This means that there is a risk that the complex relationships of care work are reduced to a series of tasks, which challenges care workers’ self‐worth and self‐efficacy and negatively affects the delivery of PCC. It might be demoralizing to practice PCC in such an organization. At worst, the working conditions resulted in ethical dilemmas for staff. Therefore, Kadri et al. (2018) suggest that the status of the care staff as persons should be explicitly considered in quality standards and supported by employers’ policies. This is in conjunction with Buber's work on the I–thou relation (Buber, 1971; Buber & Kaufmann, 1970). His work has most commonly been used in underscoring the need to see the patient as a “thou” rather than an “it,” but as the professional relationship is mutual – a subject‐to‐subject relationship – it is important that the professional is not reduced to an “it.” This is in line with the Mead and Bower paper on patient‐centred care (Mead & Bower, 2000), stating that “the doctor as person” is one of the core aspects of patient‐centred care. Patient‐ and person‐centred care share many features and acknowledging a subject‐to‐subject relationship is one of them.
3.2.4. Risk for compassion fatigue
There is a constant risk of healthcare staff being overloaded by duties and engagement in their patients. This increases the risk for compassion fatigue, characterized by a gradual lessening of compassion and exhaustion. Compassion fatigue includes feelings of hopelessness, constant stress and anxiety and sleeplessness or nightmares.
Compassionate care is included in the PCC approach, however, meaning a bond between the healthcare provider and the ill person (Håkansson Eklund et al., 2018). On the one hand, compassionate care is positive but on the other hand there is a risk.
Too much compassion may lead to compassion fatigue (Coetzee & Klopper, 2010; Hansen et al., 2018; Joison, 1992). Coetzee and Klopper (2010) identified risk factors, causes, processes and manifestations of compassion fatigue. It is “a state where the compassionate energy that is expended by nurses has surpassed their restorative processes” (Coetzee & Klopper, 2010). Risk factors for compassion fatigue include contact with patients and use of self. In PCC, genuine contact with patients and the use of self are definitional features. Although compassion is at the heart of all care, it is even more crucial in PCC. Therefore, the risk of compassion fatigue in PCC needs consideration (Leplege et al., 2007).
3.2.5. Unfairness due to empathy
Empathy can be described as one of the fundamental aspects of PCC and as a positive value in care. However, there is a risk when one is “too empathetic.” Showing excessive empathy to certain persons can be unjust and unfair and is against the principles of ethics, even if it is unintentional.
Previous research has described that empathy is one of the constituents of PCC (Håkansson Eklund et al., 2018). In a meta‐synthesis, Håkansson Eklund et al. (2018) found empathy to be a core component of all the synthesized review articles. For example, Leplege et al. (2007) stated that in PCC “one should listen to the person with empathy” (p. 1557).
In social psychology, there is a massive body of research showing that empathy often causes people to help others, even altruistically (Batson, 2011). However, there is also evidence from experiments that empathy‐based helping directed towards one specific individual can be unfair to others who do not receive help. There are several reasons for this. First, empathy is a powerful source of motivation, which often makes people direct their attention towards one individual while forgetting others (Batson, 2011). For example, in two experiments Batson, Klein, Highberger, and Shaw (1995) asked participants to make a decision that affected the well‐being of other people. Before making this decision, some participants were induced to feel empathy for one of the other people. Participants who were not induced to feel empathy acted fairly, while those who were induced to feel empathy acted in a partial way to benefit the person for whom they felt empathy. Second, people tend to feel more empathy for people who are similar to themselves (Krebs, 1975). Third, people tend to feel more empathy for people they like (Batson, Eklund, Chermok, Hoyt, & Ortiz, 2007). Applying these experimental results to the context of healthcare, there seems to be a risk that PCC, due to its empathic nature, tends to unfairly favour patients who happen to be within the health provider's span of attention and are similar to the health provider and whom the health provider likes.
3.3. Potential paradoxes
The aim of this discussion paper was to elucidate the advantages and disadvantages of PCC in health care. We have identified some crucial points that seem to be paradoxes. These paradoxes need further consideration among staff when choosing the PCC approach. First, while a positive aspect of PCC is the increased well‐being of and respect for the patient as a person, negative aspects include unsuitability for specific groups and increased risks of falls.
Thus, a first potential paradox is that PCC might simultaneously increase and decrease patient well‐being. Second, an advantage of PCC appears to be improved mutual interactions while a disadvantage seems to favour some patients while ignoring others, which is unfair. Thus, a second potential paradox is that PCC at the same time tends to improve and worsen interactions. Third, PCC can contribute to an improved work environment while at the same time entailing risks of excluding staff's personhood and for compassion fatigue. Therefore, a third potential paradox is that PCC tends to both improve and worsen the work environment. Fourth, PCC appears to reduce costs, while at the same time it seems that it is relatively resource‐demanding; examples of costs are the consequences of falls and of compassion fatigue. Therefore, a fourth potential paradox is that PCC might both reduce and increase costs (Figure 1).
Figure 1.
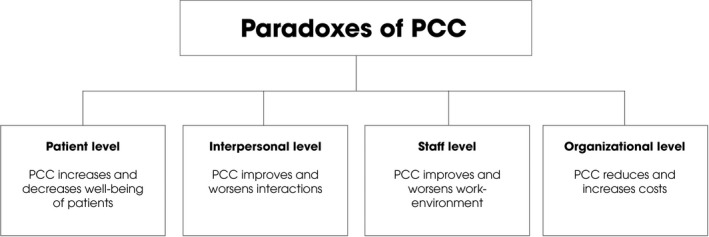
Four potential paradoxes of person‐centred care
4. CONCLUSION
The PCC approach might be simultaneously underrated and overrated: it can be underrated by those who do not regard it as a powerful approach to creating a meaningful life for the patient, whereas it can be overrated by those who believe it is free from paradoxes and has only a positive impact on care. These two perspectives might come from a limited understanding of the relationships between health provider, patient(s), organizations, society and available resources. An awareness of these paradoxes might offer managers, staff and researchers insights when implementing, practicing and researching PCC. Future research may lead to a better understanding of the complexity of this phenomenon. It is likely that further research will find solutions to some of these paradoxes, while others might remain a dilemma.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; involved in drafting the manuscript or revising it critically for important intellectual content; given final approval of the version to be published and each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Summer Meranius M, Holmström IK, Håkansson J, et al. Paradoxes of person‐centred care: A discussion paper. Nursing Open. 2020;7:1321–1329. 10.1002/nop2.520
REFERENCES
- Alharbi, T. S. J. , Carlström, E. , Ekman, I. , Jarneborn, A. , & Olsson, L.‐E. (2014). Experiences of person‐centred care ‐ patients’ perceptions: Qualitative study. BMC Nursing, 13(1), 28 10.1186/1472-6955-13-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa, A. , Sousa, L. , Nolan, M. , & Figueiredo, D. (2015). Effects of person‐centered care approaches to dementia care on staff. A Systematic Review. American Journal of Alzheimer’s Disease & Other Dementias®, 30(8), 713–722. 10.1177/1533317513520213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batson, C. D. (2011). Altruism in Humans, Oxford, UK: Oxford University Press. [Google Scholar]
- Batson, C. D. , Eklund, J. H. , Chermok, V. L. , Hoyt, J. L. , & Ortiz, B. G. (2007). An additional antecedent of empathic concern: Valuing the welfare of the person in need. Journal of Personality and Social Psychology, 93(1), 65–74. 10.1037/0022-3514.93.1.65 [DOI] [PubMed] [Google Scholar]
- Batson, C. D. , Klein, T. R. , Highberger, L. , & Shaw, L. L. (1995). Immorality from empathy induced altruism. Journal of Personality and Social Psychology, 68, 1042–1054. 10.1037/0022-3514.68.6.1042 [DOI] [Google Scholar]
- Beauchamp, T. L. , & Childress, J. F. (2009). Principles of biomedical ethics, (7th. ed. Oxford, UK: Oxford University Press. [Google Scholar]
- Blom, J. , den Elzen, W. , van Houwelingen, A. H. , Heijmans, M. , Stijnen, T. , Van den Hout, W. , & Gussekloo, J. (2016). Effectiveness and cost‐effectiveness of a proactive, goal‐oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: Integrated Systematic Care for older People—the ISCOPE study. Age and Ageing, 45(1), 30–41. 10.1093/ageing/afv174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolster, D. , & Manias, E. (2010). Person‐centred interactions between nurses and patients during medication activities in an acute hospital setting: Qualitative observation and interview study. International Journal of Nursing Studies, 47(2), 154–165. 10.1016/j.ijnurstu.2009.05.021 [DOI] [PubMed] [Google Scholar]
- Britten, N. , Moore, L. , Lydahl, D. , Naldemirci, O. , Elam, M. , & Wolf, A. (2017). Elaboration of the Gothenburg model of person‐centred care. Health Expectations, 20(3), 407–418. 10.1111/hex.12468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownie, S. , & Nancarrow, S. (2013). Effects of person‐centered care on residents and staff in aged‐care facilities: A systematic review. Clinical Interventions in Aging, 8, 1–10. 10.2147/CIA.S38589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buber, M. (1971). I and Thou. New York, NY: Charles Scribner’s Sons. [Google Scholar]
- Buber, M. , & Kaufmann, W. (1970). Iand Thou, (2nd ed.). New York, NY: Charles Scribner’s Sons. [Google Scholar]
- Chenoweth, L. , King, M. T. , Jeon, Y.‐H. , Brodaty, H. , Stein‐Parbury, J. , Norman, R. , … Luscombe, G. (2009). Caring for Aged Dementia Care Resident Study (CADRES) of person‐centred care, dementia‐care mapping and usual care in dementia: A cluster‐randomised trial. The Lancet Neurology, 8(4), 317–325. 10.1016/S1474-4422(09)70045-6 [DOI] [PubMed] [Google Scholar]
- Coetzee, S. K. , & Klopper, H. C. (2010). Compassion fatigue within nursing practice: A concept analysis. Nursing & Health Sciences, 12(2), 235–243. 10.1111/j.1442-2018.2010.00526.x [DOI] [PubMed] [Google Scholar]
- Coleman, E. A. (2003). Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. Journal of the American Geriatrics Society, 51(4), 549–555. 10.1046/j.1532-5415.2003.51185.x [DOI] [PubMed] [Google Scholar]
- Coyne, I. , Holmström, I. , & Söderbäck, M. (2018). Centeredness in healthcare: A concept synthesis of family‐centered care, person‐centered care and child‐centered care. Journal of Pediatric Nursing, 42, 45–56. 10.1016/j.pedn.2018.07.001 [DOI] [PubMed] [Google Scholar]
- Dewing, J. (2004). Concerns relating to the application of frameworks to promote person‐centredness in nursing with older people. Journal of Clinical Nursing, 13(s1), 39–44. 10.1111/j.1365-2702.2004.00925.x [DOI] [PubMed] [Google Scholar]
- Edvardsson, D. , Fetherstonhaugh, D. , McAuliffe, L. , Nay, R. , & Chenco, C. (2011). Job satisfaction amongst aged care staff: Exploring the influence of person‐centered care provision. International Psychogeriatrics, 23(8), 1205–1212. 10.1017/S1041610211000159 [DOI] [PubMed] [Google Scholar]
- Edvardsson, D. , Petersson, L. , Sjogren, K. , Lindkvist, M. , & Sandman, P.‐O. (2014). Everyday activities for people with dementia in residential aged care: Associations with person‐centredness and quality of life. International Journal of Older People Nursing, 9(4), 269–276. 10.1111/opn.12030 [DOI] [PubMed] [Google Scholar]
- Edvardsson, D. , Sandman, P. O. , & Borell, L. (2014). Implementing national guidelines for person‐centered care of people with dementia in residential aged care: Effects on perceived person‐centeredness, staff strain and stress of conscience. International Psychogeriatrics, 26(7), 1171–1179. 10.1017/S1041610214000258 [DOI] [PubMed] [Google Scholar]
- Edvardsson, D. , Watt, E. , & Pearce, F. (2017). Patient experiences of caring and person‐centredness are associated with perceived nursing care quality. Journal of Advanced Nursing, 73(1), 217–227. 10.1111/jan.13105 [DOI] [PubMed] [Google Scholar]
- Edvardsson, D. , Winblad, B. , & Sandman, P. (2008). Person‐centred care of people with severe Alzheimer’s disease: Current status and ways forward. The Lancet Neurology, 7(4), 362–367. 10.1016/S1474-4422(08)70063-2 [DOI] [PubMed] [Google Scholar]
- Ekman, I. , Swedberg, K. , Taft, C. , Lindseth, A. , Norberg, A. , Brink, E. , … Sunnerhagen, K. S. (2011). Person‐centered care—Ready for prime time. European Journal of Cardiovascular Nursing, 10(4), 248–251. 10.1016/j.ejcnurse.2011.06.008 [DOI] [PubMed] [Google Scholar]
- Ekman, I. , Wolf, A. , Olsson, L.‐E. , Taft, C. , Dudas, K. , Schaufelberger, M. , & Swedberg, K. (2012). Effects of person‐centred care in patients with chronic heart failure: The PCC‐HF study. European Heart Journal, 33(9), 1112–1119. 10.1093/eurheartj/ehr306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldthusen, C. , Dean, E. , Forsblad‐d’Elia, H. , & Mannerkorpi, K. (2016). Effects of person‐centered physical therapy on fatigue‐related variables in persons with rheumatoid arthritis: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 97(1), 26–36. 10.1016/j.apmr.2015.09.022 [DOI] [PubMed] [Google Scholar]
- Fletcher, J. F. (2015). Morals and Medicine: The Moral Problems of the Patient’s Right to Know the Truth, Contraception, Artificial Insemination, Sterilization, Euthanasia, Princeton, New Jersey: Princeton University Press. [Google Scholar]
- Fors, A. , Blanck, E. , Ali, L. , Ekberg‐Jansson, A. , Fu, M. , Kjellberg, I. L. , … Ekman, I. (2018). Effects of a person‐centred telephone‐support in patients with chronic obstructive pulmonary disease and/or chronic heart failure – A randomized controlled trial. PLoS ONE, 13(8), e0203031 10.1371/journal.pone.0203031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fors, A. , Ekman, I. , Taft, C. , Björkelund, C. , Frid, K. , Larsson, M. E. , … Swedberg, K. (2015). Person‐centred care after acute coronary syndrome, from hospital to primary care—A randomised controlled trial. International Journal of Cardiology, 187, 693–699. 10.1016/j.ijcard.2015.03.336 [DOI] [PubMed] [Google Scholar]
- Fors, A. , Swedberg, K. , Ulin, K. , Wolf, A. , & Ekman, I. (2017). Effects of person‐centred care after an event of acute coronary syndrome: Two‐year follow‐up of a randomised controlled trial. International Journal of Cardiology, 249, 42–47. 10.1016/j.ijcard.2017.08.069 [DOI] [PubMed] [Google Scholar]
- Fors, A. , Taft, C. , Ulin, K. , & Ekman, I. (2016). Person‐centred care improves self‐efficacy to control symptoms after acute coronary syndrome: A randomized controlled trial. European Journal of Cardiovascular Nursing, 15(2), 186–194. 10.1177/1474515115623437 [DOI] [PubMed] [Google Scholar]
- Fossey, J. , Masson, S. , Stafford, J. , Lawrence, V. , Corbett, A. , & Ballard, C. (2014). The disconnect between evidence and practice: A systematic review of person‐centred interventions and training manuals for care home staff working with people with dementia. International Journal of Geriatric Psychiatry, 29(8), 797–807. 10.1002/gps.4072 [DOI] [PubMed] [Google Scholar]
- Gabrielsson, S. , Sävenstedt, S. , & Zingmark, K. (2015). Person‐centred care: Clarifying the concept in the context of inpatient psychiatry. Scandinavian Journal of Caring Sciences, 29(3), 555–562. 10.1111/scs.12189 [DOI] [PubMed] [Google Scholar]
- Håkansson Eklund, J. , Holmström, I. K. , Kumlin, T. , Kaminsky, E. , Skoglund, K. , Höglander, J. , … Summer Meranius, M. (2018). “Same same or different?” A review of reviews of person‐centered and patient‐centered care. Patient Education and Counseling, 102(1), 3–11. 10.1016/j.pec.2018.08.029 [DOI] [PubMed] [Google Scholar]
- Halpern, J. , Johnson, M. D. , Miranda, J. , & Wells, K. B. (2004). The partners in care approach to ethics outcomes in quality improvement programs for depression. Psychiatric Services, 55(5), 532–539. 10.1176/appi.ps.55.5.532 [DOI] [PubMed] [Google Scholar]
- Hansen, E. M. , Eklund, J. H. , Hallén, A. , Bjurhager, C. S. , Norrström, E. , Viman, A. , & Stocks, E. L. (2018). Does feeling empathy lead to compassion fatigue or compassion satisfaction? The role of time perspective. The Journal of Psychology, 152(8), 630–645. 10.1080/00223980.2018.1495170 [DOI] [PubMed] [Google Scholar]
- Hansson, E. , Carlström, E. , Olsson, L.‐E. , Nyman, J. , & Koinberg, I. (2017). Can a person‐centred‐care intervention improve health‐related quality of life in patients with head and neck cancer? A randomized, controlled study. BMC Nursing, 16(1), 9 10.1186/s12912-017-0206-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson, E. , Ekman, I. , Swedberg, K. , Wolf, A. , Dudas, K. , Ehlers, L. , & Olsson, L.‐E. (2016). Person‐centred care for patients with chronic heart failure – a cost–utility analysis. European Journal of Cardiovascular Nursing, 15(4), 276–284. 10.1177/1474515114567035 [DOI] [PubMed] [Google Scholar]
- Holburn, S. , Jacobson, J. W. , Schwartz, A. A. , Flory, M. J. , & Vietze, P. M. (2004). The willowbrook futures project: A longitudinal analysis of person‐centered planning. American Journal on Mental Retardation, 109(1), 63–76. [DOI] [PubMed] [Google Scholar]
- Holmström, I. , & Röing, M. (2010). The relation between patient‐centeredness and patient empowerment: A discussion on concepts. Patient Education and Counseling, 79(2), 167–172. 10.1016/j.pec.2009.08.008 [DOI] [PubMed] [Google Scholar]
- Hughes, J. C. , Bamford, C. , & May, C. (2008). Types of centredness in health care: Themes and concepts. Medicine, Health Care and Philosophy, 11(4), 455–463. 10.1007/s11019-008-9131-5 [DOI] [PubMed] [Google Scholar]
- Jansson, I. , Fors, A. , Ekman, I. , & Ulin, K. (2018). Documentation of person‐centred health plans for patients with acute coronary syndrome. European Journal of Cardiovascular Nursing, 17(2), 114–122. 10.1177/1474515117718415 [DOI] [PubMed] [Google Scholar]
- Joison, C. (1992). Coping with compassion fatigue. Nursing, 4(22), 118–119. [PubMed] [Google Scholar]
- Kacem, A. , & Mayr, P. (2017). Analysis of footnote chasing and citation searching in an academic search engine. ArXiv:1707.02494 [Cs]. Retrieved from http://arxiv.org/abs/1707.02494 [Google Scholar]
- Kadri, A. , Rapaport, P. , Livingston, G. , Cooper, C. , Robertson, S. , & Higgs, P. (2018). Care workers, the unacknowledged persons in person‐centred care: A secondary qualitative analysis of UK care home staff interviews. PLoS ONE, 13(7), e0200031 10.1371/journal.pone.0200031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs, D. (1975). Empathy and altruism. Journal of Personality and Social Psychology, 32(6), 1134–1146. 10.1037/0022-3514.32.6.1134 [DOI] [PubMed] [Google Scholar]
- Lehuluante, A. , Nilsson, A. , & Edvardsson, D. (2012). The influence of a person‐centred psychosocial unit climate on satisfaction with care and work. Journal of Nursing Management, 20(3), 319–325. 10.1111/j.1365-2834.2011.01286.x [DOI] [PubMed] [Google Scholar]
- Leplege, P. A. , Gzil, F. , Cammelli, M. , Lefeve, C. , Pachoud, B. , & Ville, I. (2007). Person‐centredness: Conceptual and historical perspectives. Disability and Rehabilitation, 29(20–21), 1555–1565. 10.1080/09638280701618661 [DOI] [PubMed] [Google Scholar]
- Li, J. , & Porock, D. (2014). Resident outcomes of person‐centered care in long‐term care: A narrative review of interventional research. International Journal of Nursing Studies, 51(10), 1395–1415. 10.1016/j.ijnurstu.2014.04.003 [DOI] [PubMed] [Google Scholar]
- Makai, P. , Looman, W. , Adang, E. , Melis, R. , Stolk, E. , & Fabbricotti, I. (2015). Cost‐effectiveness of integrated care in frail elderly using the ICECAP‐O and EQ‐5D: Does choice of instrument matter? The European Journal of Health Economics, 16(4), 437–450. 10.1007/s10198-014-0583-7 [DOI] [PubMed] [Google Scholar]
- McCormack, B. (2004). Person‐centredness in gerontological nursing: An overview of the literature. Journal of Clinical Nursing, 13(s1), 31–38. 10.1111/j.1365-2702.2004.00924.x [DOI] [PubMed] [Google Scholar]
- McCormack, B. , & McCance, T. V. (2006). Development of a framework for person‐centred nursing. Journal of Advanced Nursing, 56(5), 472–479. 10.1111/j.1365-2648.2006.04042.x [DOI] [PubMed] [Google Scholar]
- Mead, N. , & Bower, P. (2000). Patient‐centredness: A conceptual framework and review of the empirical literature. Social Science & Medicine, 51(7), 1087–1110. 10.1016/S0277-9536(00)00098-8 [DOI] [PubMed] [Google Scholar]
- Metzelthin, S. F. , van Rossum, E. , Hendriks, M. R. C. , De Witte, L. P. , Hobma, S. O. , Sipers, W. , & Kempen, G. I. J. M. (2015). Reducing disability in community‐dwelling frail older people: Cost‐effectiveness study alongside a cluster randomised controlled trial. Age and Ageing, 44(3), 390–396. 10.1093/ageing/afu200 [DOI] [PubMed] [Google Scholar]
- O’Dwyer, C. (2013). Official conceptualizations of person‐centered care: Which person counts? Journal of Aging Studies, 27(3), 233–242. 10.1016/j.jaging.2013.03.003 [DOI] [PubMed] [Google Scholar]
- Olsson, L.‐E. , Hansson, E. , & Ekman, I. (2016). Evaluation of person‐centred care after hip replacement‐a controlled before and after study on the effects of fear of movement and self‐efficacy compared to standard care. BMC Nursing, 15(1), 53 10.1186/s12912-016-0173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsson, L.‐E. , Ung, E. J. , Swedberg, K. , & Ekman, I. (2013). Efficacy of person‐centred care as an intervention in controlled trials – a systematic review. Journal of Clinical Nursing, 22(3–4), 456–465. 10.1111/jocn.12039 [DOI] [PubMed] [Google Scholar]
- Parley, F. F. (2001). Person‐centred outcomes: Are outcomes improved where a person‐centred care model is used? Journal of Learning Disabilities, 5(4), 299–308. 10.1177/146900470100500402 [DOI] [Google Scholar]
- Ricoeur, P. (1992). Oneself as Another, Chicago, IL: University of Chicago Press. [Google Scholar]
- Robertson, S. B. , & Rosher, R. B. (2006). Tangling with the barriers to culture change: Creating a resident‐centred nursing home environment. Journal of Gerontological Nursing, 32, 19–27. 10.3928/00989134-20061001-04 [DOI] [PubMed] [Google Scholar]
- Rosher, R. B. , & Robinson, S. (2005). Impact of the Eden alternative on family satisfaction. Journal of the American Medical Directors Association, 6(3), 189–193. 10.1016/j.jamda.2005.03.005 [DOI] [PubMed] [Google Scholar]
- Sharp, S. , McAllister, M. , & Broadbent, M. (2016). The vital blend of clinical competence and compassion: How patients experience person‐centred care. Contemporary Nurse, 52(2–3), 300–312. 10.1080/10376178.2015.1020981 [DOI] [PubMed] [Google Scholar]
- Sjögren, K. , Lindkvist, M. , Sandman, P.‐O. , Zingmark, K. , & Edvardsson, D. (2014). To what extent is the work environment of staff related to person‐centred care? A cross‐sectional study of residential aged care. Journal of Clinical Nursing, 24(9–10), 1310–1319. 10.1111/jocn.12734 [DOI] [PubMed] [Google Scholar]
- Sloane, P. D. , Hoeffer, B. , Mitchell, C. M. , McKenzie, D. A. , Barrick, A. L. , Rader, J. , … Koch, G. G. (2004). Effect of person‐centered showering and the towel bath on bathing‐associated aggression, agitation and discomfort in nursing home residents with dementia: a randomized, controlled trial. Journal of the American Geriatrics Society, 52(11), 1795–1804. 10.1111/j.1532-5415.2004.52501.x [DOI] [PubMed] [Google Scholar]
- Uittenbroek, R. J. , van Asselt, A. D. I. , Spoorenberg, S. L. W. , Kremer, H. P. H. , Wynia, K. , & Reijneveld, S. A. (2018). Integrated and person‐centered care for community‐living older adults: A cost‐effectiveness study. Health Services Research, 53(5), 3471–3494. 10.1111/1475-6773.12853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulin, K. , Olsson, L.‐E. , Wolf, A. , & Ekman, I. (2016). Person‐centred care – An approach that improves the discharge process. European Journal of Cardiovascular Nursing, 15(3), e19–e26. 10.1177/1474515115569945 [DOI] [PubMed] [Google Scholar]
- van Leeuwen, K. M. , Bosmans, J. E. , Jansen, A. P. D. , Hoogendijk, E. O. , Muntinga, M. E. , van Hout, H. P. J. , … van Tulder, M. W. (2015). Cost‐effectiveness of a chronic care model for frail older adults in primary care: Economic evaluation alongside a stepped‐wedge cluster‐randomized trial. Journal of the American Geriatrics Society, 63(12), 2494–2504. 10.1111/jgs.13834 [DOI] [PubMed] [Google Scholar]
- Vassbø, T. K. , Kirkevold, M. , Edvardsson, D. , Sjögren, K. , Lood, Q. , Sandman, P. O. , & Bergland, Å. (2018). Associations between job satisfaction, person‐centredness and ethically difficult situations in nursing homes—A cross‐sectional study. Journal of Advanced Nursing, 75(5), 10.1111/jan.13890 [DOI] [PubMed] [Google Scholar]
- Wallström, S. , & Ekman, I. (2018). Person‐centred care in clinical assessment. European Journal of Cardiovascular Nursing, 17(7), 576–579. 10.1177/1474515118758139 [DOI] [PubMed] [Google Scholar]
- Wigham, S. , Robertson, J. , Emerson, E. , Hatton, C. , Elliott, J. , McIntosh, B. , … Joyce, T. (2008). Reported goal setting and benefits of person centred planning for people with intellectual disabilities. Journal of Intellectual Disabilities, 12(2), 143–152. 10.1177/1744629508090994 [DOI] [PubMed] [Google Scholar]
- Wilberforce, M. , Challis, D. , Davies, L. , Kelly, M. P. , Roberts, C. , & Clarkson, P. (2017). Person‐centredness in the community care of older people: A literature‐based concept synthesis. International Journal of Social Welfare, 26(1), 86–98. 10.1111/ijsw.12221 [DOI] [Google Scholar]
- Wildevuur, S. E. , & Simonse, L. W. (2015). Information and communication technology‐enabled person‐centered care for the “Big Five” chronic conditions: Scoping review. Journal of Medical Internet Research, 17(3), e77 10.2196/jmir.3687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoffmann, V. , Harder, I. , & Kirkevold, M. (2008). A Person‐centered communication and reflection model: Sharing decision‐making in chronic care. Qualitative Health Research, 18(5), 670–685. 10.1177/1049732307311008 [DOI] [PubMed] [Google Scholar]


