Abstract
Background
Ultra-processed food (UPF) consumption, which is increasing worldwide, has recently been associated with an increased risk of death and cardiovascular disease. We aimed to assess whether consumption of UPF is directly associated with subclinical coronary atherosclerosis in middle-aged men.
Methods
A computed tomography scan was performed on 1876 men from the Aragon Workers’ Health Study, recruited from January 2011 to December 2014, to assess coronary calcium. All participants were free of coronary heart disease. Dietary intake was collected by a validated 136-item semi-quantitative food frequency questionnaire. UPF was defined according to the NOVA classification. Associations between consumption of total energy-adjusted UPF and Coronary Calcium Agatston Score (CACS)—categorized into CACS of 0, > 0 and < 100, and ≥ 100—were cross-sectionally assessed by generalized ordered logistic regression adjusted for main confounders.
Results
No coronary calcium was detected in 60.2% of the participants, whereas 10.2% had a CACS ≥ 100. A significant dose-response association was observed between energy-adjusted UPF consumption and the risk of having a CACS ≥ 100, when compared with those in the lowest CACS categories (CACS of 0 together with CACS > 0 and < 100). The fully adjusted ORs (95% CI) of having a CACS ≥ 100 across quartiles of energy-adjusted UPF consumption (approximately 100 g/day in the lowest quartile (ref.) and 500 g/day in the highest) were 1.00 (ref.), 1.50 (0.93, 2.42), 1.56 (0.96, 2.52), and 2.00 (1.26, 3.16), p trend .005.
Conclusion
In this middle-aged worker’s sample, approximately 500 g/day of UPF consumption was associated with a 2-fold greater prevalence of subclinical coronary atherosclerosis than consuming only 100 g/day, independently of total energy intake and other well-established cardiovascular risk factors.
Keywords: Ultra-processed food, Subclinical coronary atherosclerosis, Coronary calcium, Cross-sectional cohort study, Nutritional epidemiology
Background
The food and beverage industry has experienced high growth in recent years, and the consumption of ultra-processed food (UPF) has substantially increased, fostered by attractive packaging and intensive marketing [1]. UPF consumption in Spain is low to moderate [2], but it is increasing rapidly. While in 1990, UPF consumption represented 11% of daily energy intake in Spain, it has almost tripled in 10 years [3]. In 2000, the mean contribution of UPF in total energy intake was about 35% in Spain and Italy, but it reached up to 60% in the Netherlands, Sweden, Norway, Denmark, and the UK general population [4].
UPF is formulated mostly or entirely from substances derived from food together with additives, with little, if any, intact food. Processing entails greater durability, tastier flavors, and readiness to consume at a very low price. UPF is characterized by poor nutritional value and high energy density with low fiber and micronutrient content, as well as high amounts of sodium, saturated and trans fats, and simple sugars [5, 6]. On the one hand, all aforementioned detrimental nutrients have been individually associated with subclinical atherosclerosis and cardiovascular disease (CVD) [7–9]. On the other hand, UPF also contains a great diversity of additives, many of which have shown adverse effects on the vascular system in experimental studies [10–12]. In particular, the additive phosphate, present in almost all UPF, is involved in atherosclerosis by inducing vascular calcification both in vitro and in vivo [13]. Finally, UPF consumption replaces the intake of other unprocessed or minimally processed food and freshly prepared meals that have beneficial nutritional attributes, also affecting health in an indirect way.
Recently, in the large prospective NutriNet-Santé cohort, an absolute increment of 10% of UPF in the diet has been associated with a 12%, 13%, and 11% statistically significant increase in the rates of overall CVD, coronary heart disease (CHD), and cerebrovascular disease, respectively [14]. Likewise, consumption of UPF has been associated with cardiometabolic conditions [15], such as overweight or obesity [16], hypertension [17], dyslipidemia [18], and diabetes [19], as well as with CVD mortality or total mortality [2, 20, 21].
Atherosclerosis, which underlies CVD, is a complex disease in which fat, inflammation cells, scar tissue, and deposits of calcium accumulate within the walls of the arteries [22]. The presence of calcium in the coronary arteries is an indicator of subclinical atherosclerotic disease and a marker of coronary damage [23], as well as a strong and independent predictor of future coronary heart disease [24, 25]. Current guidelines endorse the measurement of coronary calcium to improve risk prediction of coronary disease in selected asymptomatic individuals [26, 27]. Accordingly, high calcium in coronary arteries has been consistently associated with general coronary disease [28], myocardial infarction [28, 29], heart failure [29], and stroke [30].
To date, no epidemiological study has yet evaluated the direct impact of UPF consumption on the coronary arteries in asymptomatic subjects. The aim of this study is therefore to examine the association between UPF consumption and subclinical coronary atherosclerosis in a sample of middle-aged subjects with a low prevalence of clinical comorbidities.
Methods
Study design and population
The present cross-sectional study includes a sample of participants from the Aragon Workers’ Health Study (AWHS), the design of which has been described in detail elsewhere [31, 32]. Study participants are workers of Opel Spain automobile assembly plant located in Figueruelas (Zaragoza, Spain) that were recruited during a standardized clinical exam in 2009–2010 (participation rate 95.6%). In addition, between January 2011 and December 2014, all participants who were aged 40–60 years old (34% of initial participants) were invited to undergo a coronary calcification scan and provided blood and urine samples for the study biobank, as well as to answer a comprehensive questionnaire on cardiovascular and lifestyle factors, including diet. No relevant differences were detected in baseline characteristics between total participants and those who undergo the coronary calcification scan. Among the 2617 workers (all Caucasian) recruited into the AWHS imaging study, 2128 had complete quantification of coronary calcification. Likewise, those subjects with previous history of CVD (n = 28), women (n = 97), and those with an extreme total energy intake (< 600 or > 4200 kcal) (n = 127) were excluded, resulting in a final sample of 1876 participants (Fig. 1).
Fig. 1.
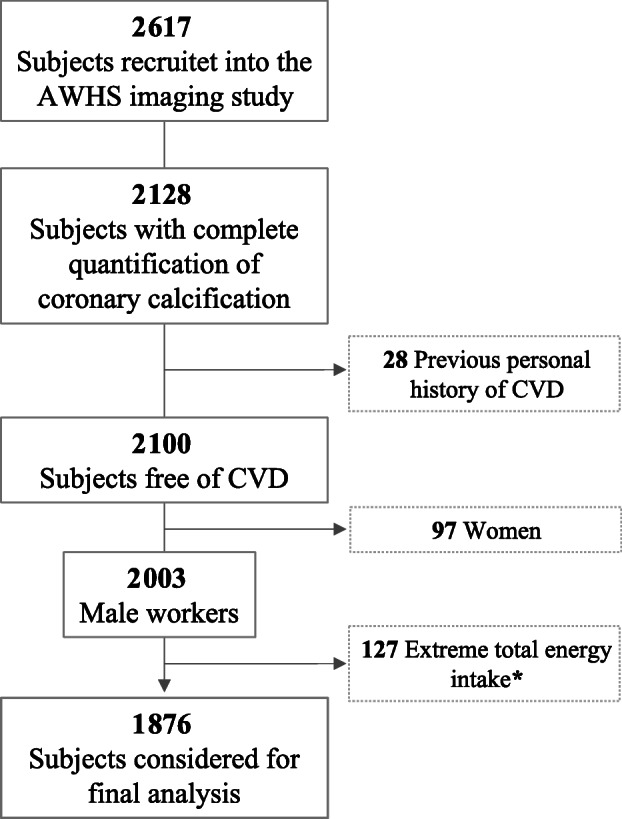
Flow chart for the study association: Coronary Artery Calcium Score and ultra-processed food consumption. *Total energy intake of < 600 or > 4200 kcal in men was considered extreme values. Subjects recruited in the imaging AWHS. AWHS, Aragon Workers’ Health Study; CVD, cardiovascular disease
Data collection
Demographic information including age, sex, marital status, educational level, smoking, sleep duration (both on weekdays and weekends), and diabetic status was obtained by questionnaires. Also, leisure-time physical activity and time spent in sedentary activities were assessed using a formerly validated questionnaire, i.e., the Health Professionals’ Follow-up physical activity questionnaire [33], that was highly correlated with objective measurements using triaxial accelerometer (RT3 Triaxial Research Tracker) as reference (Spearman’s correlation coefficient of 0.51; p < 0.001). Participants were asked about the time devoted to 17 different activities during the preceding year, and leisure-time physical activity was expressed in metabolic equivalents (METs)-h/week.
Serum samples were obtained, and cholesterol, triglycerides, and glycemia were measured. Study participants went through a standardized clinical exam with blood pressure (BP) and heart rate measurements. BP was measured three consecutive times using an automatic oscillometric sphygmomanometer after being seated for 5 min. Anthropometrics, including height, weight, and waist circumference, were also measured following standardized procedures, and body mass index (BMI, in kg/m2) was calculated.
Physicians and nurses collecting these data underwent specific training and standardization programs organized by the study investigators. Compliance with study procedures was routinely monitored, and deviations were corrected. The study conforms to the ISO9001-2008 quality standard.
Dietary assessment and ultra-processed food consumption
Their usual diet over the preceding year was assessed using a 136-item semi-quantitative food frequency questionnaire (FFQ) previously validated and repeatedly re-evaluated in Spain [34–36]. This FFQ considers seasonal variations and differences in food consumption between weekdays and weekend patterns. We measured the frequency of food consumption in nine categories (ranging from never or almost never to more than six servings per day), also including a standard portion size for each food item. To estimate daily consumption for each food item, we multiplied the portion size by the frequency of consumption.
We listed all food and beverage items of the FFQ according to NOVA classification [6] which organizes food into four groups based on the scope and purpose of industrial processing. The first group includes unprocessed or minimally processed food, which is fresh or modified by filtering, freezing, drying, or pasteurization, with no addition of salt, sugar, oils, or fats. The second group contains processed culinary ingredients. These are substances derived from nature, but have undergone processes such as pressing, refining, or milling and might contain additives to preserve the original properties (i.e., salt, sugar, honey, vegetable oils, butter, lard, and vinegar). The third group comprises processed food. This is food which has undergone preservation or preparation methods (e.g., smoking, curing, or fermentation) in order to last longer or to enhance their sensory qualities. Examples include canned or bottled vegetables and legumes, fruit in syrup, canned fish, cheese, freshly made bread, and salted/sugared nuts and seeds. The fourth group comprises ultra-processed food and drink products that are made predominantly or entirely from industrial substances and contain little or no whole food. Under this classification, we can find products such as hamburgers, frozen pizza and pasta dishes, French fries, breads, cakes, industrially manufactured biscuits (cookies), jams and confectionery, margarines, cereal bars, soft drinks and other sugary beverages such as sugared milk and fruit drinks, fruit yogurts, instant packaged soups and noodles, and sweet or savory snacks.
For each participant, total UPF consumption in grams per day (g/day) was calculated summing up the consumption from each UPF item included in the fourth group of the NOVA classification (Additional File 1: Table S1). The grams per day of UPF were adjusted for total energy intake by the residual method [37].
Outcome assessment: Coronary Agatston Calcium Score
Coronary calcium quantification was performed using non-contrast ECG-gated prospective acquisition by a 16-multidetector computed tomography scanner (Philips). Agatston’s method is a summed score of all coronary calcified lesions, accounting for both the total area and the maximum density of coronary calcium. A high Coronary Calcium Agatston Score (CACS) is a strong indicator of extensive disease with a significant amount of calcium deposits. CACS remains the reference standard and the most commonly used coronary artery calcium score in clinical practice [38].
CACS was divided into three consecutive categories: 0, > 0 and < 100, and ≥ 100. Having a CACS > 0 represents the presence of calcium, and surpassing a threshold of ≥ 100 is considered as having a moderate to severe subclinical coronary atherosclerosis and has been associated with increases in coronary heart disease rates [39].
Statistical analysis
Participants were categorized into quartiles of daily grams of UPF consumption after adjusting for total energy intake using the residual method [37]. The analyses were also carried out using quartiles of daily percentage of energy derived from UPF, revealing very similar results (data not presented).
The adequacy of the proportional odds assumption across response categories (a requirement for conducting ordered logistic regression) was examined by using tests for proportionality (Wald’s test and Brant’s test). We found a violation of this assumption (p values < 0.05). Accordingly, we estimated the odds ratio (OR) and corresponding 95% confidence intervals (CI) for having progressed to categories of more coronary artery calcium using generalized ordered logistic models (gologit/partial proportional odds model). These models are less restrictive than the proportional-odds/parallel-lines models and do not assume the equality of slopes among categories. This approach yields two ORs, one describing the relationship between the lowest vs. the two highest categories of the response variable (CACS), and the other describing the relationship between the two lowest categories vs. the highest one [40].
We additionally performed a standard binary logistic regression for the collapsed categories to estimate the OR for CACS > 0 (compared with CACS of 0) and for CACS ≥ 100 (compared with CACS < 100), to provide estimations which can easily be understood as they are widely used. So, we provide two estimators to describe the association between UPF consumption and CACS. To calculate the p for linear trend, the mean concentrations of UPF in each quartile were used and treated as a continuous variable in the model. Likewise, the standard binary logistic regression was used to perform restricted cubic splines with 3 knots (at the 10th, 50th, and 90th percentiles of the distribution) to visualize flexible dose-response associations.
We used three models with progressive adjustment for covariates that can operate as confounders [41]. Model 1 was adjusted for age (continuous, years); model 2 was further adjusted for demographic and lifestyle factors: marital status (married, not married), education (middle school, high school, professional training, and college), smoking status (never, former, and current smoker), physical activity (in MET-h/week), time spent sleeping during the weekdays (number of hours of sleep, continuous), time spent sleeping during the weekend (number of hours of sleep, continuous), and dietary factors such as alcohol consumption (g/day), total fiber (g/day), cholesterol intake,(mg/day), and total energy intake (kcal); and model 3 was further adjusted for cardiometabolic risk factors: total cholesterol in blood (mg/dL), HDL cholesterol in blood (mg/dL), systolic and diastolic blood pressure (mmHg), BMI (< 25, 25 to < 30, ≥ 30 kg/m2), and diabetes (yes, no).
To maximize the use of available information, missing values on education (< 1%) and smoking (< 1%) were included in a separate category. Missing values on hours of sleep during the week (< 1%) and BMI (< 1%) were imputed by predicted values from a multivariable regression model containing the corresponding explanatory variables. Missing values on diabetes (3%) were considered as having a non-disease status.
We tested for interactions between UPF consumption and age, BMI, smoking status, alcohol consumption, and physical activity, on the multiplicative scale using the likelihood ratio test, comparing binary logistic models with and without an interaction term.
Analyses were performed with Stata/SE, version 15.1 (StataCorp, College Station). Statistical significance was set at the two-sided 0.05 level.
Results
All participants were Caucasian males with a mean age of 51 ± 3.7 years. The average UPF consumption ranged from 117 ± 56 g/day in the lowest quartile to 484 ± 217 g/day in the highest one. Those in the highest quartile of UPF consumption were less frequently current smokers; performed less physical activity; had a lower consumption of alcohol, fiber, micronutrients (vitamins and minerals); and had lower HDL cholesterol levels. Likewise, although non-statistically significant, those consuming more UPF were more frequently obese than those consuming less. In general, no other meaningful differences in demographic and lifestyle variables were observed across UPF quartiles (Table 1).
Table 1.
Characteristics of the study participants according to quartiles of energy-adjusted ultra-processed food (UPF) consumption, the AWHS cohort study (N = 1876)
| Energy-adjusted UPF consumption (g/day)* | |||||
|---|---|---|---|---|---|
| Q1 (n = 469) | Q2 (n = 469) | Q3 (n = 469) | Q4 (n = 469) | p value | |
| Energy-adjusted UPF consumption (g/day)* | 117 ± 56 | 169 ± 66 | 263 ± 76 | 484 ± 217 | < .01 |
| Total energy intake (kcal) | 2988 ± 564 | 2685 ± 616 | 2793 ± 638.4 | 2840 ± 601 | < .01 |
| Age (years) | 51.5 ± 3.6 | 51.3 ± 3.7 | 51.0 ± 3.7 | 50.7 ± 3.9 | < .01 |
| Married (%) | 85.6 (406) | 85.5 (401) | 84.9 (398) | 85.3 (400) | .90 |
| Education (%) | .68 | ||||
| Middle school | 52.6 (245) | 49.1 (229) | 52.2 (242) | 55.0 (255) | |
| High school | 12.0 (56) | 11.8 (55) | 10.1 (47) | 10.1 (47) | |
| Professional training | 31.8 (148) | 33.5 (156) | 34.0 (158) | 30.6 (142) | |
| College | 3.6 (17) | 5.6 (26) | 3.7 (17) | 4.3 (20) | |
| Smoking (%) | < .01 | ||||
| Never | 20.6 (96) | 19.7 (92) | 26.3 (123) | 25.5 (119) | |
| Former | 29.2 (136) | 29.4 (137) | 34.1 (159) | 36.2 (169) | |
| Current | 50.2 (234) | 50.9 (237) | 39.6 (185) | 38.3 (179) | |
| Physical activity (MET-h/week) | 36.22 ± 23.8 | 31.84 ± 21.0 | 31.0 ± 22.1 | 31.5 ± 22.5 | < .01 |
| Sleep duration (hours) | |||||
| During the week | 6.3 ± 1.0 | 6.3 ± 0.9 | 6.3 ± 1.0 | 6.3 ± 1.0 | .66 |
| During the weekend | 7.3 ± 1.1 | 7.3 ± 1.2 | 7.3 ± 1.2 | 7.3 ± 1.2 | .92 |
| Body mass index (%) | .35 | ||||
| < 25 kg/m2 | 20.5(96) | 17.5 (82) | 18.8 (88) | 19.6 (92) | |
| 25 to < 30 kg/m2 | 59.9 (281) | 58.6 (275) | 57.1 (268) | 54.6 (256) | |
| ≥ 30 kg/m2 | 19.6 (92) | 23.9 (112) | 24.1 (113) | 25.8 (121) | |
| Cholesterol intake (mg/day) | 456.7 ± 139.3 | 440.5 ± 129.4 | 461.6 ± 140.6 | 460.4 ± 140.4 | .07 |
| Total cholesterol in blood (mg/dL) | 223.3 ± 36.1 | 222.1 ± 35.7 | 223.3 ± 35.4 | 220.0 ± 37.6 | .46 |
| HDL cholesterol in blood (mg/dL) | 54.1 ± 11.9 | 52.4 ± 10.9 | 52.7 ± 11.1 | 52.0 ± 11.2 | .03 |
| Blood pressure (mmHg) | |||||
| Systolic | 126.3 ± 14.3 | 125.3 ± 13.9 | 125.6 ± 14.8 | 126.6 ± 14.1 | .47 |
| Diastolic | 83.2 ± 9.6 | 82.9 ± 9.5 | 82.9 ± 9.6 | 83.8 ± 9.1 | .42 |
| Prevalent diabetes (%) | 4.5 (21) | 3.4 (16) | 4.3 (20) | 3.8 (18) | .84 |
| Alcohol consumption (g/day) | 25.2 ± 22.2 | 18.8 ± 17.7 | 20.1 ± 20.5 | 20.6 ± 18.7 | < .01 |
| Total fiber* (g/day) | 27.2 ± 7.7 | 25.2 ± 7.9 | 24.3 ± 7.0 | 23.2 ± 6.7 | < .01 |
| Omega 3 non-marine source* (g/day) | 1.6 ± 0.7 | 1.6 ± 0.6 | 1.6 ± 0.5 | 1.5 ± 0.6 | 0.08 |
| Omega 3 marine source* (g/day) | 0.73 ± 0.4 | 0.71 ± 0.4 | 0.67 ± 0.4 | 0.63 ± 0.4 | < .01 |
| Vitamin C* (mg/day) | 180.9 ± 72.8 | 184.4 ± 68.9 | 177.9 ± 61.5 | 178.4 ± 71.3 | .45 |
| Vitamin D* (μg/day) | 5.4 ± 3.3 | 5.5 ± 3.0 | 5.2 ± 2.8 | 5.0 ± 2.7 | .02 |
| Vitamin A* (μg/day) | 1226.4 ± 673 | 1220.6 ± 554 | 1272.4 ± 643 | 1206.7 ± 682 | < .01 |
| Vitamin E* (mg/day) | 10.5 ± 3.6 | 10.9 ± 3.2 | 11.4 ± 3.8 | 11.5 ± 3.7 | < .01 |
| Vitamin B6* (mg/day) | 2.5 ± 0.5 | 2.5 ± 0.5 | 2.4 ± 0.4 | 2.3 ± 0.5 | < .01 |
| Vitamin B9* (mg/day) | 379.7 ± 72.6 | 369.9 ± 71.0 | 357.4 ± 61.6 | 345.3 ± 66.6 | < .01 |
| Vitamin B12* (mg/day) | 10.1 ± 4.4 | 9.7 ± 3.4 | 9.8 ± 4.1 | 9.2 ± 4.0 | < .01 |
| Magnesium* (mg/day) | 429.6 ± 69.6 | 426.7 ± 68.3 | 415.3 ± 60.6 | 407.3 ± 61.7 | < .01 |
| Calcium* (mg/day) | 1018.9 ± 323.2 | 1035.8 ± 285.1 | 1019.0 ± 280.3 | 1019.9 ± 304.0 | .78 |
| Zinc* (mg/day) | 15.5 ± 2.1 | 14.9 ± 2.0 | 14.5 ± 1.9 | 14.3 ± 1.9 | < .01 |
| Iodine* (μg/day) | 301.3 ± 195.6 | 294.7 ± 151.1 | 276.2 ± 147.7 | 258.9 ± 156.3 | < .01 |
| Selenium* (μg/day) | 132.7 ± 27.5 | 123.0 ± 25.8 | 116. 8 ± 25.7 | 113.1 ± 26.2 | < .01 |
Continuous variables are presented as mean ± standard deviation and categorical variables as percentage (frequency, n)
p value estimates are based on one-way ANOVA (Bonferroni’s multiple-comparison test) for variables expressed as mean (standard deviation) or Pearson’s χ2 test for variables expressed as percentages
UPF ultra-processed food, Q quartiles
*Energy adjusted by the residual method
Regarding CACS, 60.2% of the participants (n = 1129) had no coronary artery calcium, 29.6% had a CACS > 0 but < 100 (n = 556), and the remaining 10.2% (n = 191) had a CACS ≥ 100 (those with a well-defined and established disease). A significant dose-response association was observed between daily consumption of UPF and the risk of progress from the two lowest categories (CACS of 0 together with CACS > 0 and < 100) to the highest category (CACS ≥ 100). The fully adjusted ORs (95% CI) of having a CACS ≥ 100 across quartiles of UPF consumption (1st quartile as reference) were 1.50 (0.93, 2.42), 1.56 (0.96, 2.52), and 2.00 (1.26, 3.16), p trend .005. However, there was no association between consumption of UPF and the risk of progressing from no coronary artery calcium (CACS of 0) to the two highest CACS categories (CACS > 0 and < 100 together with CACS ≥ 100) (Table 2).
Table 2.
Progression to higher coronary artery calcium score (CACS) categories according to quartiles of ultra-processed food (UPF) consumption, using generalized ordered logistic models, the AWHS cohort study (N = 1876)
| CACS categories | Quartiles of energy-adjusted UPF consumption (g/day)*, odds ratio (95% confidence intervals) | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | p trend | |
| From the lowest category to the two highest† | |||||
| Model 1, OR (95% CI) | 1 (ref.) | 1.10 (0.84, 1.44) | 1.18 (0.90, 1.55) | 1.15 (0.88, 1.51) | .315 |
| Model 2, OR (95% CI) | 1 (ref.) | 1.09 (0.83, 1.44) | 1.19 (0.90, 1.57) | 1.14 (0.86, 1.51) | .382 |
| Model 3, OR (95% CI) | 1 (ref.) | 1.09 (0.83, 1.45) | 1.17 (0.88, 1.56) | 1.13 (0.85, 1.50) | .425 |
| From the two lowest categories to the highestγ | |||||
| Model 1, OR (95% CI) | 1 (ref.) | 1.39 (0.88, 2.18) | 1.47 (0.93, 2.31) | 1.86 (1.20, 2.87) | .006 |
| Model 2, OR (95% CI) | 1 (ref.) | 1.37 (0.86, 2.19) | 1.54 (0.96, 2.47) | 1.96 (1.24, 3.07) | .003 |
| Model 3, OR (95% CI) | 1 (ref.) | 1.50 (0.93, 2.42) | 1.56 (0.96, 2.52) | 2.00 (1.26, 3.16) | .005 |
The generalized ordered logistic model (gologit/partial proportional odds model) allows for the no equality of slopes among categories, being less restrictive and more flexible than the ordinal ordered logistic model (parallel-lines model). OR odds ratio, CI confidence interval
Model 1: logistic regression model adjusted for age
Model 2: as in model 1 and additionally adjusted for marital status, education, smoking, physical activity, sleep duration during weekdays and during the weekend, alcohol consumption, total fiber intake, cholesterol intake, and total energy intake
Model 3: as in model 2 and additionally adjusted for cardiovascular risk factors: total serum cholesterol, HDL serum cholesterol, systolic and diastolic blood pressure, body mass index, and diabetes
*Energy adjusted by the residual method
†Lowest category: CACS of 0; the two highest categories: CACS > 0 and < 100 together with CACS ≥ 100
γTwo lowest categories: CACS of 0 together with CACS > 0 and < 100; highest category: CACS ≥ 100
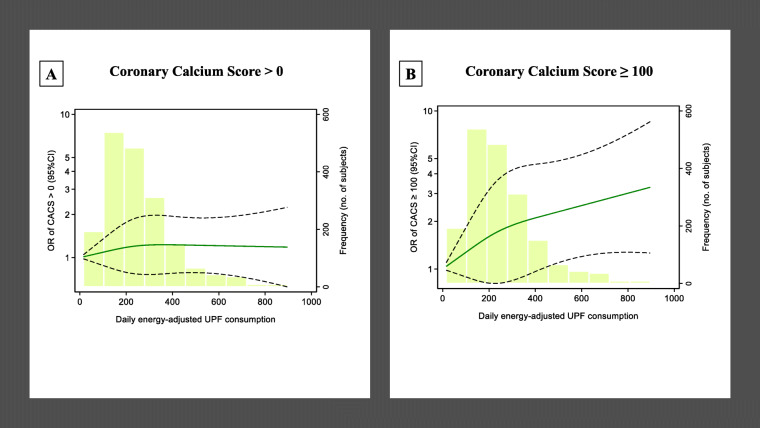
Similar results were observed when performing the standard binary logistic regression to estimate OR for CACS > 0 (with CACS of 0 as reference) and for CACS ≥ 100 (with CACS < 100 as reference) (Additional File 1:Table S2). Thus, a clear dose-response relationship between UPF consumption and coronary artery calcium was only appreciated for CACS ≥ 100 compared to those with CACS < 100 (Fig. 2).
Fig. 2.
Restricted cubic splines for the association of Coronary Artery Calcium (CACS) and ultra-processed food (UPF) consumption, in the AWHS cohort study (N = 1876). The standard binary logistic regression was used to perform restricted cubic splines with 3 knots of the distribution (at the 10th, 50th, and 90th percentiles of the distribution). Participants with an exposure above the 99th percentile were not included. Dashed lines represent 95% CIs. The histograms show the distributions of energy-adjusted ultra-processed food consumption. a The odds of CACS > 0 (p value of the Wald test for non-linearity is 0.59) and b the odds of CACS > 100 (p value of the Wald test for non-linearity is 0.029) as ultra-processed food consumption increases. Models adjusted for age, marital status, education, smoking, physical activity, sleep duration during weekdays and during the weekend, alcohol consumption, total fiber intake, cholesterol intake, total energy intake, and cardiovascular risk factors: total serum cholesterol, HDL serum cholesterol, systolic and diastolic blood pressure, body mass index, and diabetes. AWHS, Aragon Workers’ Health Study; CACS, Coronary Agatston Calcium Score; UPF, ultra-processed food; OR, odds ratio; CI, confidence interval
No interactions were detected between UPF consumption and age (p = 0.68), BMI (p = 0.25), smoking status (p = 0.15), alcohol consumption (p = 0.31), and physical activity (p = 0.61).
Discussion
This is the first epidemiological study assessing the association between UPF consumption and early subclinical atherosclerosis. In this sample of middle-aged male workers, those with the highest consumption of UPF (on average approximately 500 g/day) compared with those with the lowest consumption (on average approximately 100 g/day) have a 2-fold increased risk of having a subclinical coronary atherosclerosis outlined by a CACS ≥ 100. This association was independent of the main cardiometabolic risk factors (cholesterol level, blood pressure, BMI, and diabetes), as well as dietary and lifestyle factors. Results were robust and remained similar using different methodological approaches. When we categorized the coronary calcium as CACS ≤ 0 vs. CACS > 0, we classified as having a “positive outcome”/“positive in atherosclerosis” a very heterogeneous group of participants with mixing characteristics, including those with CACS very close to 0 and those with mild, moderate, and even severe subclinical coronary atherosclerosis. This lack of specification and the fact that subjects with very small and incipient lesions (and in some cases with the coronary calcium almost expected by age) are classified as “positive outcome”/“positive in atherosclerosis” may be the reason for not having found an association when comparing CACS > 0 vs. CACS ≤ 0. In contrast, in the second categorization (CACS < 100 vs. CACS ≥ 100), by establishing the cutoff point at a CACS equal to 100, we classified as “positive outcome”/“positive in atherosclerosis” those with a well-defined and more established disease.
Scientific evidence has placed fresh fruit, vegetables, whole grains, nuts, legumes, and olive oil—for their high content of fiber and micronutrients with antioxidant and anti-inflammatory properties—as the most protective foods for the cardiovascular system [42, 43]. Despite all this knowledge, during the last decade, there has been a worldwide rapid increase in the consumption of UPF, in which these healthy components are scarce, due to the prevailing fact that UPF is easily accessible, tasty, and cheap [44].
Of particular concern is that (i) UPF is highly energy dense and is usually consumed in large portion sizes; (ii) UPF contains excessive salt, saturated fat, and refined sugars, while lacking fiber and micronutrients such as vitamins and antioxidants; (iii) additionally, potentially harmful compounds may be added or generated during UPF processing (such as colorants, additives, acrylamide, trans-fatty acids (TFAs)). Several of these UPF characteristics are known risk factors for cardiometabolic conditions [15], as we explain next.
To begin with, dense food and sugar-sweetened beverages might delay the trigger of the internal satiety signal, leading to excessive caloric ingestion [45]. Excessive intake of energy, fat, and sugar contributes to weight gain and increases the risk of obesity [16], which is a major risk factor for CVD. However, the associations observed in this study between consumption of UPF and subclinical coronary atherosclerosis were statistically significant even after adjusting for BMI. Thus, BMI does not fully explain the association between UPF and subclinical atherosclerosis.
Most of the salt intake in high-income nations comes from UPF. Among them, bread and bakery products, cereals and grains, meat products, and dairy products are the most significant contributors to dietary salt [46]. The high salt content of these industrial products may also partly contribute to the appearance of hypertension [47], endothelial dysfunction [22, 48], and, as a consequence, also CVD [49, 50].
Moreover, for the industrial production of UPF, vegetable oils (the most used due to their low cost) are hydrogenated. If the hydrogenation is total, saturated fat is formed, but if the hydrogenation is partial, TFAs are also produced. These partially hydrogenated oils are consumed in margarine, fast food, and other UPF such as cakes, rolls, confectionery, biscuits, chocolate, potato chips, and crisps. A relationship between TFA intake and increased risk of CVD has been established [51, 52]. In a meta-analysis of prospective studies, a 2% increase in total daily energy intake from TFAs was associated with a 23% increased risk of CVD [53]. In addition, it has been observed that TFAs increase the incorporation of calcium to vascular endothelium cells [54]. Likewise, controlled dietary trials have shown that TFAs have markedly adverse effects on serum lipids [55], raising serum concentrations of LDL cholesterol [56], while also decreasing the serum concentration of HDL cholesterol [57]. TFAs have also shown to rise inflammation markers including C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α) [58]. All these factors contribute independently to the development of atherosclerosis [22]. It should be mentioned, however, that the food industry has made remarkable efforts to reduce TFAs these past few years. Consequently, their presence in current UPF may be small [59].
UPF is also much rich in saturated fatty acids (SFAs) than in monounsaturated fatty acids (MUFAs) or polyunsaturated fatty acids (PUFAs). Higher intake of SFAs from pastries and processed food has been associated with a higher risk of CVD [60]. Likewise, the isocaloric substitution of SFAs or TFAs with MUFAs or PUFAs has been consistently associated with a lower risk of CVD and death, both in cohort studies [61] and in randomized controlled trials [62] .
Refined sugars and sweeteners added in UPF have been described as implicated in the development of CVD [63, 64] and its risk factors, such as hypertension [65], diabetes [66], metabolic syndrome [67], and obesity [64].
Food additives in UPF are of special concern. Some of them, such as sulphites [12] and monosodium glutamate [11], have shown several adverse effects on cardiovascular health in experimental studies on cellular models and animals. Likewise, it has been found that long-term consumption of acesulfame K (non-caloric artificial sweetener) might accelerate atherosclerosis in cellular models [10]. However, among the additives, phosphates deserve special mention [68]. UPFs with high amounts of added phosphates are processed meat, ham, sausages, canned fish, baked goods, cola drinks, and other soft drinks. Phosphorus in inorganic phosphate coming from UPF is very effectively absorbed in the gastrointestinal tract (absorbed by approximately 90%) with respect to naturally occurring phosphorus in food (absorbed by 40–60%) [69]. Phosphate induces vascular calcification both in vitro and in vivo [13, 70]. The promoted process is not merely the passive precipitation of calcium by phosphate, but rather an active cellular process in which smooth-muscle cells in blood vessels are reprogrammed to become osteoblast-like cells [13]. This alteration also seems to occur in the human arteries [71, 72]. Moreover, it has been shown that increased phosphate intake leads to an endothelial-cell function impairment in the vascular system, in both animals and humans [73]. High to normal serum phosphate concentrations are associated with coronary calcification in young healthy men [74] and were found to be a predictor of cardiovascular events in the Framingham study [75].
Neo-formed substances which are produced through packaging, moisture removal, heat treatments, chilling and freezing, acidity control, reaction with chemical additives, and irradiation might also contribute to the harmful effect derived from UPF consumption. An example of a neo-formed substance from packaging is bisphenol A, which has been related to CVD [76]. Likewise, acrylamide, which is produced by heat treatments and found in fried potatoes, biscuits, bread, processed meat, and even coffee, has also been associated with CVD [77, 78].
Further research is needed to identify what specific processes, compounds, or UPF subtypes play an important role in this association found between UPF consumption and increased risk of early atherosclerosis, also taking into account the possibility of synergic effects among the abovementioned mechanisms. This knowledge will allow, in the short term, to recommend a reduction of the consumption of these products and, in the long term, to refine the processes of the food industry with the aim of providing a healthier offer.
Some limitations of our study must be recognized. First, the cross-sectional design of our study prevents us from establishing a causal link between consumption of UPF and subclinical coronary atherosclerosis. However, since calcium in the coronary artery is subclinical, reverse causation is highly unlikely. Also, although we adjust for a wide range of potential confounders, we cannot rule out residual confounding.
Although the FFQ provides an adequate assessment of an individual’s usual diet [35], because of its self-reported nature and the potential recall bias, inaccuracies in the exposure assessment cannot be ruled out. Likewise, the FFQ was not designed specifically to collect data on UPF following the methodology of the NOVA classification, which could lead to misclassification. Nonetheless, the applied methodology is the most frequently used classification of UPF in epidemiological studies. Despite the NOVA classification being reproducible and easily incorporated into messages and its consequent utility for public health, it is not exempted from controversies [79, 80].
We should note that the CACS fails to capture information about the regional distribution of calcification within the coronary tree and does not incorporate information on the number or size of calcified coronary lesions. The limited external validity of our findings should also be mentioned, as the cohort was not representative of the general population.
This study notably presents important strengths, such as its novelty and the quality of the methodology used to collect clinical data and to quantify coronary calcium, which is a measurement with strong published support of its value for clinical risk prediction. Also, the detailed data collection for confounders, including accurate measurements of blood pressure and serum lipids, helps reduce confounding. Finally, another asset is the consistency of the findings after using different statistical approaches to assess the association between UPF and subclinical atherosclerosis.
Conclusion
In conclusion, in this study of asymptomatic Spanish working men, we found that those consuming the highest amount of UPF had twice as much probability of having subclinical coronary atherosclerosis, regardless of blood lipids, hypertension, BMI, and other cardiovascular risk factors.
Supplementary information
Additional file 1: Table S1 Food-items included as UPF; Table S2 UPF-CACS association.
Acknowledgments
Our thanks to the Juan de la Cierva post-doctoral scholarship-training awarded to CD-V from the Ministry of Spain.
Abbreviations
- AWHS
Aragon Workers’ Health Study
- BMI
Body mass index
- CACS
Agatston's Coronary Artery Calcium Score (CACS)
- CI
Confidence interval
- CVD
Cardiovascular disease
- OR
Odds ratio
- UPF
Ultra-processed food
Authors’ contributions
PG-C conceived the presented idea. CD-V and HMS performed the computations and were the major contributors in writing the manuscript. PG-C and ML verified the analytical methods and supervised the findings of this work. All authors read and approved the final manuscript.
Funding
AWHS was funded through a collaboration agreement between the Aragonese Institute of Health Sciences (I+CS) of the Regional Government of Aragon, the National Cardiovascular Research Centre (CNIC) of the Carlos III Health Institute, and Opel Spain. This study was also partially supported by grants: PI17/1709 (Secretary of State for R&D and ERDF/ESF), and Integrated Projects of Excellence in Health Research Institutes PIE16/00022 (Secretary of State for R&D and ERDF/ESF), the ATHLOS Project (EU H2020-ID project: 635316), CIBERCV and CIBERESP of the Carlos III Health Institute, Madrid, Spain.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the central Institutional Review Board of Aragón (CEICA), the National Center for Cardiovascular Research (CNIC), and the management and employee representatives of General Motors, Spain.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Table S1 displays the food-items in the AWHS food frequency questionnaire classified as ultra-processed foods according to degree of processing (NOVA group 4). Table S2 Association between Agatston's Coronary Artery Calcium Score and quartiles of UPF consumption by using the standard binary logistic regression. The =R(95% CI) for CACS > 0 (compared with CACS score ≤ 0) and for CACS score ≥ 100 (compared to CACS score < 100) are displayed. Supplementary information accompanies this paper at 10.1186/s12916-020-01678-8.
References
- 1.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14(Suppl 2):21–28. doi: 10.1111/obr.12107. [DOI] [PubMed] [Google Scholar]
- 2.Blanco-Rojo R, Sandoval-Insausti H, Lopez-Garcia E, Graciani A, Ordovas JM, Banegas JR, et al. Consumption of ultra-processed foods and mortality: a national prospective cohort in Spain. Mayo Clin Proc. 2019;94(11):2178–2188. doi: 10.1016/j.mayocp.2019.03.035. [DOI] [PubMed] [Google Scholar]
- 3.Latasa P, Louzada M, Martinez Steele E, Monteiro CA. Added sugars and ultra-processed foods in Spanish households (1990-2010) Eur J Clin Nutr. 2018;72(10):1404–1412. doi: 10.1038/s41430-017-0039-0. [DOI] [PubMed] [Google Scholar]
- 4.Slimani N, Deharveng G, Southgate DA, Biessy C, Chajes V, van Bakel MM, et al. Contribution of highly industrially processed foods to the nutrient intakes and patterns of middle-aged populations in the European Prospective Investigation into Cancer and Nutrition study. Eur J Clin Nutr. 2009;63(Suppl 4):S206–S225. doi: 10.1038/ejcn.2009.82. [DOI] [PubMed] [Google Scholar]
- 5.Food, Nations AOotU. Guidelines on the collection of information on food processing through food consumption surveys. Food and Agriculture Organization of the United Nations Rome; 2015.
- 6.Monteiro CA, Cannon G, Levy R, Moubarac J-C, Jaime P, Martins AP, et al. NOVA. The star shines bright. 2016;7(1–3):28–38. [Google Scholar]
- 7.Merchant AT, Kelemen LE, de Koning L, Lonn E, Vuksan V, Jacobs R, et al. Interrelation of saturated fat, trans fat, alcohol intake, and subclinical atherosclerosis. Am J Clin Nutr. 2008;87(1):168–174. doi: 10.1093/ajcn/87.1.168. [DOI] [PubMed] [Google Scholar]
- 8.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174(4):516–524. doi: 10.1001/jamainternmed.2013.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao X, Yang X, Zhang X, Li Y, Zhao X, Ren L, et al. Dietary salt intake and coronary atherosclerosis in patients with prehypertension. J Clin Hypertens (Greenwich) 2014;16(8):575–580. doi: 10.1111/jch.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jang W, Jeoung NH, Cho KH. Modified apolipoprotein (apo) A-I by artificial sweetener causes severe premature cellular senescence and atherosclerosis with impairment of functional and structural properties of apoA-I in lipid-free and lipid-bound state. Mol Cells. 2011;31(5):461–470. doi: 10.1007/s10059-011-1009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh K, Ahluwalia P. Effect of monosodium glutamate on lipid peroxidation and certain antioxidant enzymes in cardiac tissue of alcoholic adult male mice. J Cardiovasc Dis Res. 2012;3(1):12–18. doi: 10.4103/0975-3583.91595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Q, Bai Y, Yang Z, Tian J, Meng Z. The molecular mechanisms of sodium metabisulfite on the expression of K ATP and L-Ca2+ channels in rat hearts. Regul Toxicol Pharmacol. 2015;72(3):440–446. doi: 10.1016/j.yrtph.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Giachelli CM. The emerging role of phosphate in vascular calcification. Kidney Int. 2009;75(9):890–897. doi: 10.1038/ki.2008.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srour B, Fezeu LK, Kesse-Guyot E, Alles B, Mejean C, Andrianasolo RM, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Sante) BMJ. 2019;365:l1451. doi: 10.1136/bmj.l1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silva Meneguelli T, Viana Hinkelmann J, Hermsdorff HHM, Zulet MA, Martinez JA, Bressan J. Food consumption by degree of processing and cardiometabolic risk: a systematic review. Int J Food Sci Nutr. 2020:1–15. [DOI] [PubMed]
- 16.Mendonca RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes AC, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr. 2016;104(5):1433–1440. doi: 10.3945/ajcn.116.135004. [DOI] [PubMed] [Google Scholar]
- 17.Mendonça RD, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra Project. Am J Hypertens. 2017;30(4):358–366. doi: 10.1093/ajh/hpw137. [DOI] [PubMed] [Google Scholar]
- 18.Rauber F, Campagnolo PD, Hoffman DJ, Vitolo MR. Consumption of ultra-processed food products and its effects on children's lipid profiles: a longitudinal study. Nutr Metab Cardiovasc Dis. 2015;25(1):116–122. doi: 10.1016/j.numecd.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Srour B, Fezeu LK, Kesse-Guyot E, Alles B, Debras C, Druesne-Pecollo N, et al. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Sante prospective cohort. JAMA Intern Med. 2019;180(2):283-291. [DOI] [PMC free article] [PubMed]
- 20.Kim H, Hu EA, Rebholz CM. Ultra-processed food intake and mortality in the USA: results from the Third National Health and Nutrition Examination Survey (NHANES III, 1988-1994) Public Health Nutr. 2019;22(10):1777–1785. doi: 10.1017/S1368980018003890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rico-Campa A, Martinez-Gonzalez MA, Alvarez-Alvarez I, Mendonca RD, de la Fuente-Arrillaga C, Gomez-Donoso C, et al. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ. 2019;365:l1949. doi: 10.1136/bmj.l1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993;362(6423):801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 23.Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, Blumenthal RS, et al. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2009;53(4):345–352. doi: 10.1016/j.jacc.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lo-Kioeng-Shioe MS, Rijlaarsdam-Hermsen D, van Domburg RT, Hadamitzky M, Lima JAC, Hoeks SE, et al. Prognostic value of coronary artery calcium score in symptomatic individuals: a meta-analysis of 34,000 subjects. Int J Cardiol. 2020;299:56–62. doi: 10.1016/j.ijcard.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Tota-Maharaj R, Blaha MJ, Blankstein R, Silverman MG, Eng J, Shaw LJ, et al. Association of coronary artery calcium and coronary heart disease events in young and elderly participants in the multi-ethnic study of atherosclerosis: a secondary analysis of a prospective, population-based cohort. Mayo Clin Proc. 2014;89(10):1350–1359. doi: 10.1016/j.mayocp.2014.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blaha MJ, Mortensen MB, Kianoush S, Tota-Maharaj R, Cainzos-Achirica M. Coronary artery calcium scoring: is it time for a change in methodology? JACC Cardiovasc Imaging. 2017;10(8):923–937. doi: 10.1016/j.jcmg.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Hecht H, Blaha MJ, Berman DS, Nasir K, Budoff M, Leipsic J, et al. Clinical indications for coronary artery calcium scoring in asymptomatic patients: expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2017;11(2):157–168. doi: 10.1016/j.jcct.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 29.Leening MJ, Elias-Smale SE, Kavousi M, Felix JF, Deckers JW, Vliegenthart R, et al. Coronary calcification and the risk of heart failure in the elderly: the Rotterdam study. JACC Cardiovasc Imaging. 2012;5(9):874–880. doi: 10.1016/j.jcmg.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 30.Hermann DM, Gronewold J, Lehmann N, Moebus S, Jockel KH, Bauer M, et al. Coronary artery calcification is an independent stroke predictor in the general population. Stroke. 2013;44(4):1008–1013. doi: 10.1161/STROKEAHA.111.678078. [DOI] [PubMed] [Google Scholar]
- 31.Casasnovas JA, Alcaide V, Civeira F, Guallar E, Ibanez B, Borreguero JJ, et al. Aragon workers’ health study--design and cohort description. BMC Cardiovasc Disord. 2012;12:45. doi: 10.1186/1471-2261-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laclaustra M, Casasnovas JA, Fernandez-Ortiz A, Fuster V, Leon-Latre M, Jimenez-Borreguero LJ, et al. Femoral and carotid subclinical atherosclerosis association with risk factors and coronary calcium: the AWHS study. J Am Coll Cardiol. 2016;67(11):1263–1274. doi: 10.1016/j.jacc.2015.12.056. [DOI] [PubMed] [Google Scholar]
- 33.Martinez-Gonzalez MA, Lopez-Fontana C, Varo JJ, Sanchez-Villegas A, Martinez JA. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005;8(7):920–927. doi: 10.1079/phn2005745. [DOI] [PubMed] [Google Scholar]
- 34.de la Fuente-Arrillaga C, Ruiz ZV, Bes-Rastrollo M, Sampson L, Martinez-Gonzalez MA. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010;13(9):1364–1372. doi: 10.1017/S1368980009993065. [DOI] [PubMed] [Google Scholar]
- 35.Fernández-Ballart JD, Piñol JL, Zazpe I, Corella D, Carrasco P, Toledo E, et al. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain 2010;103(12):1808–1816. [DOI] [PubMed]
- 36.Martin-Moreno JM, Boyle P, Gorgojo L, Maisonneuve P, Fernandez-Rodriguez JC, Salvini S, et al. Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol. 1993;22(3):512–519. doi: 10.1093/ije/22.3.512. [DOI] [PubMed] [Google Scholar]
- 37.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124(1):17–27. doi: 10.1093/oxfordjournals.aje.a114366. [DOI] [PubMed] [Google Scholar]
- 38.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 39.Erbel R, Mohlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol. 2010;56(17):1397–1406. doi: 10.1016/j.jacc.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 40.Williams RJTJoMS. Understanding and interpreting generalized ordered logit models. 2016;40(1):7–20.
- 41.Ahmed HM, Blaha MJ, Nasir K, Jones SR, Rivera JJ, Agatston A, et al. Low-risk lifestyle, coronary calcium, cardiovascular events, and mortality: results from MESA. Am J Epidemiol. 2013;178(1):12–21. doi: 10.1093/aje/kws453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, et al. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004;292(12):1440–1446. doi: 10.1001/jama.292.12.1440. [DOI] [PubMed] [Google Scholar]
- 43.Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts 2018;378(25):e34. [DOI] [PubMed]
- 44.Waterlander WE, de Haas WE, van Amstel I, Schuit AJ, Twisk JW, Visser M, et al. Energy density, energy costs and income - how are they related? Public Health Nutr. 2010;13(10):1599–1608. doi: 10.1017/S1368980009992989. [DOI] [PubMed] [Google Scholar]
- 45.Benelam B. Satiety and the anorexia of ageing. Br J Community Nurs. 2009;14(8):332–335. doi: 10.12968/bjcn.2009.14.8.43512. [DOI] [PubMed] [Google Scholar]
- 46.Bhat S, Marklund M, Henry ME, Appel LJ, Croft KD, Neal B, et al. A systematic review of the sources of dietary salt around the world. Advances in nutrition (Bethesda, Md). 2020. [DOI] [PMC free article] [PubMed]
- 47.Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. doi: 10.1136/bmj.f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tzemos N, Lim PO, Wong S, Struthers AD, MacDonald TM. Adverse cardiovascular effects of acute salt loading in young normotensive individuals. Hypertension. 2008;51(6):1525–1530. doi: 10.1161/HYPERTENSIONAHA.108.109868. [DOI] [PubMed] [Google Scholar]
- 49.He FJ, MacGregor GA. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol. 2018;15(6):371–377. doi: 10.1038/s41569-018-0004-1. [DOI] [PubMed] [Google Scholar]
- 50.Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oh K, Hu FB, Manson JE, Stampfer MJ, Willett WC. Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the nurses’ health study. Am J Epidemiol. 2005;161(7):672–679. doi: 10.1093/aje/kwi085. [DOI] [PubMed] [Google Scholar]
- 52.Oomen CM, Ocke MC, Feskens EJ, van Erp-Baart MA, Kok FJ, Kromhout D. Association between trans fatty acid intake and 10-year risk of coronary heart disease in the Zutphen Elderly Study: a prospective population-based study. Lancet (London, England) 2001;357(9258):746–751. doi: 10.1016/s0140-6736(00)04166-0. [DOI] [PubMed] [Google Scholar]
- 53.Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354(15):1601–1613. doi: 10.1056/NEJMra054035. [DOI] [PubMed] [Google Scholar]
- 54.Ballesteros-Vásquez M, Valenzuela-Calvillo L, Artalejo-Ochoa E, Robles-Sardin AE. Ácidos grasos trans: un análisis del efecto de su consumo en la salud humana, regulación del contenido en alimentos y alternativas para disminuirlos. Nutr Hosp. 2012;27(1):54–64. doi: 10.1590/S0212-16112012000100007. [DOI] [PubMed] [Google Scholar]
- 55.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77(5):1146–1155. doi: 10.1093/ajcn/77.5.1146. [DOI] [PubMed] [Google Scholar]
- 56.Mauger JF, Lichtenstein AH, Ausman LM, Jalbert SM, Jauhiainen M, Ehnholm C, et al. Effect of different forms of dietary hydrogenated fats on LDL particle size. Am J Clin Nutr. 2003;78(3):370–375. doi: 10.1093/ajcn/78.3.370. [DOI] [PubMed] [Google Scholar]
- 57.Matthan NR, Welty FK, Barrett PH, Harausz C, Dolnikowski GG, Parks JS, et al. Dietary hydrogenated fat increases high-density lipoprotein apoA-I catabolism and decreases low-density lipoprotein apoB-100 catabolism in hypercholesterolemic women. Arterioscler Thromb Vasc Biol. 2004;24(6):1092–1097. doi: 10.1161/01.ATV.0000128410.23161.be. [DOI] [PubMed] [Google Scholar]
- 58.Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, et al. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction. J Nutr. 2005;135(3):562–566. doi: 10.1093/jn/135.3.562. [DOI] [PubMed] [Google Scholar]
- 59.Perez-Farinos N, Dal Re Saavedra MA, Villar Villalba C, Robledo de Dios T. Trans-fatty acid content of food products in Spain in 2015. Gac Sanit 2016;30(5):379–382. [DOI] [PubMed]
- 60.Guasch-Ferre M, Babio N, Martinez-Gonzalez MA, Corella D, Ros E, Martin-Pelaez S, et al. Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am J Clin Nutr. 2015;102(6):1563–1573. doi: 10.3945/ajcn.115.116046. [DOI] [PubMed] [Google Scholar]
- 61.Jakobsen MU, O’Reilly EJ, Heitmann BL, Pereira MA, Balter K, Fraser GE, et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89(5):1425–1432. doi: 10.3945/ajcn.2008.27124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hooper L, Summerbell CD, Thompson R, Sills D, Roberts FG, Moore HJ, et al. Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane Database of Systematic Reviews. Version published: 16 May 2012 Available in: 10.1002/14651858.CD002137.pub3. [DOI] [PMC free article] [PubMed]
- 63.de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation. 2012;125(14):1735–1741. doi: 10.1161/CIRCULATIONAHA.111.067017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121(11):1356–1364. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brown IJ, Stamler J, Van Horn L, Robertson CE, Chan Q, Dyer AR, et al. Sugar-sweetened beverage, sugar intake of individuals, and their blood pressure: international study of macro/micronutrients and blood pressure. Hypertension. 2011;57(4):695–701. doi: 10.1161/HYPERTENSIONAHA.110.165456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murray I, Kazman S. Sugar-sweetened beverages, weight gain, and diabetes. JAMA. 2005;293(4):422. doi: 10.1001/jama.293.4.422-b. [DOI] [PubMed] [Google Scholar]
- 67.Martinez Steele E, Juul F, Neri D, Rauber F, Monteiro CA. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev Med. 2019;125:40–48. doi: 10.1016/j.ypmed.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 68.Karalis M, Murphy-Gutekunst L. Enhanced foods: hidden phosphorus and sodium in foods commonly eaten. J Ren Nutr. 2006;16(1):79–81. doi: 10.1053/j.jrn.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 69.Uribarri J. Phosphorus homeostasis in normal health and in chronic kidney disease patients with special emphasis on dietary phosphorus intake. Semin Dial. 2007;20(4):295–301. doi: 10.1111/j.1525-139X.2007.00309.x. [DOI] [PubMed] [Google Scholar]
- 70.Stubbs JR, Liu S, Tang W, Zhou J, Wang Y, Yao X, et al. Role of hyperphosphatemia and 1,25-dihydroxyvitamin D in vascular calcification and mortality in fibroblastic growth factor 23 null mice. J Am Soc Nephrol. 2007;18(7):2116–2124. doi: 10.1681/ASN.2006121385. [DOI] [PubMed] [Google Scholar]
- 71.Moe SM, O’Neill KD, Duan D, Ahmed S, Chen NX, Leapman SB, et al. Medial artery calcification in ESRD patients is associated with deposition of bone matrix proteins. Kidney Int. 2002;61(2):638–647. doi: 10.1046/j.1523-1755.2002.00170.x. [DOI] [PubMed] [Google Scholar]
- 72.Shroff RC, McNair R, Skepper JN, Figg N, Schurgers LJ, Deanfield J, et al. Chronic mineral dysregulation promotes vascular smooth muscle cell adaptation and extracellular matrix calcification. J Am Soc Nephrol. 2010;21(1):103–112. doi: 10.1681/ASN.2009060640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shuto E, Taketani Y, Tanaka R, Harada N, Isshiki M, Sato M, et al. Dietary phosphorus acutely impairs endothelial function. J Am Soc Nephrol. 2009;20(7):1504–1512. doi: 10.1681/ASN.2008101106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA. Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol. 2009;20(2):397–404. doi: 10.1681/ASN.2008020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dhingra R, Sullivan LM, Fox CS, Wang TJ, D’Agostino RB, Sr, Gaziano JM, et al. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med. 2007;167(9):879–885. doi: 10.1001/archinte.167.9.879. [DOI] [PubMed] [Google Scholar]
- 76.Rancière F, Lyons JG, Loh VH, Botton J, Galloway T, Wang T, et al. Bisphenol A and the risk of cardiometabolic disorders: a systematic review with meta-analysis of the epidemiological evidence. Envioron Health. 2015;14(1):46. doi: 10.1186/s12940-015-0036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.DeJarnett N, Conklin DJ, Riggs DW, Myers JA, O’Toole TE, Hamzeh I, et al. Acrolein exposure is associated with increased cardiovascular disease risk. J Am Heart Assoc. 2014;3(4):e000934. 10.1161/JAHA.114.000934. [DOI] [PMC free article] [PubMed]
- 78.Zhang Y, Huang M, Zhuang P, Jiao J, Chen X, Wang J, et al. Exposure to acrylamide and the risk of cardiovascular diseases in the National Health and Nutrition Examination Survey 2003-2006. Environ Int. 2018;117:154–163. doi: 10.1016/j.envint.2018.04.047. [DOI] [PubMed] [Google Scholar]
- 79.Gibney MJ, Forde CG, Mullally D, Gibney ER. Ultra-processed foods in human health: a critical appraisal. Am J Clin Nutr. 2017;106(3):717–724. doi: 10.3945/ajcn.117.160440. [DOI] [PubMed] [Google Scholar]
- 80.Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. Ultra-processing. An odd ‘appraisal’. Public Health Nutr. 2018;21(3):497–501. doi: 10.1017/S1368980017003287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1 Food-items included as UPF; Table S2 UPF-CACS association.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.