Abstract
Immune checkpoint blockade (ICB) therapies such as anti-programmed death 1 (PD-1) and anti-CTLA-4 (cytotoxic T lymphocyte-associated protein 4) have dramatically transformed treatment in solid tumor oncology. While immunotherapeutic approaches such as stem cell transplantation and anti-cancer monoclonal antibodies have made critical contributions to improve outcomes in hematological malignancies, clinical benefits of ICB are observed in only limited tumor types that are particularly characterized by a high infiltration of immune cells. Importantly, even patients that initially respond to ICB are unable to achieve long-term disease control using these therapies. Indeed, primary and acquired resistance mechanisms are differentially orchestrated in hematological malignancies depending on tumor types and/or genotypes, and thus, an in-depth understanding of the disease-specific immune microenvironments will be essential in improving efficacy. In addition to PD-1 and CTLA-4, various T cell immune checkpoint molecules have been characterized that regulate T cell responses in a non-redundant manner. Several lines of evidence suggest that these T cell checkpoint molecules might play unique roles in hematological malignancies, highlighting their potential as therapeutic targets. Targeting innate checkpoint molecules on natural killer cells and/or macrophages has also emerged as a rational approach against tumors that are resistant to T cell-mediated immunity. Given that various monoclonal antibodies against tumor surface proteins have been clinically approved in hematological malignancies, innate checkpoint blockade might play a key role to augment antibody-mediated cellular cytotoxicity and phagocytosis. In this review, we discuss recent advances and emerging roles of immune checkpoint blockade in hematological malignancies.
Keywords: Immunotherapy, Immune checkpoint molecule, Tumor microenvironment, Hematological malignancy
Background
Immunotherapy has emerged as a new pillar of cancer treatment. Over the past decade, immune checkpoint blockade (ICB) therapies such as monoclonal antibodies (mAbs) that target cytotoxic T lymphocyte-associated protein 4 (CTLA-4) or the programmed cell death protein 1 (PD-1) pathway have dramatically changed therapeutic strategies in certain types of advanced malignancies. Humanized anti-CTLA-4 antibody, ipilimumab, reportedly doubles 10-year survival rates for metastatic melanoma compared to historical control data, and its FDA approval marked a turning point for immunotherapy [1, 2]. Blockade of PD-1 or its ligand, PD-1 ligand (PD-L1), has displayed superior clinical responses with fewer side effects in a broad range of cancers [3–9].
Historically, immunotherapy has been well-studied in hematological malignancies as supported by the success of stem cell transplantation (SCT) and various mAbs against tumor surface proteins. While newly developed ICB therapies are actively being tested, primary and acquired resistance remain major barriers in utilizing them against a broad range of hematological malignancies. To this end, it is critically important to understand the complex immune regulatory mechanisms mediated by immune checkpoint molecules as well as the disease-specific immune milieu. In addition to therapeutic blockade of PD-1 and CTLA-4, various immune checkpoint molecules that regulate innate and/or adaptive immune responses have emerged as potential therapeutic targets. In this review, we will provide an overview of the basic and clinical aspects of ICB therapy and discuss their potential in harnessing anti-tumor immunity in hematological malignancies.
Immune regulation by PD-1 and CTLA-4
Over the past decade, various ICB drugs have received FDA approval including anti-CTLA-4 (ipilumumab), anti-PD-1 (pembrolizumab, nivolumab, and cemiplimab), and anti-PD-L1 (atezolizumab, avelumab, and durvalumab). It is appreciated that the interaction between CTLA-4 and its ligands CD80 (B7-1) and CD86 (B7-2) critically regulates T cell priming at the interface between T cells and antigen-presenting cells (APCs), whereas the interaction between PD-1/PD-L1 controls T cell responses at the effector phase [10]. Immune-related adverse events (irAEs) are commonly seen in patients treated with either anti-CTLA-4 or anti-PD-1/PD-L1, but the incidence of severe irAEs (grade 3 or 4) is much more frequent in patients treated with CTLA-4 blockade [11]. It should be noted that even after clinical approval of these therapies, a number of studies have revealed new molecular mechanisms of immune regulation by PD-1 and CTLA-4. Their immune regulatory mechanisms are far more complicated; therefore, an in-depth understanding of the complex interplay will provide new insights into the mechanisms of ICB therapies.
CTLA-4
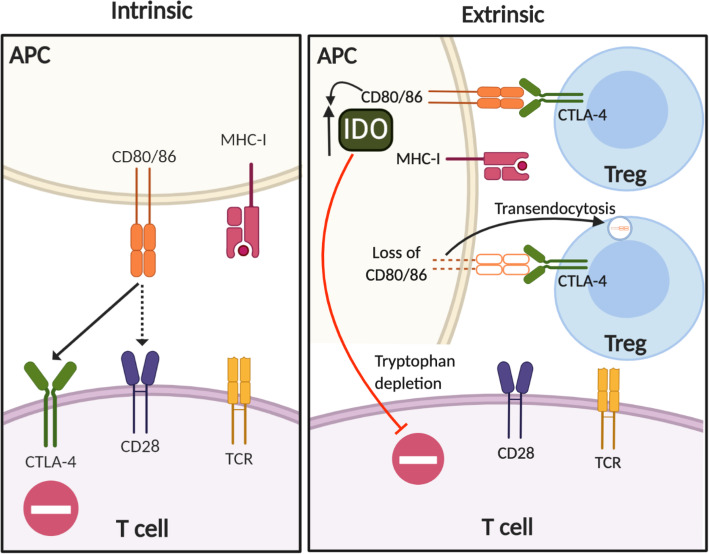
CTLA-4 expression and function are intrinsically associated with T cell activation (Fig. 1, left). Upon T cell receptor (TCR) engagement, CTLA-4 is upregulated with peak expression occurring 2 to 3 days after activation [12]. CTLA-4 accumulates at the immunological synapse between T cells and APCs, where CTLA-4 is stabilized by CD80 ligand binding [13, 14]. Due to its higher avidity and affinity for CD80/CD86, CTLA-4 competes with the costimulatory molecule CD28 leading to the negative regulation of activated T cells [15–17].
Fig. 1.
CTLA-4-mediated immune regulation. Schematic illustrating T cell-intrinsic (left) and extrinsic regulation by CTLA-4 (right). Left: CTLA-4 is upregulated on activated T cells and competes with the CD28 co-stimulatory receptor due to its higher affinity for CD80/CD86. Right: CTLA-4 plays a critical role in Treg-mediated immune regulation. The CTLA-4/CD80 interaction between Treg/APCs induces indoleamine 2,3-dioxygenase (IDO), a key enzyme that suppresses T cells by tryptophan deprivation. Additionally, Tregs down-modulate CD80/86 expression on APCs by transendocytosis
In addition to cell-intrinsic regulation, CTLA-4 also regulates T cell activation in a cell-extrinsic manner that is primarily mediated by regulatory T cells (Tregs) (Fig. 1, right) [18, 19]. Indeed, Treg-specific deletion of CTLA-4 results in aberrant T cell activation and autoimmunity highlighting CTLA-4 as a key functional molecule for Treg-mediated immune tolerance [20, 21]. Of note, extrinsic regulation by CTLA-4 cannot be simply explained by the competitive inhibition of the interaction between CD28 and CD80/86 at the immunological synapse. For example, the interaction between CTLA-4 and CD80/86 upregulates indoleamine 2,3-dioxygenase (IDO) in DCs, a key enzyme for tryptophan catabolism [22]. Thus, the interaction between Tregs and DCs limits antigen-specific T cell responses by IDO-mediated tryptophan depletion.
Another regulatory mechanism of CTLA-4 is its ability to rapidly capture CD80/CD86 from APCs by a process of trans-endocytosis [23]. Although both effector lymphocytes and Tregs are known to have the ability to mediate CTLA-4-dependent deprivation of CD80/CD86 from APCs [24], Ovcinnikovs et al. recently demonstrated that Tregs, rather than activated conventional T cells, are predominantly responsible for the trans-endocytosis of CD80/CD86 in vivo [25]. They also showed that migratory DCs, rather than tissue resident DCs in lymph nodes, are the major target for CTLA-4-dependent deprivation of CD80/CD86, providing an important mechanistic insight into anti-CTLA-4 therapy [25]. While the CTLA-4-dependent trans-endocytosis of CD80/86 and subsequent degradation of these ligands contribute to immune tolerance, CTLA-4 itself is constitutively internalized in a ligand-independent manner, undergoing both recycling and degradation in activated T cells [26]. Recently, Lo et al. provided evidence that optimal recycling of CTLA-4 is critical for maintaining immune tolerance [27]. It is reported that patients with loss-of-function of the LRBA gene (encoding the lipopolysaccharide-responsive and beige-like anchor protein) develop early-onset autoimmunity and lymphoproliferative disease, a similar syndrome seen in patients with IPEX (immunodysregulation polyendocrinopathy enteropathy X-linked) syndrome caused by FOXP3 mutations [28]. Lo et al. showed that LRBA co-localizes with CTLA-4 in recycling endosomes and that LRBA deficiency accelerates CTLA-4 turnover leading to degradation in lysosomes [27]. The balance between CTLA-4 recycling and degradation provides an important implication for therapeutic strategies targeting CTLA-4. Indeed, immune-related adverse events (irAEs) remain as a major barrier in the therapeutic targeting of CTLA-4, occurring in 60–65% of patients treated with ipilimumab [29]. Zhang et al. showed that irAE-prone anti-CTLA-4 mAbs (including ipilimumab) rapidly direct surface CTLA-4 for lysosomal degradation by preventing binding of CTLA-4 to LRBA. In contrast, engineered anti-CTLA-4 mAbs that dissociate from CTLA-4 in response to low pH in endosomal vesicles allow CTLA-4 to be recycled in an LRBA-dependent manner. Strikingly, these novel pH-sensitive anti-CTLA-4 mAbs prevent irAEs with an enhanced preclinical anti-tumor efficacy [30]. Thus, CTLA-4 recycling should be an important consideration for CTLA-4 blockade.
PD-1
Like CTLA-4, PD-1 also plays a critical role for regulating T cell activation and maintenance of peripheral tolerance [31–33]. Upon engagement of its ligands PD-L1 or PD-L2 during antigen stimulation, PD-1 becomes clustered with the TCR and subsequently recruits the tyrosine phosphatase SHP2 to its cytoplasmic domain [34]. By analyzing the direct targets of PD-1-bound phosphatase(s), Hui et al. recently showed that CD28 signaling is the most sensitive target for PD-1-SHP2-mediated dephosphorylation, while only a part of the TCR signaling components undergo dephosphorylation [35]. Another independent group also demonstrated that CD28 co-simulation is indispensable for optimal CD8 T cell responses against tumors and viral infections by PD-1 blockade [36]. These findings highlight CD28 signaling as a key target of PD-1-mediated immune regulation. Of note, PD-1 also transcriptionally regulates T cell activation by suppressing genes induced by TCR activation [37]. Specifically, genes induced by a strong TCR signal (including genes encoding cytokines and effector molecules) are highly sensitive to PD-1-mediated repression whereas genes that are efficiently induced by TCR stimulation (e.g., genes related to cell survival and cell signaling) show resistance [37]. Thus, in addition to the PD-1/SHP2-mediated dephosphorylation of CD28, PD-1 is implicated in transcriptional regulation of TCR-induced effector molecules, highlighting a broad impact of PD-1 on T cell activation.
In addition to the interaction between PD-1 and PD-L1 on T cells and APCs (namely, the PD-1/PD-L1 trans-interaction), respectively, PD-L1 interactions in cis with PD-1 or CD80 have emerged as important factors for immune modulation. Zhao et al. initially showed that a subset of tumor-infiltrating APCs co-express PD-1 and PD-L1 and that PD-L1/PD-1 cis interaction can prevent PD-L1 binding to T cell intrinsic PD-1 in trans [38]. However, given that only a small subset of DCs co-express PD-L1 and PD-1, the significance of this interaction for ICB therapies remains unclear. More recently, several lines of evidence demonstrate that the cis interaction between PD-L1 and CD80 is predominantly implicated in immune modulation on APCs [39–41] (Fig. 2). Indeed, Sugiura et al. showed that the CD80/PD-L1 cis interaction on dendritic cells (DCs) can impede the PD-L1/PD-1 trans binding between DCs and T cells in a competitive manner [40]. Strikingly, gene-modified mice that cannot form the PD-L1/CD80 cis-heterodimer ameliorate anti-tumor T cell responses as well as autoimmunity, suggesting that the PD-1/PD-L1 inhibitory pathway is enhanced in the absence of the PD-L1/CD80 cis-heterodimer [40]. These findings highlight that CD80 on APCs augments T cell activity not only by CD28-mediated co-stimulatory signals but by also restricting PD-L1 (Fig. 2).
Fig. 2.
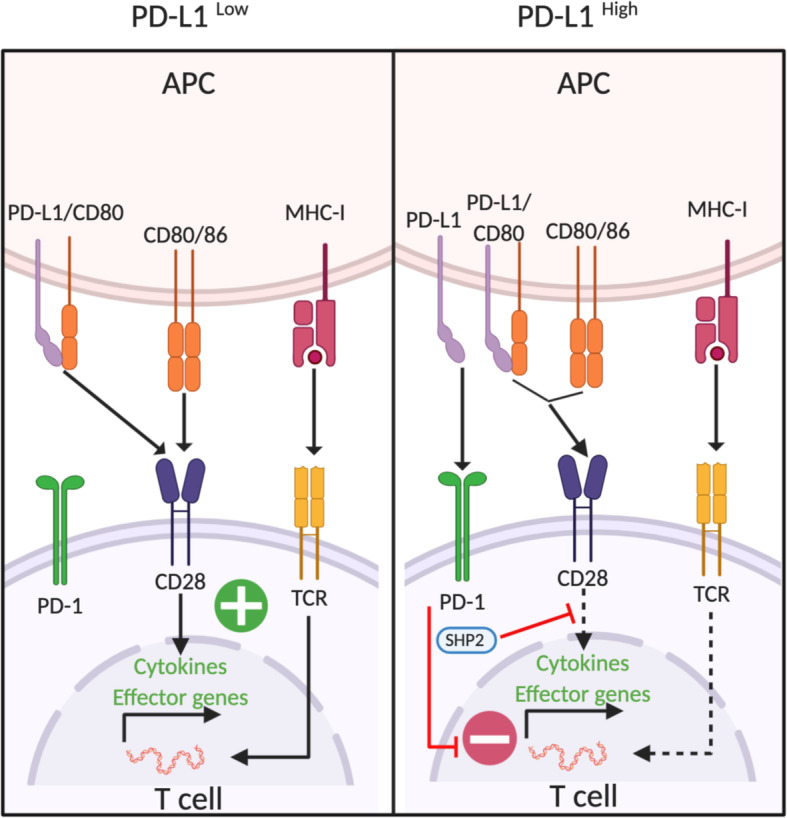
PD-1-mediated immune regulation. Under low expression levels of PD-L1, CD80 restricts PD-L1 function by forming the PD-L1/CD80 cis-heterodimer. The PD-L1/CD80 cis-heterodimer prevents the PD-1/PD-L1 trans-interaction, whereas the ability to bind to the CD28 co-stimulatory receptor is retained (left). Upregulation of PD-L1 on APCs allows the PDL-1/PD-1 trans-interaction, leading to SHP2-dependent negative regulation of the CD28 signaling pathway as well as transcriptional repression of TCR-induced effector genes (right)
Not surprisingly, the PD-L1/CD80 cis-heterodimer also affects CTLA-4-mediated immune regulation. Recently, Zhao et al. showed that the PD-L1/CD80 cis-heterodimer prevents the interaction between CTLA-4 and CD80 as well as the subsequent trans-endocytosis of CD80 while allowing the CD80 and CD28 interaction to remain intact [41]. Notably, inhibiting the formation of the PD-L1/CD80 cis-heterodimer by anti-PD-L1 mAb led to the loss of CD80 from APCs, whereas anti-PD-L1 mAb in combination with anti-CTLA-4 maintained CD80 expression on APCs [41]. These results suggest that selective blockade of the PD-1/PD-L1 trans-interaction, but not the PD-L1/CD80 cis-heterodimer formation, may be an important therapeutic approach. Moreover, soluble forms of PD-L1 and/or exosomal PD-L1 have emerged as immunosuppressive mediators [42, 43]. Yet, it remains to be elucidated how membrane-bound form of PD-L1 and soluble PD-L1 differentially regulate T cell responses.
The complex interplay between the B7 family of ligands (CD80, CD86, and PD-L1) and the CD28 receptor superfamily (CD28, CTLA-4, and PD-1) is implicated in fine-tuning immune responses at the T cell APC interface. Indeed, Lin et al. provided preclinical evidence that PD-L1 expression on APCs is indispensable for tumor control by PD-1/PD-L1 blockade, whereas neither knockout nor overexpression of PD-L1 in tumor cells affects efficacy [44]. Notably however, overexpression of tumor PD-L1 is associated with the clinical efficacy of PD-1/PD-L1 blockade in various hematological malignancies, as discussed in the next section. Moreover, the expression of CD80/CD86, in contrast to solid malignancies, is frequently observed in tumor cells from hematological malignancies (such as B cell lymphoma) [45] raising the possibility that the crosstalk between the B7 ligand family and the CD28 receptor superfamily may be further complicated in hematological malignancies. Altogether, the extent to which individual mechanisms prevail and effect clinical response to ICB may depend on the immune landscape that can be influenced by several factors in the various hematological malignancies.
Clinical response and resistance to immune checkpoint blockade in hematological malignancies
With a growing understanding of cancer biology, as well as the tumor microenvironment (TME), it is becoming increasingly clear that resistance as well as response to ICB can be strongly influenced by disease-specific factors including the immune landscape of the disease. A number of studies have reported encouraging results in various hematologic malignancies. Some of the basic and clinical aspects (Table 1) of those findings will be the focus of our discussion here.
Table 1.
Notable clinical trials targeting immune checkpoints in hematological malignancies
| Clinical trial | Phase | Patient characteristics | Intervention | Response | Reference |
|---|---|---|---|---|---|
| NCT01592370 | I | Relapsed or refractory HL | Nivolumab | ORR 87% | [46] |
| CheckMate 205 (NCT02181738) | II |
cHLCohort A: brentuximab vedotin naïve Cohort B: brentuximab vedotin after auto-HCT Cohort C: brentuximab vedotin before and/or after auto-HCT Cohort D: nivolumab monotherapy followed by nivolumab plus doxorubicin, vinblastine, and dacarbazine for newly diagnosed HL |
Nivolumab |
ORR: Cohort A 65% Cohort B 68% Cohort C 73% Cohort D 84% |
[47, 48] |
| KEYNOTE-013 (NCT01953692) | I | cHL after brentuximab vedotin failure | Pembrolizumab | ORR 65% | [49] |
| KEYNOTE-087 (NCT02453594) | II |
Relapsed or refractory cHL, Cohort 1: after ASCT/brentuximab vedotin Cohort 2: ineligible for ASCT and experienced treatment failure with brentuximab vedotin Cohort 3: No brentuximab vedotin after ASCT |
Pembrolizumab |
ORR: Cohort 1 73.9% Cohort 2 64.2% Cohort 3 70% |
[50] |
| NCT02038933 | II |
Relapsed or refractory DLBCL Cohort 1: auto-HCT-failed Cohort 2: auto-HCT-ineligible |
Nivolumab |
ORR: Cohort 1 10% Cohort 2 3% |
[51] |
| NCT02446457 | II | Relapsed FL |
Pembrolizumab Rituximab |
Pre-planned interim analysis: ORR 80% | [52] |
| NCT03245021 | II | Previously untreated FL | Single-agent nivolumab followed by combined nivolumab and rituximab | Pre-planned interim analysis: ORR 84% | [53] |
| NCT03278782 | I/II | Relapsed or refractory peripheral T cell lymphoma (PTCL) |
Pembrolizumab Romidepsin |
ORR 44% | [54] |
| NCT02243579 | II | Recurrent mycosis fungoides and Sezary syndrome | Pembrolizumab | ORR 38% | [55] |
| KEYNOTE-023 (NCT02036502) | I | Relapsed or refractory MM | Pembrolizumab combined with lenalidomide and low-dose dexamethasone | ORR 44% | [56] |
| KEYNOTE-183 (NCT02576977) | III | Relapsed or refractory MM | Pembrolizumab plus pomalidomide and dexamethasone |
Pembrolizumab plus pomalidomide and dexamethasone group: Median PFS: 5.6 months (95% CI 3.7–7.5); Pomalidomide and dexamethasone group: 8.4 months (5.9–not reached) |
[57] |
| KEYNOTE-185 (NCT02579863) | III | Treatment-naive MM | Pembrolizumab plus lenalidomide and dexamethasone | Progression-free survival estimates at 6-months were 82.0% (95% CI 73.2–88.1) versus 85.0% (76.8–90.5; hazard ratio [HR] 1.22; 95% CI 0.67–2.22; p = 0.75) | [58] |
| NCT01822509 | I |
Patients with relapse after allogeneic transplantation: AML (in 12 patients, including 3 with leukemia cutis and 1 with a myeloid sarcoma), HL (in 7), NHL (in 4), and myelodysplastic syndrome (in 2). One patient each had MM, myeloproliferative neoplasm, and acute lymphoblastic leukemia |
Ipilimumab | Patients that received a dose of 10 mg/kg: CR (23%) | [59] |
| NCT02397720 | II | Relapsed or refractory AML | Azacitidine and nivolumab | ORR 33% | [60] |
cHL classic Hodgkin lymphoma, NHL non-Hodgkin’s lymphoma, PTCL peripheral T cell lymphoma, MM multiple myeloma, AML acute myeloid leukemia, ASCT allogeneic stem cell transplantation, HCT hematopoietic cell transplantation, ORR objective response rate, CR complete response, HR hazard ratio, PFS progression-free survival, FL follicular lymphoma, DLBCL diffuse large B cell lymphoma
Hodgkin lymphoma
Among various hematological malignancies, therapeutic benefits of PD-1 blockade have been best demonstrated in patients with Hodgkin lymphoma (HL). In an early clinical trial of 23 relapsed or refractory HL patients, nivolumab showed an objective response rate (ORR) of 87%, with a complete response (CR) of 17% [46]. Clinical efficacy and safety profile of nivolumab monotherapy was further demonstrated in the CheckMate 205 trial of 80 HL patients who failed autologous stem-cell transplantation and brentuximab vedotin (an antibody-drug conjugate comprising anti-CD30 mAb conjugated to an anti-microtubule agent) [47, 48, 61]. Another PD-1 mAb, pembrolizumab, also showed similar efficacy against HL in clinical trials such as KEYNOTE-013 [49] and KEYNOTE-087 [50]. These results led to the FDA approval of nivolumab (in 2016) and pembrolizumab (in 2017) for relapsed or refractory HL patients who had failed multiple lines of therapy.
Clinical responsiveness to PD-1 blockade in HL has been explained by multiple unique tumor intrinsic and extrinsic factors. In solid malignancies, high TMB (high TMB; ≥ 20 coding mutations per megabase) has been recognized as an independent predictor for clinical responses to ICB therapies [62]. However, in HL, it is reported that TMB does not correlate with responsiveness [63]. Indeed, Liang et al. investigated TMB in 34 HL patients and found that only 15% of the patients had high TMB [64]. Despite this fact, amplification of 9p24.1 (locus-containing JAK2/PDL1/PDL2), a frequently observed cytogenetic abnormality in classical HL patients, induces aberrant overexpression of PD-L1 on tumor cells [65], suggesting that tumor PD-L1 might dampen anti-tumor immunity. Indeed, Epstein-Barr virus (EBV) infection can also contribute to PD-L1 upregulation [66]. While similar frequencies of 9p24.1 amplification in EBV-related or EBV-unrelated cases have been reported in cHL, EBV-positive cHL cases have been shown to be more likely to have higher PD-L1 expression levels [67]. Additionally, through viral oncoprotein latent membrane protein 1 (LMP1), EBV may also sustain an immune suppressive microenvironment [68]. Thus, it is possible that the presence of these immune suppressive features in EBV-related cHL may allow patients with this particular sub-type to be more susceptible to ICB.
In addition to the tumor-intrinsic overexpression of PD-L1, the immune microenvironment of HL is critically responsible for responsiveness to PD-1 blockade. The TME of classical HL consists of rare (0.1–1%) malignant cells called Hodgkin Reed-Sternberg (HRS) cells and an abundant immune cell infiltrate which is markedly distinct from the TME observed in non-Hodgkin’s lymphoma (NHL) [69]. Thus, the unique immunologically “hot” (or inflamed) TME critically contributes to responsiveness to PD-1 blockade [70]. To understand the immune landscape, Cader et al. recently performed mass cytometry of 7 newly diagnosed classical HL patients [71]. Notably, they found that CD4+ T cells especially Th1-polaralized effector cells and Tregs were major T cell subsets in the TME and that MHC-I expression was frequently lost in tumor cells [71]. This result raises the possibility that CD4+ T cells, rather than CD8+ T cells, may be key players in anti-tumor immunity against HL. Indeed, Roemer et al. also reported that β2-microglobulin (β2M) and MHC-I were not expressed on tumor cells in more than 60% of HL patients and that the expression level of MHC-II and PD-L1 predicts therapeutic response to nivolumab in HL patients [72]. More recently, Patel et al. investigated checkpoint molecules by multiplexed immunofluorescence imaging and observed the expansion of CTLA-4+ PD-1− CD4 T cells in close proximity to CD86+ tumor cells or tumor-associated macrophages (TAMs) [73]. This suggests that the interaction between CTLA-4 and CD86 might also act as a key negative regulator in HL.
Overall, these results highlight the importance of characterizing the disease-specific TME and T cell phenotypes in order to determine optimal therapeutic targets. Despite the clinical benefits of PD-1 blockade, some HL patients experience recurrence after PD-1 blockade therapy. Currently, the randomized phase 2 study of brentuximab vedotin and nivolumab with or without ipilimumab is ongoing (NCT01896999) to assess the efficacy of dual CTLA-4 and PD-1 blockade. LAG-3 might be a potential target considering the recent single-cell RNA sequence (scRNA-seq) analysis which showed that a subset of HL-associated T cells expressed high levels of this checkpoint molecule [74]. Alternatively, given that loss of MHC-II confers therapeutic resistance to HL, harnessing innate immunity might be a key approach. The PD-1 and PD-L1 interaction is implicated in negative regulation of NK cells and monocytes/macrophages [75]. As discussed later, several innate immune checkpoint inhibitors are being developed. The combination of innate checkpoint inhibitors may improve clinical responses against HL with acquired resistance to T cell-mediated anti-tumor immunity.
Non-Hodgkin lymphoma
In contrast to HL patients, PD-1 blockade has not shown remarkable clinical responses in patients with NHL such as diffuse large B cell lymphoma (DLBCL) and follicular lymphoma (FL). In a phase 2 clinical trial of nivolumab in relapsed or refractory DLBCL, ORR of monotherapy was 3% and 10% in transplant-ineligible patients and relapsed patients after autologous SCT, respectively [51]. The efficacy of nivolumab and ibrutinib (a Bruton’s tyrosine kinase inhibitor) combination has been evaluated in relapsed or refractory NHL (DLBCL and FL) and chronic lymphocytic leukemia patients. However, overall response of the combination was comparable to that of ibrutinib monotherapy [76], suggesting that PD-1 blockade had limited contribution to disease control. Indeed, PD-1 blockade in combination with rituximab has been shown to be effective in rituximab refractory FL [52]. However, ICB can also be utilized to prime the immune system prior to such tumor-targeted therapies. In fact, this concept was trialed in a phase 2 study in treatment of naïve FL patients using a combination of nivolumab and rituximab [53]. Interim analyses indicate an ORR of 84% with 47% achieving CR, suggesting a favorable toxicity profile along with high overall and complete response rates [53].
Differential responsiveness to PD-1 blockade between DLBCL patients and HL patients can be primarily explained by their different levels of immune infiltration. Indeed, the transcriptional and histological comparison of the immune microenvironment between HL and DLBCL showed an immunologically “cold” (or “non-inflamed”) TME in DLBCL in contrast to the “hot” (or “inflamed”) TME in HL [77]. Of note, in DLBCL patients treated with rituximab-based standard chemo-immunotherapy (R-CHOP), high infiltration of T cells predicts better prognosis, whereas the presence of PD-1high T cells predicts poor prognosis [78, 79] indicating that anti-lymphoma immunity still plays an indispensable role for disease control against immunologically cold DLBCL.
The immunologically “cold” TME is created by tumor-intrinsic factors such as high proliferation rate of lymphoma cells and oncogene-driven immune exclusion [70]. Various factors are reported to be associated with immunologically “cold” TME such as double rearrangements of MYC and BCL2 and/or BCL6 [80], deletion or mutation of PTEN [81], and Epstein-Barr virus-related subtypes [82]. Above all, several lines of evidence suggest that EZH2 mutations critically contribute to immune exclusion phenotypes. It is reported that MHC-I and MHC-II are lost in 40–60% and 20–40% of DLBCL patients, respectively, and EZH2 mutations are highly enriched in MHC-deficient subsets of patients [83]. The EZH2-mediated silencing of genes related to MHC-I expression is implicated in immune evasion in a wide range of other malignancies, as Burr et al. also demonstrated this immune evasion mechanism by a whole genome CRISPR/Cas9 screen [84]. Thus, inhibition of EZH2 activity by a small molecule inhibitor might be a potential approach to sensitize tumor cells to T cell-mediated anti-tumor immunity.
As seen in HL, EBV has also been linked to a number of malignant NHLs [85]. In a recent study, Kim et al. reported that more patients with EBV-positive NHL responded to pembrolizumab than EBV-negative subtypes [86]. Moreover, high PD-L1 expression was reported in EBV-positive NHL as compared to EBV-negative NHL [86]. In agreement with this, Kataoka et al. recently reported a high frequency of PD-L1/PD-L2 containing somatic aberrations in various EBV-positive lymphoma subtypes [87]. In addition, a distinct pattern of somatic alterations in EBV-positive DLBCL was reported where the genetic profile was found to be distinct from EBV-negative DLBCL [87]. While ICB in treating virus-associated cancers appears promising, more clinical trials are needed to verify if viral infections such as EBV can effectively predict ICB efficacy.
Another important tumor-intrinsic factor is gene alterations (amplifications or translocations) of PD-L1 that are observed in ~ 25% of DLBCL patients (especially the non-germinal center type) [88]. This DLBCL subset with aberrantly overexpressed PD-L1 is characterized by high infiltration of clonal T cells and low expression of tumor MHC-I. While patients with this type of DLBCL show inferior progression-free survival following front-line chemo-immunotherapy, they show, strikingly, good responsiveness to PD-1 blockade [88]. Thus, PD-L1 alterations may be a useful biomarker in predicting responsiveness to PD-1 blockade in DLBCL patients. Still, it remains unknown how we can overcome therapeutic resistance in patients with the immunologically “cold” DLBCL (low T cell infiltration and low MHC expression on tumor cells). Blockade of innate checkpoint molecules in combination with rituximab might be a possible approach to augment NK cell-mediated antibody-dependent cellular cytotoxicity (ADCC) and macrophage-mediated antibody-dependent cellular phagocytosis (ADCP).
NK/T cell lymphomas have a distinct immunophenotype, and PD-1 blockade has shown some efficacy in relapsed or refractory NK/T cell lymphomas [89]. In a recent retrospective study of seven patients with relapsed or refractory NK/T cell lymphomas treated with pembrolizumab at diagnosis, the ORR was reported to be 57.1% with a complete response occurring in 2 patients [90]. Large scale trials are warranted to further assess long-term clinical responses. Notably, modest responses to single agent PD-1 blockade have been observed in peripheral T cell lymphomas (PTCL) [91]. Indeed, mutations in epigenetic modifier genes are often observed in PTCL, and such mutations may promote immune escape. To this end, a recent phase I/II trial combined pembrolizumab and a histone deacetylase inhibitor in relapsed or refractory PTCL patients [54]. From the 15 evaluable patients, 3 were complete responders that remained in remission for at least 10 months [54]. These early findings are encouraging, and therefore, further effort in this direction should be pursued. Furthermore, some responses to ICB have also been reported in patients with common subtypes of cutaneous T cell lymphomas. PD-1 blockade led to an ORR of 38% in patients with mycosis fungoides or Sézary syndrome in a phase 2 trial demonstrating a favorable safety profile and modest anti-tumor activity [55]. Notably, some flare reactions such as worsening of erythema were reported in patients with Sézary syndrome, and such skin flare reactions were found to be associated with high PD-1 expression on circulating Sezary cells before therapy [55]. Although high PD-1 expression may be an effective predictor of this reaction, further validation is warranted. On the contrary, PD-1 blockade led to rapid progression in patients with adult T cell leukemia/lymphoma (ATLL) in a recent study [92]. Rapid clonal expansion of malignant T cells was observed in patients treated with PD-1 blockade, suggesting a tumor-intrinsic regulatory role of PD-1 in ATLL [93]. This is in line with a previous report from a T cell lymphoma mouse model where PD-1 activity enhanced PTEN levels, and PD-1 deletion after an oncogenic insult resulted in aggressive lymphomas in vivo [94]. These data highlight the growing need to mechanistically understand the underlying mechanisms of ICB as we attempt to extend their promise to an ever-increasing list of malignancies.
Multiple myeloma
Multiple myeloma (MM) remains an incurable malignancy, and new immunotherapeutic approaches are actively being tested. In relapsed and refractory MM patients, an early clinical trial supported good efficacy (ORR 44%) with an acceptable safety profile of pembrolizumab, lenalidomide (an immunomodulatory imide drug: IMiD), and low dose dexamethasone [56]. However, the combination of pembrolizumab and IMiD showed unfavorable benefit-risk profile in following phase III trials in relapsed and refractory MM (KEYNOTE-183) and newly diagnosed MM (KEYNOTE-185) [57, 58].
It remains poorly understood why PD-1 blockade failed to show clinical benefits in MM patients. As MM predominantly grows in the bone marrow (BM), the unique TME in the MM BM might be implicated in therapeutic resistance [95]. One of the key factors is an altered T cell phenotype in the MM BM. In general, T cell subsets with a senescent phenotype represent dysfunctional T cells in the TME and often result in hypo-responsiveness to ICB therapy [96]. A recent scRNA-seq analysis of the MM immune microenvironment showed that a senescent T cell subset emerges in a premalignant state (i.e., smoldering MM) [97], indicating that symptomatic MM patients already have dysfunctional T cells at diagnosis. Moreover, dysfunctional T cells are increased in patients who experience relapse after autologous SCT [98] indicating that there is difficulty in reinvigorating T cells in relapsed and refractory MM patients. Another key barrier for anti-tumor immunity is immunosuppressive subsets in the TME. As myeloid cells and their progenitors abundantly exist in the BM, MM progression triggers conversion of these cells into myeloid-derived suppressor cells (MDSCs). Indeed, the transcriptional landscape in MM patients revealed an inverse correlation between MDSC-related genes and cytotoxic lymphocyte-related genes suggesting that MDSCs might contribute to T cell exclusion in the MM BM [99]. MM-associated Tregs are important targetable immunosuppressive cells since CD38+ Tregs can be depleted by daratumumab (anti-CD38 mAb) [100]. However, a phase 1 clinical trial of daratumumab in combination with anti-PD-1 mAb (JNJ-63723283) in relapsed and refractory MM (MMY2036, NCT03357952) was terminated due to limited clinical responses with increased adverse events in the combination group compared to daratumumab monotherapy.
While PD-1 blockade has not demonstrated clinical benefits in MM patients, it is noteworthy that some patients achieved long-term remissions after stopping pembrolizumab in clinical trials [101]. Thus, further investigations are necessary to predict responder patients. Alternatively, T cell immunoreceptor with Ig and ITIM domains (TIGIT) has emerged as an important immune checkpoint on MM T cells [102]. The inhibitory mechanisms of this new immune checkpoint will be discussed later in this review.
Myeloid malignancies
Early phase 1 trials showed lack of efficacy of anti-PD-1 mAb as monotherapy in patients with acute myeloid leukemia (AML) [103] or high-risk myelodysplastic syndrome (MDS) [104]. Similarly, CTLA-4 blockade using ipilimumab failed to show clinical benefits in high-risk MDS patients [105].
Although these early trial results are disappointing, ipilimumab treatment after allogeneic-hematopoietic stem cell transplantation (HSCT) showed good responses in 22 patients with various hematological malignancies including 12 AML patients (CR 23% in 4 patients with extramedullary AML and 1 with MDS developing into AML) [59], suggesting that ipilimumab can augment graft-versus-leukemia (GvL) effects. Of course, the key concern remains to be immune-related adverse events (irAEs), especially graft-versus-host disease (GVHD). However, among 22 patients, 3 patients in total developed GVHD (1 patient with grade II acute GVHD of the gut and 2 patients with chronic GVHD of the liver) which was able to be controlled by glucocorticoids [59]. PD-1 blockade after allogeneic HSCT is also being tested, but so far, it has shown modest clinical benefits [106].
Another potential approach to improve ICB efficacy is using a hypomethylating agent (HMA) such as azacytidine. Azacytidine is clinically approved for MDS and AML and has shown immunomodulatory effects including upregulation of MHC-I. In a recent trial, the combination of nivolumab and azacytidine showed an ORR of 33% and CR rate of 22% in 70 patients with relapse/refractory AML [60]. Intriguingly, while high infiltration of effector T cells before therapy predicted good responsiveness to the combination therapy, an increase in CTLA-4+ effector lymphocytes after treatment predicted non-responder patients [60]. The combination of HMAs and PD-1 blockade are currently being tested in several trials [106], but co-blockade of PD-1 and CTLA-4 may potentially overcome therapeutic resistance.
Immune dysregulation in AML remains incompletely understood as it might be differentially organized and depends on multiple factors such as tumor subtypes, presence or absence of the MDS state, patients’ age, and treatment history. Kong et al. originally showed high TIGIT expression on CD8+ T cells in AML patients, and that siRNA mediated TIGIT knockdown can reinvigorate cytokine production suggesting that TIGIT is expressed on dysfunctional T cells [107]. Another independent group also showed that PD-1+ TIGIT+ CD8+ T cells with low expression levels of DNAM-1 (DNAX accessory molecule 1 or CD226) represent dysfunctional T cells [108], further providing evidence that TIGIT represents a key checkpoint molecule in AML. In terms of mechanisms of immune escape after HSCT, Christopher et al. recently performed exome sequencing on paired samples obtained at diagnosis and at post-HSCT relapse demonstrating that downregulation of MHC II-related genes is a key feature of relapsed AML [109]. This result suggests that CD4+ T cells might play a critical role for controlling relapse. Thus, it might be possible to augment CD4-mediated GvL effects by blockade of LAG-3-MHC-II interaction. Another immune checkpoint TIM-3 is also expressed on AML T cells [110], but tumor TIM-3 has a unique tumor-intrinsic role, as discussed later. Thus, TIGIT, LAG-3, and TIM-3 are differentially implicated in AML immune-regulation and are rational therapeutic targets in combination with PD-1 blockade and/or CTLA-4 blockade.
Compared to MDS and AML, therapeutic benefits of ICB may be better achieved in myeloproliferative neoplasms (MPNs), a heterogeneous group of diseases characterized by clonal expansion of myeloid cells. Significant advances have been made to control disease progression by targeting JAK2, one of the key driver mutations in MPNs. However, it is still challenging to treat high-risk patients who are refractory to JAK1/JAK2 inhibitors [111]. Prestipino et al. showed that JAK2 mutations can trigger the overexpression of PD-L1 on myeloid cells, leading to metabolic and functional impairment of T cells [112]. Importantly, PD-1 blockade improved survival in human MPN xenograft and primary murine MPN models [112] suggesting potential roles for immunotherapy in MPNs. Another notable aspect is immunogenicity of MPNs. The JAK2V617F mutation is seen in > 50% of patients with MPNs, and this mutation-associated neoantigen can elicit tumor-specific CD8+ T cell responses [113]. Somatic frameshift mutation of the calreticulin gene (CALR) is another MPN-restricted key driver mutation found in 67% and 88% of patients with essential thrombocythemia and primary myelofibrosis respectively [114]. These CALR mutations induce a shared MPN-specific neoantigen leading to the generation of mutant calreticulin–specific T cell responses [115, 116]. Thus, due to the unique immunogenicity and induction of neoantigen-specific T cell responses, ICB might play an important role for disease control in MPNs. However, further clinical investigations are warranted.
Beyond PD-1 and CTLA-4 blockade
Therapeutic blockade of PD-1/PD-L1 or CTLA-4 has shown clinical benefits in only certain types of hematological malignancies such as HL. Obviously, inhibiting different immune checkpoint molecules on T cells (such as LAG-3, TIM-3, and TIGIT) can be a potential approach since these molecules inhibit T cell responses in a non-redundant manner (Fig. 3).
Fig. 3.

Negative regulators of T cell immunity other than PD-1 and CTLA-4. Schematic illustrating receptors and their ligands regulating T cell immunity. Multiple immune checkpoint molecules are differentially implicated in the regulation of activated T cells including LAG-3, TIM-3, and TIGIT. Plus and minus signs denote stimulatory and inhibitory signaling respectively. Single-headed and double-headed arrows denote uni-directional and bi-directional signaling respectively. APC, antigen-presenting cell; TCR, T cell receptor; LAG-3, lymphocyte-activation gene 3; CD112R, CD112 receptor; MHC, major histocompatibility complex; FGL1, fibrinogen-like protein 1; DNAM-1, DNAX accessory molecule 1; TIGIT, T cell immunoreceptor with Ig and ITIM domains; TIM-3, T cell immunoglobulin mucin-3
LAG-3
Lymphocyte-activation gene 3 (LAG-3, CD223) is a transmembrane protein reported to be primarily expressed on tumor-infiltrating T cells. It consists of four extracellular immunoglobulin (Ig)-like domains (D1–D4) with high homology to CD4 [117], and it binds to complexes of peptides and MHC-II [118].
Although the impacts of LAG-3-MHC-II interaction on CD4+ T cell immunity have been well studied, it was poorly understood as to how LAG-3 negatively regulates CD8+ T cell-mediated anti-tumor immunity [119, 120]. Recently, Wang et al. identified fibrinogen-like protein 1 (FGL1) as a high affinity soluble ligand for LAG-3 and reported that FGL1-LAG3 interaction critically impedes CD8+ T cell-mediated anti-tumor immunity [121]. While FGL-1 is upregulated in solid tumor tissues such as lung, prostate, and breast cancer [121], it remains unknown whether hematological malignancies also produce abundant FGL-1. It should be noted that unlike solid tumor cells, hematological tumor cells frequently express MHC-II, and thus, the LAG-3-MHC-II interaction still plays a key inhibitory role in CD4+ T cell-mediated control. As LAG-3 is frequently co-expressed with PD-1 in tumor infiltrating lymphocytes, combined efficacy of PD-1 and LAG-3 blockade (NCT03005782 and NCT02061761) or a bispecific antibody against PD-1 and LAG-3 (NCT03219268) are actively being investigated in various types of malignancies including blood cancers. More recently, Keane et al. investigated LAG-3 expression in DLBCL patients. Indeed, LAG-3 was co-expressed with PD-1 on Tregs and CD8+ T cells; however, strikingly, LAG-3 expression was also observed on tumor-associated macrophages and a proportion of malignant B cells [122]. In addition to the clinical efficacy of dual PD-1 and LAG-3 blockade, functional impacts of myeloid LAG-3 and tumor-intrinsic LAG-3 will require further investigation.
Tim-3
TIM-3 (T cell immunoglobulin and mucin domain 3) is often co-expressed with PD-1 on tumor infiltrating T cells and has been recognized as a potential target for combination blockade with PD-1 [123–125]. TIM-3 signaling can induce tolerance in T cells upon recognition of its major ligand (galectin-9) [126] that is widely expressed in various types of malignancies including blood cancers. While TIM-3 acts as one of the T cell immune checkpoint molecules, TIM-3 on non-lymphoid cells is also implicated in immune-regulation. In preclinical breast cancer models treated with paclitaxel and anti-TIM-3 mAb, TIM-3+ intra-tumor CD103+ dendritic cells (DCs) are a key target subset that can mobilize CD8+ T cells via CXCL9 production in response to the combination therapy [127]. Additionally, by analyzing tumor tissues from NHL patients, Huang et al. showed that TIM-3 is highly expressed on endothelial cells (ECs) in the lymphoma microenvironment. Importantly, TIM-3 on ECs inhibits CD4+ T cell-mediated immunity, and thus, high expression levels of TIM-3 on the endothelium are associated with advanced stage and higher international prognosis index scores [128]. Another notable role of TIM-3 is its tumor-intrinsic function in AML. TIM-3 is one of the markers highly expressed on leukemia stem cells [129], and tumor-derived galectin-9 promotes self-renewal in an autocrine manner [130]. Since TIM-3 is highly expressed on T cells in AML patients [110, 131], TIM-3 blockade might have multiple therapeutic benefits in AML. In a phase 1 clinical trial of anti-TIM-3 mAb with or without anti-PD-L1 mAb in patients with advanced cancers, both monotherapy and combination therapy showed a good safety profile [132]. Given the broad expression of TIM-3 on innate and adaptive immune cells, endothelial cells, and certain types of tumor cells, it is possible that TIM-3 blockade might have pleiotropic effects. Further studies are warranted to understand the expression and function of TIM-3 in disease-specific tumor microenvironments.
TIGIT
An activating receptor DNAM-1 (CD226) on cytotoxic lymphocytes plays a critical role for recognition and elimination of tumor cells by recognition of its ligand CD155 and CD112. Its inhibitory counterparts, TIGIT and CD96, also share CD155 as a ligand, and thus, these inhibitory receptors negatively regulate DNAM-1-dependent functions [133]. CD112, on the other hand, can also bind to the co-inhibitory CD112 receptor expressed on T cells where it can compete with CD226 binding to CD112 [134]. Among these receptors, TIGIT has the highest binding affinity to CD155. Of note, TIGIT-mediated inhibitory functions are explained by multiple mechanisms beyond competition with DNAM-1 for CD155 binding. At the interface between T cells and APCs, the TIGIT-CD155 interaction can bi-directionally inhibit T cells and APCs [135]. Moreover, TIGIT+ Tregs potently suppress anti-tumor immunity [136]. Although crucial inhibitory mechanisms remain unknown, growing evidence suggests that TIGIT is a key T cell immune checkpoint in hematological malignancies. As described earlier, DNAM-1lowPD-1+TIGIT+ subset represents dysfunctional T cells in AML patients, and an increased frequency of this subset predicts poor prognosis in AML patients [108]. In MM, TIGIT is the most frequently upregulated checkpoint molecule among PD-1, CTLA-4, LAG-3, and TIM-3, and TIGIT+ T cells represent a dysfunctional T cell subset [102]. In a mouse Vk*MYC MM model, DNAM-1lowPD-1+TIGIT+ dysfunctional T cells are increased at post-transplant relapse [137] suggesting that the emergence of dysfunctional T cells might be tightly associated with immune escape. Additionally, TIGIT also negatively regulates NK cell-dependent control of tumors [138]. Since CD155 is expressed in a broad range of malignancies including blood cancers, therapeutic blockade of TIGIT might have broad implications for immunotherapy against hematological malignancies.
Innate checkpoints
ICB therapies such as anti-PD-1 and anti-CTLA-4 predominantly depend on T cells for their therapeutic efficacy. However, multiple factors are implicated in primary and acquired resistance including (1) low TMB and neoantigen load, (2) low infiltration of tumor-specific T cells, and (3) loss of β2M/MHC-I. In this light, harnessing innate anti-tumor immunity by NK cells [139] or macrophages [140] may be a potential approach (Fig. 4).
Fig. 4.
Negative regulators of innate anti-tumor immunity. Schematic illustrating receptors and their ligands regulating anti-tumor immunity by NK cells (top) and macrophages (bottom). In NK cells, inhibitory receptors that recognize MHC class 1 molecules are recognized as a potential target to enhance NK cell-mediated cytotoxicity against tumors. Targeting macrophage phagocytosis checkpoints has also emerged as a potential approach in combination with various cancer mAb therapies due to its potential in enhancing the elimination of antibody-coated tumor cells. An immunosuppressive metabolite, adenosine, also potently inhibits innate and adaptive anti-tumor immunity. ADCP, antibody-dependent cellular phagocytosis; ADCC, antibody-dependent cellular cytotoxicity; DNAM-1, DNAX accessory molecule 1; TIGIT, T cell immunoreceptor with Ig and ITIM domains; NKG2A, NK group 2 member A; KIRs, killer-cell immunoglobulin-like receptors; HLA, human leukocyte antigen; MHC, major histocompatibility complex; LILRB1, leukocyte immunoglobulin-like receptor B1; SIRPα, signal regulatory protein α, Siglec-10, Sialic acid-binding Ig-like lectin 10
NK cell inhibitory checkpoints
The activation of NK cells is regulated by a balance between activation receptor signaling and inhibitory receptor signaling. While activation receptors such as NKG2D (natural-killer group 2, member D) and DNAM-1 recognize ligands upregulated on malignantly transformed cells, inhibitory receptors such as NKG2A (NK group 2 member A) and KIRs (killer cell immunoglobulin-like receptors) recognize non-classical MHC-I (HLA-E) and classical MHC-I, respectively. Thus, NK cells can eliminate transformed cells that express self-induced danger ligands “induced-self recognition” or abnormal cells that lose MHC-I expression “missing-self recognition” [141].
NKG2A is expressed on both NK cells and T cells, and its ligand HLA-E is frequently overexpressed in various malignancies including DLBCL, MM, and AML [142, 143] which allows tumor cells to evade from cytotoxicity. Indeed, an early clinical study demonstrated that anti-NKG2A mAb (monalizumab) in combination with cetuximab (anti-EGFR mAb) augments therapeutic efficacy by enhancing ADCC in head and neck cancer patients [144]. The therapeutic potential of NKG2A blockade in combination with various mAbs with ADCC activity requires further investigation in hematological malignancies.
IPH2101 (1-7F9) is an anti-KIR mAb that inhibits the interaction between KIRs (KIR2DL-1, KIR2DL-2, and KIR2DL-3) and their HLA-C ligands. It showed a good safety profile in phase I clinical trials [145, 146]; however, a subsequent phase II trial in smoldering MM patients showed limited clinical benefits as monotherapy [147]. The combination of IPH2101 and lenalidomide showed some responses in relapsed and refractory MM [148]. Currently, the recombinant version with a stabilized hinge, lirilumab (IPH2102/BMS-986015), is being tested in various malignancies. Recently, a combination of lirilimumab and nivolumab was trialed in a small number of patients with relapsed or refractory lymphoid malignancies. The combination was unable to improve on the already strong therapeutic efficacy of nivolumab in cHL, and no therapeutic benefits of the combination were recorded in an unselected cohort of NHL or MM patients [149].
Macrophage phagocytosis checkpoints
Tumor-associated macrophages (TAMs) are educated to promote tumor growth and immunosuppression, and their abundance is often correlated with poor prognosis in various types of malignancies including blood cancers [140]. However, TAMs critically contribute to the therapeutic efficacy of cancer mAb-based therapies by their Fc receptor-dependent ADCP activity. In this context, several negative regulators of ADCP have been identified, and blockade of “don’t eat me signals” has emerged as a new approach to augment engulfment and clearance of tumor cells by monocytes/macrophages [150].
The interaction between signal regulatory protein α (SIRPα) and its ligand CD47 is one of the best characterized “don’t eat me” signals. The SIRPα receptor contains an immunoreceptor tyrosine-based inhibitory motif (ITIM), and upon CD47 recognition, this receptor transmits negative signals that attenuate phagocytic activity [151]. While its ligand, CD47, is expressed on various normal cell types, it is often found to be overexpressed in malignant tumor cells. Indeed, growing preclinical evidence supports that CD47 blockade augments lymphoma cell clearance either as monotherapy [152] or in combination with rituximab [153]. Of note, CD47 blockade can also induce adaptive immunity by enhancing DC-mediated cross-priming [152] suggesting that the combination of CD47 blockade with ICB might also be a rational approach. In a recent clinical trial, anti-CD47 mAb (Hu5F9-G4) in combination with rituximab has shown good clinical responses in relapsed and refractory NHL with a CR of 43% (in FL patients) and 33% (in DLBCL patients) [154]. Given that these patients were heavily pretreated, the efficacy of the combination is promising. Importantly, on-target adverse events such as anemia (due to phagocytosis of erythrocytes) were manageable and transient which support its safety profile [154]. Currently, several CD47 blocking agents are actively being tested in clinical trials in various types of hematological malignancies. More recently, other mediators for “don’t eat me signals” have been identified such as the interaction of LILRB1-MHC-I [155], Siglec-10-CD24 [156], and immunosuppressive adenosine signaling [157]. While their redundant and non-redundant roles require further investigation, these phagocytosis regulators are promising targets for enhancing ADCP against hematological malignancies.
ICB and CAR T cell therapy
Chimeric antigen receptor (CAR) T cells are synthetically engineered T cells expressing a CAR that has the target specificity to bind an antigen in an MHC-independent manner [158]. Encouraging results from recent trials with anti-CD19 CAR T cell therapies lead to their FDA approval for treatment of relapsed or refractory B cell acute lymphoblastic leukemia (ALL) and adult large B cell lymphoma [159–165].
Despite encouraging outcomes of anti-CD19 CAR T cell therapies, poor T cell persistence remains to be a major reason for relapse or a lack of response after CAR T cell therapy. Indeed, only 29% of the CLL patients had a CR to anti-CD19 CAR T cell therapy [166] in contrast to the 90% CR rate reported in ALL patients [167]. Notably, non-responder CLL patients showed transcriptional upregulation of genes related to apoptosis and exhaustion while responder patients had lower proportions of PD-1-expressing CAR T cells [168]. Moreover, co-expression of PD-1 with LAG-3 or TIM-3 on CAR T cells were associated with poor responses [168], highlighting the critical role of T cell immune checkpoint molecules for limiting CAR T cell activity. Still, clinical benefits of combining PD-1/PD-L1 inhibitors with CD19 CAR T cell therapy are yet to be determined though this combination is thus far reported to have an acceptable safety profile [169, 170]. Another recent trial of CD19 CAR T cell therapy in combination with PD-1 blockade in 14 children with heavily pre-treated B-ALL provided further evidence of the safety profile of this combination therapy. In fact, 3 of 6 patients that received CAR T cell therapy with a PD-1 inhibitor re-established B cell aplasia, suggesting that PD-1 blockade may prolong CAR T cell activity [171].
Alternatively, genetic modification of CAR T cells is another potential approach to augment the efficacy of CAR T cell therapy. Various “Armoured” CAR T cells have been generated to express immuno-stimulatory ligands and cytokines such as CD40 ligand [172], Fms-like tyrosine kinase 3 ligand (Flt3L) [173], IL-12 [174, 175], and IL-18 [176]. To inhibit CAR T cell-intrinsic PD-1, shRNA or engineering PD-1 dominant negative receptors have been developed [177]. Additionally, genome editing techniques such as CRISPR/Cas9 [178] as well as TALEN [179] have also been used to delete PD-1, and PD-1-deficient CAR T cells have shown improved cytotoxicity in vivo [178]. However, off-target cleavage and guide-RNA associated genotoxicity should be thoroughly interrogated prior to clinical applications. More recently, Rafiq et al. developed modified CAR T cells that secrete PD-1-blocking single-chain variable fragments (scFv). Notably, this approach has demonstrated improved anti-tumor responses in addition to mobilizing the bystander tumor-specific T cells in solid and hematological malignancies [180]. It is possible that the smaller size of scFvs locally released in the TME may help reduce the risk of irAEs compared to systemic ICB therapies.
Possibly, combination with inhibitory molecules such as TIM-3 and LAG-3, in addition to PD-1 blockade, may further improve CAR T cell function though much remains to be studied to support the proof-of-concept. Given the high incidence of cytokine release syndrome associated with CAR T cell therapies [181], safety concerns remain a major barrier to simultaneously target multiple immune checkpoint molecules in combination. Nonetheless, safety strategies that can limit exacerbation of toxicities should be considered such as the suicide gene “safety switch” systems, including iCaspase-9, already employed in clinical trials [182]. Efficient manufacturing of CAR T cell products remains another major issue in patients with highly proliferative circulating leukemic blasts with relatively fewer T cells available [183]. To this end, off-the-shelf, allogeneic CAR T cells or induced pluripotent stem cell (iPSC)–derived CAR T products hold great potential to overcome problems associated with CAR T cell production. Overall, advances in genome editing as well as manufacturing processes may lead to potentially curative therapies for patients with hematological malignancies.
Concluding remarks
Although ICB therapies, particularly PD-1/PD-L1 blockade, are being actively tested in a number of hematological malignancies, it remains to be fully understood why blockade of PD-1/PD-L1 shows efficacy in only limited tumor types. The immunologically “cold” TME might act as a major barrier for therapeutic blockade of T cell checkpoints, and combining ICB with chimeric antigen receptor (CAR) T cell therapy or bispecific T cell engagers is an active area of investigation [184, 185]. Indeed, irAEs are a major concern since cytokine-release syndrome is frequently observed in patients treated with T cell-based approaches. In addition to primary resistance, acquired resistance mechanisms of ICB remain to be elucidated. Even in patients with HL, most eventually experience disease progression during anti-PD1 therapy [186]. Targeting other T cell checkpoint molecules may be a potential approach to overcome acquired resistance. However, an in-depth characterization of T cell function and checkpoint molecules will be highly warranted to determine the optimal therapeutic approach. Harnessing innate anti-tumor immunity by NK cells and macrophages could be another rational approach against tumors with downregulated MHC-I expression. Again, a comprehensive understanding of the immune microenvironment will provide a clue for identifying biomarkers that can predict responsiveness to ICB. Alternatively, a personalized approach may be necessary given that the disease-specific immune microenvironment can be sculpted by multiple factors including tumor genotypes, treatment history, and comorbidities in patients. Therefore, a mechanistic understanding of the role of tumor intrinsic and extrinsic modulators of therapeutic response will hopefully inform avenues for durable disease control from ICB with minimal immune-related toxicities.
Acknowledgements
Figures were created with BioRender.com.
Ethical approval and consent to participate
Not applicable
Abbreviations
- ADCC
Antibody-dependent cellular cytotoxicity
- ADCP
Antibody-dependent cellular phagocytosis
- AML
Acute myeloid leukemia
- APC
Antigen presenting cells
- BM
Bone marrow
- CALR
Calreticulin
- CAR
Chimeric antigen receptor
- CR
Complete response
- CTLA-4
Cytotoxic T lymphocyte-associated protein 4
- DCs
Dendritic cells
- DLBCL
Diffuse large B cell lymphoma
- DNAM-1
DNAX accessory molecule 1
- FGL-1
Fibrinogen-like protein 1
- FL
Follicular lymphoma
- GVHD
Graft-versus-host disease
- GvL
Graft-versus-leukemia
- HL
Hodgkin lymphoma
- HLA
Human leukocyte antigen
- HMA
Hypomethylating agent
- HRS
Hodgkin Reed-Sternberg
- HSCT
Hematopoietic stem cell transplantation
- ICB
Immune checkpoint blockade
- IMiDs
Immunomodulatory imide drugs
- IPEX
Immunodysregulation polyendocrinopathy enteropathy X-linked
- irAEs
Immune-related adverse events
- ITIM
Immunoreceptor tyrosine-based inhibitory motif
- KIRs
Killer cell immunoglobulin-like receptors
- LAG-3
Lymphocyte-activation gene 3
- LILRB1
Leukocyte immunoglobulin-like receptor B1
- LRBA
Lipopolysaccharide-responsive and beige-like anchor protein
- mAb
Monoclonal antibodies
- MDS
Myelodysplastic syndrome
- MDSCs
Myeloid-derived suppressor cells
- MM
Multiple myeloma
- MPNs
Myeloproliferative neoplasms
- NHL
Non-Hodgkin lymphoma
- NK cell
Natural killer cell
- NKG2A
NK group 2 member A
- ORR
Objective response rate
- PD-1
Programmed cell death protein 1
- PD-L1
Programmed death ligand 1
- scRNA-seq
Single-cell RNA sequencing
- SCT
Stem cell transplant
- Siglec-10
Sialic acid-binding Ig-like lectin 10
- SIRPα
Signal-regulatory protein α
- TAMs
Tumor-associated macrophages
- TCR
T cell receptor
- TIGIT
T cell immunoreceptor with Ig and ITIM domains
- TIM-3
T cell immunoglobulin and mucin domain 3
- TMB
Tumor mutation burden
- TME
Tumor microenvironment
- Tregs
Regulatory T cells
- β2M
β2-microglobulin
Authors’ contributions
B.S and K.N. wrote the manuscript. M.J.S. critically reviewed and edited the manuscript. The authors read and approved the final manuscript.
Funding
M. J. S. is supported by a NH&MRC Investigator Grant (1173958) and Program Grant (1132519). K.N. is supported by the Naito Foundation and NHMRC Project Grant (1159593). M.J.S and K.N. were recipients of a Leukemia Foundation of Australia SERP grant.
Availability of data and materials
Not applicable
Consent for publication
Not applicable
Competing interests
Mark J. Smyth has research agreements with Bristol Myers Squibb and Tizona Therapeutics and serves on the Scientific Advisory Board of Tizona Therapeutics and Compass Therapeutics.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schadendorf D, Hodi FS, Robert C, Weber JS, Margolin K, Hamid O, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33(17):1889–1894. doi: 10.1200/JCO.2014.56.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen LT, Satoh T, Ryu MH, Chao Y, Kato K, Chung HC, et al. A phase 3 study of nivolumab in previously treated advanced gastric or gastroesophageal junction cancer (ATTRACTION-2): 2-year update data. Gastric Cancer. 2020;23(3):510–519. doi: 10.1007/s10120-019-01034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kato K, Cho BC, Takahashi M, Okada M, Lin CY, Chin K, et al. Nivolumab versus chemotherapy in patients with advanced oesophageal squamous cell carcinoma refractory or intolerant to previous chemotherapy (ATTRACTION-3): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(11):1506–1517. doi: 10.1016/S1470-2045(19)30626-6. [DOI] [PubMed] [Google Scholar]
- 5.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–1550. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg JE, Hoffman-Censits J, Powles T, van der Heijden MS, Balar AV, Necchi A, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387(10031):1909–1920. doi: 10.1016/S0140-6736(16)00561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2017;377(14):1345–1356. doi: 10.1056/NEJMoa1709684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei SC, Duffy CR, Allison JP. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 2018;8(9):1069–1086. doi: 10.1158/2159-8290.CD-18-0367. [DOI] [PubMed] [Google Scholar]
- 11.Sosa A, Lopez Cadena E, Simon Olive C, Karachaliou N, Rosell R. Clinical assessment of immune-related adverse events. Ther Adv Med Oncol. 2018;10:1758835918764628. doi: 10.1177/1758835918764628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunner MC, Chambers CA, Chan FK, Hanke J, Winoto A, Allison JP. CTLA-4-mediated inhibition of early events of T cell proliferation. J Immunol. 1999;162(10):5813–5820. [PubMed] [Google Scholar]
- 13.Egen JG, Allison JP. Cytotoxic T lymphocyte antigen-4 accumulation in the immunological synapse is regulated by TCR signal strength. Immunity. 2002;16(1):23–35. doi: 10.1016/s1074-7613(01)00259-x. [DOI] [PubMed] [Google Scholar]
- 14.Pentcheva-Hoang T, Egen JG, Wojnoonski K, Allison JP. B7-1 and B7-2 selectively recruit CTLA-4 and CD28 to the immunological synapse. Immunity. 2004;21(3):401–413. doi: 10.1016/j.immuni.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 15.Linsley PS, Brady W, Urnes M, Grosmaire LS, Damle NK, Ledbetter JA. CTLA-4 is a second receptor for the B cell activation antigen B7. J Exp Med. 1991;174(3):561–569. doi: 10.1084/jem.174.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linsley PS, Greene JL, Brady W, Bajorath J, Ledbetter JA, Peach R. Human B7-1 (CD80) and B7-2 (CD86) bind with similar avidities but distinct kinetics to CD28 and CTLA-4 receptors. Immunity. 1994;1(9):793–801. doi: 10.1016/s1074-7613(94)80021-9. [DOI] [PubMed] [Google Scholar]
- 17.van der Merwe PA, Bodian DL, Daenke S, Linsley P, Davis SJ. CD80 (B7-1) binds both CD28 and CTLA-4 with a low affinity and very fast kinetics. J Exp Med. 1997;185(3):393–403. doi: 10.1084/jem.185.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedline RH, Brown DS, Nguyen H, Kornfeld H, Lee J, Zhang Y, et al. CD4+ regulatory T cells require CTLA-4 for the maintenance of systemic tolerance. J Exp Med. 2009;206(2):421–434. doi: 10.1084/jem.20081811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Read S, Greenwald R, Izcue A, Robinson N, Mandelbrot D, Francisco L, et al. Blockade of CTLA-4 on CD4 + CD25+ regulatory T cells abrogates their function in vivo. J Immunol. 2006;177(7):4376–4383. doi: 10.4049/jimmunol.177.7.4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jain N, Nguyen H, Chambers C, Kang J. Dual function of CTLA-4 in regulatory T cells and conventional T cells to prevent multiorgan autoimmunity. Proc Natl Acad Sci U S A. 2010;107(4):1524–1528. doi: 10.1073/pnas.0910341107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, et al. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322(5899):271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 22.Boasso A, Herbeuval JP, Hardy AW, Winkler C, Shearer GM. Regulation of indoleamine 2,3-dioxygenase and tryptophanyl-tRNA-synthetase by CTLA-4-fc in human CD4+ T cells. Blood. 2005;105(4):1574–1581. doi: 10.1182/blood-2004-06-2089. [DOI] [PubMed] [Google Scholar]
- 23.Qureshi OS, Zheng Y, Nakamura K, Attridge K, Manzotti C, Schmidt EM, et al. Trans-endocytosis of CD80 and CD86: a molecular basis for the cell-extrinsic function of CTLA-4. Science. 2011;332(6029):600–603. doi: 10.1126/science.1202947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corse E, Allison JP. Cutting edge: CTLA-4 on effector T cells inhibits in trans. J Immunol. 2012;189(3):1123–1127. doi: 10.4049/jimmunol.1200695. [DOI] [PubMed] [Google Scholar]
- 25.Ovcinnikovs V, Ross EM, Petersone L, Edner NM, Heuts F, Ntavli E, et al. CTLA-4-mediated transendocytosis of costimulatory molecules primarily targets migratory dendritic cells. Sci Immunol. 2019;4(35):eaaw0902. doi: 10.1126/sciimmunol.aaw0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qureshi OS, Kaur S, Hou TZ, Jeffery LE, Poulter NS, Briggs Z, et al. Constitutive clathrin-mediated endocytosis of CTLA-4 persists during T cell activation. J Biol Chem. 2012;287(12):9429–9440. doi: 10.1074/jbc.M111.304329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lo B, Zhang K, Lu W, Zheng L, Zhang Q, Kanellopoulou C, et al. AUTOIMMUNE DISEASE. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science. 2015;349(6246):436–440. doi: 10.1126/science.aaa1663. [DOI] [PubMed] [Google Scholar]
- 28.Charbonnier LM, Janssen E, Chou J, Ohsumi TK, Keles S, Hsu JT, et al. Regulatory T-cell deficiency and immune dysregulation, polyendocrinopathy, enteropathy, X-linked-like disorder caused by loss-of-function mutations in LRBA. J Allergy Clin Immunol. 2015;135(1):217–227. doi: 10.1016/j.jaci.2014.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boutros C, Tarhini A, Routier E, Lambotte O, Ladurie FL, Carbonnel F, et al. Safety profiles of anti-CTLA-4 and anti-PD-1 antibodies alone and in combination. Nat Rev Clin Oncol. 2016;13(8):473–486. doi: 10.1038/nrclinonc.2016.58. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Y, Du X, Liu M, Tang F, Zhang P, Ai C, et al. Hijacking antibody-induced CTLA-4 lysosomal degradation for safer and more effective cancer immunotherapy. Cell Res. 2019;29(8):609–627. doi: 10.1038/s41422-019-0184-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5(12):1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- 32.Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192(7):1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Latchman Y, Wood CR, Chernova T, Chaudhary D, Borde M, Chernova I, et al. PD-L2 is a second ligand for PD-1 and inhibits T cell activation. Nat Immunol. 2001;2(3):261–268. doi: 10.1038/85330. [DOI] [PubMed] [Google Scholar]
- 34.Yokosuka T, Takamatsu M, Kobayashi-Imanishi W, Hashimoto-Tane A, Azuma M, Saito T. Programmed cell death 1 forms negative costimulatory microclusters that directly inhibit T cell receptor signaling by recruiting phosphatase SHP2. J Exp Med. 2012;209(6):1201–1217. doi: 10.1084/jem.20112741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hui E, Cheung J, Zhu J, Su X, Taylor MJ, Wallweber HA, et al. T cell costimulatory receptor CD28 is a primary target for PD-1-mediated inhibition. Science. 2017;355(6332):1428–1433. doi: 10.1126/science.aaf1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kamphorst AO, Wieland A, Nasti T, Yang S, Zhang R, Barber DL, et al. Rescue of exhausted CD8 T cells by PD-1-targeted therapies is CD28-dependent. Science. 2017;355(6332):1423–1427. doi: 10.1126/science.aaf0683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shimizu K, Sugiura D, Okazaki IM, Maruhashi T, Takegami Y, Cheng C, et al. PD-1 imposes qualitative control of cellular transcriptomes in response to T cell activation. Mol Cell. 2020;77(5):937–50.e6. doi: 10.1016/j.molcel.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 38.Zhao Y, Harrison DL, Song Y, Ji J, Huang J, Hui E. Antigen-presenting cell-intrinsic PD-1 neutralizes PD-L1 in cis to attenuate PD-1 signaling in T cells. Cell Rep. 2018;24(2):379–90.e6. doi: 10.1016/j.celrep.2018.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chaudhri A, Xiao Y, Klee AN, Wang X, Zhu B, Freeman GJ. PD-L1 binds to B7-1 only in cis on the same cell surface. Cancer Immunol Res. 2018;6(8):921–929. doi: 10.1158/2326-6066.CIR-17-0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sugiura D, Maruhashi T, Okazaki IM, Shimizu K, Maeda TK, Takemoto T, et al. Restriction of PD-1 function by cis-PD-L1/CD80 interactions is required for optimal T cell responses. Science. 2019;364(6440):558–566. doi: 10.1126/science.aav7062. [DOI] [PubMed] [Google Scholar]
- 41.Zhao Y, Lee CK, Lin CH, Gassen RB, Xu X, Huang Z, et al. PD-L1:CD80 cis-heterodimer triggers the co-stimulatory receptor CD28 while repressing the inhibitory PD-1 and CTLA-4 pathways. Immunity. 2019;51(6):1059–73.e9. doi: 10.1016/j.immuni.2019.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen G, Huang AC, Zhang W, Zhang G, Wu M, Xu W, et al. Exosomal PD-L1 contributes to immunosuppression and is associated with anti-PD-1 response. Nature. 2018;560(7718):382–386. doi: 10.1038/s41586-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rossille D, Gressier M, Damotte D, Maucort-Boulch D, Pangault C, Semana G, et al. High level of soluble programmed cell death ligand 1 in blood impacts overall survival in aggressive diffuse large B-cell lymphoma: results from a French multicenter clinical trial. Leukemia. 2014;28(12):2367–2375. doi: 10.1038/leu.2014.137. [DOI] [PubMed] [Google Scholar]
- 44.Lin H, Wei S, Hurt EM, Green MD, Zhao L, Vatan L, et al. Host expression of PD-L1 determines efficacy of PD-L1 pathway blockade-mediated tumor regression. J Clin Invest. 2018;128(2):805–815. doi: 10.1172/JCI96113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dakappagari N, Ho SN, Gascoyne RD, Ranuio J, Weng AP, Tangri S. CD80 (B7.1) is expressed on both malignant B cells and nonmalignant stromal cells in non-Hodgkin lymphoma. Cytometry B Clin Cytom. 2012;82(2):112–119. doi: 10.1002/cyto.b.20631. [DOI] [PubMed] [Google Scholar]
- 46.Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med. 2015;372(4):311–319. doi: 10.1056/NEJMoa1411087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Armand P, Engert A, Younes A, Fanale M, Santoro A, Zinzani PL, et al. Nivolumab for relapsed/refractory classic Hodgkin lymphoma after failure of autologous hematopoietic cell transplantation: extended follow-up of the multicohort single-arm phase II CheckMate 205 trial. J Clin Oncol. 2018;36(14):1428–1439. doi: 10.1200/JCO.2017.76.0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramchandren R, Domingo-Domènech E, Rueda A, Trněný M, Feldman TA, Lee HJ, et al. Nivolumab for newly diagnosed advanced-stage classic Hodgkin lymphoma: safety and efficacy in the phase II CheckMate 205 study. J Clin Oncol. 2019;37(23):1997–2007. doi: 10.1200/JCO.19.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Armand P, Shipp MA, Ribrag V, Michot JM, Zinzani PL, Kuruvilla J, et al. Programmed death-1 blockade with pembrolizumab in patients with classical Hodgkin lymphoma after brentuximab vedotin failure. J Clin Oncol. 2016;34(31):3733–3739. doi: 10.1200/JCO.2016.67.3467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen R, Zinzani PL, Fanale MA, Armand P, Johnson NA, Brice P, et al. Phase II study of the efficacy and safety of pembrolizumab for relapsed/refractory classic Hodgkin lymphoma. J Clin Oncol. 2017;35(19):2125–2132. doi: 10.1200/JCO.2016.72.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ansell SM, Minnema MC, Johnson P, Timmerman JM, Armand P, Shipp MA, et al. Nivolumab for relapsed/refractory diffuse large B-cell lymphoma in patients ineligible for or having failed autologous transplantation: a single-arm, phase II study. J Clin Oncol. 2019;37(6):481–489. doi: 10.1200/JCO.18.00766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nastoupil LJ, Westin JR, Fowler NH, Fanale MA, Samaniego F, Oki Y, et al. Response rates with pembrolizumab in combination with rituximab in patients with relapsed follicular lymphoma: interim results of an on open-label, phase II study. J Clin Oncol. 2017;35(15_suppl):7519. [Google Scholar]
- 53.Barraclough A, Chong G, Gilbertson M, Grigg A, Churilov L, Fancourt T, et al. Immune priming with single-agent nivolumab followed by combined nivolumab & rituximab is safe and efficacious for first-line treatment of follicular lymphoma; interim snalysis of the ‘1st FLOR’ study. Blood. 2019;134(Supplement_1):1523. [Google Scholar]
- 54.Iyer SP, Neelapu SS, Burns E, Nair R, Hosing C, Nieto Y, et al. A phase I/II study to examine the safety and efficacy of pembrolizumab 200 mg fixed dose administered every 3 weeks (Q3W) in combination with romidepsin in relapsed or refractory peripheral T-cell lymphoma (PTCL) Blood. 2019;134(Supplement_1):1546. [Google Scholar]
- 55.Khodadoust MS, Rook AH, Porcu P, Foss F, Moskowitz AJ, Shustov A, et al. Pembrolizumab in relapsed and refractory mycosis fungoides and Sézary syndrome: a multicenter phase II study. J Clin Oncol. 2020;38(1):20–28. doi: 10.1200/JCO.19.01056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mateos MV, Orlowski RZ, Ocio EM, Rodriguez-Otero P, Reece D, Moreau P, et al. Pembrolizumab combined with lenalidomide and low-dose dexamethasone for relapsed or refractory multiple myeloma: phase I KEYNOTE-023 study. Br J Haematol. 2019;186(5):e117–ee21. doi: 10.1111/bjh.15946. [DOI] [PubMed] [Google Scholar]
- 57.Mateos MV, Blacklock H, Schjesvold F, Oriol A, Simpson D, George A, et al. Pembrolizumab plus pomalidomide and dexamethasone for patients with relapsed or refractory multiple myeloma (KEYNOTE-183): a randomised, open-label, phase 3 trial. Lancet Haematol. 2019;6(9):e459–ee69. doi: 10.1016/S2352-3026(19)30110-3. [DOI] [PubMed] [Google Scholar]
- 58.Usmani SZ, Schjesvold F, Oriol A, Karlin L, Cavo M, Rifkin RM, et al. Pembrolizumab plus lenalidomide and dexamethasone for patients with treatment-naive multiple myeloma (KEYNOTE-185): a randomised, open-label, phase 3 trial. Lancet Haematol. 2019;6(9):e448–ee58. doi: 10.1016/S2352-3026(19)30109-7. [DOI] [PubMed] [Google Scholar]
- 59.Davids MS, Kim HT, Bachireddy P, Costello C, Liguori R, Savell A, et al. Ipilimumab for patients with relapse after allogeneic transplantation. N Engl J Med. 2016;375(2):143–153. doi: 10.1056/NEJMoa1601202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Daver N, Garcia-Manero G, Basu S, Boddu PC, Alfayez M, Cortes JE, et al. Efficacy, safety, and biomarkers of response to azacitidine and nivolumab in relapsed/refractory acute myeloid leukemia: a nonrandomized, open-label, phase II study. Cancer Discov. 2019;9(3):370–383. doi: 10.1158/2159-8290.CD-18-0774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Younes A, Santoro A, Shipp M, Zinzani PL, Timmerman JM, Ansell S, et al. Nivolumab for classical Hodgkin’s lymphoma after failure of both autologous stem-cell transplantation and brentuximab vedotin: a multicentre, multicohort, single-arm phase 2 trial. Lancet Oncol. 2016;17(9):1283–1294. doi: 10.1016/S1470-2045(16)30167-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goodman AM, Kato S, Bazhenova L, Patel SP, Frampton GM, Miller V, et al. Tumor mutational burden as an independent predictor of response to immunotherapy in diverse cancers. Mol Cancer Ther. 2017;16(11):2598–2608. doi: 10.1158/1535-7163.MCT-17-0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Keenan TE, Burke KP, Van Allen EM. Genomic correlates of response to immune checkpoint blockade. Nat Med. 2019;25(3):389–402. doi: 10.1038/s41591-019-0382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liang WS, Vergilio JA, Salhia B, Huang HJ, Oki Y, Garrido-Laguna I, et al. Comprehensive genomic profiling of Hodgkin lymphoma reveals recurrently mutated genes and increased mutation burden. Oncologist. 2019;24(2):219–228. doi: 10.1634/theoncologist.2018-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xu-Monette ZY, Zhou J, Young KH. PD-1 expression and clinical PD-1 blockade in B-cell lymphomas. Blood. 2018;131(1):68–83. doi: 10.1182/blood-2017-07-740993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Green MR, Rodig S, Juszczynski P, Ouyang J, Sinha P, O'Donnell E, et al. Constitutive AP-1 activity and EBV infection induce PD-L1 in Hodgkin lymphomas and posttransplant lymphoproliferative disorders: implications for targeted therapy. Clin Cancer Res. 2012;18(6):1611–1618. doi: 10.1158/1078-0432.CCR-11-1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roemer MG, Advani RH, Ligon AH, Natkunam Y, Redd RA, Homer H, et al. PD-L1 and PD-L2 genetic alterations define classical Hodgkin lymphoma and predict outcome. J Clin Oncol. 2016;34(23):2690–2697. doi: 10.1200/JCO.2016.66.4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carbone A, Gloghini A, Carlo-Stella C. Are EBV-related and EBV-unrelated Hodgkin lymphomas different with regard to susceptibility to checkpoint blockade? Blood. 2018;132(1):17–22. doi: 10.1182/blood-2018-02-833806. [DOI] [PubMed] [Google Scholar]
- 69.Scott DW, Gascoyne RD. The tumour microenvironment in B cell lymphomas. Nat Rev Cancer. 2014;14(8):517–534. doi: 10.1038/nrc3774. [DOI] [PubMed] [Google Scholar]
- 70.Kline J, Godfrey J, Ansell SM. The immune landscape and response to immune checkpoint blockade therapy in lymphoma. Blood. 2020;135(8):523–533. doi: 10.1182/blood.2019000847. [DOI] [PubMed] [Google Scholar]
- 71.Cader FZ, Schackmann RCJ, Hu X, Wienand K, Redd R, Chapuy B, et al. Mass cytometry of Hodgkin lymphoma reveals a CD4(+) regulatory T-cell-rich and exhausted T-effector microenvironment. Blood. 2018;132(8):825–836. doi: 10.1182/blood-2018-04-843714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roemer MGM, Redd RA, Cader FZ, Pak CJ, Abdelrahman S, Ouyang J, et al. Major histocompatibility complex class II and programmed death ligand 1 expression predict outcome after programmed death 1 blockade in classic Hodgkin lymphoma. J Clin Oncol. 2018;36(10):942–950. doi: 10.1200/JCO.2017.77.3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Patel SS, Weirather JL, Lipschitz M, Lako A, Chen PH, Griffin GK, et al. The microenvironmental niche in classic Hodgkin lymphoma is enriched for CTLA-4-positive T cells that are PD-1-negative. Blood. 2019;134(23):2059–2069. doi: 10.1182/blood.2019002206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aoki T, Chong LC, Takata K, Milne K, Hav M, Colombo A, et al. Single-cell transcriptome analysis reveals disease-defining T-cell subsets in the tumor microenvironment of classic Hodgkin lymphoma. Cancer Discov. 2020;10(3):406–421. doi: 10.1158/2159-8290.CD-19-0680. [DOI] [PubMed] [Google Scholar]
- 75.Vari F, Arpon D, Keane C, Hertzberg MS, Talaulikar D, Jain S, et al. Immune evasion via PD-1/PD-L1 on NK cells and monocyte/macrophages is more prominent in Hodgkin lymphoma than DLBCL. Blood. 2018;131(16):1809–1819. doi: 10.1182/blood-2017-07-796342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Younes A, Brody J, Carpio C, Lopez-Guillermo A, Ben-Yehuda D, Ferhanoglu B, et al. Safety and activity of ibrutinib in combination with nivolumab in patients with relapsed non-Hodgkin lymphoma or chronic lymphocytic leukaemia: a phase 1/2a study. Lancet Haematol. 2019;6(2):e67–e78. doi: 10.1016/S2352-3026(18)30217-5. [DOI] [PubMed] [Google Scholar]
- 77.Pericart S, Tosolini M, Gravelle P, Rossi C, Traverse-Glehen A, Amara N, et al. Profiling immune escape in Hodgkin’s and diffuse large B-cell lymphomas using the transcriptome and immunostaining. Cancers (Basel) 2018;10(11):415. doi: 10.3390/cancers10110415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Keane C, Vari F, Hertzberg M, Cao KA, Green MR, Han E, et al. Ratios of T-cell immune effectors and checkpoint molecules as prognostic biomarkers in diffuse large B-cell lymphoma: a population-based study. Lancet Haematol. 2015;2(10):e445–e455. doi: 10.1016/S2352-3026(15)00150-7. [DOI] [PubMed] [Google Scholar]
- 79.Xu-Monette ZY, Xiao M, Au Q, Padmanabhan R, Xu B, Hoe N, et al. Immune profiling and quantitative analysis decipher the clinical role of immune-checkpoint expression in the tumor immune microenvironment of DLBCL. Cancer Immunol Res. 2019;7(4):644–657. doi: 10.1158/2326-6066.CIR-18-0439. [DOI] [PubMed] [Google Scholar]
- 80.Ennishi D, Jiang A, Boyle M, Collinge B, Grande BM, Ben-Neriah S, et al. Double-hit gene expression signature defines a distinct subgroup of germinal center B-cell-like diffuse large B-cell lymphoma. J Clin Oncol. 2019;37(3):190–201. doi: 10.1200/JCO.18.01583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang X, Cao X, Sun R, Tang C, Tzankov A, Zhang J, et al. Clinical significance of PTEN deletion, mutation, and loss of PTEN expression in de novo diffuse large B-cell lymphoma. Neoplasia. 2018;20(6):574–593. doi: 10.1016/j.neo.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jiang XN, Yu BH, Yan WH, Lee J, Zhou XY, Li XQ. Epstein-Barr virus-positive diffuse large B-cell lymphoma features disrupted antigen capture/presentation and hijacked T-cell suppression. Oncoimmunology. 2020;9(1):1683346. doi: 10.1080/2162402X.2019.1683346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ennishi D, Takata K, Beguelin W, Duns G, Mottok A, Farinha P, et al. Molecular and genetic characterization of MHC deficiency identifies EZH2 as therapeutic target for enhancing immune recognition. Cancer Discov. 2019;9(4):546–563. doi: 10.1158/2159-8290.CD-18-1090. [DOI] [PubMed] [Google Scholar]
- 84.Burr ML, Sparbier CE, Chan KL, Chan YC, Kersbergen A, Lam EYN, et al. An evolutionarily conserved function of polycomb silences the MHC Class I antigen presentation pathway and enables immune evasion in cancer. Cancer Cell. 2019;36(4):385–401.e8. [DOI] [PMC free article] [PubMed]
- 85.Grywalska E, Rolinski J. Epstein-Barr virus-associated lymphomas. Semin Oncol. 2015;42(2):291–303. doi: 10.1053/j.seminoncol.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 86.Kim SJ, Hyeon J, Cho I, Ko YH, Kim WS. Comparison of efficacy of pembrolizumab between Epstein-Barr virus–positive and –negative relapsed or refractory non-Hodgkin lymphomas. Cancer Res Treat. 2019;51(2):611–622. doi: 10.4143/crt.2018.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kataoka K, Miyoshi H, Sakata S, Dobashi A, Couronné L, Kogure Y, et al. Frequent structural variations involving programmed death ligands in Epstein-Barr virus-associated lymphomas. Leukemia. 2019;33(7):1687–1699. doi: 10.1038/s41375-019-0380-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Godfrey J, Tumuluru S, Bao R, Leukam M, Venkataraman G, Phillip J, et al. PD-L1 gene alterations identify a subset of diffuse large B-cell lymphoma harboring a T-cell-inflamed phenotype. Blood. 2019;133(21):2279–2290. doi: 10.1182/blood-2018-10-879015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kwong YL, Chan TSY, Tan D, Kim SJ, Poon LM, Mow B, et al. PD1 blockade with pembrolizumab is highly effective in relapsed or refractory NK/T-cell lymphoma failing l-asparaginase. Blood. 2017;129(17):2437–2442. doi: 10.1182/blood-2016-12-756841. [DOI] [PubMed] [Google Scholar]
- 90.Li X, Cheng Y, Zhang M, Yan J, Li L, Fu X, et al. Activity of pembrolizumab in relapsed/refractory NK/T-cell lymphoma. J Hematol Oncol. 2018;11(1):15. doi: 10.1186/s13045-018-0559-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Barta SK, Zain J, MacFarlane AW, Smith SM, Ruan J, Fung HC, et al. Phase II study of the PD-1 inhibitor pembrolizumab for the treatment of relapsed or refractory mature T-cell lymphoma. Clin Lymphoma Myeloma Leuk. 2019;19(6):356–64.e3. doi: 10.1016/j.clml.2019.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ratner L, Waldmann TA, Janakiram M, Brammer JE. Rapid progression of adult T-cell leukemia-lymphoma after PD-1 inhibitor therapy. N Engl J Med. 2018;378(20):1947–1948. doi: 10.1056/NEJMc1803181. [DOI] [PubMed] [Google Scholar]
- 93.Rauch DA, Conlon KC, Janakiram M, Brammer JE, Harding JC, Ye BH, et al. Rapid progression of adult T-cell leukemia/lymphoma as tumor-infiltrating Tregs after PD-1 blockade. Blood. 2019;134(17):1406–1414. doi: 10.1182/blood.2019002038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wartewig T, Kurgyis Z, Keppler S, Pechloff K, Hameister E, Öllinger R, et al. PD-1 is a haploinsufficient suppressor of T cell lymphomagenesis. Nature. 2017;552(7683):121–125. doi: 10.1038/nature24649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nakamura K, Smyth MJ, Martinet L. Cancer immunoediting and immune dysregulation in multiple myeloma. Blood. 2020. Jul 9;blood.2020006540. [DOI] [PubMed]
- 96.Zhao Y, Shao Q, Peng G. Exhaustion and senescence: two crucial dysfunctional states of T cells in the tumor microenvironment. Cell Mol Immunol. 2020;17(1):27–35. doi: 10.1038/s41423-019-0344-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bailur JK, McCachren SS, Doxie DB, Shrestha M, Pendleton K, Nooka AK, et al. Early alterations in stem-like/resident T cells, innate and myeloid cells in the bone marrow in preneoplastic gammopathy. JCI Insight. 2019;5. [DOI] [PMC free article] [PubMed]
- 98.Chung DJ, Pronschinske KB, Shyer JA, Sharma S, Leung S, Curran SA, et al. T-cell exhaustion in multiple myeloma relapse after autotransplant: optimal timing of immunotherapy. Cancer Immunol Res. 2016;4(1):61–71. doi: 10.1158/2326-6066.CIR-15-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nakamura K, Kassem S, Cleynen A, Chretien ML, Guillerey C, Putz EM, et al. Dysregulated IL-18 is a key driver of immunosuppression and a possible therapeutic target in the multiple myeloma microenvironment. Cancer Cell. 2018;33(4):634–48.e5. [DOI] [PubMed]
- 100.Krejcik J, Casneuf T, Nijhof IS, Verbist B, Bald J, Plesner T, et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128(3):384–394. doi: 10.1182/blood-2015-12-687749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Badros AZ, Ma N, Rapoport AP, Lederer E, Lesokhin AM. Long-term remissions after stopping pembrolizumab for relapsed or refractory multiple myeloma. Blood Adv. 2019;3(11):1658–1660. doi: 10.1182/bloodadvances.2019000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Guillerey C, Harjunpää H, Carrié N, Kassem S, Teo T, Miles K, et al. TIGIT immune checkpoint blockade restores CD8(+) T-cell immunity against multiple myeloma. Blood. 2018;132(16):1689–1694. doi: 10.1182/blood-2018-01-825265. [DOI] [PubMed] [Google Scholar]
- 103.Berger R, Rotem-Yehudar R, Slama G, Landes S, Kneller A, Leiba M, et al. Phase I safety and pharmacokinetic study of CT-011, a humanized antibody interacting with PD-1, in patients with advanced hematologic malignancies. Clin Cancer Res. 2008;14(10):3044–3051. doi: 10.1158/1078-0432.CCR-07-4079. [DOI] [PubMed] [Google Scholar]
- 104.Garcia-Manero G, Tallman MS, Martinelli G, Ribrag V, Yang H, Balakumaran A, et al. Pembrolizumab, a PD-1 inhibitor, in patients with myelodysplastic syndrome (MDS) after failure of hypomethylating agent treatment. Blood. 2016;128(22):345. [Google Scholar]
- 105.Zeidan AM, Knaus HA, Robinson TM, Towlerton AMH, Warren EH, Zeidner JF, et al. A multi-center phase I trial of ipilimumab in patients with myelodysplastic syndromes following hypomethylating agent failure. Clin Cancer Res. 2018;24(15):3519–3527. doi: 10.1158/1078-0432.CCR-17-3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liao D, Wang M, Liao Y, Li J, Niu T. A review of efficacy and safety of checkpoint inhibitor for the treatment of acute myeloid leukemia. Front Pharmacol. 2019;10:609. doi: 10.3389/fphar.2019.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kong Y, Zhu L, Schell TD, Zhang J, Claxton DF, Ehmann WC, et al. T-cell immunoglobulin and ITIM domain (TIGIT) associates with CD8+ T-cell exhaustion and poor clinical outcome in AML patients. Clin Cancer Res. 2016;22(12):3057–3066. doi: 10.1158/1078-0432.CCR-15-2626. [DOI] [PubMed] [Google Scholar]
- 108.Wang M, Bu J, Zhou M, Sido J, Lin Y, Liu G, et al. CD8(+)T cells expressing both PD-1 and TIGIT but not CD226 are dysfunctional in acute myeloid leukemia (AML) patients. Clin Immunol. 2018;190:64–73. doi: 10.1016/j.clim.2017.08.021. [DOI] [PubMed] [Google Scholar]
- 109.Christopher MJ, Petti AA, Rettig MP, Miller CA, Chendamarai E, Duncavage EJ, et al. Immune escape of relapsed AML cells after allogeneic transplantation. N Engl J Med. 2018;379(24):2330–2341. doi: 10.1056/NEJMoa1808777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kong Y, Zhang J, Claxton DF, Ehmann WC, Rybka WB, Zhu L, et al. PD-1(hi)TIM-3(+) T cells associate with and predict leukemia relapse in AML patients post allogeneic stem cell transplantation. Blood Cancer J. 2015;5(7):e330. doi: 10.1038/bcj.2015.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Vannucchi AM, Harrison CN. Emerging treatments for classical myeloproliferative neoplasms. Blood. 2017;129(6):693–703. doi: 10.1182/blood-2016-10-695965. [DOI] [PubMed] [Google Scholar]
- 112.Prestipino A, Emhardt AJ, Aumann K, O'Sullivan D, Gorantla SP, Duquesne S, et al. Sci Transl Med. 2018;10(429):eaam7729. doi: 10.1126/scitranslmed.aam7729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Holmström MO, Hjortsø MD, Ahmad SM, Met Ö, Martinenaite E, Riley C, et al. The JAK2V617F mutation is a target for specific T cells in the JAK2V617F-positive myeloproliferative neoplasms. Leukemia. 2017;31(2):495–498. doi: 10.1038/leu.2016.290. [DOI] [PubMed] [Google Scholar]
- 114.Klampfl T, Gisslinger H, Harutyunyan AS, Nivarthi H, Rumi E, Milosevic JD, et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013;369(25):2379–2390. doi: 10.1056/NEJMoa1311347. [DOI] [PubMed] [Google Scholar]
- 115.Cimen Bozkus C, Roudko V, Finnigan JP, Mascarenhas J, Hoffman R, Iancu-Rubin C, et al. Immune checkpoint blockade enhances shared neoantigen-induced T-cell immunity directed against mutated calreticulin in myeloproliferative neoplasms. Cancer Discov. 2019;9(9):1192–1207. doi: 10.1158/2159-8290.CD-18-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Holmström MO, Martinenaite E, Ahmad SM, Met Ö, Friese C, Kjær L, et al. The calreticulin (CALR) exon 9 mutations are promising targets for cancer immune therapy. Leukemia. 2018;32(2):429–437. doi: 10.1038/leu.2017.214. [DOI] [PubMed] [Google Scholar]
- 117.Andrews LP, Marciscano AE, Drake CG, Vignali DA. LAG3 (CD223) as a cancer immunotherapy target. Immunol Rev. 2017;276(1):80–96. doi: 10.1111/imr.12519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Maruhashi T, Okazaki IM, Sugiura D, Takahashi S, Maeda TK, Shimizu K, et al. LAG-3 inhibits the activation of CD4(+) T cells that recognize stable pMHCII through its conformation-dependent recognition of pMHCII. Nat Immunol. 2018;19(12):1415–1426. doi: 10.1038/s41590-018-0217-9. [DOI] [PubMed] [Google Scholar]
- 119.Grosso JF, Kelleher CC, Harris TJ, Maris CH, Hipkiss EL, De Marzo A, et al. LAG-3 regulates CD8+ T cell accumulation and effector function in murine self- and tumor-tolerance systems. J Clin Invest. 2007;117(11):3383–3392. doi: 10.1172/JCI31184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Woo SR, Turnis ME, Goldberg MV, Bankoti J, Selby M, Nirschl CJ, et al. Immune inhibitory molecules LAG-3 and PD-1 synergistically regulate T-cell function to promote tumoral immune escape. Cancer Res. 2012;72(4):917–927. doi: 10.1158/0008-5472.CAN-11-1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang J, Sanmamed MF, Datar I, Su TT, Ji L, Sun J, et al. Fibrinogen-like protein 1 is a major immune inhibitory ligand of LAG-3. Cell. 2019;176(1-2):334–47.e12. doi: 10.1016/j.cell.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Keane C, Law SC, Gould C, Birch S, Sabdia MB. Merida de Long L, et al. LAG3: a novel immune checkpoint expressed by multiple lymphocyte subsets in diffuse large B-cell lymphoma. Blood Adv. 2020;4(7):1367–1377. doi: 10.1182/bloodadvances.2019001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Koyama S, Akbay EA, Li YY, Herter-Sprie GS, Buczkowski KA, Richards WG, et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat Commun. 2016;7:10501. doi: 10.1038/ncomms10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ngiow SF, von Scheidt B, Akiba H, Yagita H, Teng MW, Smyth MJ. Anti-TIM3 antibody promotes T cell IFN-γ-mediated antitumor immunity and suppresses established tumors. Cancer Res. 2011;71(10):3540–3551. doi: 10.1158/0008-5472.CAN-11-0096. [DOI] [PubMed] [Google Scholar]
- 125.Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J Exp Med. 2010;207(10):2187–2194. doi: 10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Anderson AC. Tim-3: an emerging target in the cancer immunotherapy landscape. Cancer Immunol Res. 2014;2(5):393–398. doi: 10.1158/2326-6066.CIR-14-0039. [DOI] [PubMed] [Google Scholar]
- 127.de Mingo PÁ, Gardner A, Hiebler S, Soliman H, Rugo HS, Krummel MF, et al. TIM-3 regulates CD103(+) dendritic cell function and response to chemotherapy in breast cancer. Cancer Cell. 2018;33(1):60–74.e6. doi: 10.1016/j.ccell.2017.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Huang X, Bai X, Cao Y, Wu J, Huang M, Tang D, et al. Lymphoma endothelium preferentially expresses Tim-3 and facilitates the progression of lymphoma by mediating immune evasion. J Exp Med. 2010;207(3):505–520. doi: 10.1084/jem.20090397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kikushige Y, Shima T, Takayanagi S, Urata S, Miyamoto T, Iwasaki H, et al. TIM-3 is a promising target to selectively kill acute myeloid leukemia stem cells. Cell Stem Cell. 2010;7(6):708–717. doi: 10.1016/j.stem.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 130.Kikushige Y, Miyamoto T, Yuda J, Jabbarzadeh-Tabrizi S, Shima T, Takayanagi S, et al. A TIM-3/Gal-9 autocrine stimulatory loop drives self-renewal of human myeloid leukemia stem cells and leukemic progression. Cell Stem Cell. 2015;17(3):341–352. doi: 10.1016/j.stem.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 131.Li C, Chen X, Yu X, Zhu Y, Ma C, Xia R, et al. Tim-3 is highly expressed in T cells in acute myeloid leukemia and associated with clinicopathological prognostic stratification. Int J Clin Exp Pathol. 2014;7(10):6880–6888. [PMC free article] [PubMed] [Google Scholar]
- 132.Harding JJ, Patnaik A, Moreno V, Stein M, Jankowska AM, Mendizabal NVd, et al. A phase Ia/Ib study of an anti-TIM-3 antibody (LY3321367) monotherapy or in combination with an anti-PD-L1 antibody (LY3300054): interim safety, efficacy, and pharmacokinetic findings in advanced cancers. J Clin Oncol. 2019;37(8_suppl):12.
- 133.Blake SJ, Dougall WC, Miles JJ, Teng MW, Smyth MJ. Molecular pathways: targeting CD96 and TIGIT for cancer immunotherapy. Clin Cancer Res. 2016;22(21):5183–5188. doi: 10.1158/1078-0432.CCR-16-0933. [DOI] [PubMed] [Google Scholar]
- 134.Zhu Y, Paniccia A, Schulick AC, Chen W, Koenig MR, Byers JT, et al. Identification of CD112R as a novel checkpoint for human T cells. J Exp Med. 2016;213(2):167–176. doi: 10.1084/jem.20150785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Manieri NA, Chiang EY, Grogan JL. TIGIT: a key inhibitor of the cancer immunity cycle. Trends Immunol. 2017;38(1):20–28. doi: 10.1016/j.it.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 136.Kurtulus S, Sakuishi K, Ngiow SF, Joller N, Tan DJ, Teng MW, et al. TIGIT predominantly regulates the immune response via regulatory T cells. J Clin Invest. 2015;125(11):4053–4062. doi: 10.1172/JCI81187. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 137.Minnie SA, Kuns RD, Gartlan KH, Zhang P, Wilkinson AN, Samson L, et al. Myeloma escape after stem cell transplantation is a consequence of T-cell exhaustion and is prevented by TIGIT blockade. Blood. 2018;132(16):1675–1688. doi: 10.1182/blood-2018-01-825240. [DOI] [PubMed] [Google Scholar]
- 138.Zhang Q, Bi J, Zheng X, Chen Y, Wang H, Wu W, et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity. Nat Immunol. 2018;19(7):723–732. doi: 10.1038/s41590-018-0132-0. [DOI] [PubMed] [Google Scholar]
- 139.Guillerey C, Huntington ND, Smyth MJ. Targeting natural killer cells in cancer immunotherapy. Nat Immunol. 2016;17(9):1025–1036. doi: 10.1038/ni.3518. [DOI] [PubMed] [Google Scholar]
- 140.Nakamura K, Smyth MJ. Myeloid immunosuppression and immune checkpoints in the tumor microenvironment. Cell Mol Immunol. 2020;17(1):1–12. doi: 10.1038/s41423-019-0306-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Raulet DH, Vance RE. Self-tolerance of natural killer cells. Nat Rev Immunol. 2006;6(7):520–531. doi: 10.1038/nri1863. [DOI] [PubMed] [Google Scholar]
- 142.Kamiya T, Seow SV, Wong D, Robinson M, Campana D. Blocking expression of inhibitory receptor NKG2A overcomes tumor resistance to NK cells. J Clin Invest. 2019;129(5):2094–2106. doi: 10.1172/JCI123955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Mahaweni NM, Ehlers FAI, Bos GMJ, Wieten L. Tuning natural killer cell anti-multiple myeloma reactivity by targeting inhibitory signaling via KIR and NKG2A. Front Immunol. 2018;9:2848. doi: 10.3389/fimmu.2018.02848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.André P, Denis C, Soulas C, Bourbon-Caillet C, Lopez J, Arnoux T, et al. Anti-NKG2A mAb is a checkpoint inhibitor that promotes anti-tumor immunity by unleashing both T and NK cells. Cell. 2018;175(7):1731–43.e13. doi: 10.1016/j.cell.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Benson DM, Jr, Hofmeister CC, Padmanabhan S, Suvannasankha A, Jagannath S, Abonour R, et al. A phase 1 trial of the anti-KIR antibody IPH2101 in patients with relapsed/refractory multiple myeloma. Blood. 2012;120(22):4324–4333. doi: 10.1182/blood-2012-06-438028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Vey N, Bourhis JH, Boissel N, Bordessoule D, Prebet T, Charbonnier A, et al. A phase 1 trial of the anti-inhibitory KIR mAb IPH2101 for AML in complete remission. Blood. 2012;120(22):4317–4323. doi: 10.1182/blood-2012-06-437558. [DOI] [PubMed] [Google Scholar]
- 147.Korde N, Carlsten M, Lee MJ, Minter A, Tan E, Kwok M, et al. A phase II trial of pan-KIR2D blockade with IPH2101 in smoldering multiple myeloma. Haematologica. 2014;99(6):e81–e83. doi: 10.3324/haematol.2013.103085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Benson DM, Jr, Cohen AD, Jagannath S, Munshi NC, Spitzer G, Hofmeister CC, et al. A phase I trial of the anti-KIR antibody IPH2101 and lenalidomide in patients with relapsed/refractory multiple myeloma. Clin Cancer Res. 2015;21(18):4055–4061. doi: 10.1158/1078-0432.CCR-15-0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Armand P, Lesokhin A, Borrello I, Timmerman J, Gutierrez M, Zhu L, et al. A phase 1b study of dual PD-1 and CTLA-4 or KIR blockade in patients with relapsed/refractory lymphoid malignancies. Leukemia. 2020. [DOI] [PMC free article] [PubMed]
- 150.Feng M, Jiang W, Kim BYS, Zhang CC, Fu YX, Weissman IL. Phagocytosis checkpoints as new targets for cancer immunotherapy. Nat Rev Cancer. 2019;19(10):568–586. doi: 10.1038/s41568-019-0183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Barclay AN, Brown MH. The SIRP family of receptors and immune regulation. Nat Rev Immunol. 2006;6(6):457–464. doi: 10.1038/nri1859. [DOI] [PubMed] [Google Scholar]
- 152.Liu X, Pu Y, Cron K, Deng L, Kline J, Frazier WA, et al. CD47 blockade triggers T cell-mediated destruction of immunogenic tumors. Nat Med. 2015;21(10):1209–1215. doi: 10.1038/nm.3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chao MP, Alizadeh AA, Tang C, Myklebust JH, Varghese B, Gill S, et al. Anti-CD47 antibody synergizes with rituximab to promote phagocytosis and eradicate non-Hodgkin lymphoma. Cell. 2010;142(5):699–713. doi: 10.1016/j.cell.2010.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Advani R, Flinn I, Popplewell L, Forero A, Bartlett NL, Ghosh N, et al. CD47 blockade by Hu5F9-G4 and rituximab in non-Hodgkin’s lymphoma. N Engl J Med. 2018;379(18):1711–1721. doi: 10.1056/NEJMoa1807315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Barkal AA, Weiskopf K, Kao KS, Gordon SR, Rosental B, Yiu YY, et al. Engagement of MHC class I by the inhibitory receptor LILRB1 suppresses macrophages and is a target of cancer immunotherapy. Nat Immunol. 2018;19(1):76–84. doi: 10.1038/s41590-017-0004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Barkal AA, Brewer RE, Markovic M, Kowarsky M, Barkal SA, Zaro BW, et al. CD24 signalling through macrophage Siglec-10 is a target for cancer immunotherapy. Nature. 2019;572(7769):392–396. doi: 10.1038/s41586-019-1456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Nakamura K, Casey M, Oey H, Vari F, Stagg J, Gandhi MK, et al. Targeting an adenosine-mediated “don’t eat me signal” augments anti-lymphoma immunity by anti-CD20 monoclonal antibody. Leukemia. 2020. 10.1038/s41375-020-0811-3. [DOI] [PubMed]
- 158.Jackson HJ, Rafiq S, Brentjens RJ. Driving CAR T-cells forward. Nat Rev Clin Oncol. 2016;13(6):370–383. doi: 10.1038/nrclinonc.2016.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380(1):45–56. doi: 10.1056/NEJMoa1804980. [DOI] [PubMed] [Google Scholar]
- 160.Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Locke FL, Ghobadi A, Jacobson CA, Miklos DB, Lekakis LJ, Oluwole OO, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019;20(1):31–42. doi: 10.1016/S1470-2045(18)30864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kochenderfer JN, Somerville RPT, Lu T, Yang JC, Sherry RM, Feldman SA, et al. Long-duration complete remissions of diffuse large B cell lymphoma after anti-CD19 chimeric antigen receptor T cell therapy. Mol Ther. 2017;25(10):2245–2253. doi: 10.1016/j.ymthe.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kochenderfer JN, Dudley ME, Kassim SH, Somerville RP, Carpenter RO, Stetler-Stevenson M, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33(6):540–549. doi: 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kochenderfer JN, Dudley ME, Feldman SA, Wilson WH, Spaner DE, Maric I, et al. B-cell depletion and remissions of malignancy along with cytokine-associated toxicity in a clinical trial of anti-CD19 chimeric-antigen-receptor-transduced T cells. Blood. 2012;119(12):2709–2720. doi: 10.1182/blood-2011-10-384388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang M, Munoz J, Goy A, Locke FL, Jacobson CA, Hill BT, et al. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2020;382(14):1331–1342. doi: 10.1056/NEJMoa1914347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Porter DL, Hwang WT, Frey NV, Lacey SF, Shaw PA, Loren AW, et al. Chimeric antigen receptor T cells persist and induce sustained remissions in relapsed refractory chronic lymphocytic leukemia. Sci Transl Med. 2015;7(303):303ra139. doi: 10.1126/scitranslmed.aac5415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371(16):1507–1517. doi: 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Fraietta JA, Lacey SF, Orlando EJ, Pruteanu-Malinici I, Gohil M, Lundh S, et al. Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia. Nat Med. 2018;24(5):563–571. doi: 10.1038/s41591-018-0010-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Locke FL, Westin JR, Miklos DB, Herrara AF, Jacobson CA, Lee J, et al. Phase 1 results from ZUMA-6: axicabtagene ciloleucel (axi-cel; KTE-C19) in combination with atezolizumab for the treatment of patients with refractory diffuse large B cell lymphoma (DLBCL) Blood. 2017;130(Supplement 1):2826. [Google Scholar]
- 170.Siddiqi T, Abramson JS, Lee HJ, Schuster S, Hasskarl J, Montheard S, et al. Safety of lisocabtagene maraleucel given with durvalumab in patients with relapsed/refractory aggressive B-cell non Hodgkin lymphoma: first results from the platform study. Hematol Oncol. 2019;37(S2):171–172. [Google Scholar]
- 171.Li AM, Hucks GE, Dinofia AM, Seif AE, Teachey DT, Baniewicz D, et al. Checkpoint inhibitors augment CD19-directed chimeric antigen receptor (CAR) T cell therapy in relapsed B-cell acute lymphoblastic leukemia. Blood. 2018;132(Supplement 1):556. [Google Scholar]
- 172.Curran KJ, Seinstra BA, Nikhamin Y, Yeh R, Usachenko Y, van Leeuwen DG, et al. Enhancing antitumor efficacy of chimeric antigen receptor T cells through constitutive CD40L expression. Mol Ther. 2015;23(4):769–778. doi: 10.1038/mt.2015.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lai J, Mardiana S, House IG, Sek K, Henderson MA, Giuffrida L, et al. Adoptive cellular therapy with T cells expressing the dendritic cell growth factor Flt3L drives epitope spreading and antitumor immunity. Nat Immunol. 2020;21(8):914–26. [DOI] [PubMed]
- 174.Yeku OO, Purdon TJ, Koneru M, Spriggs D, Brentjens RJ. Armored CAR T cells enhance antitumor efficacy and overcome the tumor microenvironment. Sci Rep. 2017;7(1):10541. doi: 10.1038/s41598-017-10940-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Pegram HJ, Purdon TJ, van Leeuwen DG, Curran KJ, Giralt SA, Barker JN, et al. IL-12-secreting CD19-targeted cord blood-derived T cells for the immunotherapy of B-cell acute lymphoblastic leukemia. Leukemia. 2015;29(2):415–422. doi: 10.1038/leu.2014.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Avanzi MP, Yeku O, Li X, Wijewarnasuriya DP, van Leeuwen DG, Cheung K, et al. Engineered tumor-targeted T cells mediate enhanced anti-tumor efficacy both directly and through activation of the endogenous immune system. Cell Rep. 2018;23(7):2130–2141. doi: 10.1016/j.celrep.2018.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cherkassky L, Morello A, Villena-Vargas J, Feng Y, Dimitrov DS, Jones DR, et al. Human CAR T cells with cell-intrinsic PD-1 checkpoint blockade resist tumor-mediated inhibition. J Clin Invest. 2016;126(8):3130–3144. doi: 10.1172/JCI83092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Rupp LJ, Schumann K, Roybal KT, Gate RE, Ye CJ, Lim WA, et al. CRISPR/Cas9-mediated PD-1 disruption enhances anti-tumor efficacy of human chimeric antigen receptor T cells. Sci Rep. 2017;7(1):737. doi: 10.1038/s41598-017-00462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gautron AS, Juillerat A, Guyot V, Filhol JM, Dessez E, Duclert A, et al. Fine and predictable tuning of TALEN gene editing targeting for improved T cell adoptive immunotherapy. Mol Ther Nucleic Acids. 2017;9:312–321. doi: 10.1016/j.omtn.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Rafiq S, Yeku OO, Jackson HJ, Purdon TJ, van Leeuwen DG, Drakes DJ, et al. Targeted delivery of a PD-1-blocking scFv by CAR-T cells enhances anti-tumor efficacy in vivo. Nat Biotechnol. 2018;36(9):847–856. doi: 10.1038/nbt.4195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Neelapu SS, Tummala S, Kebriaei P, Wierda W, Gutierrez C, Locke FL, et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat Rev Clin Oncol. 2018;15(1):47–62. doi: 10.1038/nrclinonc.2017.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Di Stasi A, Tey SK, Dotti G, Fujita Y, Kennedy-Nasser A, Martinez C, et al. Inducible apoptosis as a safety switch for adoptive cell therapy. N Engl J Med. 2011;365(18):1673–1683. doi: 10.1056/NEJMoa1106152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Sabatino M, Choi K, Chiruvolu V, Better M. Production of anti-CD19 CAR T cells for ZUMA-3 and -4: phase 1/2 multicenter studies evaluating KTE-C19 in patients with relapsed/refractory B-precursor acute lymphoblastic leukemia (R/R ALL) Blood. 2016;128(22):1227. [Google Scholar]
- 184.Velasquez MP, Bonifant CL, Gottschalk S. Redirecting T cells to hematological malignancies with bispecific antibodies. Blood. 2018;131(1):30–38. doi: 10.1182/blood-2017-06-741058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Wang H, Kaur G, Sankin AI, Chen F, Guan F, Zang X. Immune checkpoint blockade and CAR-T cell therapy in hematologic malignancies. J Hematol Oncol. 2019;12(1):59. doi: 10.1186/s13045-019-0746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Manson G, Mear JB, Herbaux C, Schiano JM, Casasnovas O, Stamatoullas A, et al. Long-term efficacy of anti-PD1 therapy in Hodgkin lymphoma with and without allogenic stem cell transplantation. Eur J Cancer. 2019;115:47–56. doi: 10.1016/j.ejca.2019.04.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable