Abstract
Angiosarcoma is a malignant endothelial cell tumor that involves a variety of anatomic sites with the skin being the most common. Cutaneous angiosarcoma is a diagnostic challenge as it can be confused with lesions such as rosacea, hemangiomas and hematomas. Since the tumor has a propensity for early metastasis and extensive intradermal spread, early diagnostic intervention via punch biopsy may prevent delays in diagnosis and improve tumor resectability and prognosis. We present a case of cutaneous angiosarcoma on the nose and cheeks of a 75-year-old male that resembled rosacea.
Keywords: Cutaneous angiosarcoma, rosacea, telangiectasia, punch biopsy, early diagnosis
Introduction
Angiosarcoma is a rare, malignant neoplasm that originates from vascular or lymphatic endothelial cells. It accounts for 1%–2% of soft tissue sarcomas and only 1% of head and neck cancers.1–3 Angiosarcoma most often involves the skin of the head and neck, with the scalp and face being the most commonly affected regions.1–3 A majority of patients diagnosed with cutaneous angiosarcoma of the head and neck are older Caucasian adults.3 In many cases, the etiology of angiosarcoma is unknown; however, some important risk factors include prior radiation exposure, chronic lymphedema (Stewart-Treves syndrome) and exposure to carcinogens such as arsenic and vinyl chloride.2
Cutaneous angiosarcoma presents insidiously as an erythematous, violaceous or bruise-like lesion; lesions can be nodular, macular, plaque-like or ulcerative.1,2 Early clinical detection is essential as angiosarcoma has a high rate of distant metastasis and is associated with a poor prognosis.1 However, the diagnosis is often delayed because lesions can be confused with rosacea, hemangiomas, hematomas, eczema or infection.2,4,5 Therefore, early clinical suspicion and biopsy of skin lesions that resemble angiosarcoma should be considered.
Case report
A 75-year-old male presented to the dermatology clinic with a 4-week history of a nonhealing and enlarging lesion on the nose. On physical examination, a 5-mm pearly papule distributed on the nasal supratip was detected. The nose and adjacent cheek areas were also noted to be erythematous with a purple hue and highly vascular with telangiectasias scattered throughout. The patient stated that he has a long history of previously diagnosed rosacea of his nose and cheeks. A shave biopsy was performed on the enlarging lesion which demonstrated a typical nodular basal cell carcinoma (BCC). The patient was subsequently scheduled for Mohs surgery.
The area was prepped with Hibiclens and local anesthesia was injected. The tumor was first debulked with a curette and subsequently excised as per Mohs protocol. The first stage was clear of any residual BCC but the lateral and deep margins demonstrated a dense population of poorly characterized spindle cells. After two more stages failed to yield clear margins, the surgeon decided to dress the wound and defer further excision until a definitive histological diagnosis was made. The specimens from the Mohs procedure were sent to offsite pathology for further characterization. Immunohistochemistry was positive for CD31, ERG and Ki-67. A diagnosis of angiosarcoma with spindle cell differentiation, high-grade cytology, anastomosing vascular spaces and solid growth was made.
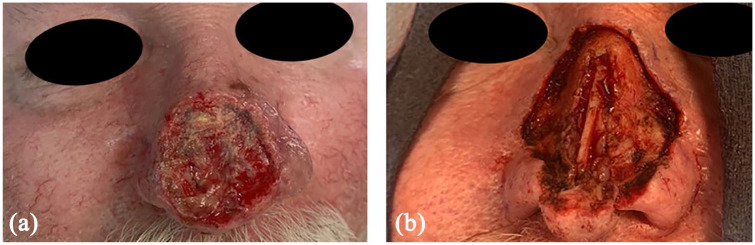
Following the pathology report, the patient was referred to plastic surgery for further resection and reconstruction. Initially, the surgeon excised the lesion with a margin of 5 mm and sent the specimen to surgical pathology for analysis. Margins were not clear of the tumor, and a 1-cm margin around the lesion was subsequently excised and sent to pathology (Figure 1). The tumor was noted to extend deeply into the nasal septum and the adjacent nasal cheek areas. Still unable to obtain clear margins despite wide resection, the plastic surgeon referred the patient to an oncologist for further workup and management. The oncologist determined that the best course of treatment was a combination of radiotherapy and chemotherapy. The patient agreed to the treatment plan, and we continue to follow up with the patient every month.
Figure 1.
Nose and cheeks following surgical resection with (a) 5 mm margins and (b) 1 cm margins. Note the red/purple discoloration of the nose and cheeks and the telangiectasias scattered throughout the same area. The tumor involved extensive portions of the nose/nasal septum and extended into the adjacent cheek areas bilaterally.
Discussion
Due to its variable clinical manifestations, propensity for early metastasis and overall rarity, cutaneous angiosarcoma of the head and neck is both a diagnostic challenge and a difficult disease to manage. The prognosis is poor, with the 5-year overall survival rate ranging from 10% to 35%.6,7 Studies have shown that only half of patients survive over 15–18 months.1,4 Prognostic factors include tumor size greater than 5 cm in diameter, depth of invasion, margin status, recurrence and metastases.1,2,3,7
Current treatment modalities include complete surgical resection, radiation therapy and chemotherapy.2,4,5 Chemo-therapy is recommended for metastatic disease, and chemotherapeutic agents that have shown activity against angiosarcoma include anthracyclines and taxanes.2,5 However, cutaneous angiosarcoma of the head and neck can present with multifocal lesions, indistinct borders and extensive skin involvement due to clinically undetectable intradermal spread.2,6 This makes it difficult or even impossible to attain negative margins during surgical resection and contributes to the high rates of local recurrence.1,2 A delay in the definitive diagnosis may play a role in the extensive skin involvement and metastasis seen in many patients. Therefore, early discovery could potentially enhance tumor resectability and improve the prognosis in patients with cutaneous angiosarcoma.
In this particular case, the prior existence of extensive rosacea may have led to a false attribution of the purplish/erythematous appearance of his nose to just a further manifestation of his rosacea. It is important to recognize that long-standing erythema with a purplish hue may in fact represent an underlying cutaneous angiosarcoma and not simply rosacea. Therefore, persistent findings of erythematous/violaceous patches or plaques (especially in patients who are fair-skinned) should raise the clinician’s index of suspicion for the possibility of the existence of malignant vascular tumors. As such, early diagnostic intervention via punch biopsy of the area could prevent delays in diagnosis. As established methods for screening of this difficult malignancy are lacking, the physician’s clinical intuition remains a key aspect in early diagnosis.
Acknowledgments
The authors would like to thank Dr Jaime Flores for providing the images in this case report.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for this case report; the patient provided consent for the publication of clinical information and body images/pictures including the face.
References
- 1. Hackman T, Mullins B. Angiosarcoma of the head and neck. Int Arch Otorhi 2015; 19(3): 191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Patel SH, Hayden RE, Hinni ML, et al. Angiosarcoma of the scalp and face: the Mayo clinic experience. JAMA Otolaryngol Head Neck Surg 2015; 141(4): 335–340. [DOI] [PubMed] [Google Scholar]
- 3. Albores-Saavedra J, Schwartz AM, Henson DE, et al. Cutaneous angiosarcoma. Analysis of 434 cases from the surveillance, epidemiology, and end results program, 1973-2007. Ann Diagn Pathol 2011; 15(2): 93–97. [DOI] [PubMed] [Google Scholar]
- 4. Vora R, Anjaneyan G, Gupta R. Cutaneous angiosarcoma of head and neck. Indian J Dermatol 2014; 59(6): 632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bhatti Z, Bhatti R, Brangman S, et al. Extensive cutaneous scalp angiosarcoma. Case Rep Dermatol Med 2018; 2018: 8409820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morrison WH, Byers RM, Garden AS, et al. Cutaneous angiosarcoma of the head and neck: a therapeutic dilemma. Cancer 1995; 76(2): 319–327. [DOI] [PubMed] [Google Scholar]
- 7. Morgan MB, Swann M, Somach S, et al. Cutaneous angiosarcoma: a case series with prognostic correlation. J Am Acad Dermatol 2004; 50(6): 867–874. [DOI] [PubMed] [Google Scholar]