Abstract
Background:
Symptomatic genu recurvatum is a challenging condition to treat. Both osseous and soft tissue treatment options have been reported to address symptomatic genu recurvatum.
Purpose/Hypothesis:
The purpose of this article was to review the current literature on surgical treatment options for symptomatic genu recurvatum and to describe the associated clinical outcomes. We hypothesized that anterior opening-wedge proximal tibial osteotomy (PTO) would be the most common surgical technique described in the literature and that this intervention would allow for successful long-term management of symptomatic genu recurvatum.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, with the inclusion criterion of surgical treatment options for symptomatic genu recurvatum. Recurvatum secondary to polio, cerebrovascular accident, or cerebral palsy was excluded from this review.
Results:
A total of 311 studies were identified, of which 6 studies with a total of 80 patients met the inclusion criteria. Causes of genu recurvatum included physeal arrest; soft tissue laxity; and complications related to fractures, such as prolonged immobilization and malalignment. Mean follow-up times ranged from 1 to 14.5 years postoperatively. There were 5 studies that described anterior opening-wedge PTO, 2 of which used the Ilizarov distraction technique. All 3 studies that used PTO without the Ilizarov technique reported correction of recurvatum and increased posterior tibial slope; 2 of these studies also included subjective outcomes scores, reporting good or excellent outcomes in 70% (21/30) of patients. Of the studies that used the Ilizarov technique, both reported correction of recurvatum and increased posterior slope from preoperative to postoperative assessments. Both of these studies reported good or excellent subjective outcomes postoperatively in 89.5% (17/19) of patients. Additionally, 1 study successfully corrected recurvatum by performing a retensioning of the posterior capsule to address knee hyperextension, although follow-up was limited to 1 year postoperatively.
Conclusion:
Anterior opening-wedge PTO, with or without postoperative external fixation with progressive distraction, was found to be a reliable surgical treatment for symptomatic genu recurvatum. After surgical management with PTO, patients can expect to achieve correction of knee hyperextension, restoration of a more posterior tibial slope, and increased subjective outcome scores.
Keywords: genu recurvatum, proximal tibial osteotomy, complex knee, tibial slope, heel height
Symptomatic genu recurvatum, which has been defined as symptomatic hyperextension of the knee beyond 5°, is a challenging condition to treat.22 The most common symptoms associated with this condition include pain, weakness, instability, leg-length discrepancy, and decreased range of motion.7,25 Genu recurvatum can be congenital33 or acquired secondary to trauma,14 cerebrovascular accident, polio,23 physeal arrest,6 Osgood-Schlatter disease,25 or prolonged casting.5
Dejour et al11 described 3 primary types of genu recurvatum: (1) pure osseous deformity, in many cases due to damage to the tibial tubercle growth plate; (2) chronic hyperextension secondary to soft tissue laxity either from trauma or gradual tissue stretching; and (3) a mixed-type deformity resulting from a combination of osseous and soft tissue abnormalities. The source of symptomatic genu recurvatum can also be idiopathic.25
Given the distinct pathological origins of the condition, treatment of symptomatic genu recurvatum can be grouped into 3 major categories: osseous surgical management, often entailing osteotomy of the tibia; soft tissue surgical management, aimed at tensioning the posterior soft tissues; and nonoperative management, which focuses on strengthening the supporting musculature, bracing the knee, or correcting gait patterns.11 The purpose of this study was to review the current literature on surgical treatment options for symptomatic genu recurvatum and to describe the associated clinical outcomes. We hypothesized that anterior opening-wedge proximal tibial osteotomy (PTO) would be the most common surgical technique described in the literature and that this intervention would allow for successful long-term management of symptomatic genu recurvatum.
Methods
Article Identification and Selection
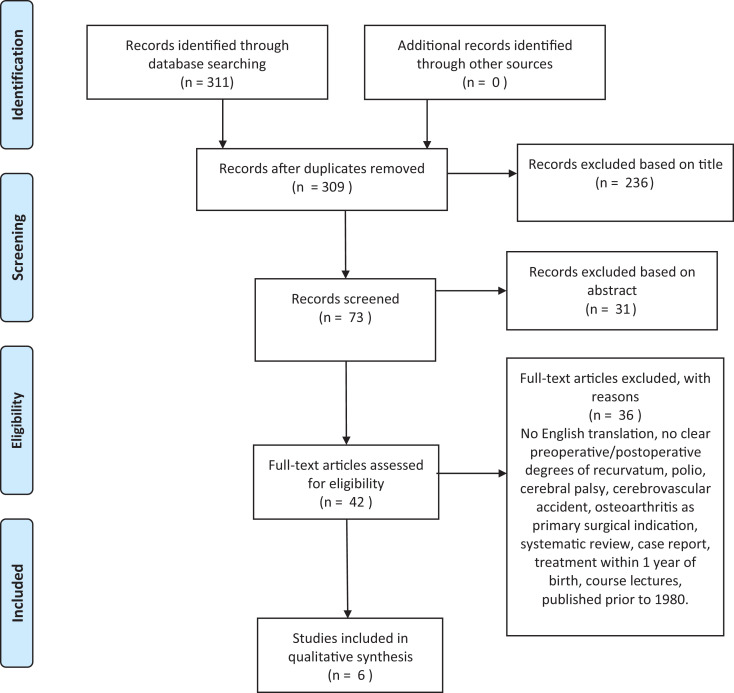
A systematic review of articles was completed through use of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines on the surgical treatment options for symptomatic genu recurvatum using PubMed (1980-2019); the query was performed in July 2019 (Figure 1).32 Registration of this systematic review was performed in August 2019 via the PROSPERO international prospective register of systematic reviews (ID No. 145707). The search terms used were “Genu recurvatum” AND “Treatment” OR “Management” OR “Outcomes” OR “Surgery” OR “Operation.”
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart describing application of selection criteria to the studies identified using the search strategy.
The inclusion criteria consisted of English-language studies on the treatment of symptomatic genu recurvatum. Genu recurvatum was defined as a pathologic hyperextension of the knee joint beyond 5°. Exclusion criteria were recurvatum secondary to polio, cerebrovascular accident or cerebral palsy, studies published before 1980, diagnosis of genu recurvatum after previous knee surgery, surgery-induced recurvatum, treatment of skeletally immature patients, systematic reviews, course lectures, case reports (level 5 evidence), and studies that failed to state the degree of recurvatum before or after treatment. Additionally, studies that considered patients with combined anterior/posterior cruciate ligament and posterolateral knee insufficiency were not included in the current review because ligament reconstruction is the well-established gold standard for surgical management of this cause of genu recurvatum. Two investigators (R.S.D., N.R.G.) independently reviewed the abstracts from all identified articles. If necessary, full-text articles were obtained for review to allow further application of the established inclusion and exclusion criteria. Additionally, reference lists from the included studies were reviewed and reconciled to verify that all eligible articles were considered. Studies were grouped by specific surgical technique for subanalysis.
Data Collection
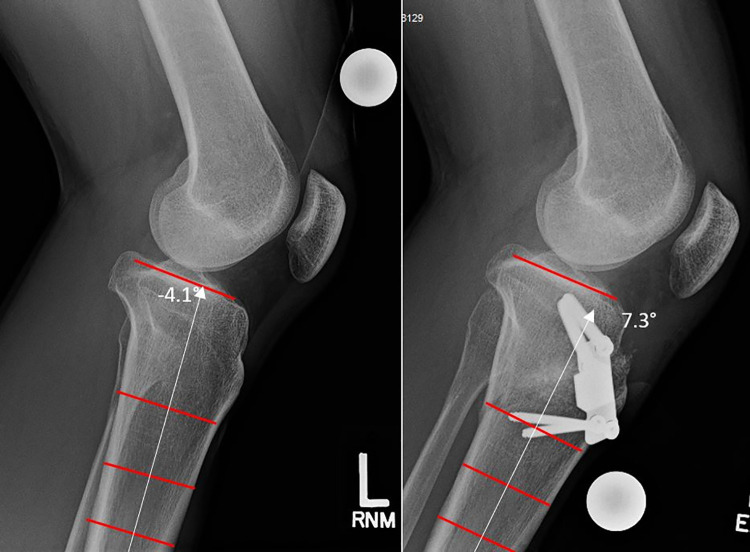
The variables of interest that were extracted from each study included the degree of posterior tibial slope identified on plain radiographs; the change in posterior tibial slope after intervention (Figure 2); preoperative and postoperative knee range of motion (ROM); and postoperative outcome scores, including the outcome scoring system described by Lecuire et al20 (Table 1). This scoring system provides a numerical value (0-200) and corresponding categorical assessment (poor, <80; fair, 80-125; good, 130-170; excellent, 175-200) through a combination of anatomic measurements (degree of recurvatum, tibial slope, and patellar height) and subjective functional results (pain, instability, ROM, weakness, sports activity, and self-evaluation). Extracted from all studies were patient demographics, surgical technique, and preoperative and postoperative measurements of recurvatum measured in degrees beyond neutral. For continuous variables (eg, age, outcome scores), the mean and standard deviation were obtained when available.
Figure 2.
Example of lateral radiographic images demonstrating the correction of symptomatic genu recurvatum using an anterior opening-wedge proximal tibial osteotomy from our practice. The posterior tibial slope (PTS) was corrected to a more posterior position; the tibial slope of the preoperative image (left) was –4.1° (tibial slope in the anterior direction), and the PTS after correction (right) was 7.3°.
Table 1.
Outcome Scoring System According to Lecuire et al20
| Results | Points |
|---|---|
| Anatomic (radiographic) results | |
| Angle of recurvatum | |
| 0°-3° | 40 |
| 4°-6° | 30 |
| 7°-9° | 20 |
| 10°-12° | 10 |
| >12° | 0 |
| Tibial slope | |
| 2° to 10° | 30 |
| –2° to 1° or 11° to 14° | 20 |
| –6° to –3° or 15° to 18° | 10 |
| ≤−6° or >18° | 0 |
| Patellar height (A:B ratio)a | |
| 0.66-0.94 | 30 |
| 0.51-0.65 or 0.95-1.09 | 20 |
| 0.36-0.50 or 1.10-1.24 | 10 |
| <0.36 or >1.24 | 0 |
| Total anatomic (radiographic) score | |
| Excellent | 90-100 |
| Good | 70-80 |
| Fair | 40-60 |
| Poor | <40 |
| Functional results | |
| Pain | |
| None | 20 |
| Slight | 10 |
| Mild | 5 |
| Severe | 0 |
| Instability | |
| None | 15 |
| Mild or slight | 5 |
| Severe | 0 |
| Range of motion | |
| Full | 20 |
| Decreased 1°-20° | 10 |
| Decreased >20° | 0 |
| Weakness | |
| None | 15 |
| Slight | 10 |
| Mild | 5 |
| Severe | 0 |
| Sports activity | |
| Yes | 10 |
| No | 0 |
| Patient evaluation of the result | |
| Excellent | 20 |
| Good | 10 |
| Fair | 5 |
| Poor | 0 |
| Total functional score | |
| Excellent | 85-100 |
| Good | 60-80 |
| Fair | 40-55 |
| Poor | <40 |
| Total combined score | |
| Excellent | 175-200 |
| Good | 130-170 |
| Fair | 80-125 |
| Poor | <80 |
aA:B ratio is the Blackburne and Peel patellar height ratio.
Results
The literature search identified 311 studies, of which 6 were included in the final analysis (Table 2). In total, the studies included for analysis entailed 80 patients. Among studies included for analysis, the reported causes of symptomatic genu recurvatum included prolonged immobilization, physeal arrest related to fracture, physeal arrest of unknown origin, soft tissue laxity, malalignment secondary to fracture treated nonoperatively, and idiopathic osseous deformity. Our search identified 5 studies that evaluated patients who underwent an anterior opening-wedge PTO to correct their deformity2,7,17,25,33; of these, 2 studies used the Ilizarov method, which implements postoperative progressive distraction to increase tibial slope via an external fixator.2,7 Additionally, 1 study evaluated patients who underwent retensioning of the posterior soft tissues via advancement and rotation of 2 bone blocks containing the femoral origin of the posterior capsule.29
Table 2.
Study Characteristics and Measuresa
| Lead Author (Year) | No. of Patients | Mean Follow-up, y | Procedure | Preoperative Recurvatumb | Postoperative Recurvatumb | Decrease in Recurvatum | Preoperative Tibial Slopeb,c | Postoperative Tibial Slope | Increase in Tibial Slope |
|---|---|---|---|---|---|---|---|---|---|
| Moroni25 (1992) | 25 (18 M, 7 F)d | 14.5 | PTO (mix of distal and proximal to tibial tubercle) | 28.9 ± 4.6 | 5.9 ± 4.6 | –23.0 | –15.0 ± 10.5 | 9.0 ± 8.3 | 24.0 |
| Choi7 (1999) | 10 (4 M, 6 F) | 4.4 | Ilizarov | 19.6 ± 3.1 | 3 ± 2.2 | –16.6 | –13.4 ± 7.2 | 5 ± 3.0 | 18.4 |
| Piriou29 (2002) | 11 | 1 | Bone-block reinsertion | 32.3 ± 7.2 | 3.6 ± 4.5 | –28.6 | NR | NR | NR |
| van Raaij33 (2006) | 20 (3 M, 17 F) | 7.4 | PTO (anterior, proximal to tibial tubercle) | ≥15 | 0 | NR | 11.7 ± 3.5 | 21.1 ± 5.7 | 9.4 ± 5.1 |
| Babu2 (2012) | 9 (6 M, 3 F) | 4.4 | Ilizarov | 28 ± 6.3 | 7.1 ± 4.4 | –20.9 | –21.4 ± 4.6 | 3.1 ± 2.5 | 24.5 |
| Kim17 (2017) | 5 (3 M, 2 F) | 3.9 | PTO (anterior oblique distal to tibial tubercle) | 17 ± 4.2 | 0.4 ± 3.3 | –16.6 | –10.2 ± 6.6 | 8.4 ± 2.4 | 18.6 |
aRecurvatum and tibial slope are expressed in degrees as mean or mean ± SD. F, female; M, male; NR, not reported; PTO, proximal tibial osteotomy.
bMeasurements were taken on plain film radiograph.
cNegative values indicate anterior tilted tibial slope.
dStudy reported on 27 knees from 25 patients.
All but 1 study reported the mean preoperative degree of recurvatum. Each of the other studies reportedly measured the degree of preoperative and postoperative recurvatum on either standing or supine lateral radiographs.2,7,17,25,29 None of the included studies reported the amount of knee hyperextension on clinical examination as a measure of genu recurvatum. Among studies that reported the mean preoperative genu recurvatum, the mean degree of hyperextension on radiographs ranged from 17° to 32°.2,7,17,25,29
Proximal Tibial Osteotomy
Among the 5 studies that used a PTO for treatment of genu recurvatum, correction demonstrated a reduction in hyperextension, with mean knee hyperextension ranging from 0° to 7° postoperatively.2,7,17,25,33 Posterior tibial slope was reported to increase (ie, become more posterior) postoperatively among all studies that used an anterior opening-wedge PTO for treatment, with a range of 9.4° to 24.5° increase in tibial slope.2,7,17,25,33 Further, 4 of the 5 osteotomy studies reported that anterior tibial slope was present preoperatively, which was corrected to a posterior tibial slope postoperatively (Table 2).2,7,17,25
A total of 3 studies performed an isolated opening-wedge PTO technique.17,25,33 All 3 studies reported a correction of symptomatic genu recurvatum and an increased amount of posterior tibial slope postoperatively (Table 2).17,25,33 We noted that 2 of these studies reported the Lecuire subjective outcome scores. In the study by Kim et al,17 all 5 patients demonstrated good or excellent postoperative outcomes, whereas Moroni et al25 reported that 18 of 27 knees in 25 patients demonstrated good or excellent postoperative outcomes.
We found that 2 studies performed a PTO with postoperative progressive distraction using the Ilizarov method to treat genu recurvatum.2,7 Both studies reported a correction of recurvatum and an increased posterior tibial slope among all patients (Table 2).2,7 Lecuire subjective outcome scores were reported in both studies: 9 of 10 patients reported by Choi et al7 and 8 of 9 patients reported by Babu et al2 demonstrated good or excellent postoperative outcomes (Table 3).
Table 3.
Subjective Clinical Outcomes Scores Described by Lecuire et al20 a
| Outcome Score, n (%)b | ||||||
|---|---|---|---|---|---|---|
| Study | Mean Follow-up, y | No. of Patients | Excellent (175-200) | Good (130-170) | Fair (80-125) | Poor (<80) |
| Choi7 (1999) | 4.4 | 10 (4 M, 6 F) | 3 (30.0) | 6 (60.0) | 1 (10.0) | 0 (0.0) |
| Babu2 (2012) | 4.4 | 9 (6 M, 3 F) | 5 (55.6) | 3 (33.3) | 1 (11.1) | 0 (0.0) |
| Kim17 (2017) | 3.9 | 5 (3 M, 2 F) | 3 (60.0) | 2 (40.0) | 0 (0.0) | 0 (0.0) |
| Moroni25 (1992) | 14.5 | 25 (18 M, 7 F)c | 10 (37.0) | 8 (29.6) | 8 (29.6) | 1 (3.7) |
aF, female; M, male.
bNumber and percentage of patients within each study with subjective outcomes in the respective category.
cStudy reported on 27 knees from 25 patients.
Posterior Soft Tissue Tensioning
Only 1 study reported clinical outcomes with soft tissue retensioning of the posterior capsule for the treatment of genu recurvatum. The study included 11 patients, with a mean 32° ± 6.9° of hyperextension preoperatively. The investigators reported a mean 3.6° ± 4.5° of hyperextension postoperatively, with no significant loss of correction at 1 year postoperatively29 (Table 2).
Complications
Patients who underwent PTO had the following reported complications: infection at the operative site (n = 2; 2.9%),2,7 transient neuropathy (n = 2; 2.9%),2,7 patella infera (n = 1; 1.4%),7 pain over the lateral thigh (n = 2; 2.9%),33 anterior cruciate ligament (ACL) rupture 2 years postoperatively (n = 1; 1.4%),33 and a 7° loss of correction at an unspecified time postoperatively (n = 1; 1.4%).33 Moroni et al25 reported a 13-fold increased relative risk for a fair or poor subjective outcome score in patients without a purely osseous origin of genu recurvatum relative to patients with a purely osseous deformities. Further, it was reported that patients who had a PTO distal to the tibial tubercle had a relative risk of a fair or poor outcome 36 times that of patients with PTOs proximal to the tibial tubercle.25
Discussion
The most important findings of this systematic review were that clinical evidence supports surgical management of symptomatic genu recurvatum by increasing tibial slope through use of an anterior opening-wedge PTO. Overall, patients demonstrated a reduction in the degree of knee hyperextension, a more posterior tibial slope, and good or excellent subjective postoperative outcome scores. However, this systematic review revealed a relative paucity of objective reporting on the surgical treatment of genu recurvatum. Additionally, studies were inconsistent in reporting their specific technique for measurement of hyperextension. Future research investigating the treatment of symptomatic genu recurvatum would benefit from using and documenting a more objective, reliable measurement of knee hyperextension.
We found that 5 of the included studies determined the degree of preoperative and postoperative hyperextension using measurement techniques on either standing or supine lateral radiographs.2,7,17,25,29 A more objective way that clinicians can identify and measure genu recurvatum, both preoperatively and postoperatively, is by evaluating side-to-side differences in heel height.8 Previous clinical studies have reported that 1 cm of increased heel height corresponds to 1.06° of knee extension.30 The heel-height test has demonstrated a high correlation with the traditional use of a goniometer and is more reliable in determining subtle side-to-side differences.19,31 Given its efficiency and reliability, measurement of heel height is a more clinically relevant and objective technique than is evaluation with a goniometer for assessment of surgical correction intraoperatively and at postoperative follow-up.
In the current systematic review, 5 studies performed a PTO for the correction of symptomatic genu recurvatum; 3 studies performed PTO as a 1-step procedure, whereas the other 2 studies additionally used postoperative progressive distraction via the Ilizarov technique.2,7,17,25,33 Each of these studies reported a reduction in the degree of knee hyperextension and an increased amount of tibial slope postoperatively. Of note, all but 133 of the studies that reported tibial slope found that patients with symptomatic genu recurvatum had an anterior tibial slope before the osteotomy surgery. It was theorized that correcting the anterior tibial slope to a more anatomic, posterior orientation allowed the ligaments to return to their normal tension and restored the native knee biomechanics.1,4,13 Variations in tibial slope have previously been correlated with the degree of knee hyperextension; specifically, a greater degree of posterior tibial slope correlates with a lesser degree of knee hyperextension.35
We noted that 1 study included in the current review reported a mean preoperative slope of 11.7° for patients with genu recurvatum, which is closer to the reported mean posterior tibial slope of the healthy individuals. After PTO in this study, the patients’ tibial slope was increased to a mean of 21.1° postoperatively.33 Although this study reported improved subjective outcome scores according to the Hospital for Special Surgery scoring system (mean, 90.3 ± 9.0) and a high rate (83%) of patient satisfaction, such a significant degree of postoperative tibial slope may increase the risk of ACL instability at later follow-up.3 This same study reported only 1 case of a postoperative ACL tear; however, such a large increase in posterior tibial slope compared with normal ranges increases the risk of future ACL tears and must be considered when surgically correcting genu recurvatum using a tibial osteotomy.3,12,34
The reviewed studies that entailed osteotomies reported similar degrees of preoperative genu recurvatum in patients treated using either PTO alone or the Ilizarov method. Both corrective techniques also demonstrated similar subjective postoperative outcomes.2,7,17,25,33 The literature has reported that postoperative proximal tibial distraction techniques are typically used to correct severe genu recurvatum that is beyond the corrective scope of a single-stage PTO alone.21 However, the reviewed studies indicated that this may not be necessary, as PTO with or without proximal tibial distraction demonstrated similar degrees of correction.
Most studies included in the current review identified anterior (decreased) tibial slope as the predominant cause of genu recurvatum. In a biomechanical study, Morgan et al24 reported that knees with decreased tibial slope had an increased amount of hyperextension after ligament injuries of the knee. Thus, it is logical that increasing tibial slope using a PTO was the most common surgical treatment of the chronic injuries because most patients had an anteriorly tilted (decreased) tibial slope in this systematic review.
Although only 1 soft tissue correction study met the current inclusion criteria, several soft tissue operations have previously been described for genu recurvatum secondary to capsuloligamentous insufficiency that were not included in this systematic review. Older studies have suggested surgically inserting a restrictive soft tissue graft at the posterior aspect of the knee to prevent hyperextension.15,16,28 Noyes and Barber-Westin26,27 addressed knee hyperextension in the setting of chronic multiligament knee instability through plication or advancement of the posterolateral capsule. These studies were each limited by a lack of patient outcomes and follow-up data related to the sustained correction. Included in the current review, Piriou et al29 reported a reduction in recurvatum (from 32° to 3.6°) that was maintained at 1-year follow-up using their capsular bone-block reinsertion technique. However, the short-term follow-up reported in this study warrants observation beyond 1 year because soft tissue corrections may stretch over time and cause a patient’s knee to revert back to hyperextension. To date, an anatomic-based surgical reconstruction to treat genu recurvatum has not been proposed in the biomechanical or clinical literature. Furthermore, genu recurvatum secondary to soft tissue laxity is often chronic in nature,22,27 and the literature consistently reports that treatment of chronic ligamentous laxity demonstrates inferior outcomes compared with treatment in the acute setting.9,10,18 A previous biomechanical study showed that the oblique popliteal ligament’s midtibial attachment is the most significant restraint to knee hyperextension.24 As such, it is essential to identify and treat ligamentous causes of symptomatic knee hyperextension in the acute setting when possible.
We acknowledge that this systematic review has some limitations. First, despite composing a significant proportion of the cases of genu recurvatum, patients who developed genu recurvatum secondary to stroke, polio, or cerebral palsy were not included in the analysis because they often require individualized, multifactorial, and often complex treatment strategies that are not generalizable to the field of orthopaedic sports medicine. Additionally, the specific method of measurement for the degree of recurvatum was not uniformly detailed in each study. Because all studies that met inclusion criteria were level 4 evidence, we were unable to conduct a risk of bias analysis. Finally, there was a paucity of long-term clinical outcome measures after treatment of genu recurvatum; as such, only the degrees of recurvatum and tibial slope were included as objective outcome measures. Future research should examine treatment options with additional validated, subjective and objective, long-term outcome data to help properly develop a treatment protocol.
Conclusion
Anterior opening-wedge PTO, with or without postoperative external fixation with progressive distraction, was found to be a reliable surgical treatment for genu recurvatum. After surgical management using a PTO, patients can expect to achieve correction of knee hyperextension, restoration of a more posterior tibial slope, and increased subjective outcome scores.
Footnotes
Final revision submitted March 13, 2020; accepted March 25, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.F.L. has received grant support from Arthrex, Linvatec, Ossur, and Smith & Nephew; educational support from Arthrex; consulting fees from Arthrex and Smith & Nephew; and royalties from Arthrex and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abdelrahman T, Getgood A. Role of osteotomy in multiligament knee injuries. Ann Joints. 2019;4:8–8. [Google Scholar]
- 2. Babu M, Fassier F, Rendon JS, Saran N, Hamdy RC. Correction of proximal tibial recurvatum using the Ilizarov technique. J Pediatr Orthop. 2012;32(1):35–41. [DOI] [PubMed] [Google Scholar]
- 3. Bernhardson AS, Aman ZS, Dornan GJ, et al. Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47(2):296–302. [DOI] [PubMed] [Google Scholar]
- 4. Bilsel K, Erdil M, Elmadag M, Sen C. Realignment osteotomies in the treatment of chronic instabilities of the knee associated with malalignment (case report). Int J Surg Case Rep. 2012;3(7):231–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bowen JR. Treatment of genu recurvatum by proximal tibial closing-wedge/anterior displacement osteotomy. J Pediatr Orthop. 1984;4(2):266. [PubMed] [Google Scholar]
- 6. Chen LC, Chan YS, Wang CJ. Opening-wedge osteotomy, allografting with dual buttress plate fixation for severe genu recurvatum caused by partial growth arrest of the proximal tibial physis: a case report. J Orthop Trauma. 2004;18(6):384–387. [DOI] [PubMed] [Google Scholar]
- 7. Choi IH, Chung CY, Cho TJ, et al. Correction of genu recurvatum deformity by Ilizarov method. J Bone Joint Surg Br. 1999;81(5):769–774. [DOI] [PubMed] [Google Scholar]
- 8. Cinque ME, Geeslin AG, Chahla J, et al. The heel height test: a novel tool for the detection of combined anterior cruciate ligament and fibular collateral ligament tears. Arthroscopy. 2017;33(12):2177–2181. [DOI] [PubMed] [Google Scholar]
- 9. Clancy WG, Sutherland TB. Combined posterior cruciate ligament injuries. Clin Sports Med. 1994;13(3):629–647. [PubMed] [Google Scholar]
- 10. Covey DC. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83(1):106–118. [DOI] [PubMed] [Google Scholar]
- 11. Dejour D, Bonin N, Locatelli E. Tibial antirecurvatum osteotomies. Oper Tech Sports Med. 2000;8(1):67–70. [Google Scholar]
- 12. Dejour D, Kuhn A, Dejour H. Osteotomie tibiale de déflexion et laxité chronique antérieure à propos de 22 cas. Rev Chir Orthop. 1998;84(suppl II)(28):28–29. [Google Scholar]
- 13. Fening SD, Miniaci A, Kovacic J, Kambic H, McLean S, Scott J. The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: a human cadaveric study. J Knee Surg. 2008;21(3):205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gaskill TR, Pierce CM, James EW, LaPrade RF. Anterolateral proximal tibial opening wedge osteotomy to treat symptomatic genu recurvatum with valgus alignment: a case report. JBJS Case Connect. 2014;4(3):e71–e75. [DOI] [PubMed] [Google Scholar]
- 15. Gill A. Operation for correction of paralytic genu recurvatum. J Bone Joint Surg. 1931;13(1):49. [Google Scholar]
- 16. Heyman CH. Operative treatment of paralytic genu recurvatum. J Bone Joint Surg Am. 1947;29(3):644–649. [PubMed] [Google Scholar]
- 17. Kim TW, Lee S, Yoon JR, Han HS, Lee MC. Proximal tibial anterior open-wedge oblique osteotomy: a novel technique to correct genu recurvatum. Knee. 2017;24(2):345–353. [DOI] [PubMed] [Google Scholar]
- 18. LaPrade R, Konowalchuk B, Wentorf F. Posterolateral corner injuries. Orthop Knowl Online. 2003;1(5):53–71. [Google Scholar]
- 19. Laurà G, Berruto M, Bianchi M. Genu recurvatum following distal epiphysiodesis of the femur: X-ray evaluation and therapeutical approach. Ital J Orthop Traumatol. 1992;18(4):505–514. [PubMed] [Google Scholar]
- 20. Lecuire F, Lerat JL, Bousquet G, Dejour H, Trillat A. The treatment of genu recurvatum. Rev Chir Orthop Reparatrice Appar Mot. 1980;66(2):95–103. [PubMed] [Google Scholar]
- 21. Lee DC, Byun SJ. High tibial osteotomy. Knee Surg Relat Res. 2012;24:61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loudon J, Goist H, Loudon K. Genu recurvatum syndrome. J Orthop Sport Phys Ther. 1998;27:361–367. [DOI] [PubMed] [Google Scholar]
- 23. Mehta S, Mukherjee A. Flexion osteotomy of the femur for genu recurvatum after poliomyelitis. J Bone Joint Surg Br. 1991;73(2):200–202. [DOI] [PubMed] [Google Scholar]
- 24. Morgan PM, LaPrade RF, Wentorf FA, Cook JW, Bianco A. The role of the oblique popliteal ligament and other structures in preventing knee hyperextension. Am J Sports Med. 2010;38(3):550–557. [DOI] [PubMed] [Google Scholar]
- 25. Moroni A, Pezzuto V, Pompili M, Zinghi G. Proximal osteotomy of the tibia for the treatment of genu recurvatum in adults. J Bone Joint Surg Am. 1992;74:577–586. [PubMed] [Google Scholar]
- 26. Noyes F, Barber-Westin S. Long-term assessment of posterolateral ligament femoral-fibular reconstruction in chronic multiligament unstable knees. Am J Sports Med. 2011;39(3):497–505. [DOI] [PubMed] [Google Scholar]
- 27. Noyes F, Barber-Westin S. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med. 1996;24(4):415–426. [DOI] [PubMed] [Google Scholar]
- 28. Perry J, O’Brien JP, Hodgson AR. Triple tenodesis of the knee: a soft tissue operation for the correction of paralytic genu recurvatum. J Bone Joint Surg Am. 1976;58(7):978–985. [PubMed] [Google Scholar]
- 29. Piriou P, Garreau C, Combelles F, Judet T. Original technique for the treatment of ligament-related genu recurvatum: preliminary results. Knee Surg Sports Traumatol Arthrosc. 2002;10(4):260–264. [DOI] [PubMed] [Google Scholar]
- 30. Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17(6):760–765. [DOI] [PubMed] [Google Scholar]
- 31. Schlegel TF, Boublik M, Hawkins RJ, Steadman JR. Reliability of heel-height measurement for documenting knee extension deficits. Am J Sports Med. 2002;30(4):479–482. [DOI] [PubMed] [Google Scholar]
- 32. Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- 33. van Raaij TM, De Waal Malefijt J. Anterior opening wedge osteotomy of the proximal tibia for anterior knee pain in idiopathic hyperextension knees. Int Orthop. 2006;30(4):248–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 35. Yamaguchi KT, Cheung EC, Markolf KL, et al. Effects of anterior closing wedge tibial osteotomy on anterior cruciate ligament force and knee kinematics. Am J Sports Med. 2018;46(2):370–377. [DOI] [PubMed] [Google Scholar]