Abstract
Following the emergence of the coronavirus disease 19 (COVID-19) pandemic, healthcare organizations began concentrating on the preparation for and management of the surge of COVID-19 cases while trying to protect the healthcare workers and other patients from getting COVID-19. Changing the way people work requires innovative approaches and questioning some long-held medical practices. There are multiple factors contributing to the apparent reduced utilization of healthcare services to non–COVID-19 patients. The current world crisis is highlighting the need of re-engineering the way we deliver inpatient and outpatient health care, including bolstering social support, in order to be prepared when the next calamity will present itself.
Following the emergence of the coronavirus disease 19 (COVID-19) pandemic, healthcare organizations began concentrating on the preparation for and management of the surge of COVID-19 cases while trying to protect the healthcare workers and other patients from getting COVID-19 (Rosenbaum, 2020; Al-Tawfiq et al., 2020a). This latter task is critically important as patients are the most vulnerable victims of COVID-19 because they are usually older adults, with chronic medical conditions, frequently multiple, or immunocompromised. The rapid adoption of alternative ways to deal with those patients was unprecedented across the globe. The actions implemented by the different healthcare organizations fell into one or another of the categories of controls illustrated in the hierarchy of controls, popularized by the United States Centers for Disease Control and Prevention (CDC) (CDC, n.d.). The most immediate intervention was the mandatory use of personal protective equipment (PPE) of different nature when dealing with confirmed or suspected cases of COVID-19.
The risk of aerosolization and thus the risk of dissemination of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seem higher in certain surgical and aerosol-generating procedures (Vukkadala et al., 2020; Workman et al., 2020). For those procedures, appropriate PPE including N-95 or PAPR use is needed during these procedures, aerosol-. In addition to these measures, alternative nonsurgical management strategies, should be sought (Fastenberg et al., 2020).
Changing the way people work requires innovative approaches and questioning some long-held medical practices. Medical therapy such as in the case of acute coronary syndrome catheterization is presently undergoing re-evaluation, where nonsurgical interventions such as the use of thrombolysis therapies are being considered in place of catheterization (Welt et al., 2020). In one study of urologic services, 19 of 53 (35.8%) consultations were performed via telemedicine (Borchert et al., 2020). Adopting virtual visits through telephone calls and video calls is another avenue of great potential. This is particularly helpful for patients who do not require invasive procedure and do not require in-hospital care. These visits will allow the healthcare worker to assess the patient’s progress and response to therapy, and to adjust or refill medications. Clearly, each country’s laws and regulation need to be supporting the legality of virtual visits. In combination with virtual visits, home delivery or delivery at satellite pharmacy locations is becoming more popular. Our own organization has implemented in selected cases both virtual visits and home delivery of medications.
The next category of intervention consists of isolating people from the hazard. Many healthcare organizations, including ours, decided to defer certain procedures and elective cases in order to lower the risk of transmission (Welt et al., 2020). Various factors are used for classifications to prioritize non–COVID-19 patients depending on the acuity of the disease, risk of intensifying chronic disease symptoms without intervention, risk of exposure to COVID-19 in relation to geography, and availability of technology with video capabilities. One such classification of patients was based on the urgency of the condition, creating the following 4 categories: care needed in 0–6 h, 6–48 h, 48 h to 14 days, and >14 days (Fastenberg et al., 2020). That organization functioned on the presumption that all patients and staff could be positive asymptomatic cases requiring social distancing of staff and residents during case discussions, rounds, and classes, in addition to the use of PPE and universal masking (Fastenberg et al., 2020; Tirupathi et al., 2020).
The concern about possible transmission of COVID-19 in the hospital setting has also moved the practice from more invasive to more conservative procedures. Evidence-based medicine articles looked at various medications, such as aspirin, B-blocks, angiotensin-converting enzyme inhibitors, and statin therapy that could reduce non–COVID-19 hospital admission (Bobrovitz et al., 2020). Hospitals developed internal policies limiting sitters and companion in the units and ensuring compliance with universal masking for both healthcare worker as well as the patients, social distancing, hand hygiene, and cough etiquette.
Hospitals began screening each visitor (patients and staff) for history of COVID-19 symptoms, and checking the temperature was adopted, directing those identified as possible COVID-19 patients to the appropriate testing facilities and disposition (Johns Hopkins Aramco Healthcare, n.d.). Furthermore, in order to properly care for non–COVID-19 patients, it had been suggested that there should be separate hospitals for those with COVID-19 and those without COVID-19 (Welt et al., 2020), introducing the concept of segregation at the level of the hospital rather than the level of a unit or ward in a specific hospital.
To be prepared for a potential surge in the need for intensive care beds for COVID-19 patients, major logistical efforts become necessary. Logistics and preparedness of healthcare organization to accommodate non–COVID-19 patients such as the availability of ICU beds for both non-COVID and COVID-19 patients rely on other community activities for the control of COVID-19, such as self-isolation, quarantine facilities, and curfew. In one study, the need for ICU beds was estimated to be 569 ICU bed days per 10,000 population in case of no self-isolation of infected patients (Moghadas et al., 2020). This number is reduced by 23.5% and 53.6% assuming that 20% and 40% of cases practiced self-isolation, respectively (Moghadas et al., 2020). The true need of hospital, and in particular ICU, beds actually seems dependent on several factors. A very important (and controllable) factor is the policy regarding management of confirmed positive asymptomatic cases. The option, sanctioned by the local government, to (successfully) quarantine such patients at home or in designated quarantine facilities would dramatically “decompress” healthcare organizations that would then focus on symptomatic patients only. Another important (but noncontrollable) factor determining the need of hospital beds is the average age of the population. As it became apparent in Europe, nations with a high percentage of elderly individuals cared for in nursing and retirement homes have experienced an overwhelming surge of severely symptomatic elderly individuals with an associated mortality 1 order of magnitude higher than nations with a lower average age (Al-Tawfiq et al., 2020b). The US CDC had proposed for nursing home residents who are asymptomatic to have increasing monitoring from daily to every shift to more rapidly detect any resident with new symptoms (CDC, 2020). However, how those asymptomatic COVID-19–positive patients in nursing homes or other long-term care facilities should be managed is not clear.
However, it is not clear how to protect patients and healthcare workers from those so-called “non–COVID-19” who might be asymptomatically infected with SARS-CoV-2. Would routine nasopharyngeal swabs and polymerase chain reaction testing be screening of high enough sensitivity that a negative test would indicate that those patients are not infected? What about those who might be incubating or are in the presymptomatic stage? Data suggest that the nasopharyngeal swab had about 75% positivity from a single swab and that 3 swabs are needed to reach more than 95% (Al-Tawfiq and Memish, 2020a). The utility of antibody use in the diagnosis of COVID-19 had not been recommended at this time. Currently, the evidence for the use of serologic testing of SARS-CoV-2 is not optimal. Serologic tests have variable sensitivity and specificity, with different timing of the appearance of these antibodies, and it is not clear if these antibodies confirm protection (Al-Tawfiq and Memish, 2020b).
All the measures mentioned above had dramatic effects on the utilization of healthcare resources. One study reported a decrease by up to 75% of referrals for suspected cancer (Fastenberg et al., 2020). Another study showed a reduction in trauma-related cases in emergency department and hospital admissions (Christey et al., 2020). In an additional study, the emergency room visits of non–COVID-19 patients had significantly decreased over time in Italy due to the COVID-19 pandemic (Hartnett et al., 2020). In a study of 2537 dental visits, dental urgent visits decreased by 38% and nonurgent case visits decreased by 45% (Guo et al., 2020). A recent report pointed out a decreased number of admissions for emergencies such as coronary artery disease and cerebrovascular accidents (Garcia et al., 2020). Similarly, there was a reduction of 39.4% of patients admitted with acute coronary syndrome (Metzler et al., 2020).
There are multiple factors contributing to the apparent reduced utilization of healthcare services by non–COVID-19 patients. Firstly, there is a fear to visit clinics as they might be a place carrying a higher risk of getting infected with SARS-CoV-2 (Rosenbaum, 2020). There are other factors contributing to low patient volume of non–COVID-19 in the healthcare system (Fig. 1 ) besides the fear of patient of becoming infected, as mentioned previously. The greatly curtailed ability to move at times of curfew or lockdown is creating a new challenge. Additional factors include the reduced offering of nonurgent and routine clinic visits or their outright cancellation. The underlying causes for such administrative decisions include the desire to decrease the crowding and its associated increased risk of spread and decreased availability of healthcare workers, often reassigned to meet the increasing demand to care for COVID.
Fig. 1.
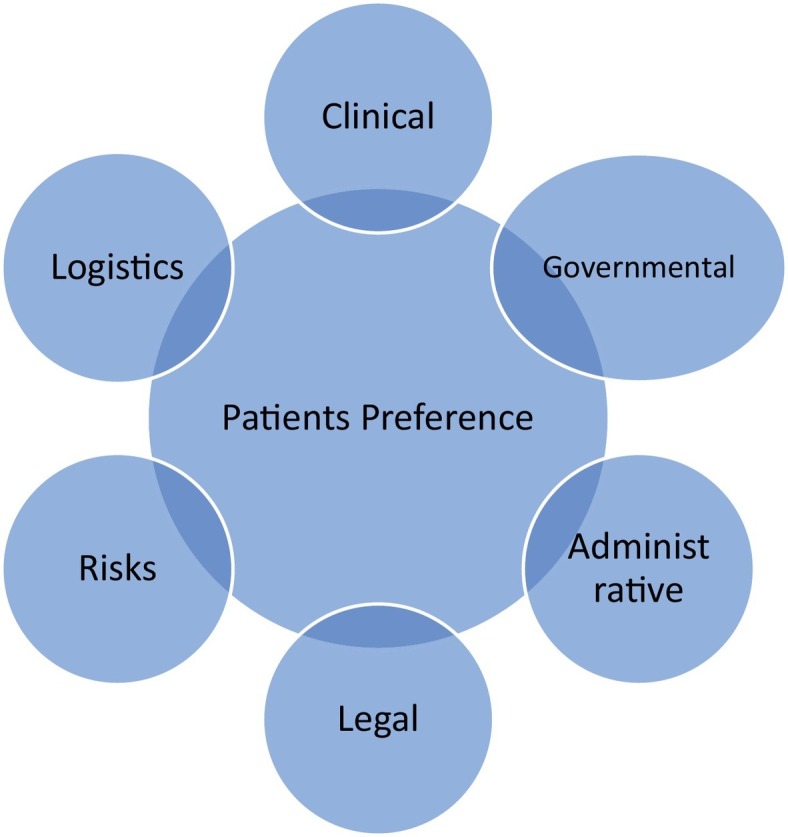
Venn diagram showing a complex interaction of multiple factors contributing to effect of COVID-19 on non–COVID-19 cases.
It is becoming evident, however, that we need to develop new solutions on how healthcare organizations should provide care of non–COVID-19 patients, especially those with chronic diseases. While insisting on keeping patients outside the hospital as much as possible to enhance physical distancing, it is important to bolster social support, as patients might need to come to clinic and not be able to visit the clinics independently. Healthcare workers must take the appropriate precautions to reduce the transmissions of SARS-CoV-2 in the healthcare settings (See Table 1 .). It is the duty of healthcare professionals to reach out to those patients as they feel they are invisible (Welt et al., 2020).
Table 1.
Appropriate precautions to reduce the chances of SARS-CoV-2 transmission in the clinic.
| Call the clinic ahead of time |
| • Practice hand hygiene |
| • Follow social distancing guidelines |
| • Minimize physical contact |
| • Clean and disinfect surfaces and frequently touched items |
| • Respiratory triage to elucidate symptoms, exposure to COVID-19, and travel questions on arrival to the clinic |
| • Wear PPE |
In conclusion, the current COVID-19 pandemic has affected how we treat non–COVID-19 patients and challenged long-held assumptions on how to deliver proper medical care. It behooves healthcare organizations to rethink the way care is provided to COVID-19 and non–COVID-19 patients. Things such virtual visits are an excellent complement to the existing care delivery paradigms and are likely to continue after the pandemic. It is, however, equally clear that even if this pandemic is eventually over and a vaccine can remove the risk of infection and spread of COVID-19, the current world crisis is highlighting the need of re-engineering the way we deliver inpatient and outpatient health-care, including bolstering social support, in order to be prepared when the next calamity will present itself..
References
- Al-Tawfiq J.A., Memish Z.A. Diagnosis of SARS-CoV-2 infection based on CT scan vs. RT-PCR: reflecting on experience from MERS-CoV. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Tawfiq J.A., Memish Z.A. Serologic testing of coronaviruses from MERS-CoV to SARS-CoV-2: learning from the past and anticipating the future. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Tawfiq J.A., Garout M.A., Gautret P. Preparing for emerging respiratory pathogens such as SARS-CoV, MERS-CoV, and SARS-CoV-2. Le Infez Med. 2020;28:64–70. [PubMed] [Google Scholar]
- Al-Tawfiq J.A., Leonardi R., Fasoli G., Rigamonti D. Prevalence and fatality rates of COVID-19: what are the reasons for the wide variations worldwide? Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobrovitz N., Lee J., Mahtani K.R. Preventing non–COVID-19 hospital admissions during a pandemic: a rapid overview of the evidence for high-value medications — CEBM. 2020. https://www.cebm.net/covid-19/preventing-non-covid-19-hospital-admissions-during-a-pandemic-a-rapid-overview-of-the-evidence-for-high-value-medications/
- Borchert A., Baumgarten L., Dalela D., Jamil M., Budzyn J., Kovacevic N. Managing urology consultations during COVID-19 pandemic: application of a structured care pathway. Urology. 2020 doi: 10.1016/j.urology.2020.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Hierarchy of controls n.d. https://www.cdc.gov/niosh/topics/hierarchy/default.html
- Centers for Disease Control and Prevention (CDC) Preparing for COVID-19 in nursing homes. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
- Christey G., Amey J., Campbell A., Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133:81–88. http://www.ncbi.nlm.nih.gov/pubmed/32325471 (accessed July 6, 2020) [PubMed] [Google Scholar]
- Fastenberg J.H., Bottalico D., Kennedy W.A., Sheikh A., Setzen M., Rodgers R. The impact on non–COVID-19 otolaryngology patients during the pandemic! Commentary and insights from orbital emergencies. Otolaryngol Neck Surg. 2020 doi: 10.1177/0194599820931082. 2020 May 26;194599820931082. [DOI] [PubMed] [Google Scholar]
- Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H., Zhou Y., Liu X., Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 2020 doi: 10.1016/j.jds.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartnett K.P., Kite-Powell A., DeVies J., Coletta M.A., Boehmer T.K., Adjemian J. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins Aramco Healthcare. New coronavirus disease (COVID-19) – patients and visitors | Johns Hopkins Aramco Healthcare n.d. https://www.jhah.com/en/new-coronavirus/patients-and-visitors (accessed July 6, 2020).
- Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghadas S.M., Shoukat A., Fitzpatrick M.C., Wells C.R., Sah P., Pandey A. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci U S A. 2020;117:9122–9126. doi: 10.1073/pnas.2004064117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum L. The untold toll — the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020 doi: 10.1056/nejmms2009984. [DOI] [PubMed] [Google Scholar]
- Tirupathi R., Bharathidasan K., Palabindala V., Salim S.A., Al-Tawfiq J.A. Comprehensive review of mask utility and challenges during the COVID-19 pandemic. Le Infez Med. 2020;28:57–63. [PubMed] [Google Scholar]
- Vukkadala N., Qian Z.J., Holsinger F.C., Patel Z.M., Rosenthal E. COVID-19 and the otolaryngologist — preliminary evidence-based review. Laryngoscope. 2020 doi: 10.1002/lary.28672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welt F.G.P., Shah P.B., Aronow H.D., Bortnick A.E., Henry T.D., Sherwood M.W. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic. From the ACC’s Interventional Council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workman A.D., Welling D.B., Carter B.S., Curry W.T., Holbrook E.H., Gray S.T. Endonasal instrumentation and aerosolization risk in the era of COVID-19: simulation, literature review, and proposed mitigation strategies. Int Forum Allergy Rhinol. 2020 doi: 10.1002/alr.22577. [DOI] [PubMed] [Google Scholar]


