Abstract
Background
The Centers for Disease Control and Prevention recommends aggressive contact tracing to control the COVID-19 pandemic. In this work, we (1) describe the development of a COVID-19 contact tracing initiative that includes medical, nursing, and public health students, and is led by clinicians and infectious disease epidemiologists within our health system, and, (2) articulate process steps for contact tracing including workflows and telephone scripts, and, (3) highlight the key challenges and strategies to overcome these challenges.
Methods
A single academic institution-based contact tracing initiative was rapidly scaled to 110 health professional students, four physicians, two epidemiologists, and a research team. Following training, students called patients who were COVID-19 positive and the individuals they were in contact with to ensure proper isolation and quarantine measures. Students also assisted those who faced barriers to quarantine.
Implications
In total, between March 24 and May 28 – this initiative completed contact tracing for 536 confirmed cases, which resulted in the identification of 953 contacts. We aim to disseminate this process, including telephone scripts and workflow, to other health systems for use in their initiatives to respond to the COVID-19 pandemic and future public health emergencies.
Key Words: Contact tracing, Medical education, Coronavirus (COVID-19)
Introduction
In the context of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and the pandemic of the coronavirus disease-2019 (COVID-19) in the United States (US), the Centers for Disease Control and Prevention (CDC) has recommended the identification of symptomatic and asymptomatic infected individuals can contribute to control of the pandemic.1 , 2 The process of contract tracing, with an emphasis on quarantine and isolation, has been previously used to control diseases such as tuberculosis, Middle East Respiratory Syndrome, and Severe Acute Respiratory Syndrome Coronavirus.3, 4, 5 In the US, contact tracing is routinely used for sexually transmitted disease such as syphilis and human immunodeficiency virus (HIV).6 For COVID-19, preliminary results in China, Singapore, South Korea and the state of Washington show evidence that contact tracing can attenuate the spread of disease within the first three months of the pandemic.7 Contact tracing allows for identification of new cases as SARS-CoV-2 transmission has been shown to by highest among close contacts such as household members.8 When effectively implemented in South Korea, contact tracing identified 53 of their first 100 COVID-19 cases.9
Despite the importance of contact tracing in controlling the spread of COVID-19, there some limitations that may hamper its success in the US. Contact tracing requires a coordinated team of many trained individuals operating in a timely manner. Historically, many contact tracing efforts end when the necessary workload and staff requirements overwhelm the team's capacity.10 Presently, the Johns Hopkins Center for Health Security has estimated that the US needs an additional 100,000 contact tracing staff to curb the pandemic.11 In the US, given the limited number of recent large-scale epidemics, state and local Departments of Health (DoH) have been the primary entity responsible for contact tracing, thereby limiting the experience in expanding the workforce to include other individuals. Some state-level DoHs are collaborating with community partners, including librarians, researchers, students, and volunteer nurses, to increase the call capacity to bolster the limited pool of full-time employees available to contact trace.12 In Massachusetts, the Community Tracing Collective, a partnership between the DoH and the non-profit Partners in Health, has trained thousands of English-literate individuals with high school degrees to preform contact tracing work as paid employees.13
A novel solution to expand the contact tracing workforce includes the integration of health professional students. Students have prerequisite skills, such as health information privacy compliance training, interpersonal communication, and knowledge of disease transmission, to perform contact tracing, particularly at times when they cannot be in clinical care settings due safety risks.14 However, little work has described a process for leveraging health professional students to contribute to contact tracing during the time of a pandemic. Early in the pandemic, our academic health system developed and implemented a contact tracing initiative independent of the state DoH. Based upon this experience, we (1) describe the development of a contact tracing initiative that includes medical, nursing, and public health students and is led by clinicians and infectious disease epidemiologists within our health system, and, (2) articulate process steps for contact tracing, and, (3) highlight the key challenges and strategies to overcome these challenges for others to use in the design of their initiative. We aim to disseminate this process, including telephone scripts and workflow, to other academic health systems for use in their initiatives to respond as a community to the COVID-19 pandemic and potential future public health emergencies.
Methods
At the end of March 2020, health professional students at Penn State College of Medicine (PSCOM) were required to withdraw from in-person clinical care of patients.14 In response, students along with education and health system leadership designed the PSCOM Response Team to remotely assist in the pandemic.15 This student-led initiative paired students with nearly 20 health systems-aligned projects to meet the needs of patients and support the health system, including the surrounding community. Task forces met four criteria – all tasks were: 1) performed remotely, 2) faculty-supervised, 3) educationally beneficial, and 4) were aligned with health system needs. By design, active participation in a taskforce provided the opportunity for students to receive educational credit.
The contact tracing taskforce was developed to meet the need for mitigation of community spread of COVID-19 in central Pennsylvania and acted to supplement the State DoH. The goals of the initiative were to build a student-run team of motivated students to perform contact tracing, ensure individuals were using proper isolation/quarantine measures, and identify probable COVID-19 cases (i.e., symptomatic contacts). A secondary goal was for students to develop the core competencies of clinical and health systems science inclusive of public health, methods for disease control, social determinants of health, and interprofessional collaboration.16
Our Process
Our initial step in developing a contact tracing initiative was to recruit health professional students with an interest in public health or passion for contributing to the disease control effort. The primary team consisted of nine medical students, one internal medicine physician (C.S.), and one infectious disease epidemiologist (P.D.) with contact tracing experience. The team was also supported by research staff (of C.S.) who volunteered time to provide technical support in project management and database design (i.e. HIPAA compliant Research Electronic Data Capture (REDCap).17 Daily meetings were vital in developing a shared understanding of the work and creating the communication script to be used for calling individuals who were (1) laboratory-confirmed COVID-19 positive (“cases”) or (2) exposed to a known case (“contacts”). Students received several training sessions that utilized simulated case vignettes with group observation and feedback. We adapted methods from those designed by the World Health Organization during the Ebola Outbreak.18
Organizational and Team Structure
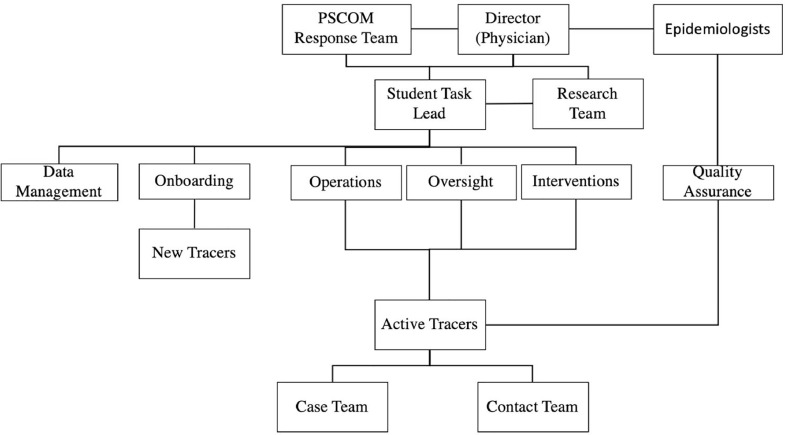
An organizational structure was developed in mid-April 2020. Student involvement encompassed a student lead who provided oversight of several committees: Intervention, Quality Assurance, Operations, Oversight, Data Management and Onboarding. An overview of the expanded team structure is outlined in Figure 1 . A description of roles and responsibilities of the all team members and subcommittees is outlined in Table 1 .
Figure 1.
Expanded Contact Tracing Initiative Structure. Director, epidemiologists, and the research team were faculty and employees, while all other teams were run by and composed of students. PSCOM = Penn State College of Medicine
Table 1.
Contact Tracing Initiative Roles and Responsibilities of Leaders and Subcommittees
| PSCOM Response Team | Oversight all of student task forces & recruitment of students to task forces |
|---|---|
| Director | Oversight of entire contact tracing effort and approval of contact testing |
| Epidemiologists | Development of case and contact scripts with input from Interventions to optimize caller satisfaction, contact identification, and data extraction. Oversight of active tracers as a measure of quality control via three-way phone calls |
| Student Task Lead | Oversight of all student subcommittees and point of contact for PSCOM Response Team |
| Research Team | Implementation of scripts into a survey with branching logic using REDCap software to ensure the protection of PHI |
| Data Management | Development of daily of key performance indicators KPI to track efficacy and timeliness of the contact tracing program |
| Onboarding | Training of new callers on using REDCap, following workflows, and making calls |
| Operations | Management of standard operating procedure & optimization of workflow |
| Oversight | Input new cases into the REDCap system and distributes calls to case and contact callers |
| Interventions | Workshop the case and contact scripts to optimize caller satisfaction, contact identification, and data extraction as well as identify barriers to effective quarantining. Connect cases/contacts with resources to overcome these barriers. |
| Quality Assurance | Joined three-way calls at random intervals with recently trained case/contact team members and cases/contacts to provide feedback and ensure that up-to-date information is delivered and the standard operative procedures are followed. |
PSCOM = Penn State College of Medicine, PHI = Personal Health Information, REDCap = HIPAA compliant Research Electronic Data Capture, KPI = Key Performance Indicator
Contact Tracing Workflow
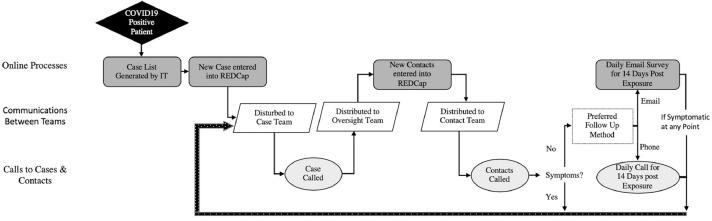
Early in the development of the initiative, we created two teams to perform the work- a case team and a contact team. Using REDCap capabilities, the contact team was unable to access information about confirmed cases as a built-in measure to protect the confidentiality. Figure 2 demonstrates the workflow from a patient with a COVID-19 positive test result through the follow-up procedure of their contacts. Cases consisted of patients who tested positive for COVID-19 at our institution, a tertiary care and designated regional COVID-19 treatment center.
Figure 2.
Contact Tracing Workflow. Case information was given to the Oversight team, who logged the patient in REDCap (as an identification number) and distributed the patient to the case team. The case team called cases and identified contacts. Oversight then added contacts into REDCap (as an identification number) and distributed them to the contact team for follow-up. Follow-up was conducted via email or telephone for 14 days after exposure based on the contact's personal preference. If a contact was symptomatic at any point, they were referred for testing and to the case team for contact tracing. REDCap = HIPAA compliant Research Electronic Data Capture, IT = Information Technology
When contacting cases or contacts, students used pre-made phone scripts designed with assistance from infectious disease epidemiologists (P.D., C.E.) and further optimized by Operations and Intervention. Phone scripts were integrated into REDCap with branching logic. During a case interview, students gathered the information for all individuals who had been in contact with the patient 48 hours prior to symptom onset up to the time of the case call. Key features of the case phone script are shown in Appendix A. For contact calls, these individuals were notified of their possible COVID-19 exposure but were not informed of who or when they may have been exposed. Key aspects of this contact phone script are outlined in Appendix B. If the contact was symptomatic at the time of the initial contact call or became symptomatic during the follow-up period, they were designated as a presumptive case and passed back to the case team for subsequent contact identification. If the contact was asymptomatic at the time of initial call, they were followed for 14 days (Day 0 was initial exposure) to assess for the development of new symptoms. The 14-day follow up period is based on the estimated maximum incubation period for the 99th-percentile of individuals exposed to SARS-CoV-2.19 REDCap provided an automated number of days the individual should quarantine and be followed after the phone call based on the day they were exposed. For example, if the contact was called two days after exposure they were instructed to quarantine for 12 days. For 14 consecutive days after exposure, the contact was assessed for COVID-19 symptoms via an emailed electronic survey through REDCap or a daily phone call, based on the contact's personal preference. The email option provided automated feedback to the Operations team if a contact became symptomatic at any point during the follow up period.
Follow-Up with Case and Contact Issues
If a contact was symptomatic or developed new symptoms consistent with COVID-19, an internal medicine physician was notified. The physician then ordered COVID-19 testing for the contact at our institution as these individuals were considered to have a high likelihood of having contracted COVID19 given their exposure with a confirmed or presumptive case. Additionally, the contact was immediately referred to the case team to be interviewed as a presumptive positive COVID-19 case.
Onboarding Additional Team Members
Given the exponential rise of COVID-19 cases during the pandemic, it was vital to develop an effective and consistent onboarding program to rapidly integrate students into the contract tracing process. By the end of April 2020 and within a month of starting the initiative, an additional 101 students, three physicians, and an epidemiologist (C.E.) were incorporated into the contact tracing initiative. Figure 3 demonstrates the process from recruitment to integration into the workflow of calling cases/contacts. In addition to general orientation sessions that introduced students to contact tracing and the workflow, our process used “veteran team members” experienced in making case/contact calls to aid in training team members. New tracers listened to a call made by a veteran caller, and then they made a call that was observed by the veteran caller. This model allowed for large-scale education and integration of students into the process. Training was considered complete when new tracers were observed by one of the Quality Assurance officers, a team that was led by our infectious disease epidemiologists and functioned to standardize the quality of calls. The training process aimed to generate specialized case and contact callers with the flexibility to adapt to continuously changing standard operating procedures. Students spent approximately five hours of onboarding training prior to making their first official phone call.
Figure 3.
Contact Tracing Onboarding Process. Contact Tracers were selected from student volunteers on a first-come-first-serve basis and underwent online REDCap training. After a large group onboarding session, which explains the workflow and standard operating procedure to the new members, they were divided into Case and Contact Teams. The students were paired off to train with partners, listen to a call by a veteran team member, and then were observed by the same veteran caller. Lastly, the Quality Assurance team observed each caller at least once before they were fully onboarded to the team. REDCap = HIPAA compliant Research Electronic Data Capture
Challenges Encountered, Key Performance Indicators, and Solutions
The challenges we encountered mirror those encountered in previous reviews on contact tracing during the Ebola outbreak, including effective testing, organizational efficiency, interventional efficacy, cultural and language barriers, community buy-in and effective isolation.20 First, the effectiveness of contact tracing can be affected by low testing capacity. While our impact may be limited by inadequate or delayed testing, our phone calls with cases/contacts provided advice on effective isolation and quarantine with the goal to interrupt disease transmission within the community. Second, it is imperative to track time from case identification to contact notification. To do this, we followed the latency of each step shown in the contact tracing workflow (Figure 2). Notable delays in our contact tracing process were a result of slow test results (average 5.2 days) and reporting of test results to the contact tracing program (average 2 days). As the process continued the average time of test result was reduced with an increase in testing capacity at our institution. This was vital to the success of our program given that timely test is key for successful contact tracing.21 While the program had little control over delays in test results, the program refined protocols continuously to minimize time between test date and first communication. Tracking these times helped identify which processes were rate-limiting steps that were addressed by optimizing workflow handoffs, training additional callers to support fluctuations in cases loads, and improving management of active callers.
To optimize interventional efficacy and based upon prior studies on contact tracing, the data management team identified Key Performance Indicators (KPIs) to help track the impact of the initiative. 9 , 20 , 22 One KPI is the ratio of contacts per case, which characterized the number of people potentially exposed by one individual. However, contacts per case have been cited to range from 1-122 in respiratory diseases like tuberculosis, and there is mixed opinion about the utility of this indicator.22 Additionally, contacts per case is predictably lower during a stay at home order, again limiting its utility. In total, between March 24 and May 28 – this initiative completed contact tracing for 536 confirmed cases, which resulted in the identification of 953 contacts. Of the 953 contacts, 27% developed symptoms and were treated as presumptive cases. The 261 contacts who were treated as presumptive cases were an important measure of success as the rapid identification of symptoms allowed for timely quarantining and prevention of community spread.
A KPI we have used to guide our initiative is “contact knowledge of exposure.” Our intervention's impact is maximized when reaching contacts that are unaware that they have been exposed as these individuals are less likely to be appropriately quarantining or to have noticed symptom onset. The benefit provided to those already aware of their exposure is different, but not negligible. For those individuals, we provided education and resources to address challenges with quarantining. This was done both verbally during the phone call as well as through text, pictures, and resource links that were compiled into one comprehensive document and sent to cases and contacts via e-mail after each call.
To address language and cultural barriers, we asked cases and contacts for their preferred language. If their preferred language was not English, we used a third-party translation service employed by our institution. For identified cultural communities with significant spread, we consulted physicians familiar with the patient population to understand the best way to care for that particular group. We also recruited students who were fluent in the non-English languages we most frequently encountered to translate our information and resource sheets into those languages.
To measure community buy-in, we tracked the number of calls rejected and identified callers that were resistant to quarantining. To improve our outcomes, the Interventions team adjusted the scripts to establish rapport, elicit the case/contact's perspective, and emphasize the positive impact of quarantining. Approximately, 94% of cases and 84% of contacts agreed to participate in the contact tracing program and agreed to receive follow-up calls or emails, but strict compliance with isolation and quarantine procedures were not measured.
Finally, we encountered extensive challenges in individuals’ ability to effectively isolate or quarantine. Many cases and contacts share rooms, kitchens and bathrooms, which dramatically increases household spread. Others lack social and financial resources to deliver essentials and purchase food. To address these problems, the Interventions team gathered a variety of social resources and served as resource consultants for callers. Resources ranged from grocery delivery services to mask-making instructions. Some cases and contacts required a referral to social work. Eight percent of individuals received support services to aid in quarantine. Partnering with other student groups, local resource centers, and those in social service roles within our health system was key in facilitating the delivery of these resources.
Implications
Here, we present a real-world framework for establishing a contact tracing initiative using medical, nurse practitioner, and public health students removed from clinical obligations. Students were incentivized to participate by academic credit. The framework described can be adopted by Academic Healthcare Centers, Institutions, or community-based practices, that have an available workforce. This framework can help to suppress the resurgence of COVID-19 within local communities. While modeling suggests that contact tracing is most effective in the beginning of epidemics when local transmission is limited, the main arguments proposed against continuing contact tracing efforts are based on costliness and workforce requirements.23 Our volunteer-based contact tracing initiative helps to bypass these two limitations by leveraging an available workforce and providing alternative incentives. Therefore, we hope other institutions can adopt this framework immediately and begin their own contact tracing effort. This is particularly important in areas that lack an aggressive contact tracing process.
Furthermore, contact tracing that overlaps with other institutions’ initiatives is not necessarily duplicative and should not be considered mutually exclusive. While combined efforts cannot be reasonably expected to double the impact of contact tracing, the resources and approaches we provide to assist case and contact quarantine are inherently different and can ultimately contribute to the success of future efforts.
Contact tracing workforces may not be limited to healthcare professional students with clinical knowledge. The minimum requirements to apply for the Massachusetts Community Tracing Collective include a high school diploma and English literacy.24 If the training process can sufficiently prepare callers to conduct a baseline screen for symptoms in contacts and provide advice about quarantining and hygiene, extensive healthcare experience for callers is not necessary. We posit this model can be adopted by any public or private healthcare institution with 1) ongoing testing for an infectious disease process, 2) access to a willing and available workforce (hospital volunteers, community volunteers, students), 3) experienced personnel capable of training contact tracers, and, 4) the technical ability to ensure privacy and HIPAA compliance and cybersecurity. While this approach can be adopted anywhere, medical institutions that have removed students, volunteers, or employees from clinical care to minimize exposure risk and personal protective equipment utilization have created a unique workforce to opportunity to capitalize on an existing, motived workforce.
While the noble cause of preventing transmission of disease and saving lives during a pandemic may be enough to recruit an adequate number of volunteers, it may be beneficial to have incentives in place to encourage energized participation. Contact tracing is a time consuming and labor-intensive process in which long and frequent calls are required to maximize impact. Therefore, institutions that can offer academic credit for contact tracing have a unique advantage. Alternatively, participants can be incentivized through volunteer hours. If funding can be acquired, callers can be paid directly, per the Community Tracing Collective's model.24
Modeling suggests that intensive contact tracing is enough to control a new COVID-19 outbreak in three months. The model also predicts that shortened time from symptom onset to isolation, increased identification of cases by contact tracing and limited transmission before symptom onset decrease this value further.25 As infection from the SARS-CoV-2 pathogen continues to spread in communities, we encourage institutions to use this framework to leverage health professional students to trace cases and their contacts to suppress the pandemic including any future surges in cases during the reopening of the country. The framework will also simultaneously provide students the opportunity to learn and practice skills in communication, collaboration, and health systems science.
Footnotes
Conflict of Interest: None to report.
Acknowledgments: We thank Dr. Christopher Sciamanna (Penn State College of Medicine), Dr. Ping Du (Penn State College of Medicine), and Dr. Cara Exten (Penn State College of Nursing) for their leadership and support of this contact tracing program. The authors would also like to acknowledge Sheilah Yohn (Penn State College of Nursing) for her efforts in organizing the interprofessional collaboration on this initiative in addition to Jim Marks (Penn State College of Medicine) for his work as REDCap support and database management. Further, we thank the more than one hundred student volunteer contact tracers for their commitment to this program and to the health of our community. This manuscript is a direct result of that commitment.
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.ajic.2020.08.012.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Simmons-Duffin S, Stein R. CDC Director: 'Very Aggressive' Contact Tracing Needed For U.S. To Return To Normal. National Public Radio. Published April 10, 2020. Available at:https://www.npr.org/sections/health-shots/2020/04/10/831200054/cdc-director-very-aggressive-contact-tracing-needed-for-u-s-to-return-to-normal. Accessed April 21, 2020
- 2.Lalvani A, Pathan AA, Durkan H, et al. Enhanced contact tracing and spatial tracking of Mycobacterium tuberculosis infection by enumeration of antigen-specific T cells. Lancet. 2001;357:2017‐2021. doi: 10.1016/S0140-6736(00)05115-1. [DOI] [PubMed] [Google Scholar]
- 3.Fox GJ, Barry SE, Britton WJ, Marks GB. Contact investigation for tuberculosis: a systematic review and meta-analysis [published correction appears in Eur Respir J. 2015 Aug;46(2):578] Eur Respir J. 2013;41:140‐156. doi: 10.1183/09031936.00070812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ki HK, Han SK, Son JS, Park SO. Risk of transmission via medical employees and importance of routine infection-prevention policy in a nosocomial outbreak of Middle East respiratory syndrome (MERS): a descriptive analysis from a tertiary care hospital in South Korea. BMC Pulm Med. 2019;19:190. doi: 10.1186/s12890-019-0940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glasser JW, Hupert N, McCauley MM, Hatchett R. Modeling and public health emergency responses: lessons from SARS. Epidemics. 2011;3:32–37. doi: 10.1016/j.epidem.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macke BA, Maher JE. Partner notification in the United States: an evidence-based review. Am J Prev Med. 1999;17:230–242. doi: 10.1016/s0749-3797(99)00076-8. [DOI] [PubMed] [Google Scholar]
- 7.Pung R, Chiew CJ, Young BE, et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039–1046. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bi Q, Wu Y, Mei S, et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study [published correction appears in Lancet Infect Dis. 2020 Jul;20(7):e148] Lancet Infect Dis. 2020;20:911–919. doi: 10.1016/S1473-3099(20)30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ng Y, Li Z, Chua YX, et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore - January 2-February 29, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:307–311. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhillon RS, Srikrishna D. When is contact tracing not enough to stop an outbreak? Lancet Infect Dis. 2018;18:1302–1304. doi: 10.1016/S1473-3099(18)30656-X. [DOI] [PubMed] [Google Scholar]
- 11.Watson C, Cicero A, Blumenstock J, Fraser M. Center for Health Security. 2020. A National Plan to Enable Comprehensive COVID-19 Case Finding and Contact Tracing in the US; pp. 1–16.https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2020/a-national-plan-to-enable-comprehensive-COVID-19-case-finding-and-contact-tracing-in-the-US.pdf Available at: Accessed April, 21 2020. [Google Scholar]
- 12.Westervelt E. San Francisco Ramps Up Back-To-Basics Contact Tracing To Stop COVID-19. National Public Radio. Published April 16, 2020. Available at: https://www.npr.org/sections/health-shots/2020/04/16/835396565/san-francisco-ramps-up-back-to-basics-contact-tracing-to-stop-covid-19. Accessed April 21, 2020.
- 13.Mass.Gov. 2020. Baker-Polito Administration Announces COVID-19 Community Tracing Collaborative to Further Mitigate the Spread of Virus [press release]https://www.mass.gov/news/baker-polito-administration-announces-covid-19-community-tracing-collaborative-to-further Available at: Accessed April 21, 2020. [Google Scholar]
- 14.Whelan A, Prescott M, Young G, Catanese VM, Mckinney R. Association of American Medical Colleges; 2020. Guidance on Medical Students’ Participation in Direct Patient Contact Activities; pp. 1–6.https://www.aamc.org/system/files/2020-04/meded-April-14-Guidance-on-Medical-Students-Participation-in-Direct-Patient-Contact-Activities.pdf Available at: [Google Scholar]
- 15.Carlson S, Gonzalo J, Hammound MM, Havemann C, Lomis KD. American Medical Association Innovations in Medical Education Webinar Series; 2020. Deploying Students in alternative roles during COVID-19: Preserving clinical educational objectives and supporting competency development.https://www.ama-assn.org/system/files/2020-04/april-2020-covid-19-webinar.pdf Available at: [Google Scholar]
- 16.Skochelak SE, Hawkins RE, Lawson LE, Starr SR, Borkan J, Gonzalo JD. 1st ed. Elsevier; 2017. Health Systems Science. [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization . 2015. Contact tracing during an outbreak of Ebola virus disease; pp. 1–36.https://www.who.int/csr/resources/publications/ebola/contact-tracing/en/ Available at: [Google Scholar]
- 19.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saurabh S, Prateek S. Role of contact tracing in containing the 2014 Ebola outbreak: a review. Afr Health Sci. 2017;17:225–236. doi: 10.4314/ahs.v17i1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kretzschmar ME, Rozhnova G, Bootsma MCJ, van Boven M, van de Wijgert JHHM, Bonten MJM. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. Lancet Public Health. 2020;5:E452–E459. doi: 10.1016/S2468-2667(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baxter S, Goyder E, Chambers D, Johnson M, Preston L, Booth A. NIHR Journals Library; Southampton (UK): 2017. Interventions to improve contact tracing for tuberculosis in specific groups and in wider populations: an evidence synthesis. [PubMed] [Google Scholar]
- 23.Farrahi K, Emonet R, Cebrian M. Epidemic contact tracing via communication traces. PLoS One. 2014;9:e95133. doi: 10.1371/journal.pone.0095133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.2020. Partners In Health to Help State Trace Contacts of COVID-19 Patients in Landmark Agreement with MA Gov's Office.https://www.pih.org/ma-response Available at: [Google Scholar]
- 25.Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. The Lancet Global health. 2020;8:e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.