Abstract
Background
Over the past 20 years, the development of regional ST-elevation myocardial infarction (STEMI) care systems has led to remarkable progress in achieving timely coronary reperfusion with attendant improvement in clinical outcomes, including survival. Despite this progress, contemporary STEMI care does not consistently meet the national guideline-recommended goals, which offers an opportunity for further improvement in STEMI outcomes. The lack of single, comprehensive, national STEMI registry complicates our ability to improve STEMI outcomes in particular for high-risk STEMI subsets such as cardiac arrest (CA) and/or cardiogenic shock (CS).
Objectives
To address this need, the Midwest STEMI Consortium (MSC) was created as a collaboration of 4 large, regional STEMI care systems to provide a comprehensive, multicenter, and prospective STEMI registry without any exclusionary criteria.
Methods
The MSC is a collaboration of 4 large, regional STEMI care systems: Iowa Heart Center in Des Moines, IA; Minneapolis Heart Institute Foundation in Minneapolis, MN; Prairie Heart Institute in Springfield, IL; and The Christ Hospital in Cincinnati, OH. Each has similar standardized STEMI protocol and together include 6 percutaneous coronary intervention (PCI)-capable hospitals and over 100 non-PCI-capable hospitals. Each center had a prospective database that was transferred to a data coordinating center to create the multicenter database. The comprehensive database includes traditional risk factors, cardiovascular history, medications, time to treatment data, detailed angiographic characteristics, and short- and long-term clinical outcomes up to 5-year for myocardial infarction, stroke, and cardiovascular and all-cause mortality. Ten-year mortality rates were assessed by using national death index.
Results
Currently, the comprehensive database (03/2003–01/2020) includes 14,911 consecutive STEMI patients with mean age of 62.3 ± 13.6 years, female gender (29%), and left anterior descending artery as the culprit vessel (34%). High risk features included: Age >75 years (19%), left ventricular ejection fraction <35% (15%), CA (10%), and CS (8%).
Conclusion
This collaboration of 4 large, regional STEMI care systems with broad entry criteria including high-risk STEMI subsets such as CA and/or CS provides a unique platform to conduct clinical research studies to optimize STEMI care.
Abbreviation: ACC, American College of Cardiology; AHA, American Heart Association; CABG, Coronary artery bypass grafting; CA, Cardiac arrest; CCL, Cardiac catheterization laboratory; CS, Cardiogenic shock; D2B, Door-to-balloon; ECMO, Extracorporeal membrane oxygenation; ED, Emergency department; EKG, Electrocardiogram; EMS, Emergency medical service; IABP, Intra-aortic balloon pump; IHC, Iowa Heart Center; LBBB, Left-bundle-branch block; MHIF, Minneapolis Heart Institute Foundation; PHI, Prairie Heart Institute; PCI, Percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction; TCH, The Christ Hospital
Keywords: Registry, Myocardial infarction, Angioplasty, Cardiogenic shock, Cardiac arrest
1. Introduction
ST-elevation myocardial infarction (STEMI) is the consequence of acute occlusion of an epicardial coronary artery [1]. Based on the concept of “time is muscle”, the optimal therapy for STEMI is immediate restoration of coronary artery blood flow [2]. In the US, the number and geographical distribution of percutaneous coronary intervention (PCI)-capable hospitals, lack of a single organized emergency medical service (EMS), and absence of a single, comprehensive, national STEMI registry create challenges to achieve timely reperfusion in STEMI [3].
A comprehensive and accurate STEMI database is essential to overcome the challenges in STEMI care. A variety of different national programs have launched registries to populate STEMI data. However, remarkable variability exists between these registries especially during the process of identification and selection of STEMI patients, which limit their accuracy and generalizability. For instance, the CathPCI Registry by American College of Cardiology's (ACC) NCDR (National Cardiovascular Data Registry) only includes STEMI patients undergoing PCI, thereby excluding patients without PCI or a culprit artery, requiring coronary artery bypass graft surgery, or treated with fibrinolytics or medical therapy [4]. Another example, the ACTION-GWTG (Acute Coronary Treatment and Intervention Outcomes Network-Get With The Guidelines) Registry by ACC's NCDR and American Heart Association (AHA) included a modest number of centers and have now separated into two different registries. The ACTION-GWTG registry excludes in-hospital or periprocedural STEMI patients [5]. In addition to these registries facilitated by professional societies, payor STEMI databases such as Centers for Medicare & Medicaid Services and Hospital Quality Alliance or Nationwide Inpatient Sample ICD-10-CM/PCS have many limitations [6,7]. The former excludes the majority of patients under age of 65 and the latter is hampered by the challenge of ICD coding.
The development of regional STEMI care systems has facilitated remarkable improvements in STEMI outcomes over the past 2 decades [3,8]. Prehospital electrocardiogram (EKG), prehospital cardiac catheterization laboratory (CCL) activation, predetermined interhospital transfer protocols, and emergency department (ED) bypass at PCI-capable hospitals constitute the key components of regional STEMI care systems [9]. While the national registries and payor databases often fail to capture all STEMI patients and in particularly lack details regarding high-risk STEMI patients such as cardiac arrest (CA) and/or cardiogenic shock (CS); regional STEMI registries are able to overcome these limitations by tracking all consecutive STEMI patients including those with high-risk features. Thereby, regional STEMI registries allows a comprehensive assessment including detailed angiographic characteristics and short- and long-term clinical outcomes [[10], [11], [12], [13]].
Building on the concept of regional STEMI care systems, the AHA and Duke Clinical Research Institute designed the “largest” regional STEMI care systems' projects, Mission: Lifeline STEMI Systems Accelerator-1 and -2 in 16 and 12 regions across the US, respectively. There was a significant reduction in first medical contact-to-balloon time for both direct presenter (via EMS) and transferred STEMI patients in the Accelerator-1 project. However, in-hospital mortality rates were unchanged during the study period [14]. In the Accelerator-2 project, there were significant reductions in both reperfusion time and in-hospital mortality rates for direct presenter (via EMS) STEMI patients [15]. It is noteworthy that only in-hospital outcomes were assessed in both projects. More important, over one-third of the Accelerator-2 study participants were excluded from the data analysis, including those with high risk features such as CA or need for intubation. Therefore, the Accelerator projects' findings may not necessarily reflect a “real-world” practice.
The Midwest STEMI Consortium (MSC) is a collaborative engagement of 4 high-volume regional STEMI centers, located in Des Moines, IA; Minneapolis, MN; Springfield, IL; and Cincinnati, OH. These regional STEMI care systems centers were designed to standardize care within a broad spectrum of urban, semi-urban, and rural communities in the region. Over the past 2 decades, these centers have prospectively collected comprehensive clinical data on all consecutive STEMI patients within their respective systems. As such, the MSC provides a unique, “real-world” perspective regarding care processes and clinical outcomes among a diverse STEMI population without any exclusionary criteria. Therefore, the MSC registry provides a unique clinical archive that can be utilized as a tool to conduct comparative analysis for ongoing clinical trials and as a conduit to facilitate the expeditious exploration of evolving pharmacological and interventional therapies in a contemporary STEMI population.
2. Methods
2.1. Consortium organization, oversight, and approval
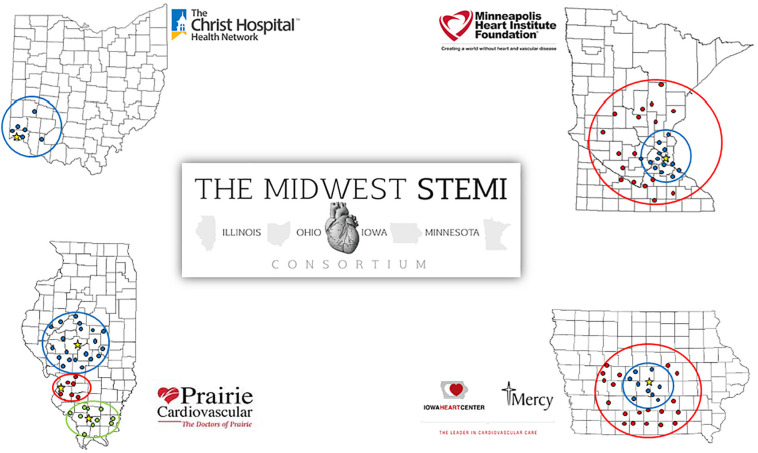
The MSC is a collaboration of Iowa Heart Center in Des Moines, IA (IHC); Minneapolis Heart Institute Foundation in Minneapolis, MN (MHIF); Prairie Heart Institute in Springfield, IL (PHI); and The Christ Hospital in Cincinnati, OH (TCH) (Fig. 1 ). The MSC executive committee is comprised of 12 members: Two cardiologists and 1 STEMI coordinator from each center. Members meet monthly via conference call to share ideas and determine future strategies. Each center has 1 principal investigator who oversees the implementation of the standardized STEMI protocol and optimizes the database operation.
Fig. 1.
The Midwest STEMI Consortium map.
TCH serves as the coordinating center and MHIF as the data coordinating center. The data coordinating center is responsible for creation and maintenance of the master database and execution of statistical analyses.
The study protocol, data sharing agreement, and relevant supporting information have been approved by Institutional Review Boards (IRB) in each center. The MSC was funded by a grant from ACC Accreditation Services.
2.2. Consortium resources
MHIF is a group of over 70 cardiovascular, vascular, and cardiothoracic surgeon specialists at Abbott Northwestern Hospital in Minneapolis, MN. MHIF created the Level 1 MI program which was one of the foremost regional transfer systems using a standardized protocol designed to improve time to reperfusion for STEMI patients who initially presented to non-PCI-capable hospitals. Thirty-one non-PCI-capable hospitals have participated in the Level 1 MI program, of those, 11 are situated within 60-mile from MHIF (designated as Zone 1) and 20 within 60- to 210-mile (Zone 2). Of note, hospitals in Zone 2 use a pharmaco-invasive approach for patients with anticipated door-to-balloon (D2B) time over 120-min. Standardized STEMI protocol and predetermined transfer plans (ground or air based on locations, availability, and weather) were implemented in each non-PCI-capable hospital. STEMI patients transferred from non-PCI-capable hospitals bypass the ED and proceed directly to the CCL. Experiences from the Level 1 program have contributed to advances in STEMI care particularly in improving time to reperfusion, initiating therapeutic hypothermia protocol for out-of-hospital CA, lowering false-positive CCL activation, caring in-hospital STEMI patients, and approaching to new or presumed new left bundle branch block in STEMI patients [10,11,[16], [17], [18], [19], [20], [21], [22]].
IHC is a group of over 60 cardiovascular, vascular, and cardiothoracic surgeon specialists at MercyOne Des Moines Medical Center in Des Moines, IA. IHC adopted AHA Mission: Lifeline as a standardized STEMI protocol throughout the state [13]. The IHC protocol was designed similar to the MHIF Level 1 protocol including Zone 1 and 2 hospitals. IHC has referral relationship with 30 non-PCI hospitals to expedite care by bypassing the ED and proceed directly to the CCL.
PHI is a group of over 70 cardiovascular, vascular, and cardiothoracic surgeon specialists at 3 tertiary hospitals located in Springfield, O'Fallon, and Carbondale, IL and integrated within Hospital Sisters Health System. PHI has referral relationships with 34 non-PCI-capable hospitals. The PHI STAT Heart transfer program was one of the first in the US to focus on streamlining emergent STEMI care to meet the national goals of reperfusion times [12]. Standardized STEMI protocol with predetermined transfer routes were implemented to ensure timely transfer of STEMI patients by bypassing the ED and proceeding directly to the CCL.
TCH is a large, 555-bed, tertiary referral center in Cincinnati, OH with 44 cardiovascular, vascular, and cardiothoracic surgeon specialists. TCH was one of the first hospitals in the US to facilitate 12-lead EKG transmission by EMS and empower EMS to activate the CCL. TCH developed Chest Pain Network in 2007 to standardize protocols and develop transfer plans for STEMI patients with 6 non-PCI-capable hospitals. All patients either directly presented to PCI-capable hospitals by EMS or were transferred from non-PCI-capable hospitals bypass the ED and proceed directly to the CCL.
2.3. Standardized STEMI protocol
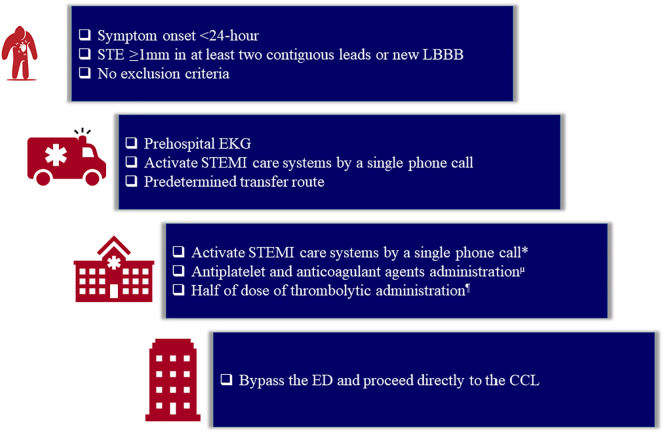
IHC, MHIF, PHI, and TCH described their well-established regional STEMI care systems in multiple publications by using similar standardized STEMI protocols; Statewide STEMI, Level 1, STAT HEART, and STEMI ALERT, respectively. The MSC's standardized STEMI protocol was created by combining of the existing standardized STEMI protocols in each center (Fig. 2 ).
Fig. 2.
The Midwest STEMI Consortium standardized STEMI protocol. Created by using well-established standardized protocols in each center. Abbreviations: CCL: cardiac catheterization laboratory; ED: emergency department; EKG: electrocardiogram; LBBB: left bundle branch block; STE: ST-elevation; STEMI: ST-elevation myocardial infarction. *Unless STEMI care systems were activated by emergency medical services. μAspirin 324 mg, Ticagrelor 180 mg or Clopidogrel 600 mg, and Heparin 50 U/kg (max 4000 U). ¶TNKase IVP, if expected time to reperfusion exceed 120-min.
The core steps in the protocol could be summarized as (1) acquiring a prehospital EKG, (2) activating the STEMI care systems by a single phone call, (3) administering the guideline-recommended initial antithrombotic therapy prior arrival to PCI-capable hospitals, (4) routing predetermined transfer plan to PCI-capable hospitals, and (5) bypassing the ED to proceed directly to the CCL at PCI-capable hospital.
2.4. Patient population
MHIF was the pioneer among all the centers to start enrolling consecutive adult patients with STEMI in a prospective registry since 2003. IHC, PHI, and TCH created their prospective registries in 2004, 2005, and 2007, respectively. Adult patients with ST-elevation ≥1 mm in at least 2 contiguous leads or presumably new left-bundle-branch block (LBBB) within 24-h of symptom onset included in the prospective registry. There were no exclusion criteria; thus, each registry included all consecutive adult patients with STEMI activations including those with CA, CS, advanced age, or initial non-diagnostic EKG to name few.
2.5. Data collection
Each STEMI coordinator abstracted data prospectively via chart review. Data elements can be categorized into risk factors, medications, pre-admission status, time data, cardiac assessment, angiographic details, diagnostic tests, and outcomes. Supplement 1 presents the data collection form and details/definitions.
The database in each center was stored on a secure and HIPAA compliant server with a firewall-protected network and sent to the data coordinating center, MHIF, via encrypted email to create the multicenter, master database.
2.6. Data analysis
Continuous variables will be presented as means or medians and assessed by using analysis of t-tests. Categorical variables will be presented as frequencies or percentages and assessed by using analysis of χ2 or Fisher exact tests. Survival rates will be presented as Kaplan-Meier plots and assessed by using log-rank tests. All analyses will be performed with Stata and p value of <0.05 will be considered as statistically significant.
3. Results
From 03/2003 to 01/2020, the data for 14,911 consecutive STEMI patients have been collected. Table 1 presents the baseline characteristics. The mean age was 62.3 ± 13.6 years. Elderly patients (age ≥75 years) represent 19% and female 29%. At baseline, 28% had prior coronary artery disease, 61% hypertension, 55% hyperlipidemia, 22% diabetes mellitus, and 60% smoking history. Left anterior descending artery was the culprit vessel in one-third of patients. Severely reduced left ventricular ejection fraction (<35%) was seen in 15%. The proportion of patients with CA was 10% while 8% developed CS prior to primary PCI.
Table 1.
Baseline characteristics of the Midwest STEMI Consortium prospective registry from 03/2003 to 01/2020. Abbreviations: LAD: Left anterior descending; LVEF: Left ventricular ejection fraction; PCI: Percutaneous coronary intervention.
| All, N | 14,911 |
|---|---|
| Age (years), mean ± SD | 62.3 ± 13.6 |
| Age > 75 years, N (%) | 2822 (19) |
| Female sex, N (%) | 4360 (29) |
| Medical history, N (%) | |
| Coronary artery disease | 3683 (28) |
| Hypertension | 8237 (61) |
| Hyperlipidemia | 7328 (55) |
| Diabetes mellitus | 2939 (22) |
| Smoking history | 7966 (60) |
| LAD, as the culprit, N (%) | 4670 (34) |
| Severely reduced LVEF at presentation (<35%), N (%) | 1894 (15) |
| Cardiac arrest and/or cardiogenic shock, N (%) | 1905 (13) |
| Cardiac arrest, N (%) | 1314 (10) |
| Cardiogenic shock prior to primary PCI, N (%) | 1140 (8) |
4. Discussion
The MSC is a unique collaboration of 4 well-established Midwestern STEMI care systems, which forms a comprehensive STEMI registry involving nearly 15,000 consecutive STEMI patients without any exclusionary criteria. The MSC is a dynamic platform holding regular meetings, whereby consortium members exchange ideas to provide a guidance to conduct clinical research studies related to STEMI care.
The comprehensive MSC database could be queried in real-time to answer critical questions such as temporal trends in cardiovascular risk factors, clinical outcomes, and impact of novel therapies in STEMI care. For instance, examination of this database has revealed significant changes in STEMI population over the past 15 years such as increases in age at presentation and rates of diabetes mellitus, CA, and CS, demonstrating that in-hospital mortality rates have significantly increased during the study period [23].
Similarly, the MSC database may be used to assess the eligibility criteria on participant enrollment for clinical trials. In that respect, we recently performed an analysis by using the enrollment criteria of the “DTU-STEMI” trial (Door-To-Unload in STEMI) which proposes a novel interventional approach to unload left ventricle by Impella for 30-min prior to primary PCI in patients with anterior STEMI [24]. In our sub-cohort, overall in-hospital and long-term (up to 5-year) mortality rates were extremely low. More important, delay to reperfusion by 30-min significantly increased 1-year mortality rates by 38%. The findings were presented at ACC 2020 Scientific Sessions [25].
The MSC database has been particularly useful during the COVID-19 pandemic to verify anecdotal observations of a decline in STEMI activations across the globe [26]. In this regard, the MSC recently collaborated with the Society for Cardiovascular Angiography and Interventions (SCAI) and the Canadian Association of Interventional Cardiology (CAIC) to develop the North American Covid-19 ST-Segment Elevation Myocardial Infarction (NACMI) registry with the intention to assess clinical characteristics, treatment strategies, and in-hospital and 1-year clinical outcomes of STEMI patients with suspected or confirmed COVID-19 [27,28].
A major goal of the MSC is to improve quality of care and clinical outcomes in STEMI challenges such as CA and/or CS, major influences on STEMI mortality [29,30]. Recent subgroup analysis of AHA Mission: Lifeline STEMI Accelerator projects reported a modest improvement in time to reperfusion among out-of-hospital CA or CS complicating STEMI patients from 2012 to 2014 without a significant change in in-hospital mortality rates [31,32]. In-hospital mortality rates were doubled when CA and CS were both present as reported in MHIF Level 1 study and continues to be a risk for mortality at 5-year follow-up [33]. In order to improve time to reperfusion as well as survival in CA and/or CS complicating STEMI patients, it's essential to have an accurate and comprehensive database [34,35]. However, STEMI patients complicated by CA and/or CS are often excluded from observational registries due to expected delays in reperfusion. In contrast, the MSC plays a pivotal role by including all consecutive CA and/or CS complicating STEMI patients with a detailed data source including but not limited to status of tracheal intubation, therapeutic hypothermia, inotropic agents, Swan-Ganz catheterization, IABP, Impella, and ECMO. Furthermore, the role of novel intravenous antiplatelet agent, cangrelor, deserves further investigation in STEMI patients complicated by CA and/or CS, whom unable to tolerate oral agents. In that manner, the MSC plans to perform a matched-cohort analysis to compare the safety and efficacy of cangrelor on high-risk STEMI patients.
5. Conclusion
“Regionalization” is a milestone in STEMI care which has led to highly coordinated and standardized care processes resulting in timely coronary reperfusion among a broad spectrum of STEMI patients. The MSC advances this concept further to provide more valuable insight for better understanding of challenges in STEMI care by creating a comprehensive, multicenter, and prospective database inclusive of all consecutive STEMI patients without any exclusionary criteria. Withal, the MSC seeks to collaborate with national societies and industry partners to identify the opportunities of improving STEMI outcomes especially among the high-risk subsets such as CA and/or CS.
The Midwest STEMI Consortium data collection forms and definitions.
Funding
The American College of Cardiology’s Accreditation Services.
Declaration of competing interest
None.
References
- 1.Vogel B., Claessen B.E., Arnold S.V., Chan D., Cohen D.J., Giannitsis E. ST-segment elevation myocardial infarction. Nat Rev Dis Primers. 2019;5:39. doi: 10.1038/s41572-019-0090-3. [DOI] [PubMed] [Google Scholar]
- 2.Antman E.M. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52:1216–1221. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 3.Henry T.D. From concept to reality: a decade of progress in regional ST-elevation myocardial infarction systems. Circulation. 2012;126:166–168. doi: 10.1161/CIRCULATIONAHA.112.114140. [DOI] [PubMed] [Google Scholar]
- 4.CathPCI Registry https://cvquality.acc.org/NCDR-Home/registries/hospital-registries/cathpci-registry
- 5.Chest Pain MI Registry https://cvquality.acc.org/NCDR-Home/registries/hospital-registries/chest-pain-mi-registry
- 6.Outcome Measures CMS. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures
- 7.HCUP-US NIS Overview https://www.hcup-us.ahrq.gov/nisoverview.jsp
- 8.Bates Eric R., M. D., Alice K., Jacobs M. Time to treatment in patients with STEMI. N Engl J Med. 2013;369:889–892. doi: 10.1056/NEJMp2009027. [DOI] [PubMed] [Google Scholar]
- 9.Fordyce C.B., Henry T.D., Granger C.B. Implementation of regional ST-segment elevation myocardial infarction systems of care: successes and challenges. Interv Cardiol Clin. 2016;5:415–425. doi: 10.1016/j.iccl.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Henry T.D., Unger B.T., Sharkey S.W., Lips D.L., Pedersen W.R., Madison J.D. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. Am Heart J. 2005;150:373–384. doi: 10.1016/j.ahj.2005.01.059. [DOI] [PubMed] [Google Scholar]
- 11.Henry T.D., Sharkey S.W., Burke M.N., Chavez I.J., Graham K.J., Henry C.R. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 12.Aguirre F.V., Varghese J.J., Kelley M.P., Lam W., Lucore C.L., Gill J.B. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: the Stat Heart Program. Circulation. 2008;117:1145–1152. doi: 10.1161/CIRCULATIONAHA.107.728519. [DOI] [PubMed] [Google Scholar]
- 13.Smith L.G., Duval S., Tannenbaum M.A., Brown S.J., Poulose A.K., Iannone L.A. Are the results of a regional ST-elevation myocardial infarction system reproducible? Am J Cardiol. 2012;109:1582–1588. doi: 10.1016/j.amjcard.2012.01.382. [DOI] [PubMed] [Google Scholar]
- 14.Jollis J.G., Al-Khalidi H.R., Roettig M.L., Berger P.B., Corbett C.C., Dauerman H.L. Regional systems of care demonstration project: american heart association mission: lifeline STEMI systems accelerator. Circulation. 2016;134:365–374. doi: 10.1161/CIRCULATIONAHA.115.019474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jollis J.G., Al-Khalidi H.R., Roettig M.L., Berger P.B., Corbett C.C., Doerfler S.M. Impact of regionalization of ST-segment-elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: mission: lifeline accelerator. Circulation. 2018;137:376–387. doi: 10.1161/CIRCULATIONAHA.117.032446. [DOI] [PubMed] [Google Scholar]
- 16.Larson D.M., Duval S., Sharkey S.W., Garberich R.F., Madison J.D., Stokman P.J. Safety and efficacy of a pharmaco-invasive reperfusion strategy in rural ST-elevation myocardial infarction patients with expected delays due to long-distance transfers. Eur Heart J. 2012;33:1232–1240. doi: 10.1093/eurheartj/ehr427. [DOI] [PubMed] [Google Scholar]
- 17.Mooney M.R., Unger B.T., Boland L.L., Burke N, Kebed K.Y., Graham K.J. Therapeutic hypothermia after out-of-hospital cardiac arrest: evaluation of a regional system to increase access to cooling. Circulation. 2011;124:206–214. doi: 10.1161/CIRCULATIONAHA.110.986257. [DOI] [PubMed] [Google Scholar]
- 18.Larson D.M., Menssen K.M., Sharkey S.W., Duval S., Schwartz R.S., Harris J. “False-positive” cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA. 2007;298:2754–2760. doi: 10.1001/jama.298.23.2754. https://jamanetwork.com/ [DOI] [PubMed] [Google Scholar]
- 19.Miedema M.D., Newell M.C., Duval S., Garberich R.F., Handran C.B., Larson D.M. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation. 2011;124:1636–1644. doi: 10.1161/CIRCULATIONAHA.111.033118. [DOI] [PubMed] [Google Scholar]
- 20.Graham K.J., Strauss C.E., Boland L.L., Mooney M.R., Harris K.M., Unger B.t. Has the time come for a national cardiovascular emergency care system? Circulation. 2012;125:2035–2044. doi: 10.1161/CIRCULATIONAHA.111.084509. [DOI] [PubMed] [Google Scholar]
- 21.Garberich R.F., Traverse J.H., Claussen M.T. ST-elevation myocardial infarction diagnosed after hospital admission. Circulation. 2014;129:1225–1232. doi: 10.1161/CIRCULATIONAHA.113.005568. [DOI] [PubMed] [Google Scholar]
- 22.Pera V.K., Larson D.M., Sharkey S.W., Garberich R.F., Solie C.J., Wang Y.L. New or presumed new left bundle branch block in patients with suspected ST-elevation myocardial infarction. Eur Hear J Acute Cardiovasc Care. 2018;7:208–217. doi: 10.1177/2048872617691508. [DOI] [PubMed] [Google Scholar]
- 23.Garcia S., Schmidt C.W., Garberich R., Henry T.D., Bradley S.M., Brilakis E.S. Temporal changes in patient characteristics and outcomes in ST-segment elevation myocardial infarction 2003-2018. Catheter Cardiovasc Interv. April 2020 doi: 10.1002/ccd.28901. [DOI] [PubMed] [Google Scholar]
- 24.Kapur N.K., Alkhouli M.A., DeMartini T.J., Faraz H., George Z.H, Goodwin M.J. Unloading the left ventricle before reperfusion in patients with anterior ST-segment-elevation myocardial infarction. Circulation. 2019;139:337–346. doi: 10.1161/CIRCULATIONAHA.118.038269. [DOI] [PubMed] [Google Scholar]
- 25.Henry T.D., Garcia S., Schmidt C., Garberich R., Aguirre F.V., Tannenbaum M. Clinical outcomes of anterior STEMI patients eligible for the door to unload trial. J Am Coll Cardiol. 2020;75:25. doi: 10.1016/S0735-1097(20)30652-5. [DOI] [Google Scholar]
- 26.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.COVID-19 Resources - SCAI http://www.scai.org/covid-19-resources
- 28.Dehghani P., Davidson L.J., Grines C.L., Nayak K., Saw J., Kaul P. North American COVID-19 ST-segment elevation myocardial infarction (NACMI) registry: rationale, design, and implications. Am Heart J. 2020 May 16;227:11–18. doi: 10.1016/j.ahj.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krishnan U., Brejt J.A., Schulman-Marcus J., Swaminathan R.V., Feldman D.N., Goyal P. Temporal trends in the clinical acuity of patients with ST-segment elevation myocardial infarction. Am J Med. 2018;131:100.e9–100.e20. doi: 10.1016/j.amjmed.2017.06.040. [DOI] [PubMed] [Google Scholar]
- 30.Granger C.B., Bates E.R., Jollis J.G., Antman E.M., Nichol G., O'Connor R.E. Improving care of STEMI in the United States 2008 to 2012. J Am Heart Assoc. 2019;8 doi: 10.1161/jaha.118.008096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kragholm K., Lu D., Chiswell K., Al-Khalidi H.R., Roettig M.L., Roe M. Improvement in care and outcomes for emergency medical service-transported patients with ST-elevation myocardial infarction (STEMI) with and without prehospital cardiac arrest: a mission: lifeline STEMI accelerator study. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.005717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kochar A., Al-Khalidi H.R., Hansen S.M., Shavadia J.S., Roettig M.L., Fordyce C.B. Delays in primary percutaneous coronary intervention in ST-segment elevation myocardial infarction patients presenting with cardiogenic shock. JACC Cardiovasc Interv. 2018;11:1824–1833. doi: 10.1016/j.jcin.2018.06.030. [DOI] [PubMed] [Google Scholar]
- 33.Omer M.A., Tyler J.M., Henry T.D., Garberich R., Sharkey S.W., Schmidt C.W. Comparison of clinical characteristics and outcomes of ST-segment elevation myocardial infarction patients with cardiogenic shock and cardiac arrest. JACC Cardiovasc Interv. 2020 May 25;13:1211–1219. doi: 10.1016/j.jcin.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 34.Valle J.A., Ho P.M. Excluding the elephant in the room: cardiac arrest. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.011381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jentzer J.C., van Diepen S., Henry T.D. Understanding how cardiac arrest complicates the analysis of clinical trials of cardiogenic shock. Circ Cardiovasc Qual Outcomes. 2020 doi: 10.1161/CIRCOUTCOMES.120.006692. [In Press] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Midwest STEMI Consortium data collection forms and definitions.