Abstract
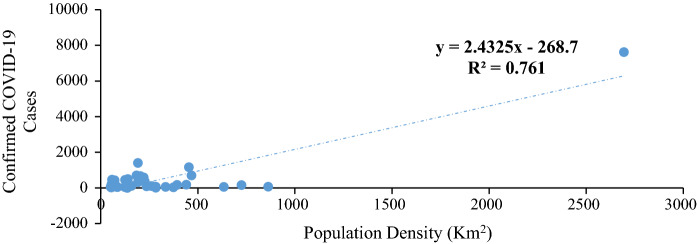
An understanding of the COVID-19 spread is growing around the world, yet little is known of Africa. This paper explores the time–space geographies of COVID-19 infection focusing on Africa and Nigeria especially. We appraise the global-to-local situation of confirmed cases, deaths and recoveries as well as measures engaged in response to the pandemic. Findings reveal that South Africa accounts for 40% of the total confirmed cases in Africa, followed by Egypt (18%), Nigeria (6.8%), Ghana (4.6%) and Algeria (3.6). Our study shows a significant relationship between population density and COVID-19 cases in Nigeria (R2 = 0.76; y = 2.43x − 268.7). This expression suggests that high population densities catalyze the spread of COVID-19. While Nigeria has only recorded about 25,964 cases as at the time of writing, the country is struggling to match pressures from rising cases as a result of existing disparities in health care systems.
Keywords: COVID-19, Health care, Nigeria, Population densities, Time–space geographies
Introduction
The outbreak of the novel human Coronavirus, SARS-CoV2 (Severe Acute Respiratory Syndrome-Coronavirus 2) which is the causative agent of COVID-19 disease, was reported in December 2019, in Wuhan City, Hubei Province, China (Li et al. 2020). This virus belongs to a family of viruses identified as Coronaviruses which are known to infect vertebrates (Yadav and Saxena 2020). Being a zoonotic RNA virus, this pathogen has the potential to cause a global pandemic partly due to their unique proteins (enzyme) make-up and the plasticity of their genomes as previously noted (Jaimes et al. 2020). As an RNA virus, Coronaviruses can easily mutate thereby making it possible to jump from one species to the other as well as transmit from humans to humans (Woolhouse et al. 2014). In the case of SARS-CoV2, the virus has been shown to jump from bats to other mammals and then to humans (Sun et al. 2020; WHO 2020a; Woolhouse et al. 2014). It also possesses the capacity to spread from humans to humans since our actions as human beings create an enabling platform that aids the spread and infection of these viruses (Sanche et al. 2020).
Furthermore, studies have also shown that both symptomatic and asymptomatic infected persons are infectious and can transmit the virus to other humans (Sanche et al. 2020). The concept of super spreaders has also been described as another factor enhancing the transmission of the virus (Chen et al. 2020). Since the dynamics of this newly emerging virus keeps changing, it has been difficult to determine the basic reproductive number, R0, defined as the average number of secondary cases attributable to infection by an index case after the case is introduced into a susceptible population (Li et al. 2020; Sanche et al. 2020). As noted by Sanche et al. (2020), limitations such as data availability, unavailability of diagnostic reagents, surveillance challenges, improper case definitions as well as overwhelmed healthcare systems have confounded the estimation of R0 for SARS-CoV2.
By the end of February 2020, SARS-CoV2 had spread to several regions of the world causing morbidity and mortality. Initially, the World Health Organization declared the outbreak on the 30th of January, 2020, as a Public Health Emergency of international concern but later it was labeled as a pandemic on the 11th of March 2020. Within this period, most countries of the world including Nigeria had started recording cases of COVID-19 disease (Akande-Sholabi and Adebisi 2020; Amzat et al. 2020; Bowale et al. 2020; Ohia et al. 2020; Olapegba and Ayandele 2020). The pandemic has since then plunged the global economy and the entire means of production into an entirely new era of uncharted terrain going by the unpredictability of the outbreak and unavailability of data as to R0 of the infection.
The history of pandemics in Nigeria can be traced back to the early twentieth century. The Bubonic plague appeared at two different decades in colonial Lagos. The first outbreak of the devastating influenza was in October 1918. It was estimated that over fifteen thousand deaths were recorded in Lagos (NAI 1950). The impact of the pandemic reconfigured social, economic, political and administrative activities to a degree that the Native Courts and Schools were the first to be indefinitely closed (Davies 2014). Trade stagnated and it was almost impossible to access basic items such as food, drinks and other essential amenities. The second outbreak of the pandemic in the 1930s also brought about the need for more hands in the health care systems. This led to the establishment in 1939 of the first medical school in Nigeria, the Yaba Medical College (NAI 1950). At first, it trained medical assistants but was later upgraded to train assistant medical officers. By special arrangement between the Colonial Office and The Royal Colleges of Surgeons and Physicians of Great Britain, most of the assistant medical officers were granted Licentiate Diplomas, after a short exposure in Britain (Scott-Emuakpor 2010).
The situation between pandemics, health-care workers and facilities in the country since colonial times to date, as revealed by the COVID-19 outbreak in the country shows clearly the state of readiness and the level of improvement in health-care facilities in the country. The state of the health care system and the personnel are a reflection of the neglect of the sector by the government. In most global south countries such as Nigeria, the pandemic has exposed the weakened and total neglect of health facilities and medical infrastructures by the state (Ogunbekun et al. 1999). This is obvious considering the health-seeking behaviour of most elites and public servants in the country (see Cohen 2013; https://thisisafrica.me/politics-and-society/nigerias-president-buhari-medical-trips-signal-no-end-medical-tourism/; https://mg.co.za/article/2020-04-07-covid-19-grounds-nigerias-medical-tourists/). This study aims to examine the geography of the emergence of COVID-19 in Nigeria. To achieve the stated aim, the study reviewed the progression of COVID-19 from Wuhan in China to the rest of the world in three phases, geographies of health and environment in Nigeria including the political–ecological effects of the COVID-19 pandemic and finally the local responses and initiatives employed in meeting the challenges posed by the spread of the disease in Nigeria.
This paper draws largely from the general systems theory (Von Bertalanffy 1968) and the theory of relative social deprivation (Runciman et al. 1966). These conceptual prisms offer a deeper understanding of decades of systemic neglect of the Nigerian Health Care systems vis-à-vis the acute deprivation of the Nigerian masses by the political elites. The theories essentially illuminate the understanding of the state of modern basic social amenities for the vast neglected populace, the status-seeking elites especially political office holders and the lackadaisical posture of the Nigerian government towards the health sector in the country.
von Bertalanffy (1968) asserted in his book on general systems theory, that a system is a complex of interacting elements and that they are open to, and interact with their environments. In the context of a society, the systems theory lens sees the society as a structure, with several multi-complex sub-structures with dependent and interdependent intersections (Anderson 1998). In the context of this discourse, the state represents the system, while public institutions are the sub-systems, with the people depending on the efficacies of the two for a decent social existence. The theory further highlights the interdependence of the physical social services and infrastructure which the system should transmit to the sub-systems. Furthermore, from the social theory lens, the state of public health facilities and poorly funded medical services in Nigeria presents a situation where a preponderant of the population of a particular social formation are marginalized and deprived of essential and basic social amenities. Raza et al. (1983), posits that social deprivation is often consequences of complacent disposition of public representatives and political gladiators towards a neglected population. According to Igbozurike (1983) and Raza et al. (1983), social deprivation manifests in the society, when the physical and social welfare of the populace depreciates amidst available resources and opportunities. The major evidence of social deprivation could be the absence of modern medical and health centers, electricity, housing, public transportation, recreational facilities, water supply and social welfare institutions (Imhabehkai 2009). Social deprivation theory is deployed in this paper to depicting the role of government in the provision of effective medical and health care systems. The paper argues, based on this theory that Nigeria’s health sector has been deprived of enabling medical infrastructure, despite the enormous resources and opportunities, the medical conditions of the Nigerian people have remained virtually unaffected by the prevailing circumstances. The most dominant and common characteristics of the Nigerian health care system are weakened medical infrastructures, decaying social amenities and inequality in the distribution of social goods and services. Rather than addressing the state of health care systems in Nigeria, political office holders in the country embark on medical tourism to different parts of the world.
Method
Study design
Although the emphasis of this study is on the occurrence of COVID-19 within African countries, especially in Nigeria, the analysis however is classed into three (3) parts to cover the sequential ends of the pandemic. We rely entirely on the WHO report on the disease outbreak for the coverage of the maiden nCoV strain observed in China as the first part of the Initial Phase (I-a) of our analysis (WHO 2020a). Also, we consider the 24th February 2020 WHO update on “Middle East respiratory syndrome coronavirus (MERS-CoV)—The Kingdom of Saudi Arabia” in a brief analysis of the near-simultaneous occurrence of MERS-CoV strain observed in Saudi Arabia as the second part of the Initial Phase (I-b) of this study (see the WHO site at: https://www.who.int/csr/don/24-february-2020-mers-saudi-arabia/en/). While we take the 2nd Day of December 2019 as the first date of occurrence of nCoV recorded in Wuhan, the 4th Day of December 2019 was the first date of occurrence of MERS-CoV in eastern parts of Saudi Arabia thus effectively making duration of 50 days to the 20th Day of January 2020.
The Global Phase (II) of our analysis is considered as the post-China transmissions and outbreak across the world starting particularly from 21st Day of January 2020 when a man in his 30 s from Washington State who had traveled to Wuhan was diagnosed with the novel Coronavirus became the first confirmed case of COVID-19 recorded in the United States of America. This date serves the purpose of mark-point to differentiate the second classification of our analysis from the first phase and provide justification for time-step differentials, although, some neighbouring countries to China reported their first cases of COVID-19 on January 13 (Thailand) and on January 16 (Japan).
This period (II) is marked off by the global health emergency of international concern declaration by the World Health Organisation (WHO) on the 30th day of January 2020, making about 10 days from the beginning to the end of this phase. This period marked the spread of COVID-19 from the eastern hemisphere to the west especially Europe and North America. Since this is not the primary focus of the study, a brief analysis is done while considering the implications of this period and the spread of the virus to the rest of the world particularly Africa.
The African Phase (III) of our analysis covers the post-30th January 2020 declaration of a global health emergency of international concern. This was the period when the first cases of COVID-19 began to be successively recorded across Africa, specifically through infected human carriers who traveled into the continent from countries already experiencing the outbreak.
Sources of data
Secondary data was employed for this study. Data were extracted from the World Health Organization COVID-19 dashboard (https://covid19.who.int/) and Worldometer (https://www.worldometers.info/coronavirus/?) for the global scale while for Africa, the Center for Disease Control COVID-19 dashboard was used (https://africacdc.org/covid-19/#). For cases within Nigeria, the Nigerian Center for Disease Control, NCDC was used (https://covid19.ncdc.gov.ng/gis/) to account for local variation within the country.
Statistical analysis
A line of best fit was performed between population density and confirmed cases of COVID-19 in Nigeria. The equation is expressed as:
| 1 |
Results and discussion
Initial phase (I-a) starting point of the pandemic: China
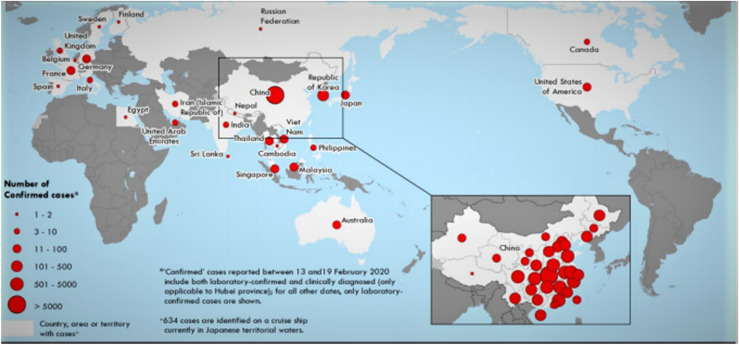
It has been recounted in several studies and reports that the Chinese authorities declared on January 7, 2020, that a new type of Coronavirus (novel Coronavirus, nCoV) or SARS-CoV-2 was isolated and as of 20th February 2020 (Fig. 1), a cumulative total of 75,465 COVID-19 cases were reported in China with 2114 deaths among the 55,924 laboratory-confirmed cases giving a crude fatality ratio of 3.8% (WHO 2020b; Sun et al. 2020). Furthermore, this mortality was observed to have been escalating with age, as the highest amount of death occurs amid people above the age of 80 years to give crude fatality rates as high as 21.9%. It was also observed that males (4.7%) had higher rates of infection compared to females (2.8%), while retirees and old self-employed people recorded 8.9%, the highest death rates in terms of occupation (WHO 2020b).
Fig. 1.
Countries, territories or areas with reported confirmed cases of COVID-19 as of 21 February 2020.
Source: WHO (World 2020a) (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200221-sitrep-32-covid-19.pdf)
However, it was staggering to note that patients with comorbidity had very high death rates as compared with those who had no comorbid conditions (1.4%) before their infection. Specifically, the burden of the disease indicated that the death rates varied among Cardiovascular Disease (13.2%), Diabetes (9.2%), Hypertension (8.4%), Chronic Respiratory Disease (8.0%), and Cancer (7.6%) with the temporal rate of disease progression from symptom onset to laboratory confirmation decreasing from between 8 and 18 days about early January to 3-7 days as at early February 2020 (WHO 2020b). These figures are important for the intervention in Africa, as they provide insights into how best to respond to the outbreak (Fig. 1).
The spatial spread of COVID-19 within China was particularly low as more than two-thirds of the occurrences revolved around the Hubei province from where the first outbreak started, while about half of the entire cases were reported in Wuhan alone (WHO 2020b). Although not much was published about the geographical nature of the epidemic within this phase, it is, however, clear that the distribution was contained around Wuhan, the location of onset, concentrically occurring in few neighbouring provinces. As at the time of writing, China has recorded 83,534 cases with over 4500 deaths. Within China, Hubei (68,135) province still has the highest number of confirmed followed by Guangdong (1641), Henan (1276), Zheijang (1269), Hunan (1019), etc.
Initial phase (I-b) simultaneous to the pandemic: Saudi Arabia
Whereas the whole world seems focused on the COVID-19 pandemic as having stemmed from the SARS-CoV-2 of which much has been documented, only a few observed that MERS-CoV was also simultaneously ravaging Saudi Arabia just as China was in focus. Humans are infected with MERS-CoV from direct or indirect contact with Dromedaries (https://www.who.int/csr/don/24-february-2020-mers-saudi-arabia/en/). According to reports from WHO, the onset of this silent respiratory epidemic was on the 4th of December, 2019 when a case was reported in Eastern parts of Saudi Arabia where a 65-year-old male reportedly showed symptoms. Eighteen (18) more patients of similar demographics were reported within the space of 25 days interval, among which about seven (7) more also died to make a total of 8 deaths in 19 cases within 25 days interval. Although, not many studies have emphasized this staggering 42.1% crude fatality rates within such a short period and limited spatial extent, the threat of this particular strain for Africa was not as anticipated as that of SARS-CoV-2 despite the huge religious tourism potentials of Saudi Arabia and the existence of Dromedaries in Africa especially north and south of the Sahara. A lesson to note from this, therefore, is the relevance of economic international passenger networks vis-à-vis religious tourism. Similarly, the fact that this strain has never been encountered in Africa, just as the strain of SARS-CoV-2 (before now) has made the scare less anticipated. However, even though virtually 80% of the recounted MERS-CoV cases have been in Saudi Arabia alone, about 2519 cases and 866 associated fatalities between 2012 and 31st January 2020 (https://www.who.int/csr/don/24-february-2020-mers-saudi-arabia/en/), makes it an important infection Africa must be wary of (Altamimi et al. 2020). According to WHO, several travel-related cases have already befallen Greece, Germany, France, Philippines, the United Kingdom, Malaysia, Egypt, Italy, the Netherlands, Turkey, South Korea, Algeria, Austria, China, and the United States (WHO 2019). To date, the major plague of MERS-CoV, after Saudi Arabia, happened in South Korea from May through July of 2015, with 186 stated cases and 39 deaths to make a 21% case fatality rate (Altamimi et al. 2020). It will, therefore, be instructive, for Africa to brace up to the challenge of a future possibility of a MERS-CoV outbreak.
Global phase (II) of the pandemic: USA, Europe and others
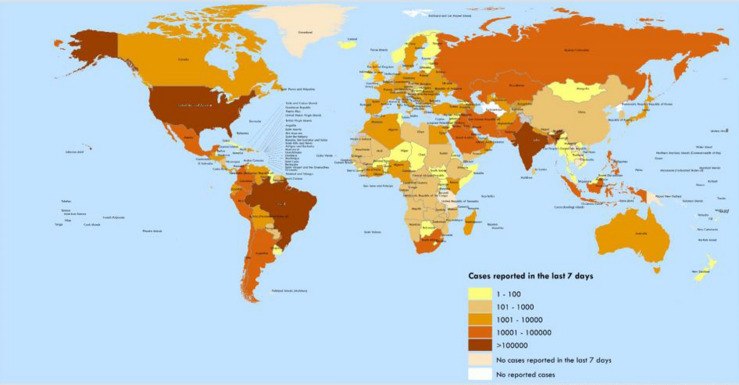
In terms of geographical distribution, it is pertinent to note that COVID-19 has exhaustively covered the world as we know it today with over 10million recorded cases and over 500,000 deaths at the time of this writing (Fig. 2). As many studies have shown, the rate of transmission and the route as well have aided the spread of the pandemic across more than 180 countries and regions of the world (Sun et al. 2020; Boulos and Geraghty 2020). While the spatial distribution all over the globe is actively being tracked using geographical skills and tools (Figs. 1 and 2), the alarming pace of the spread is not only staggering but scary, considering that the most developed countries have been deemed to have the utmost effective health systems, facilities and the most qualified health care personnel. The news and reports of the calamitous fatalities being disseminated to Africa through the media are quite staggering and calls for sober reflection (Gilbert et al. 2020; Kishamawe et al. 2019). That notwithstanding, the geographical implications of the current pandemic are helping to review many established knowledge on several fronts. Whereas China and the United States of America, USA, have huge trade relationships, the bilateral contests between them often obscure the closeness of the two world economic dominators. It is however noteworthy that it did not quite take more than 1 month for the USA to record the first case after China reported the epidemic to WHO (Fig. 1). This says much of the networks and interactions that have made the world a global village, it also casts aspersion on the gains of globalization (Saker et al. 2004). Without gainsaying, the current mode of COVID-19 spread suggests that truly globalization may be triggering intense volatile alterations in not only the biological but also social and economic state of global affairs while also altering the ecological landscapes in no small ways. All these contribute together as factors characterizing the burden of transmittable diseases albeit in dramatically unpredictable measures among human populations (FIRS 2017; IHME 2018; Rosenthal 2010; Salvi et al. 2018; Saker et al. 2004; WHO 2007).
Fig. 2.
Number of confirmed COVID-19 cases reported in the last seven days by country, territory or area, 4 July to 10 July.
Source: WHO (2020c) (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200710-covid-19-sitrep-172.pdf?sfvrsn=70724b90_2)
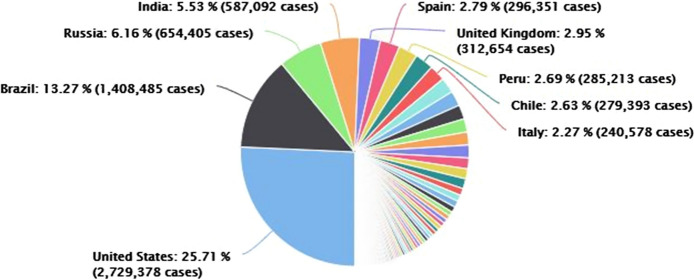
Although it is not within the scope of the current study to examine the global onsets of the pandemic at country levels, many useful lessons are emerging with the outbreak within this phase. It is useful to note that it took 4 days from the date of the singular first occurrence in the USA, for another lone case to be observed. In just 2 more days 3 cases were reported to make it 5 total cases within 6 days and then yet another 4 days for the next lone case reported. Then one more case each for the next two consecutive days before another 3 cases surfaced. However, it took another 19 days for 19 cases in a single day to occur within which some 5 staggered singular cases also occurred, and 3 days after, 18 cases in a day were reported. Within the next 6 days, 16 cases were reported after which 20 cases were reported in 1 day. The lesson is that by the 46th day after the first case was reported in the USA, the first fatality was recorded. From thence on, the figures started doubling astronomically and by the time of writing, the United States of America, USA sits at the top of the chart with over 2million reported cases followed by Brazil, with over a million reported cases and then Russia with about 600,000 reported cases (Fig. 3). The total number of deaths recorded between these three countries is over 200,000 deaths out of the total 514,638 as reported by WHO. This is by far greater than 10,197 deaths reported in Africa out of about 400,000 cases.
Fig. 3.
Global phase (II) of the pandemic.
Source: worldometer
In several other advanced economies with very high HDI, similar trends have been observed. For example, it took about 28 days of staggered 13 reported cases with no death until the 36th day by which a cumulative 115 cases had been reported in the United Kingdom. In Italy, it took 22 days for an added report after 3 cases were reported on the first date and the first 2 mortalities just 2 days after. This being the case in the most advanced health system leaves much to be desired in the African story. Numerous health workers across the developed world have been reported to have died due to infection with COVID-19, and dozens more have fallen ill, while the world is yet to find a cure.
Phase III: the African/Nigerian phase of the pandemic
The outbreak of the novel COVID-19 pandemic is perhaps the most important public health challenge that has confronted the global community in several decades. The scale and rapid spread of the virus across international boundaries has been largely unabated in both developed and developing countries. The far-reaching effect of this pandemic among nations has so far spanned every aspect of any society with social, economic, political disruption to the livelihood of individuals and nations. Nations across the globe are therefore challenged to implement measures to help limit widespread transmission and eventually stop the wave of transmission of the virus.
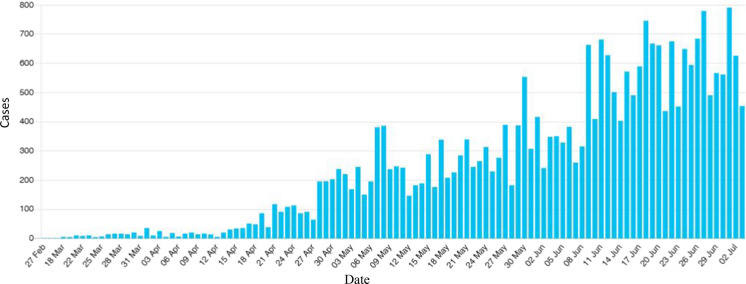
Since the COVID-19 virus made its landfall on the 14th of February in Egypt, the poorly equipped health care system among member states has been of utmost concern in the effort to defeat the virus. Almost all the African countries infected as at 30th of March had a two-week window of the index case in the continent (Fig. 4). The importance of basic preventative measures by individuals, communities and nations remains the most powerful tool to prevent the spread of diseases particularly the dreaded COVID-19. The response of African countries to the outbreak has been classified into two, active and passive preparation. The evidence of active preparations in the African continent among member states is associated with the support from the World Health Organization (WHO). These include the supply of COVID-19 testing kits, training of health workers to strengthening/coordinating surveillance, measures for quarantine, clinical care/treatment, data modelling and diagnostics. About Forty-seven countries in Africa were able to test for the COVID-19 after this intervention. Before the outbreak, there were only two countries that could test for the virus.
Fig. 4.
Cases by date since the first record of COVID-19 in Africa.
Source: http://covid-19-africa.sen.ovh/
On the other hand, the passive preparations which are measures put in place in reaction to the presence of the virus among member states as at 30th of March 2020. As of the last day of March, all African nations besides Burundi, Malawi, and Zambia had completely severed international transport linkage shutting down both domestic and international airport services. Similarly, most had in place a complete border closure with neighboring countries to stop the flow of imported cases into their country. Most countries however exempted from the blockade the passage of vital supplies such as food, medical equipment and pharmaceutical products. Nearly all African countries that have reported the presence of the virus are currently enforcing a partial lockdown in every part of the country. This partial lockdown restricts all forms of motorized movements while a few others have imposed a dusk to dawn curfew across the country. All markets, educational institutions as well as social and religious engagements have been prohibited. The gathering of 10 or more persons in a single environment has been banned by most governments. Massive information drive promoting social distancing, personal hygiene is consistently being broadcast as part of the awareness campaign to educate and sensitize citizens on mitigating actions to slow the spread of the virus.
As at the time of writing, Africa has reported a total of 383,800 COVID-19 cases with over 9000 deaths giving a Case Fatality Rate (CFR) of about 2.3% (Table 1). The regional distribution of the cases reported as well as the number of deaths, the number of those who have recovered from the disease and the percentage of deaths to the number of cases is presented in Table 1. While the southern region has reported the highest number of cases (143,600), about one-third (37.41%) of all the cases reported in the continent, with the highest number of deaths (4100), it is important to note that the region also has the highest number of individuals who have recovered (71,300).
Table 1.
Confirmed COVID-19 cases reported in Africa by regions.
Source: Africa CDC
| Region | No. of cases | No. of deaths | No. of recovered | Case fatality rate (%) |
|---|---|---|---|---|
| Central region | 33,200 | 725 | 16,300 | 2.2 |
| Eastern region | 36,200 | 1000 | 17,000 | 2.7 |
| Western region | 74,000 | 1300 | 40,500 | 1.8 |
| Northern region | 96,800 | 2000 | 38,300 | 2.1 |
| Southern region | 143,600 | 4100 | 71,300 | 2.9 |
| Total | 383,800 | 9125 | 183,400 | 2.34 |
All countries in Africa have reported cases of the Coronavirus, the last being Lesotho. The first five countries leading the way based on reported cases across the continent are South Africa with 151,209 cases to make 40% of total cases reported in Africa, Egypt with 69,311 cases (18%), Nigeria with 25,964 cases (6.8%), Ghana with 17,741 cases (4.6%) and Algeria with 13,907 cases (3.6%). It is also pertinent to note that the rate of testing across most African countries is still low especially in Sub-Saharan Africa. Therefore, unknown cases are expected to be more than those reported. However, the fatality rate still places the West African region as the lowest across the continent. Even though Nigeria ranks third in terms of reported cases, the rate of testing is still very low compared to some other countries. Part of this could be due to the challenge being faced as regards testing kits, facilities, over-stretched health and medical workers and unavailability of specific demographic data needed for contact tracing.
The Nigerian health care system
The post-colonial nature of the health care system in Nigeria has been evolutionary (Scott-Emuakpor 2010). The evolutionary changes are not discussed here, however, the focus of this sub-section is to point out the major landmarks in the health care system of the country. The first major landmark in the health care system of the country came during the Fourth National Development Plan (1981-1985). The policy statement contained in this plan called for the implementation of the Basic Health Services Scheme (BHSS), provides for the establishment of three levels of health care facilities; Comprehensive Health Centers (CHC) to serve communities of more than 20,000 people; Primary Health Centers (PHC) to serve communities of 5000 to 20,000 persons; and Health Clinics (HC) to serve 2000 to 5000 persons (Scott-Emuakpor 2010).
This plan to date was never achieved and the goal remained on paper. Another landmark worth mentioning is the Health Insurance Scheme under the President Olusegun Obasanjo Regime. In May 1999, the Federal Government of Nigeria created the National Health Insurance Scheme. In his second tenure, President Olusegun Obasanjo, in 2004, enabled more legislative powers to the scheme by making further positive amendments to the original 1999 legislative act. This scheme has achieved a lot in the country and has improved the health-seeking behavior of the middle and low-income class. However, in a report in the National Dailies (Vanguard Newspaper, 5th July 2017) it was gathered that a sum of N351 billion (about $905,806,430) had been expended on health management organizations (HMOs) so far without commensurate result. With an annual population growth rate of about 2% as of 2011 (UN, 2012) and a life expectancy of 52 years with an overwhelming population density of 173.94 persons per km2, the demographic characteristics of the country are not looking good. The health indicators across the country are very worrisome; the total number of physicians in the country is under 200,000 and the total health workers are under 500,000 as of 2008 (https://data.humdata.org/dataset/who-data-for-nigeria). A country with about 200 million people can only boast of 0.5 hospital beds per thousand people, and 0.38 physicians per a thousand people (www.data.worldbank.org/indicator). Despite billions of dollars spent annually, the health sector, like any other sector in Nigeria is confronted with myriads of problems chief of which is limited funding, inadequate structures and personnel despite billions of dollars spent annually.
Presently, Nigeria operates a three-tiered health care system, comprising of tertiary health care (University Teaching Hospitals and Federal Medical Centres), secondary health care (General Hospitals, under the State Government) and primary health care under the Local Governments. The primary health centres are largely not functioning at an optimal level since they are mostly located in rural and peri-urban areas, only a few of them are still functioning optimally all over the country. They are to serve as the first point of call for most health-seeking persons, however, because of inadequate facilities and personnel, the secondary and tertiary health care provides this first-order service. Added to this fact is the almost annual industrial action of health workers based on inadequate service and low manpower. The middle- and low-income earners form a large fraction of the population who struggle to access the available health facilities in the country. The difficulty in accessing basic health facilities has resulted in self-medication and other unforeseen illnesses. However, the high-income earners, the elites and political office holders engage in medical tourism.
Elites and medical tourism in Nigeria
Medical tourism has been defined (Buzinde and Yarnal 2012a, b p. 783) as
a form of niche tourism, links leisure travel, the act of seeking form, pleasure, relaxation and bodily escape from the stresses and strains of daily life, with a purposeful escape to medical interventions, such as cardiac surgery, stem cell infections, organ and bone marrow transplants, body enhancements and dental care.
The basic idea about medical tourism is that certain people leave their country of origin to another country (destination) to access health care facilities based on different pull and push factors. Medical tourism though based on a market system of autonomy, independence and self-sufficiency (Bolton and Skountridaki 2017) has also been described as an elitist affair (Connell 2013), a situation in Nigeria where political office holders use taxpayers’ money to access health care facilities outside the shores of the country. This has been the post-colonial experience in the country where political office holders visit various health care providers across the globe for medical care and aid at the expense of improving state-owned facilities within the country. In 2005, the wife of a president in the country had to visit Spain for cosmetic surgery (https://mg.co.za/article/2020-04-07-covid-19-grounds-nigerias-medical-tourists/). President Musa Yar’Adua, during his tenure as the President of the country, traveled to Saudi Arabia several times as a sitting president for medical treatment. President Buhari, the current president of the country, has been out of the country several times to various places to seek medical attention to his health challenges (https://thisisafrica.me/politics-and-society/nigerias-president-buhari-medical-trips-signal-no-end-medical-tourism/). Asides, from those listed above, the same pattern can be said of other major political office holders in the country be it the National Assembly Members or the Governors. These set of political office holders constantly bleed the economy through capital accumulation at the expense of the citizens. Yet, they pay lip service to health reforms and directly or indirectly seek a liberal approach to the health care operations in the country. This approach has negative consequences as regards basic access to health care. The legal framings of access to basic health care are beyond the scope of this study, however, as stated in the constitution (Section 14(2)(b)) that:
the security and welfare of the people shall be the primary purpose of government
This section suggests that the functioning and the well-being of the people is the responsibility of the government. This is further echoed by Nnamuchi (2008 p. 8) that:
ensuring the availability of health care for the population is an essential obligation of government and this can only be discharged by providing adequate health and other social measures.
Therefore the patronage of commodified health-care by political office holders in the country leaves the health care system in Nigeria in a perpetual state of derelict and it has opened the door for exclusion and injustice (Bolton and Skountridaki 2017). The state has failed to fulfill her role in security and welfare and has lost control as an arbiter between production and labour. Post-colonial picture in terms of health care and infrastructures portrays a fragile health care system struggling to survive despite appalling health indicators (Nnamuchi 2008). The Nigerian government had budgeted a paltry sum of N440 billion (4.16%) for the health sector for the 2020 budget, a far cry from the 15% budgetary allocation agreed by African leaders in the Abuja Declaration of 2001 (https://africanarguments.org/2020/04/27/19-years-africa-15-health-abuja-declaration/). The Campaign for Democratic and Workers’ Right (CDWR) is demanding that Nigeria should spend 5 percent of its gross domestic product (GDP) on health as recommended by the World Health Organization (WHO) to revamp the healthcare infrastructure and employ adequate well-trained medical practitioners (WHO 2017). Given that the system, here referred to as the state, has failed over the years to respond to the complex social-medical exigencies of sub-systems, here, the health care, the unprecedented emergence of COVID-19 further shows the anomaly in the dependent relationship between the system and sub-system.
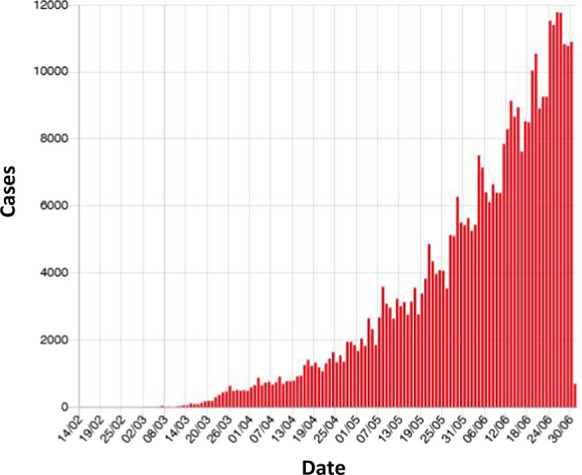
The COVID-19 experience
While Nigeria has only recorded about 25,964 cases as at the time of writing (www.ncdc.gov.ng), 42.2% of this number of cases have recovered and discharged from various isolation centres with about 600 confirmed fatalities giving a 2.3% fatality ratio. As shown in Fig. 5, there is a sustained rise in the number of confirmed cases in Nigeria.
Fig. 5.
COVID-19 progression by date in Nigeria.
Source: NCDC
The spatial distribution of the reported confirmed cases in Nigeria as shown in Fig. 6 is skewed towards Lagos (the commercial headquarters) having about 10,000 confirmed cases and a fatality ratio of 1.2%, followed at a clear distance by the Federal Capital Territory, Abuja (the administrative headquarters) with 2080 confirmed cases and a fatality ratio of 1.68%, then Oyo state with 1451 confirmed cases and a fatality ratio of 0.96%, Edo state with 1266 confirmed cases and a fatality ratio of 3.71%, Delta state with 1,1,65 confirmed cases and a fatality ratio of 2.15%, Rivers state with 1114 confirmed cases and a fatality ratio of 3.5% (https://covid19.ncdc.gov.ng/gis/). The remaining states in Nigeria record below a thousand confirmed cases while Cross-River is yet to record any known case of the virus as at the time of writing.
Fig. 6.
COVID-19 progression by states in Nigeria.
Source: NCDC
Studies have shown that population density among other factors enhances the spread of COVID-19 (Rocklöv and Sjödin 2020; Schuchat et al. 2020). In this study, our results shows a significant relationship between population density and COVID-19 (R2 = 0.76; y = 2.43x − 268.7). This expression suggests that high population densities catalyze the spread of COVID-19 (Fig. 5). This is instructive of the reproduction number (Ro) of the virus where Ro is an indication of the transmissibility representing the average number of new infections generated by an infectious person in a naïve population (Fig. 7).
Fig. 7.
Confirmed COVID-19 cases and population density across Nigeria
In the throes of the global pandemic, the existing disparities in the country and her health system was largely exposed. Nigerian ruling elites alongside other citizens of the country have had to cope with the weakened health infrastructures in Nigeria. With the lockdown measure being enforced globally, there was a restriction on the movement of people within and outside the country. The infection rate since the record of the index case in Nigeria places more of the elites as the first victims of the disease based on their travel history. As at the time of writing, some political office holders have had to be admitted to hospitals within the country owing to the lockdown of borders and airports while some passed away. Specifically, the Chief of Staff to the President (https://www.aljazeera.com/news/2020/04/nigerian-president-top-aide-dies-coronavirus-presidency-200418053325016.html), a sitting member of the Senate, a certain Chief Justice and immediate past Governor of a state in Nigeria to mention just a few (https://50minds.com/nigerian-governors-jittery-as-two-state-governors-test-positive-to-covid19-this-week/). Unfortunately, the weakened health systems within the country could not adequately match pressures from rising cases in the country (Fig. 5). It would be expedient for the government and the political elites who have siphoned the wealth of the nation at the expense of the health sector and other public sectors to rise to the task at hand.
The response of Nigeria to the COVID-19 outbreak is worth mentioning judging from the relatively slow increase in the confirmed cases despite the high population densities in most urban centers. While the government has shut all land borders like several other countries, the closure of all airports has drastically limited mobility including local flights. Perhaps the most striking of these measures is the lockdown in place since March 30 in Lagos State, neighboring Ogun State, and Abuja which was extended for another 14 days, preventing many Nigerians working in informal sectors from traveling to work or conducting their business. This new trend of working from home has its implication on the economy of the country and most especially in the private sectors but it was a welcome decision. The Nigerian government also made attempts to cater for the most vulnerable in the society by distributing cash and food items to over 3million households in the country (https://iclg.com/briefing/11746-covid-19-additional-palliatives-issued-by-the-federal-government-of-nigeria). However, it is not clear how many of the 11,045,537 people from 2,644,493 households included in the National Social Register were accommodated in the exercise. The government also announced that 77,000 metric tons of food were distributed to vulnerable households affected by the lockdown in Lagos, Ogun, and Abuja, however, little is known of the modalities for distribution. The Central Bank of Nigeria also announced a 50 billion Naira (US$ 128.5 million) credit facility aimed at supporting households as well as micro, small and medium enterprises affected by the COVID-19 pandemic. Furthermore, the House of Representatives passed the Emergency Economic Stimulus bill, to provide a 50% tax rebate for employers and business owners who will not make staff cuts in 2020 (https://iclg.com/briefing/11493-nigerian-emergency-economic-stimulus-bill-all-you-need-to-know). To further support the government, various donations from organizations, religious bodies, celebrities and several Nigerians have contributed to the fight against the pandemic since the first case was recorded in the country (https://www.bloomberg.com/news/articles/2020-03-26/access-bank-dangote-lead-nigeria-charge-against-covid-19). The government also plan to create a 500 billion naira ($1.39 billion) Coronavirus fund to strengthen its healthcare infrastructure to tackle COVID-19.
Conclusion
This paper explored the geographies of health in Nigeria within the framework of the onset and responses to the COVID-19 outbreak starting from its origins in China, to the USA and Europe and then Africa. The health environment in Nigeria showed the weak capacity before the disease outbreak with predominantly political exclusions which has largely seen the elite maintaining privileged standards beyond the reach of the general populace. Before the pandemic, the Nigerian government had been contending with weak recovery from the 2014 oil price shock and Gross Domestic Product lowering growth. These among other pressures worsen the impact of the COVID-19 outbreak limiting the capacity to confront the crisis. However, unlike several western countries and some African countries, Nigeria has fared well with a relatively lower spread of the Coronavirus and a much more reduced fatality.
Furthermore, the COVID-19 contagion is a wake-up call for Nigerian policymakers to improve the health system for citizens to benefit and reduce the elites’ reliance on the consumption of instantaneous consumers’ activities, medical tourism. The pandemic has also allowed the country to leverage on the concerted private sector and international support in meeting the demand for medical supplies and equipment.
Finally, the integrated multi-sector response in Nigeria to the pandemic includes the health, finance, and food supply especially to cater for the poor has helped significantly and ensured Nigeria escapes the pandemic trap in good time. The political and legal geographies of these responses to the Coronavirus pandemic are expected to ensure social innovation and the resultant actions will have a long-lasting impact on Nigeria.
Acknowledgements
We thank the editor and the reviewers of the manuscript. Also, the author thanks individuals and international organizations for freely providing data access for this research.
Funding
No funding was received for this research.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study does not require ethical approval as no human participant or animal subject was involved.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- African Arguments. (2020). Retrieved April 7, 2020, from https://africanarguments.org/2020/04/27/19-years-africa-15-health-abuja-declaration/.
- Akande-Sholabi W, Adebisi YA. The impact of COVID-19 pandemic on medicine security in Africa: Nigeria as a case study. PAMJ. 2020 doi: 10.11604/PAMJ.SUPP.2020.35.2.23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aljazeera. (2020). Retrieved April 7, 2020, from https://www.aljazeera.com/news/2020/04/nigerian-president-top-aide-dies-coronavirus-presidency-200418053325016.html.
- Altamimi A, Abu-Saris R, El-Metwally A, Alaifan T, Alamri A. Demographic variations of MERS-CoV infection among suspected and confirmed cases: An epidemiological analysis of laboratory-based data from Riyadh Regional Laboratory. BioMed Research International. 2020 doi: 10.1155/2020/9629747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amzat J, Aminu K, Kolo VI, Akinyele AA, Ogundairo JA, Danjibo CM. Coronavirus outbreak in Nigeria: Burden and socio-medical response during the first 100 days. International Journal of Infectious Diseases : IJID: Official Publication of the International Society for Infectious Diseases. 2020 doi: 10.1016/j.ijid.2020.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson P. The importance of theories in health care. British Medical Journal (BMJ) 1998;317(7164):1007–1010. doi: 10.1136/bmj.317.7164.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloomberg. (2020). Retrieved April 7, 2020, from https://www.bloomberg.com/news/articles/2020-03-26/access-bank-dangote-lead-nigeria-charge-against-covid-19.
- Bolton S, Skountridaki L. The medical tourist and a political economy of care. Antipode. 2017;49(2):499–516. doi: 10.1111/anti.12273. [DOI] [Google Scholar]
- Boulos MNK, Geraghty EM. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against. International Journal of Health Geographics. 2020;19(8):1–12. doi: 10.1186/s12942-020-00202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowale A, Abayomi A, Idris J, Omilabu S, Abdus-Salam I, Adebayo B, Osibogun A. Clinical presentation, case management and outcomes for the first 32 COVID-19 patients in Nigeria. Pan African Medical Journal. 2020;35(2):24. doi: 10.11604/PAMJ.SUPP.2020.35.2.23262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzinde CN, Yarnal C. Therapeutic landscapes and postcolonial theory: A theoretical approach to medical tourism. Social Science and Medicine. 2012;74(5):783–787. doi: 10.1016/j.socscimed.2011.11.016. [DOI] [PubMed] [Google Scholar]
- Cohen MA. Giving to developing countries: Controversies and paradoxes of international aid. Social Research: An International Quarterly. 2013;80(2):591–606. [Google Scholar]
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell J. Contemporary medical tourism: Conceptualisation, culture and commodification. Tourism Management. 2013;34:1–13. doi: 10.1016/j.tourman.2012.05.009. [DOI] [Google Scholar]
- Davies L. Urban renewal and associated problems in Lagos, 1924–1990. Lagos Historical Review. 2014;1924–1990:78. [Google Scholar]
- Fifty (50) Minds. (2020). Retrieved April 7, 2020, from https://50minds.com/nigerian-governors-jittery-as-two-state-governors-test-positive-to-covid19-this-week/.
- FIRS. (2017). The global impact of respiratory disease. In D. D. Marciniuk, D. E. Schraufnagel, T. Ferkol, K. M. Fong, G. Joos, V. L. Varela, & H. Zar (Eds.) European respiratory society, on behalf of the forum of international respiratory societies (FIRS) (2nd Edition). Lausanne, Switzerland.
- Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boëlle P, Colizza V. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736-20-30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mail and Guardian. (2020). Retrieved April 7, 2020, from https://mg.co.za/article/2020-04-07-covid-19-grounds-nigerias-medical-tourists/.
- ICLG. (2020). Retrieved April 7, 2020, from https://iclg.com/briefing/11746-covid-19-additional-palliatives-issued-by-the-federal-government-of-nigeria.
- ICLG. (2020). Retrieved April 7, 2020, from https://iclg.com/briefing/11493-nigerian-emergency-economic-stimulus-bill-all-you-need-to-know.
- Igbozurike, U. M. (1983). Rural Nigeria: Development and quality of life. In Proceeding of seminar on quality of life in rural Nigeria. Agriculture and Rural Management Training Institute.
- Imhabehkai CI. Management of community development programmes and projects, (Nigeria) Benin City: University of Benin Press; 2009. [Google Scholar]
- Institute for Health Metrics and Evaluation, IHME (2018) Global Burden of Disease Study 2017. Seattle, WA.
- Jaimes JA, André NM, Chappie JS, Millet JK, Whittaker GR. Phylogenetic analysis and structural modeling of SARS-CoV-2 spike protein reveals an evolutionary distinct and proteolytically sensitive activation loop. Journal of Molecular Biology. 2020 doi: 10.1016/j.jmb.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishamawe C, Rumisha SF, Mremi IR, Bwana VM, Chiduo MG, Massawe IS, Mboera LEG. Trends, patterns and causes of respiratory disease mortality among inpatients in Tanzania, 2006–2015. Tropical Medicine & International Health. 2019;24(1):91–100. doi: 10.1111/tmi.13165. [DOI] [PubMed] [Google Scholar]
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. New England Journal of Medicine. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Archive Ibadan, NAI. (1950) A hand-list of Nigerian Official Publication, File No. OX/046/1950.
- Nnamuchi O. Kleptocracy and its many faces: The challenges of justiciability of the right to health care in Nigeria. Journal of African Law. 2008;52(1):1–42. doi: 10.1017/S0021855308000016. [DOI] [Google Scholar]
- Ogunbekun I, Ogunbekun A, Orobaton N. Private health care in Nigeria: walking the tightrope. Health Policy and Planning. 1999;14(2):174–181. doi: 10.1093/heapol/14.2.174. [DOI] [PubMed] [Google Scholar]
- Ohia C, Bakarey AS, Ahmad T. COVID-19 and Nigeria: Putting the realities in context. International Journal of Infectious Diseases. 2020 doi: 10.1016/j.ijid.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okafor FC. Measuring rural development in Nigeria: the place of social indicators. Social Indicators Research. 1985;16(1):69–76. doi: 10.1007/BF00317660. [DOI] [Google Scholar]
- Olapegba PO, Ayandele O, Kolawole SO, Oguntayo R, Gandi JC, Dangiwa AL, Iorfa SK. A preliminary assessment of novel coronavirus (COVID-19) knowledge and perceptions in Nigeria. MedRxiv. 2020;04(11):20061408. doi: 10.1101/2020.04.11.20061408. [DOI] [Google Scholar]
- Raza, A., Okafor F.C., & Oyebanji, J.O. (Eds.) (1983). Social Deprivation in Rural Nigeria: Development and Quality of Life. In Proceedings of the seminar on quality of life in rural Nigeria. Held at the Agricultural and Rural Management Training Institute, Ilorin.
- Rocklöv J, Sjödin H. High population densities catalyse the spread of COVID-19. Journal of Travel Medicine. 2020;27(3):taaa038. doi: 10.1093/jtm/taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal J. Climate change and the geographic distribution of infectious diseases. EcoHealth. 2010;6:489–495. doi: 10.1007/s10393-010-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runciman WG, Runciman B. Relative deprivation and social justice: A study of attitudes to social inequality in twentieth-century England. Berkeley: University of California Press; 1966. [Google Scholar]
- Saker, L., Lee, K., Cannito, B., Gilmore, A., & Campbell-Lendrum, D. H. (2004). Globalization and infectious diseases: a review of the linkages (No. TDR/STR/SEB/ST/04.2). World Health Organization.
- Salvi S, Kumar GA, Dhaliwal RS, Paulson K, Agrawal A, Koul PA, Murray CJL. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. The Lancet Global Health. 2018;6:e1363–e1374. doi: 10.1016/S2214-109X(18)30409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerging Infectious Diseases. 2020 doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuchat, A. (2020). Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR. Morbidity and mortality weekly report (Vol. 69). [DOI] [PMC free article] [PubMed]
- Scott-Emuakpor A. The evolution of health care systems in Nigeria: Which way forward in the twenty-first century. Nigerian Medical Journal. 2010;51(2):53. [Google Scholar]
- Sun K, Chen J, Viboud C. Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowd sourced data: A population-level observational study. Lancet Digital Health. 2020;2:e201–e208. doi: 10.1016/S25897500-20-30026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- This is Africa. (2017). Retrieved April 7, 2020, from https://thisisafrica.me/politics-and-society/nigerias-president-buhari-medical-trips-signal-no-end-medical-tourism/.
- Von Bertalanffy L. General system theory: foundations, development, applications. New York: George Braziller. Inc.; 1968. [Google Scholar]
- Woolhouse ME, Adair K, Brierley L. RNA viruses: A case study of the biology of emerging infectious diseases. One Health: People, Animals, and the Environment. 2014 doi: 10.1128/microbiolspec.OH-0001-2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, WHO. (2007). Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. In Global surveillance, prevention and control of chronic respiratory diseases: A comprehensive approach (pp. vii–146).
- World Health Organization, WHO. (2017). Global Health Observatory (GHO) Data: Health-related millennium development goals and targets. Retrieved April 7, 2020, from https://www.who.int/gho/mdg/goalstragets/.
- World Health Organization, WHO. (2019). WHO MERS global summary and assessment of risk, July 2019 (No. WHO/MERS/RA/19.1). World Health Organization.
- World Health Organization, WHO. (2020a). Coronavirus disease 2019 (COVID-19) situation report 32. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200221-sitrep-32-covid-19.pdf.
- World Health Organization, WHO. (2020b). Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/whochina-joint-mission-on-covid-19-final-report.pdf.
- World Health Organization, WHO. (2020c). Coronavirus disease 2019 (COVID-19) situation report 172. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200710-covid-19-sitrep-172.pdf?sfvrsn=70724b90_2.
- Yadav T, Saxena SK. Transmission cycle of SARS-CoV and SARS-CoV-2. In: Saxena S, editor. Coronavirus disease 2019 (COVID-19). Medical virology: From pathogenesis to disease control. Singapore: Springer; 2020. [Google Scholar]