Abstract
Introduction
Since the outbreak of COVID-19, measures were taken to protect healthcare staff from infection, to prevent infection of patients admitted to the hospital and to distribute PPE according to need. To assure the proper protection without overuse of limited supply of these equipments, screening of patients before surgical or diagnostic procedure was implemented. This study evaluates the results of this screening.
Method
All patients screened for COVID-19 before procedure warranting either general, locoregional anaesthesia or sedation were included. Screening included a symptom questionnaire by phone, PCR and HRCT chest testing. Surgical or procedural details were registered together with actions taken based on screening results.
Results
Three hundred ninety-eight screenings were performed on 386 patients. The symptom questionnaire was completed in 72% of screenings. In 371 screenings, PCR testing was performed and negative. HRCT chest found 18 cases where COVID-19 could not be excluded, with negative PCR testing. Three patients had their surgery postponed due to inconclusive screening, and additional measures were taken in three other patients. There were incidental findings in 14% of HRCT chest scans.
Discussion
Pre-operative screening will differentiate if PPE is needed for procedures and which patients can safely have elective surgery during this COVID-19 pandemic and in the times to come. HRCT chest has no additional value in the pre-operative screening of asymptomatic patients. Screening can be performed with a symptom questionnaire, and additional screening with PCR testing in high-risk patient groups should be considered.
Introduction
Between 31 December 2019 and 3 January 2020, the World Health Organization (WHO) China Country Office was notified of 44 cases of pneumonia with unknown cause in the city of Wuhan, China [1]. Since then, up until 1 July 2020, 10 450 628 cases have been confirmed and 510 632 patients have lost their lives to the virus, now named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), causing coronavirus disease 2019 (COVID-19) [2]. The first COVID-19 positive test in the Netherlands was confirmed in 27 February 2020. To combat the growing number of patients suffering from COVID-19 and to ensure patient and healthcare providers safety, reductions in elective care were made and measures were taken for patients who could not wait until medical care was returning to normal, in line with precautions taken in China and Italy [3, 4].
As personal protective equipment (PPE) is in high demand, providing the best protection for healthcare workers and preventing excessive use of the limited supplies are mandatory. Research has shown that intubation and electrocautery are an aerosol-generating procedure, producing particles small enough to stay suspended in the air. This might expose healthcare providers to disease transferred through aerosols [4–7].
Additionally, in patients undergoing a procedure while suffering from COVID-19, the course of the disease can be detrimental post-operatively [8].
This study assessed the results of the screening according to our local protocol and aided the further development of pre-operative screening in this COVID-19 pandemic.
Patients and methods
Patients
The screening took place in a district teaching hospital in the Netherlands. All patients screened for COVID-19 in relation to a surgical or diagnostic intervention with anaesthesia or sedation from 6 April until 29 April 2020 were included, independent of subspecialty performing the procedure. The Dutch national guideline recommended screening patients undergoing general anaesthesia [9]. It was decided to develop a local protocol in our hospital, also including patients undergoing spinal, locoregional anaesthesia and sedation. This was to be prepared in case of conversion to general anaesthesia or deep sedation requiring manual ventilation.
Methods
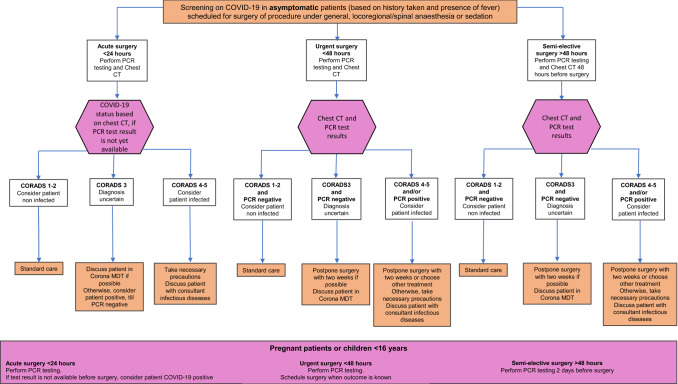
Screening included a symptom questionnaire taken by phone three working days before the procedure. It included new complaints of coughing, shortness of breath, rhinorrhoea, loss of smell and taste, sore throat or fever. Additionally, contact with suspected or confirmed COVID-19 patients was inquired after. Two days before the procedure, polymerase chain reaction (PCR) on a nasopharyngeal/oropharyngeal swab and high-resolution non-contrast computed tomography of the chest (HRCT chest), to assess the CO-RADS classification, were performed. In pregnant women or children <16 years of age, only PCR was taken. The care personnel taking the PCR was highly trained in the right method of taking a nasopharyngeal/oropharyngeal swab. In emergency admission and surgery, the screening was performed at the emergency department or as an inpatient (Fig. 1). When screening had to be repeated because of multiple interventions or postponed intervention, all screenings were recorded.
Fig. 1.
Local protocol for pre-operative and pre-procedure screening for COVID-19 disease
For each screening, patient characteristics, comorbidities and the results of the symptom questionnaire were registered along with the subspecialty performing the intervention, type of anaesthesia and results of the screening. Patients undergoing intervention were seen in standard pre-operative screening, during which American Society of Anaesthesiologists (ASA) score was determined.
HRCT scans of the chest were classified according to the COVID-19 Reporting and Data System (CO-RADS system). Five groups were described, ranging from very low likelihood of COVID-19 infection in the lungs (CO-RADS 1) to high level of suspicion (CO-RADS 5). Bilateral ground-glass opacities with or without consolidation, in the vicinity of the pleurae, were described as most important findings for establishing CO-RADS classification [10]. Scans were interpreted as CO-RADS 1 if no abnormality was found and conclusion was 'normal CT scan' or 'no abnormalities'.
Management after screening
If for any reason the time between testing and intervention became more than 48 h, repeat screening was performed. Since the result of the PCR testing would take 24 h, patients with indication for emergency surgery would be submitted to the same tests, but if the HRCT chest showed CO-RADS 1 or 2, intervention would commence without extra PPE and without waiting for the results of the PCR testing. In case of CO-RADS 3 or higher, and the PCR result was not available, surgery was performed assuming patient was COVID-19 positive. When waiting for the PCR was possible, this was preferred in patients with CO-RADS 3 or higher and the case would be discussed in a daily COVID multidisciplinary team (MDT) meeting with a consultant infectious diseases and consultant medical microbiologist.
Data analysis
Data analysis was performed using SPSS 20.0 (v24, IBM Corporation, Armonk, New York).
Results were reported as median with corresponding range.
Ethical approval
All study procedures were in accordance with the ethical standards of Dutch law (Medical Research Involving Human Subjects Act) and with the 1964 Helsinki Declaration and its later amendments.
Results
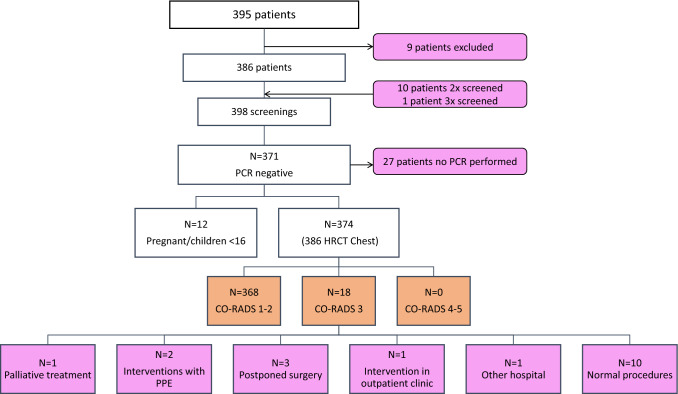
Three hundred ninety-five patients were included. Nine patients were excluded because neither HRCT chest, nor PCR testing for COVID-19 was performed. In these patients, there was no time to perform PCR testing and HRCT chest would not be performed, since these were obstetric emergencies and children under 16 years of age.
In the residual 386 patients, 398 sets of screening results were available, and 200 patients were female (52%), with a median age of 60 years (range 4–98) (Table 1).
Table 1.
Patient characteristics
| (n = 386) | |
|---|---|
| Age (years), median | 60 |
| Sex | |
| Male | 186 (48%) |
| Female | 200 (52%) |
| BMI (kg/m2), median | 26.8 |
| ASA score* | |
| I | 82 (23%) |
| II | 165 (46%) |
| III | 103 (28%) |
| IV | 11 (3%) |
| Diabetes mellitus (%) | 33 (9%) |
| Hypertension (%) | 109 (28%) |
| Cardiovascular comorbidities (%) | 99 (26%) |
| Kidney failure (%) | 10 (3%) |
BMI, Body mass index, ASA, American Society of Anaesthesiologists;
*Nine patients undergoing electric cardioversion were not seen in standard pre-operative screening, and 16 patients were screened but did not need surgical treatment. This explains why a total number of registered ASA scores do not combine to the total of 386 patients
Three hundred eighty-six patients undergoing intervention from 11 different specialties were identified. In 16 cases (4%), surgery was delayed or the decision was made not to operate at all. This included five elderly patients with a femur fracture, in which the decision was made to implement a palliative treatment. Of the remaining 370 patients, 137 patients (37%) had an indication for emergency surgery. Most interventions were performed by surgeons (n = 208, 56%). General anaesthesia was the most commonly used type of anaesthesia (n = 216 times, 59%) (Table 2).
Table 2.
Operative or procedural characteristics
| (n = 370) | |
|---|---|
| Semi-elective intervention | 233 (63%) |
| Emergency intervention (%) | 137 (37%) |
| Anaesthesia technique* | |
| General anaesthesia | 216 (59%) |
| Combined regional anaesthesia and sedation | 58 (16%) |
| Spinal anaesthesia | 49 (13%) |
| Sedation | 34 (9%) |
| Peripheral nerve block | 9 (2%) |
| Local and regional anaesthesia | 4 (1%) |
| Subspecialty | |
| General surgery | 208 (56%) |
| Orthopaedic surgery | 60 (16%) |
| Urology | 41 (11%) |
| Gynaecology | 23 (6%) |
| Cardiology | 15 (4%) |
| Plastic surgery | 9 (2%) |
| Neurosurgery | 6 (2%) |
| Gastroenterology | 4 (1%) |
| Otolaryngology | 3 (1%) |
| Pulmonology | 1 (0.3%) |
| Ophthalmology | 1 (0.3%) |
*In 16 patients, surgery was delayed or the decision was made to not operate at all, so no anaesthesia method could be registered
Screening
Of all 398 screenings, a symptom questionnaire was taken in 287 (72%) cases, including histories taken in the emergency department, where the questionnaire was not always completed (24 cases, 6%) as only coughing and shortness of breath were asked. In 24 patients, the questionnaire was negative, but exact answers were not noted. In geriatric admissions, cough, fever and dyspnoea are part of standard admission history taken on the ward. These results were scored when full symptom questionnaire was not taken (n = 16, 4% of histories). In screenings performed on 21 (5%) clinical patients, no symptom questionnaire was taken. These include seven repeated screenings for patients having repeat surgery due to complications. The symptom questionnaire was less often performed in emergency surgery compared to semi-elective surgery (49% versus 87% respectively).
Symptoms were reported during the questionnaire by 36 patients (9%), and no patients reported more than two symptoms. Fever was reported most, by 17 patients (4%). Least reported was loss of smell and taste, two times (1%) (Table 3).
Table 3.
COVID-19 symptoms
| (n = 398) | |
|---|---|
| Coughing | |
| Yes | 7 (2%) |
| No | 278 (70%) |
| N/A | 113 (28%) |
| Shortness of breath | |
| Yes | 6 (2%) |
| No | 275 (69%) |
| N/A | 117 (29%) |
| Rhinorrhoea | |
| Yes | 4 (1%) |
| No | 251 (63%) |
| N/A | 143 (36%) |
| Loss of smell and taste | |
| Yes | 2 (1%) |
| No | 248 (62%) |
| N/A | 148 (37%) |
| Sore throat | |
| Yes | 3 (1%) |
| No | 254 (64%) |
| N/A | 141 (37%) |
| Fever | |
| Yes | 17 (4%) |
| No | 380 (95%) |
| N/A | 1 (0.3%) |
| Entrance of endemic regions | |
| Yes | 3 (1%) |
| No | 247 (62%) |
| N/A | 148 (37%) |
| Contact with suspected or confirmed patients | |
| Yes | 3 (1%) |
| No | 246 (62%) |
| N/A | 149 (37%) |
All PCR tests (371 screenings) were negative. Three hundred eighty-six CT scans were performed on 374 patients. In 12 cases, no HRCT chest was performed, because of pregnancy or age under 16 years (Table 4). Three hundred sixty-seven (95%) of the HRCT chests were either negative (CO-RADS 1 or 2) or inconclusive (between CO-RADS 1 and 2, 6 cases). Six scans with unspecified CO-RADS were reviewed by radiologists. In one patient, the diagnosis changed to CO-RADS 3, but PCR was negative. The other patients were classified as CO-RADS 1 and 2.
Table 4.
Screening results
| n = 398 | |
|---|---|
| Positive PCR (%) | 0 (0%) |
| HRCT chest* | |
| CO-RADS 1 | 343 |
| CO-RADS 2 | 25 |
| CO-RADS 3 | 18 |
| CO-RADS 4 | 0 |
| CO-RADS 5 | 0 |
| Not performed | 12 |
| Incidental findings during HRCT chest | |
| Aortic aneurysm | 3 |
| Pulmonary nodule | 20 |
| Lung emphysema | 10 |
| Renal tumours | 4 |
| Bone metastasis | 2 |
| Diaphragmatic hernia | 4 |
| Colon carcinoma | 1 |
| Others | 12 |
PCR, Polymerase chain reaction, HRCT chest, high-resolution computed tomography chest, results after revision
In 18 cases total, CO-RADS 3 was found. Fifteen patients were discussed in the daily COVID MDT meeting. Three patients were not discussed, two had the intervention without extra PPE, and the other was screened before decision for palliative treatment without surgery was made. PCR testing on the others came back negative. In six cases, the MDT conclusion had impact on the surgical management and one patient was transferred to another hospital due to underlying disease. The other eight patients were operated without extra PPE as their PCR testing was negative (Fig. 2).
Fig. 2.
Patient flow and screening outcome of the study
Of the 398 screenings, ten were double screenings, and one patient had three screenings, making twelve double screenings (Fig. 2). In three of the patients with double screening, surgery was delayed due to pre-operative optimisation or logistic reasons and screening had to be repeated because the 48-h window of valid screening results had passed. Seven patients had a second screening due to repeat surgery, and one patient had two more screenings and subsequent surgeries due to complications. In one patient, PCR testing was not performed in the second screening. CO-RADS score was different in two patients (CO-RADS 2 to CO-RADS 1 and CO-RADS 2 to CO-RADS 3) on repeated HRCT chest, and this seemed due to interobserver variation.
Incidental findings
In 55 (14% of scans) patients, 56 incidental findings were made (Table 4). In total, nine abnormalities suspect for malignancy were found, together with two scans indicating metastatic disease with unknown primary tumour (20% of findings). An aortic aneurysm was found in three patients (5%). A total of 20 pulmonary nodules requiring follow-up were found, ranging from benign to malignant, constituting 36% of findings and 5% of all HRCT chests performed. In one patient, a colon carcinoma was found in addition to the pulmonary nodules. In case of an incidental finding, the attending physician was notified.
COVID-19 post-operative
Four patients developed for COVID-19 suspected symptoms post-operatively, after which repeat PCR testing came back positive. Three had negative screening before surgery. In one patient, CO-RADS 3 was reported pre-operative. In COVID-MDT, this patient was rated as not suspicious given a negative PCR and lack of symptoms and was treated as COVID negative in theatre.
These four patients were aged 87–91 years, and all received surgery for a subcapital femoral neck fracture and were admitted to the geriatric department. One patient only experienced a mild sore throat and was tested before discharge to a nursing home. One patient, the only male of the four, went into a post-operative delirium, after which palliative management was started and patient died within one day. PCR testing came back positive afterwards. One patient developed symptoms in the nursing home after discharge and was diagnosed there. The last patient experienced dyspnoea and was tested positive.
Discussion
Pre-operative and pre-procedural screening of all patients before intervention is a necessary part of protecting medical personnel, proper distribution of PPE and hospital capacity. This is emphasised by the fact that 3–20% of patients with symptomatic COVID-19 are healthcare workers [11]. In this study, the results of the screening from our local protocol were evaluated.
Screening
Clinical patients had no questionnaire taken, probably because they were under observation and symptoms would be observed by the staff. All patients were screened by a general practitioner before referral to the emergency room. This included questions to rule out COVID-19 according to Dutch guidelines. During this study, we could only collect data from the electronic patient file. The outcome of this study changed the protocol; all questions were repeated and recorded in the electronic patient file.
A limited number of patients reported symptoms, and none had more than two symptoms. There was a relatively high percentage of patients with fever. This is probably explained by the inclusion of emergency surgeries, as these conditions can present with fever.
Pre-operative HRCT chest could not rule out COVID-19 in some cases, but CO-RADS 4 or 5 was not reported. However, in six patients with CO-RADS 3, this screening changed the operative management to protect staff and patient from surgery with the chance of exposure and more serious complications of COVID-19 [5, 7, 8]. As this accounts for only 2% of all HRCT chest performed and incidental findings were made in 14%, it could be discussed if screening with HRCT chest should be advised. CT scanning of the chest in asymptomatic people for detection of COVID-19 infection produces greater disease burden through incidental findings than help diagnosing patients [12, 13]. And the added value will be affected by the low background prevalence of COVID-19 in the general population, estimated to be three to five per cent, although research into this is ongoing [14].
Sensitivity for COVID-19-related abnormalities on CT chest (72–79%) compared to PCR showed no statistically significant difference in two studies [15, 16]. As these studies were performed with symptomatic patients, it is unsure what these numbers would be for asymptomatic patients. Also, CT chest might not be as sensitive as is currently presumed [17].
Post-operative COVID-19
COVID-19 patients receiving surgery during the incubation period of the disease have a higher chance of needing treatment in ICU and a higher mortality rate. Longer surgery and more difficult procedures were predictors of more complicated disease progression, together with age and comorbidity [8]. In this study, four geriatric patients became SARS-CoV-2 positive post-operatively. Three had negative screening before surgery, and in one patient, CO-RADS 3 was reported pre-operative, but not seen as suspicious for COVID-19 by the COVID-MDT. Of these patients, two developed delirium during admission after which they tested positive. Delirium is now seen as a possible symptom of COVID-19 and warrants testing. One patient has had contact with a COVID-19 patient at unknown time and tested positive before discharge with a sore throat as sole symptom. The last patient had a single spike of fever nine days after admission, but no other symptoms, for which PCR was repeated and was positive.
We think patients either were infected as an inpatient or infected pre-operative, but due to incubation period, the viral load was low and therefore the pre-operative PCR negative.
Follow-up in COVID-19 positive patient is according to guidelines; after cessation of symptoms, two consecutive PCRs need to be negative, before isolation will be withdrawn.
We have reviewed all patients, but if patients developed symptoms at home and were managed as an outpatient, we would not be able to record; therefore, there could be more patients being infected with COVID-10 post-operatively.
Future
As the COVID-19 prevalence in the Netherlands seems to be decreasing, upscaling surgical treatment is started, but safety of staff and patients has to be maintained. Additional measures apart from screening patients can aid in this effort [18–20].
The semi-elective screening in our hospital was performed centrally for all specialities to avoid delays in surgery due to missing screening. The logistics around the screening is challenging and should be well organised. At this moment, screening in the Netherlands has been changed to only PCR testing together with a symptom questionnaire [21].
Possibly, the symptom questionnaire will be the most important tool in diagnosing COVID-19 and determining whether PCR screening should be performed [22]. This method would rely greatly on the completeness of the symptom questionnaire, and its importance should be emphasised. Additionally, PCR screening in certain asymptomatic groups of high-risk patients (>70 years old, COVID-19 mortality-related comorbidity, aerosol-producing procedures, major surgery with risk of post-operative ICU admission) should be considered.
Conclusion
All data combined suggest that screening of patients before a surgical or diagnostic procedure for COVID-19 is necessary. A symptom questionnaire to exclude symptoms suspect for COVID-19 is probably the most important tool, with further screening through PCR testing in certain risk groups. With a low prevalence of COVID-19, HRCT chest has no added value.
Dr. E. M. Huybens
A lifelong wish to become a medical professional and an interest in surgery lead Dr. Esther Huybens to the study of medicine at the University of Leiden. With an emergency room internship at the Miller School of Medicine in Miami, Florida, further sparking her interest in trauma care, she has been gathering knowledge and experience in different hospitals to prepare her for the route to becoming a specialised medical professional. She is now starting to expand her interest in the world of medical research and finding numerous questions in need of answers. With this publication, she wants to make a start to her contribution to the global medical knowledge
Funding
This work was not supported by any organisational funding.
Compliance with Ethical Standards
Conflict of interest
The authors have nothing to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Reports1. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4. Published January 21, 2020. Accessed May 7, 2020.
- 2.WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/. Currently updated daily. Accessed July 1, 2020.
- 3.Zheng HM, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Sur. 2020;272:5–6. doi: 10.1097/SLA.0000000000003924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . Infection prevention and control of epidemic- and pandemic-prone acute respiratory infections in healthcare. Geneva: WHO; 2014. [PubMed] [Google Scholar]
- 5.Seto WH. Airborne transmission and precautions: facts and myths. J Hosp Infect. 2015;89:225–228. doi: 10.1016/j.jhin.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li C, Pai J, Chen C. Characterization of smoke generated during the use of surgical knife in laparotomy surgeries. J Air Waste Manag Assoc. 2020;70(3):324–332. doi: 10.1080/10962247.2020.1717675. [DOI] [PubMed] [Google Scholar]
- 7.Veziant J, Bourdel N, Slim K. Risks of viral contamination in healthcare professionals during laparoscopy in the Covid-19 pandemic. J Visc Surg. 2020;157:S59–S62. doi: 10.1016/j.jviscsurg.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lei S, Jiang F, Su W, Chen C, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bacx R, van Berge Henegouwen MI, Boermeester MA, et al (2020) Pre-operative work-up for COVID19 infection in asymptomatic patients scheduled for surgery under general anesthesia. Version 1. Published April 2, 2020.
- 10.Prokop M, van Everdingen W, van Rees Vellinga T, et al. CO-RADS—a categorical CT assessment scheme for patients with suspected COVID-19: definition and evaluation. Radiology. 2020;296:79–104. doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ECDC. Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK– ninth update. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-ninth-update-23-april-2020.pdf. Publihed April 23, 2020. Accessed May 11, 2020.
- 12.Liu WH, Wang XW, Cai ZQ, et al. Chest CT as a screening tool for COVID-19 in unrelated patients and asymptomatic subjects without contact history is unjustified. Quant Imaging Med Surg. 2020;10(4):876–877. doi: 10.21037/qims.2020.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang Y, Cheng W, Zhao N, et al. CT screening for early diagnosis of SARS-CoV-2 infection. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30247-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanquin (2020). Ongeveer 5,5% van bloeddonors heeft corona-antistoffen. Published June 3, 2020. Accessed June 22, 2020.
- 15.Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296:115–117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He J, Luo L, Luo Z, et al. Diagnostic performance between CT and initial real-time RT-PCR for clinically suspected 2019 coronavirus disease (COVID-19) patients outside Wuhan China. Respir Med. 2020;168:105980. doi: 10.1016/j.rmed.2020.105980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waller JV, Kaur P, Tucker A, et al. Diagnostic tools for coronavirus disease (COVID-19): comparing CT and RT-PCR Viral nucleic acid testing. AJR. 2020;215:1–5. doi: 10.2214/AJR.20.23418. [DOI] [PubMed] [Google Scholar]
- 18.Gilat R, Haunschild ED, Tauro T, et al. Recommendations to optimize the safety of elective surgical care while limiting the spread of COVID-19: Primum non nocere. Arthrosc Sports Med Rehabil. 2020;2:177–183. doi: 10.1016/j.asmr.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soma M, Jacobson I, Brewer J, et al. Operative team checklist for aerosol generating procedures to minimise exposure of healthcare workers to SARS-CoV-2. Int J Pediatr Otorhinolaryngol. 2020;134:110075. doi: 10.1016/j.ijporl.2020.110075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flemming S, Hankir M, Emestus R, et al. Surgery in times of COVID-19—recommendations for hospital and patient management. Langenbecks Arch Surg. 2020;405:359–364. doi: 10.1007/s00423-020-01888-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bacx R, van Berge Henegouwen MI, Boermeester MA, et al (2020) Practice guideline Pre-operative work-up for COVID-19 infection in asymptomatic patients scheduled for surgery under general anesthesia. Version 3. Utrecht:Federatie Medisch Specialisten;2020 Version 3, Published May 1
- 22.Forrester JD, Nassar AK, Maggio PM, et al. Precautions for operating room team members during the COVID-19 pandemic. J Am Coll Surg. 2020;230(6):1098–1101. doi: 10.1016/j.jamcollsurg.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]