Abstract
Objective
Pediatric chronic pain evaluation includes self-reports and/or caregiver proxy-reports across biopsychosocial domains. Limited data exist on the effects of caregiver–child discrepancies in pediatric pain assessment. In children with chronic pain, we examined associations among discrepancies in caregiver–child reports of child anxiety and depressive symptoms and child functional impairment.
Methods
Participants were 202 children (Mage=14.49 ± 2.38 years; 68.8% female) with chronic pain and their caregivers (95.5% female). Children and caregivers completed the Revised Child Anxiety and Depression Scale (RCADS) and RCADS-Parent, respectively. Children also completed the Functional Disability Inventory. Mean difference tests examined caregiver–child discrepancies. Moderation analyses examined whether associations between child self-reported anxiety and depressive symptoms and functional impairment varied as a function of caregiver proxy-report.
Results
Children reported more anxiety and depressive symptoms compared with their caregivers’ proxy-reports (Z = −4.83, p < .001). Both informants’ reports of child anxiety and depressive symptoms were associated with child functional impairment (rs = .44, rs = .30, p < .001). Caregiver proxy-report moderated associations between child-reported anxiety and depressive symptoms and functional impairment (B = −0.007, p = .003). When caregiver proxy-report was low, child self-reported anxiety and depressive symptoms were positively related to functional impairment (B = 0.28, SE = 0.07, 95% CI [0.15, 0.41], p < .001).
Conclusions
Discrepant caregiver–child perceptions of child anxiety and depressive symptoms may be associated with functioning in children with chronic pain, especially when caregivers report less child internalizing symptoms. These findings highlight the need for further examination of the effects of caregiver–child discrepancies on pediatric chronic pain outcomes and may indicate targets for intervention.
Keywords: anxiety, children, chronic and recurrent pain, depression, informant discrepancies, parents
Introduction
Epidemiological data indicate that approximately 15–38% of children and adolescents experience chronic pain (King et al., 2011). Youth with chronic pain often report significant impairment in physical and psychosocial functioning (Gauntlett-Gilbert & Eccleston, 2007; Kashikar‐Zuck et al., 2008; Walker, 2008). Psychopathology is also common in youth with chronic pain conditions, and these youth may be at an increased risk of developing anxiety and depressive disorders, relationships that may further exacerbate poor outcomes in this population (Vinall, Pavlova, Asmundson, Rasic, & Noel, 2016).
Given the biopsychosocial nature of pain (Liossi & Howard, 2016), comprehensive, evidence-based assessment is an important part of pediatric pain treatment. Evidence-based assessment in pediatric chronic pain populations includes assessment across multiple domains, including both physical and emotional functioning (Cohen et al., 2008; Liossi & Howard, 2016). In clinical and research settings, caregivers and their children commonly provide proxy and self-reports, respectively, about pain and functioning. Thus, clinicians and researchers have to consider data from multiple informants when considering appropriate treatment targets and data analyses.
Broader child clinical literature emphasizes the clinical importance of caregiver–child discrepancy analyses and indicates that discrepancies may predict poor outcomes. Specifically, findings from research examining treatment for pediatric anxiety-related disorders indicate that poor caregiver–child symptom agreement at baseline is associated with poorer treatment response (Becker-Haimes, Jensen-Doss, Birmaher, Kendall, & Ginsburg, 2018; De Los Reyes, 2011). Other work reveals that caregiver–child discrepancies are associated with poor family functioning and child psychopathology, and that discrepancies may be a unique and clinically relevant factor beyond informant report alone (De Los Reyes & Kazdin, 2005; Laird & Weems, 2011).
Although caregiver proxy-report is deemed acceptable in pediatric pain assessment (Cohen et al., 2008), caregiver–child agreement is modest (Vetter, Bridgewater, Ascherman, Madan-Swain, & McGwin, 2014) and discrepancies exist (Varni et al., 2015). Research on children with chronic conditions indicates that caregiver–child discordance is higher for psychosocial domains and internal symptoms (Varni et al., 2015) compared with objective, more observable domains (e.g., physical functioning). Limited data in pediatric chronic pain populations reveal similar patterns of discordance for emotional and internal experiences (Cohen, Vowles, & Eccleston, 2010), with one study reporting an association between higher caregiver–child pain report discordance and child negative mood symptomatology (Gaultney, Bromberg, Connelly, Spears, & Schanberg, 2017). In a large clinical study, caregivers of children with chronic pain significantly underreported child anxiety-related symptoms compared with their child’s self-report (Tran, Jastrowski Mano, Anderson Khan, Davies, & Hainsworth, 2016). This growing body of research suggests that caregiver proxy-reports may not adequately describe internalizing symptoms and further examination of the clinical implications of discrepancy patterns in pediatric chronic pain is needed.
The analytical approach of examining informant discrepancies has received increased attention as more studies emphasize conceptualizing informant discrepancy as a clinically relevant factor as opposed to solely a reflection of measurement error (De Los Reyes & Kazdin, 2005; De Los Reyes, Salas, Menzer, & Daruwala, 2013; Laird & Weems, 2011). The conceptualization of informant discrepancy as an independent variable with potential clinical implications shifts the methodological approach of discrepancy analyses. Specifically, researchers recommend utilizing multiple regression and moderation analyses to examine the effects of the interaction between two informants’ reports on an outcome (Laird & Weems, 2011). This approach differs from difference score analyses as it tests whether associations between one informant’s report (e.g., child self-report) and an outcome differ as function of another informant’s report (e.g., caregiver proxy-report). In addition, a moderation framework can examine the effects of the interaction, or discrepancy, above and beyond the main effects of the informant reports (e.g., child self-report and caregiver proxy-report; De Los Reyes, Salas, et al., 2013; Holmbeck, Li, Schurman, Friedman, & Coakley, 2002).
The objective of the current study was to apply a moderation framework to the examination of associations between caregiver–child discrepancies of child anxiety and depressive symptoms and child functional impairment in a sample of children with chronic pain. The first aim was to compare child self-report and caregiver proxy-report on the frequency of child anxiety and depressive symptoms. We hypothesized that caregivers would underreport child symptoms of anxiety and depression (Tran et al., 2016) compared with child self-reports. The second aim was to examine associations between caregiver–child emotional report discrepancy and child functional impairment and assess whether caregiver proxy-report moderated the association between child-reported anxiety and depressive symptoms and functional impairment. In line with other data indicating that child outcomes vary as a function of the interaction between caregiver and child reports (De Los Reyes & Kazdin, 2005; De Los Reyes, Salas, et al., 2013; Ohannessian & Reyes, 2014), we hypothesized that caregiver proxy-report of child emotional symptoms would moderate the association between child self-report of emotional symptoms and child functional impairment. Given the dearth of research utilizing moderation analyses to examine discrepancies among these constructs in pediatric samples, we did not make hypotheses in regard to the direction of the interaction results.
Methods
Data for the current study were collected as part of a larger study, which assessed pain, health, and psychological factors among families attending a pediatric tertiary pain clinic. One other study has been published on this dataset. This study assessed pain, sleep, and affect in children with pain and results indicated that poor sleep quality was significantly associated with increased pain, disability, negative affect, and decreased positive affect (Evans, Djilas, Seidman, Zeltzer, & Tsao, 2017). The present findings have not been published previously.
Participants
Children and their caregivers referred to a pediatric chronic pain clinic were recruited from September 2009 through May 2014. Children were eligible to participate if they were scheduled for a new patient appointment at one of two local tertiary pediatric chronic pain clinics and between the ages of 8 and 17 years old. Children were excluded if they had a significant developmental delay that would impair their ability to complete questionnaires. Caregivers of children ages 8–17 years old were eligible to participate. Study questionnaires were only available in English, so children and caregivers who were not fluent in English were not eligible to participate. Participants in the current sample included 202 children (M = 14.49 years old; 68.8% female) and their caregivers (M = 47.37 years old; 91.1% mothers). Of the caregivers who consented to participate (N = 214), 94.4% (N = 202) identified as the primary caregiver and were included in the current study. The number of questionnaire packets distributed to patients was not recorded and therefore recruitment rates are not available. Based on clinic census approximation, an estimated 290 new patients were scheduled during the recruitment period. Thus, the estimated recruitment rate for our sample was 69.6%, which does not take into account patient eligibility. Anecdotally, reasons for nonparticipation included a lack of interested in research participation, lack of time during the appointment to conduct consent procedures, and not having completed the intake packets. A post hoc power analysis, conducted using G*power 3.1.9 (Erdfelder, Faul, & Buchner, 1996), indicated 99% power to detect a significant medium effect (f2 = .15) for a linear regression with three predictors for a sample of 202 participants.
Procedure
Approximately 2 weeks prior to the clinic visit, all families scheduled for a new patient clinic appointment were sent via mail or email a packet that included clinic intake caregiver and child questionnaires. The clinical care coordinator identified children and caregivers who were eligible for the study. Eligible children and caregivers received a study information sheet, caregiver consent and child assent forms, and a Health Insurance Portability and Accountability Act (HIPAA) research authorization form with their intake packet. Potential participants were asked to review the consent/assent and HIPAA forms prior to the child’s clinic appointment; informed consent, and assent forms were completed in-person with a research assistant during the clinic visit. All children and caregivers completed the questionnaires prior to their clinic appointment and only data from families that consented to participating in research were included in the study. All study procedures were approved by the UCLA Institutional Review Board.
Measures
Demographics
Caregivers completed a questionnaire querying their child’s age, sex, race, and ethnicity. Caregivers also reported their own age, sex, and education level.
Pain Diagnosis
Each child’s pain diagnosis was obtained from the pain clinic intake report in the medical chart. Coauthor L.K.Z. grouped pain diagnoses into the following categories: abdominal/pelvic pain, headaches/migraines, myofascial pain, fibromyalgia/widespread pain, joint pain, or complex regional pain syndrome type I or type II. If a child had multiple pain diagnoses, all diagnoses were recorded.
Pain Intensity
Children rated their overall pain intensity over the last month on a 0 (no pain) to 10 (worst pain possible) Numeric Rating Scale (NRS). The NRS has demonstrated acceptable validity in pediatric pain samples (Miró, Castarlenas, & Huguet, 2009).
Child Anxiety and Depressive Symptoms
The Revised Child Anxiety and Depression Scale (RCADS) and RCADS-Parent (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000; Ebesutani et al., 2011) assessed child self-reported anxiety and depressive symptoms and caregiver proxy-report of anxiety and depressive symptoms, respectively. The RCADS and RCADS-P are 47-item measures that assess the presence and frequency of the child’s anxiety and depressive symptoms on a four-point Likert scale (0 = never, 3 = always). The total RCADS score was used for analyses, with higher scores reflecting higher symptom frequency. Clinical elevation proportions derived from T-score calculations (Normal [T-score <65], Borderline [T-score 65 ≤ 70], and Clinical [T-score ≥70]) are also presented to characterize the sample. Internal consistency for the child and parent scales was excellent (α = .95; α = .91, respectively).
Child Functional Impairment
Children indicated their level of functional impairment via the Functional Disability Inventory (FDI; Walker & Greene, 1991). The FDI is a 15-item measure that assesses functional ability over the last 2 weeks. Children indicated the level of difficulty for each item from 0 (“no trouble”) to 4 (“impossible”). The FDI has demonstrated validity and reliability in pediatric pain samples (Kashikar-Zuck et al., 2011) and internal consistency for the current sample was excellent (α = .91).
Data Analyses
Prior to data analyses, missing data for each measure were examined and we imputed missing values per measure instructions. If no specific instructions were provided and if at least 80% of the scale was completed, we imputed missing data based on scale means. For scales with less than 80% completion, no data were imputed. Frequency of missing data was low, ranging from 1.5% to 4.5% of the sample for any individual scale (FDI, RCADS) or single outcome variable (overall pain). After imputing missing values as described above, the overall level of missing data was 2.5%. Measures scores were converted to z-scores to identify outliers (z > 3.29). One case of child self-reported of emotional symptoms was identified. Analyses were conducted with this case excluded and no differences were detected so this case was retained for analyses.
Descriptive statistics were utilized to characterize the sample (i.e., child and caregiver age, sex, race, and ethnicity, and child pain intensity and pain diagnosis) and primary variables (i.e., child self-reported anxiety and depressive symptoms, caregiver proxy-reported child anxiety and depressive symptoms, and child functional impairment). Descriptive statistics indicated that the primary variables were skewed and resistant to transformation, so nonparametric tests were used for subsequent analyses. Analyses to examine associations among demographic variables (i.e., child age, pain intensity) and primary variables were conducted with Spearman rank correlations. Mann–Whitney U mean difference tests examined whether the primary variables differed by child/caregiver sex, race, ethnicity, or child pain diagnosis. Demographic variables that were associated with both independent (i.e. self-reported and proxy-reported emotional functioning) and dependent variables (i.e., child functional impairment) were controlled for in subsequent analyses.
We utilized Wilcoxon mean difference tests to examine whether child self-reported anxiety and depressive symptoms differed from caregiver proxy-reported anxiety and depressive symptoms. To compare how caregiver under and over-reporting related to child functional impairment, Wilcoxon mean difference tests examined if child functional impairment differed when caregivers underreported or over reported (i.e., caregiver reports were lower or higher than child reports, respectively). Cohen’s d effect sizes were calculated for comparisons of mean differences (small effect = 0.20, moderate effect = 0.50, large effect = 0.80). Intraclass coefficients (ICC) were used to evaluate caregiver–child agreement across reports of child reports of child anxiety and depressive symptoms. Spearman rank correlational analyses were conducted to examine associations between child self-reported anxiety and depressive symptoms, caregiver proxy-reported anxiety and depressive symptoms, and child functional impairment.
To examine whether associations between child self-reported anxiety and depressive symptoms and functional impairment varied as a function of caregiver proxy-report, we conducted a hierarchical regression. Child sex, age, the presence of a widespread pain diagnosis, and pain intensity were associated with anxiety and depressive symptoms and functional impairment, so these variables were entered as covariates in the first step of the regression. Mean-centered child self-reported and caregiver proxy-reported anxiety and depressive symptoms were entered in the second step, and the child self-reported by caregiver proxy-reported anxiety and depressive symptoms interaction term was entered in the third step. We then conducted post hoc probing utilizing simple slope analyses to examine conditional effects at “high” (i.e., one standard deviation above the mean) and “low” (i.e., one standard deviation below the mean) levels of caregiver proxy-report (Holmbeck, 2002). For moderation analyses, Cohen f2 effect sizes are reported (small effect = 0.02, medium effect = 0.15, large effect = 0.35; Cohen, 1988).
Results
Sample demographic data are presented in Table I. Child age was positively associated with functional impairment (rs = .19, p = .009) and child-reported anxiety and depressive symptoms (rs = .18, p = .013). Female children reported higher levels of functional impairment (Z = −2.60, p = .009) and anxiety and depressive symptoms (Z = −2.25, p = .025). Child age (rs = .06, p = .39) or sex (Z = −1.31, p = .19) was not associated with caregiver proxy-report of child anxiety and depressive symptoms. Children with fibromyalgia/widespread body pain reported significantly more anxiety and depressive symptoms (Z = −2.97, p = .003) and functional impairment (Z = −3.45, p = .001) compared with children who did not have fibromyalgia/widespread body. Child pain intensity was positively associated with child functional impairment (rs = .35, p < .001) and with child-reported anxiety and depressive symptoms (rs = .16, p = .023).
Table I.
Participant Demographic and Primary Variable Descriptive Data
|
M ± SD (range) |
||
|---|---|---|
| Variable | Child | Caregiver |
| Age | 14.49 ± 2.38 (8–17) | 47.37 ± 5.65 (30–65) |
| Pain intensity | 6.47 ± 1.95 (0–10) | – |
| Child Anxiety and Depressive Symptoms | 34.53 ± 21.60 (1–115) | 27.86 ± 14.20 (0–70) |
| Child Functional Impairment | 21.45 ± 12.58 (0–47) | – |
| N (%) | ||
| Sex | ||
| Male | 63 (31.2) | 8 (4.0) |
| Female | 139 (68.8) | 193 (95.5) |
| Missing | 1 (0.5) | |
| Race | ||
| African American | 4 (2.0) | 5 (2.5) |
| Asian | 3 (1.5) | 4 (2.0) |
| American Indian/Alaska Native | 2 (1.0) | 1 (.5) |
| White | 170 (84.1) | |
| Other | 14 (6.9) | 11 (5.4) |
| Missing | 9 (4.5) | 9 (4.5) |
| Ethnicity | ||
| Latino | 34 (16.8) | 31 (15.3) |
| Non-Latino | 159 (78.7) | 166 (82.2) |
| Missing | 9 (4.5) | 9 (4.5) |
| Educational level | ||
| Less than high school | – | 3 (1.5) |
| High school | – | 11 (5.4) |
| Some college/associates degree | – | 53 (26.2) |
| College degree | – | 61 (30.2) |
| Post-graduate degree | – | 64 (31.7) |
| Other | – | 7 (3.5) |
| Missing | 3 (1.5) | |
| Pain diagnosisa | ||
| Abdominal/pelvic pain | 103 (51.0) | – |
| Headaches/migraines | 87 (43.1) | – |
| Myofascial pain (excluding headaches) | 72 (35.6) | – |
| Fibromyalgia/widespread pain | 56 (27.7) | – |
| Joint pain | 34 (16.8) | – |
| CRPS type I or type II | 27 (13.4) | – |
| Multiple pain diagnoses | 120 (59.4) | – |
| Child Anxiety and Depressive Symptoms Clinical Elevation Classification | ||
| Normal | 174 (86.1) | 163 (80.7) |
| Borderline | 14 (6.9) | 13 (6.4) |
| Clinical | 11 (5.4) | 21 (10.4) |
| Missing | 3 (1.5) | 5 (2.5) |
Note. aPercentages sum to more than 100% due to multiple pain diagnoses.
CRPS = complex regional pain syndrome.
A Wilcoxon signed rank test indicated that children reported higher frequency of anxiety and depressive symptoms (M = 34.53) compared with their caregivers’ proxy-reports (M = 27.86; Z = −4.95, p < .001, d = 0.36). Compared with child self-reports, 59.5% of caregivers underreported, 36.3% overreported, and 4.2% had the same score on child emotional symptoms. Child functional impairment was significantly higher when caregivers underreported (Z = −2.56, p = .01). Caregiver–child agreement on child anxiety and depressive symptoms was moderate (ICC = .54, 95% CI [0.40, 0.66]). Spearman rank correlational analyses revealed that child self-report of anxiety and depressive symptoms was associated with caregiver proxy-reports (rs= .64, p < .001) and higher child and caregiver reports of child anxiety and depressive symptoms were associated with higher child functional impairment (rs = .44, rs = .30, ps < .001, respectively).
Regression analyses indicated that controlling for child age, sex, widespread pain diagnosis, and pain intensity, there was a main effect for child self-reported anxiety and depressive symptoms on functional impairment (B = 0.01, SE = 0.004, p = .01). However, examination of the final step in the regression model indicated that caregiver proxy-report of child anxiety and depressive symptoms moderated the relationship between child-reported anxiety and depressive symptoms and functional impairment with a medium-large effect (B = −0.007, SE = 0.002, ΔR2 = .03, p = .003, f2 = 0.33). The interaction model accounted for 22.4% of the total variability in functional impairment (Table II). Post hoc probing of the interaction term revealed that at low levels of caregiver proxy-report of child anxiety and depressive symptoms (i.e., one standard deviation below the mean), child self-reported anxiety and depressive symptoms was significantly positively related to functional impairment (B = 0.28, SE = 0.07, 95% CI [0.15, 0.41], p < .001; Figure 1). There was no significant effect of child-reported anxiety and depressive symptoms on functional impairment at high levels of caregiver proxy-report (B = 0.09, SE = 0.05, 95% CI [−0.01, 0.20], p > .05).
Table II.
Caregiver–Child Discrepancy and Child Functional Impairment
| B | SE | t | 95% CI | R 2 Adj | FΔ | |
|---|---|---|---|---|---|---|
| Block 1 | .20 | 13.05** | ||||
| Child age | 0.86 | 0.34 | 2.54* | 0.19 to 1.53 | ||
| Child sex | 2.02 | 1.79 | 1.13 | −1.52 to 5.56 | ||
| Overall pain intensity | 2.21 | 0.42 | 5.24** | 1.34 to 3.04 | ||
| Widespread pain | 5.40 | 1.90 | 2.85* | 1.66 to 9.13 | ||
| Block 2 | .28 | 10.16** | ||||
| Child age | 0.67 | 0.33 | 2.05* | 0.02 to 1.31 | ||
| Child sex | 1.00 | 1.73 | 0.58 | −2.41 to 4.40 | ||
| Overall pain intensity | 1.88 | 0.41 | 4.59** | 1.07 to 2.68 | ||
| Widespread pain | 4.18 | 1.86 | 2.25* | 1.07 to 2.68 | ||
| Child internalizing self-report | 0.14 | 0.05 | 2.82** | 0.04 to 0.24 | ||
| Caregiver internalizing proxy-report | 0.06 | 0.07 | 0.85 | −0.08 to 0.21 | ||
| Block 3 | .31 | 9.30** | ||||
| Child age | 0.57 | 0.32 | 1.78 | −0.06 to 1.20 | ||
| Child sex | 0.84 | 1.69 | 0.50 | −2.49 to 4.17 | ||
| Overall pain intensity | 1.88 | 0.40 | 4.69** | 1.09 to 2.67 | ||
| Widespread pain | 4.30 | 1.82 | 2.37* | 0.72 to 7.88 | ||
| Child internalizing self-report | 0.18 | 0.05 | 3.63** | 0.09 to0.29 | ||
| Caregiver internalizing proxy-report | 0.09 | 0.07 | 1.18 | −0.06 to 0.23 | ||
| Child × caregiver report | −0.01 | 0.00 | −3.05** | −0.01 to 0.00 |
Note. *p < .05; **p < .01.
Figure 1.
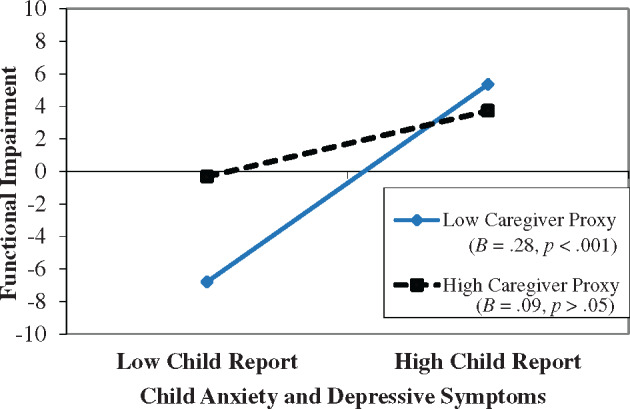
Interaction of child self-reported and caregiver proxy-reported anxiety and depressive symptoms on child functional impairment at low and high levels of caregiver proxy-report.
Discussion
Pediatric chronic pain assessment often includes gathering data from multiple informants across functional and psychosocial domains. Findings from past research indicate that although self- and proxy-reports may be correlated, caregiver–child agreement is modest and caregiver–child discrepancies are larger when assessing psychosocial domains or internalizing symptoms (Varni et al., 2015; Vetter, Bridgewater, Ascherman, Madan-Swain, & McGwin, 2014). In line with broader literature that suggests that caregiver–child discrepancies may have clinical implications and predict outcomes, the current study examined associations between caregiver–child reports of child anxiety and depressive symptoms and functional impairment and assessed whether caregiver proxy-report moderated the association between child-reported anxiety and depressive symptoms and functional impairment in a sample of children with chronic pain.
The level of functional impairment and frequency of anxiety and depressive symptoms in the current sample were mostly comparable with levels reported in other studies. Child functional impairment fell in the moderate range, which is consistent with other pediatric chronic pain samples (Kashikar‐Zuck et al., 2011). Self- and proxy-reported child anxiety and depressive symptoms were slightly higher than clinical samples (Ebesutani, Bernstein, Chorpita, & Weisz, 2012) but comparable with other pediatric pain samples (Karlson et al., 2017; Walter et al., 2016). The proportion of anxiety and depressive symptoms in the clinical range were also comparable with community (Trent et al., 2013) and clinical samples (Becker et al., 2019).
Initial examination of caregiver proxy and child self-reports revealed that caregiver–child agreement was modest and there was a strong positive correlation between child self-reported and caregiver proxy-reported anxiety and depressive symptoms. Levels of caregiver–child agreement on emotional symptoms vary across studies. The strength of association in the current sample is higher than levels reported in a diverse clinical sample (Ebesutani et al., 2012) but similar to a sample of youth with sickle cell disease (Karlson et al., 2017). Both informant reports were associated with child functional impairment. These findings are consistent with previous research that indicates agreement among caregiver–child reports (Cohen, 2008); however, further examination of caregiver and child reports revealed discrepancies. Specifically, children self-reported significantly more anxiety and depressive symptoms than did their proxies. Discordance between caregiver–child reports of internal states and emotional functioning has been documented in broader research (Kim, Choi, Ko, & Park, 2018; Varni et al., 2015). A recent study reported similar findings, demonstrating that caregivers of children with chronic pain underreported the severity of their children’s anxiety symptoms (Tran et al., 2016). Taken together, the current correlational findings may suggest that caregiver and child reports are similar, but discrepancy analyses suggest that caregivers may not have an accurate perception of their child’s experiences with anxiety and depressive symptoms (Achenbach, McConaughy, & Howell, 1987).
A primary objective of this study was to examine whether caregiver–child discrepancies in emotional functioning were associated with child functional impairment. In line with recommendations from other investigators (Laird & Weems, 2011), we utilized regression and moderation analyses to examine our primary study objective. This analytic approach allows for the examination of whether associations between an informant’s report and an outcome vary as a function of the other informant’s report (De Los Reyes, Salas, et al., 2013; Holmbeck et al., 2002; Laird & Weems, 2011).
We assessed whether the associations between child self-reported anxiety and depressive symptoms and functional impairment varied as a function of caregiver proxy-report of child anxiety and depressive symptoms. Moderation analyses revealed a significant interaction with a moderate to large effect, a finding that indicates that discrepancies between caregiver and child reports of child anxiety and depressive symptoms may affect the association between child emotional symptoms and functional impairment. Limited data have been published on the strength of caregiver–child moderation effects on child outcomes; however, the moderate to large effects seen in the current study are slightly larger than effects reported in one study examining caregiver–child discrepancy on child depressive symptoms (Laird & De Los Reyes, 2013). Examination of the conditional effects at high and low levels of caregiver proxy-report of child anxiety and depressive symptoms indicated that when caregiver proxy-report was high, child self-reported anxiety and depressive symptoms were not associated with functional impairment. At low levels of caregiver proxy-report, child self-reported anxiety and depressive symptoms were positively associated with functional impairment. These findings imply that when caregivers perceive that their child has less frequent anxiety and depressive symptoms, discrepancies between the caregiver and child’s reports may be associated with higher levels of child functional impairment. It is possible that caregiver–child discrepancy may be an indication of poor family functioning or caregiver–child relationships, both of which are factors that may be related to child functional impairment (De Los Reyes & Kazdin, 2005; Van Roy, Groholt, Heyerdahl, & Clench-Aas, 2010). Furthermore, the presence of anxiety and depressive symptoms may affect children’s ability to communicate and therefore affect their caregiver’s ability to assess internalizing symptoms (De Los Reyes, Goodman, Kliewer, & Reid-Quinones, 2008). It may also be important to consider the interaction results in the context of children’s self-reported perceptions of emotional symptoms and caregivers’ perceptions of their child’s emotional symptoms. In our sample, children’s self-reported anxiety and depressive symptoms were higher than those reported by their caregivers. Given that, on average, caregivers underreported child anxiety and depressive symptoms, the child–caregiver discrepant perceptions may be even more prominent and problematic when caregivers report even lower frequency of child anxiety and depressive symptoms.
The accurate assessment of anxiety and depressive symptoms in children with chronic pain can have important clinical and research implications as anxiety and depressive symptomatology and poor emotional functioning may have a significant effect on pain- and treatment-related outcomes (Cunningham et al., 2016; Holley, Wilson, & Palermo, 2017; Vinall et al., 2016). The current findings suggest that caregiver–child discrepant perceptions of child anxiety and depressive symptoms may be associated with functioning in children with chronic pain, a finding that is consistent with other research demonstrating that discordance among caregiver–child reports is associated with poorer child and family outcomes (De Los Reyes & Kazdin, 2005; Ohannessian & Reyes, 2014).
Work within the child psychopathology literature has informed a theoretical model that outlines potential sources of informant discrepancies in child psychopathology assessment. De Los Reyes and Kazdin (2005) proposed the Attribution Bias Context (ABC) Model, which asserts that three factors affect informant discrepancies. Specifically, this model states that variation in informant reports is a result of informant attribution biases (i.e., beliefs about the cause of a child’s behavior), decision thresholds that affect identification or priority of treatment targets, and the assessment context.
Applying the ABC Model to the current study, the internal nature of their child’s anxiety and depressive symptoms may affect caregivers’ ability to recognize that these symptoms may be affecting the child’s behaviors and functioning. Furthermore, caregivers may attribute anxiety- or depression-related behaviors (e.g., avoidance, anhedonia, sleep disturbance) to their child’s chronic pain as opposed to anxiety and/or depression. In addition, the context in which the assessment data were collected (i.e., pediatric chronic pain clinic intake) and children and caregiver’s treatment priorities and concerns (e.g., a desire to receive treatment for physical causes of pain) may have affected discrepant reports. Data from previous research suggest that families presenting to pediatric chronic pain treatment clinics may underreport emotional distress in order to direct assessment and treatment toward more physical causes of the pain and avoid symptoms being labeled as “psychological” (Logan, Claar, & Scharff, 2008; Tran et al., 2016).
The discussion of the current findings should be considered in light of the study limitations. First, the study design and assessment methods limit conclusions surrounding sequential and causal relationships between anxiety and depressive symptoms and functioning and the validity of responses. Specifically, the cross-sectional design limits conclusions about the direction of the emotional symptom–functional disability relationship and does not allow for inferences about the causal effect of caregiver–child discrepancy on functional impairment. Despite the discrepancies observed, most families completed measures at home and caregivers and children may have completed questionnaires together, which could introduce cross-source contamination (Holmbeck et al., 2002). In addition, there may be a concern about shared method variance and shared error across the child self-reported data and within the caregiver–child dyads. This may skew the findings and inflate relationships among the measures. Future work would benefit from utilizing longitudinal designs, multiple informants, and including objective outcomes (e.g., missed school) to assess child functioning and clinical outcomes. The majority of children and caregivers in our sample were female and the sample was homogeneous in terms of race and ethnicity. The data on the effects of child and caregiver gender on informant discrepancies are inconclusive, but some results suggest that gender may play a role in inter-caregiver and caregiver–child discordance (De Los Reyes & Kazdin, 2005). The examination of discrepancies in samples that include a larger proportion of male caregivers and children is needed to ensure the current results are representative of more diverse populations. Racial and ethnic disparities have been documented in pediatric chronic pain research (Nguyen, Ugarte, Fuller, Haas, & Portenoy, 2005) and the lack of diversity within our sample may limit the generalizability of our findings. Children and caregivers from different cultural backgrounds may have different perspectives surrounding the expression of anxiety and depression, and cultural beliefs or practices may affect how children and caregivers communicate about emotional concerns (De Los Reyes & Kazdin, 2005). Child age, sex, widespread pain, and pain intensity were associated with emotional and functional impairment. Although these variables were included as covariates in the regression model, separate analyses exploring demographic effects on discrepancies in a larger, more diverse sample is warranted. Given that child–caregiver agreement with regard to internalizing symptoms may differ from childhood to adolescence (Burrows et al., 2018; Vetter et al., 2014), future work examining discrepancies within specific developmental periods could enhance conclusions surrounding developmental differences in caregiver–child discrepancies.
The current study expands on the caregiver–child discrepancy literature in a pediatric chronic pain sample and utilizes moderation analyses to examine how caregiver–child discrepancies may relate to child functional impairment. Multi-informant assessment is common in pediatric chronic pain research and clinical practices, but guidance surrounding how to address informant discrepancies is limited. In a clinical setting, multiple informant reports may help providers conceptualize the pain condition, but when faced with inconsistent reports, providers may have to base their treatment decisions on one informant’s report. Data indicate that child informants are often deemed unreliable when caregiver–child disagreement exists and when a caregiver endorses more concerns than the child (De Los Reyes, Thomas, Goodman, & Kundey, 2013; Dirks, De Los Reyes, Briggs-Gowan, Cella, & Wakschlag, 2012; Van Doorn, Bodden, Jansen, Rapee, & Granic, 2018). Researchers often address informant discrepancies through examining inter-rater reliability and measurement error and ultimately choose a primary informant for data analyses. To date, limited guidance exists surrounding options for analyzing discrepancies, but researchers have proposed a framework for addressing discrepancies that reflect meaningful information versus measurement error (for a review see De Los Reyes 2013; De Los Reyes, Thomas, et al., 2013). The current findings and broader caregiver–child discrepancy literature suggest that caregiver–child discrepancies may reflect clinically meaningful information. Given that biopsychosocial factors play an important role in the maintenance and treatment of pediatric pain, accurate multi-informant assessment across multiple domains is crucial. As such, further examination of potential implications of caregiver–child discrepancies in pediatric psychology research is warranted. The integration of discrepancy analyses in future longitudinal studies can expand on the current findings to help identify mechanisms of caregiver–child discrepancies and explore how discrepancies affect clinical outcomes. Such data may inform targets for pediatric chronic pain intervention.
Funding
Sarah Martin is funded through a Ruth L. Kirschstein Postdoctoral Individual National Research Service Award Fellowship from the National Heart, Lung, and Blood Institute and National Institutes of Health (F32HL139114, PI: S. Martin). This research was supported by a National Institute of Mental Health grant R01MH063779 (PI: M. Jacob).
Conflicts of interest: None declared.
References
- Achenbach T. M., McConaughy S. H., Howell C. T. (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101, 213.. [PubMed] [Google Scholar]
- Becker S. P., Schindler D. N., Holdaway A. S., Tamm L., Epstein J. N., Luebbe A. M. (2019). The Revised Child Anxiety and Depression Scales (RCADS): Psychometric evaluation in children evaluated for ADHD. Journal of Psychopathology and Behavioral Assessment, 41, 93–106. doi: 10.1007/s10862-018-9702-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker-Haimes E. M., Jensen-Doss A., Birmaher B., Kendall P. C., Ginsburg G. S. (2018). Parent–youth informant disagreement: Implications for youth anxiety treatment. Clinical Child Psychology and Psychiatry, 23, 42–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burrows C. A., Usher L. V., Becker-Haimes E. M., McMahon C. M., Mundy P. C., Jensen-Doss A., Henderson H. A. (2018). Profiles and correlates of parent–child agreement on social anxiety symptoms in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48, 2023–2037. [DOI] [PubMed] [Google Scholar]
- Chorpita B. F., Yim L., Moffitt C., Umemoto L. A., Francis S. E. (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A Revised Child Anxiety and Depression Scale. Behaviour Research and Therapy, 38, 835–855. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Cohen L. L., Lemanek K., Blount R. L., Dahlquist L. M., Lim C. S., Palermo T. M., Weiss K. E. (2008). Evidence-based assessment of pediatric pain. Journal of Pediatric Psychology, 33, 939–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen L. L., Vowles K. E., Eccleston C. (2010). Adolescent chronic pain-related functioning: Concordance and discordance of mother-proxy and self-report ratings. European Journal of Pain, 14, 882–886. [DOI] [PubMed] [Google Scholar]
- Cunningham N. R., Jagpal A., Tran S. T., Kashikar-Zuck S., Goldschneider K. R., Coghill R. C., Lynch-Jordan A. M. (2016). Anxiety adversely impacts response to cognitive behavioral therapy in children with chronic pain. The Journal of Pediatrics, 171, 227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A. (2011). Introduction to the special section: more than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology, 40, 1–9. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A. (2013). Strategic objectives for improving understanding of informant discrepancies in developmental psychopathology research. Development and Psychopathology, 25, 669–682. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A., Goodman K. L., Kliewer W., Reid-Quinones K. (2008). Whose depression relates to discrepancies? Testing relations between informant characteristics and informant discrepancies from both informants’ perspectives. Psychological Assessment, 20, 139.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A., Kazdin A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131, 483.. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A., Salas S., Menzer M. M., Daruwala S. E. (2013). Criterion validity of interpreting scores from multi-informant statistical interactions as measures of informant discrepancies in psychological assessments of children and adolescents. Psychological Assessment, 25, 509.. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A., Thomas S. A., Goodman K. L., Kundey S. M. A. (2013). Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology, 9, 123–149. doi: 10.1146/annurev-clinpsy-050212-185617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirks M. A., De Los Reyes A., Briggs-Gowan M., Cella D., Wakschlag L. S. (2012). Embracing not erasing contextual variability in children’s behavior: theory and utility in the selection and use of methods and informants in developmental psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53, 558.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C., Bernstein A., Chorpita B. F., Weisz J. R. (2012). A transportable assessment protocol for prescribing youth psychosocial treatments in real-world settings: Reducing assessment burden via self-report scales. Psychological Assessment, 24, 141.. [DOI] [PubMed] [Google Scholar]
- Ebesutani C., Chorpita B. F., Higa-McMillan C. K., Nakamura B. J., Regan J., Lynch R. E. (2011). A psychometric analysis of the Revised Child Anxiety and Depression Scales—Parent version in a school sample. Journal of Abnormal Child Psychology, 39, 173–185. doi: 10.1007/s10802-010-9460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdfelder E., Faul F., Buchner A. (1996). GPOWER: A general power analysis program. Behavior Research Methods, Instruments, & Computers, 28, 1–11. [Google Scholar]
- Evans S., Djilas V., Seidman L. C., Zeltzer L. K., Tsao J. C. (2017). Sleep quality, affect, pain, and disability in children with chronic pain: Is affect a mediator or moderator? The Journal of Pain, 18, 1087–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaultney A., Bromberg M., Connelly M., Spears T., Schanberg L. (2017). Parent and child report of pain and fatigue in JIA: Does disagreement between parent and child predict functional outcomes? Children, 4, 11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauntlett-Gilbert J., Eccleston C. (2007). Disability in adolescents with chronic pain: Patterns and predictors across different domains of functioning. Pain, 131, 132–141. [DOI] [PubMed] [Google Scholar]
- Holley A. L., Wilson A. C., Palermo T. M. (2017). Predictors of the transition from acute to persistent musculoskeletal pain in children and adolescents: A prospective study. Pain, 158, 794–801. doi: 10.1097/j.pain.0000000000000817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G. N. (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27, 87–96. [DOI] [PubMed] [Google Scholar]
- Holmbeck G. N., Li S. T., Schurman J. V., Friedman D., Coakley R. M. (2002). Collecting and managing multisource and multimethod data in studies of pediatric populations. Journal of Pediatric Psychology, 27, 5–18. doi: 10.1093/jpepsy/27.1.5 [DOI] [PubMed] [Google Scholar]
- Karlson C. W., Baker A. M., Bromberg M. H., David Elkin T., Majumdar S., Palermo T. M. (2017). Daily pain, physical activity, and home fluid intake in pediatric sickle cell disease. Journal of Pediatric Psychology, 42, 335–344. doi:10.1093/jpepsy/jsw061 [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Flowers S. R., Claar R. L., Guite J. W., Logan D. E., Lynch-Jordan A. M., Wilson A. C. (2011). Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain, 152, 1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Lynch A. M., Slater S., Graham T. B., Swain N. F., Noll R. B. (2008). Family factors, emotional functioning, and functional impairment in juvenile fibromyalgia syndrome. Arthritis and Rheumatism, 59, 1392–1398. doi: 10.1002/art.24099 [DOI] [PubMed] [Google Scholar]
- Kim C., Choi H., Ko H., Park C. G. (2018). Agreement between parent proxy reports and self-reports of adolescent emotional distress. The Journal of School Nursing, 2, 125–134. doi: 10.1177/1059840518792073 [DOI] [PubMed] [Google Scholar]
- King S., Chambers C. T., Huguet A., MacNevin R. C., McGrath P. J., Parker L., MacDonald A. J. (2011). The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain, 152, 2729–2738. [DOI] [PubMed] [Google Scholar]
- Laird R. D., De Los Reyes A. (2013). Testing informant discrepancies as predictors of early adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology, 41, 1–14. [DOI] [PubMed] [Google Scholar]
- Laird R. D., Weems C. F. (2011). The equivalence of regression models using difference scores and models using separate scores for each informant: Implications for the study of informant discrepancies. Psychological Assessment, 23, 388.. [DOI] [PubMed] [Google Scholar]
- Liossi C., Howard R. F. (2016). Pediatric chronic pain: Biopsychosocial assessment and formulation. Pediatrics, 138, e20160331.. [DOI] [PubMed] [Google Scholar]
- Logan D. E., Claar R. L., Scharff L. (2008). Social desirability response bias and self-report of psychological distress in pediatric chronic pain patients. Pain, 136, 366–372. [DOI] [PubMed] [Google Scholar]
- Miró J., Castarlenas E., Huguet A. (2009). Evidence for the use of a numerical rating scale to assess the intensity of pediatric pain. European Journal of Pain, 13, 1089–1095. [DOI] [PubMed] [Google Scholar]
- Nguyen M., Ugarte C., Fuller I., Haas G., Portenoy R. K. (2005). Access to care for chronic pain: Racial and ethnic differences. The Journal of Pain, 6, 301–314. [DOI] [PubMed] [Google Scholar]
- Ohannessian C. M., Reyes A. D. L. (2014). Discrepancies in adolescents’ and their mothers’ perceptions of the family and adolescent anxiety symptomatology. Parenting, 14, 1–18. doi: 10.1080/15295192.2014.870009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran S. T., Jastrowski Mano K. E., Anderson Khan K., Davies W., Hainsworth K. R. (2016). Patterns of anxiety symptoms in pediatric chronic pain as reported by youth, mothers, and fathers. Clinical Practice in Pediatric Psychology, 4, 51. [Google Scholar]
- Trent L. R., Buchanan E., Ebesutani C., Ale C. M., Heiden L., Hight T. L., Young J. (2013). A measurement invariance examination of the Revised Child Anxiety and Depression Scale in a southern sample: Differential item functioning between African American and Caucasian Youth. Assessment, 20, 175–187. doi: 10.1177/1073191112450907 [DOI] [PubMed] [Google Scholar]
- Van Doorn M. M., Bodden D., Jansen M., Rapee R. M., Granic I. (2018). Linking mother–child discrepancies to behavioral observations of children’s anxiety. Child & Youth Care Forum, 47, 481–498. [Google Scholar]
- Van Roy B., Groholt B., Heyerdahl S., Clench-Aas J. (2010). Understanding discrepancies in parent-child reporting of emotional and behavioural problems: effects of relational and socio-demographic factors. BMC Psychiatry, 10, 56.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni J. W., Thissen D., Stucky B. D., Liu Y., Magnus B., He J., DeWalt D. A. (2015). Item-level informant discrepancies between children and their parents on the PROMIS® pediatric scales. Quality of Life Research, 24, 1921–1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetter T. R., Bridgewater C. L., Ascherman L. I., Madan-Swain A., McGwin G. L. (2014). Patient versus parental perceptions about pain and disability in children and adolescents with a variety of chronic pain conditions. Pain Research and Management, 19, 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinall J., Pavlova M., Asmundson G. J., Rasic N., Noel M. (2016). Mental health comorbidities in pediatric chronic pain: A narrative review of epidemiology, models, neurobiological mechanisms and treatment. Children, 3, 40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker L. S., Greene J. W. (1991). The functional disability inventory: Measuring a neglected dimension of child health status. Journal of Pediatric Psychology, 16, 39–58. [DOI] [PubMed] [Google Scholar]
- Walker S. M. (2008). Pain in children: Recent advances and ongoing challenges. BJA: British Journal of Anaesthesia, 101, 101–110. doi: 10.1093/bja/aen097 [DOI] [PubMed] [Google Scholar]
- Walter J. G., Kahn S. A., Noe J. D., Schurman J. V., Miller S. A., Greenley R. N. (2016). Feeling fine: Anxiety and depressive symptoms in youth with established IBD. Inflammatory Bowel Diseases, 22, 402–408. doi: 10.1097/MIB.0000000000000657 [DOI] [PubMed] [Google Scholar]


