Abstract
Background
Self-medication plays a key role in public health as it influences both negatively and positively on the health of individuals and the existing healthcare systems. This is especially the case during public health emergencies like the 2019 SARS-CoV-2 disease.
Objectives
The study aimed at assessing the prevalence of self-medication before and during the outbreak of COVID-19 pandemic among healthcare workers and its associated factors.
Methods
Stratified sampling was used to select 379 study respondents. The authors developed an online questionnaire, pretested and submitted to various online professional groups of different cadres of healthcare workers. Collected data was analysed using descriptive and inferential statistics. The data was presented in tables, graphs, percentages, and cross-tabulation with different variables. Multivariable logistic regression was used to ascertain factors that influence an individual’s desire to self-medicate and associations were considered significant at p < 0.05.
Results
The overall prevalence of self-medication increased from 36.2% (n = 137) before the pandemic to 60.4% (n = 229) during the pandemic. The respondents' gender, level of education, age, marital status, participation in physical activity, and drug reaction events, were significantly associated with self-medication before and during the outbreak (P < 0.05). Multivariable logistic regression analyses showed that participants engaging in physical activities, working during the day and being healthy were less likely to self-medicate (p < 0.01).
Conclusion
Self-medication is an important health issue, especially during the COVID-19 pandemic. Continuous awareness creation and sensitization could help in reducing self-medication practices among healthcare workers.
Keywords: Self-medication, Prevalence, Healthcare workers, 2019 SARS-CoV-2, Kenya, COVID-19
1. Introduction
Self-medication also known as self-care and/or self- administration of medication is a common practice across the world (Hughes et al., 2001). It involves situations where individuals, families, and/or communities take medicines to treat health conditions or symptoms without prescription or diagnosis from a qualified healthcare professional (Adolfo et al., 2000, Bennadi, 2014, Ruiz, 2010). Although self-medication has been practiced in many generations (Huffman, 2001), it is becoming a significant area of interest in healthcare research as it gives individuals with minor ailments freedom to make independent choices on how to manage their own health and wellbeing (Hughes et al., 2001). Research has demonstrated that there are a number of merits attributed to self-medication, such as improved access to medicines, especially over-the-counter drugs, which eases the burden levied to physicians and pharmacists in dealing with minor illnesses (Powis et al., 1996).
Studies have shown that although self-medication empowers individuals and communities to take control of their wellness, it has been associated with medical challenges (Mandal, 2015), which may have adverse impacts on their lives. This has been attributed to uninformed acts such as incorrect dosage, incorrect diagnosis of a particular health condition and improper route of administration of the self-medicated drugs. In addition, they may be using medicines for longer than the recommended time by the manufacturers, with a possibility of developing risk of dependence leading to abuse, improper storage of drugs, inappropriate choice of drug therapy, and increased prevalence of pathogenic resistance to drugs as some of the adverse effects (Menary et al., 2011).
Consumption of drugs without a prescription is triggered by factors such as the availability of drugs, easy access to drugs without time limits, improved supply of different varieties of medicines at affordable prices, and convenience in access to drugs compared to seeking treatment in the healthcare facilities (Smith, 1996).
A recently published google trends study on the interest in self-medication during COVID-19 pandemic indicated an upward trend. The study showed an increase in the number of searches for self-medication worldwide since the pandemic was declared, and this would be an indication of increased interests in self-medication across the globe (Onchonga, 2020).
Self-medication is commonly practised in countries where human resources for health are constrained. Mostself-medication practices are triggered by relatively long waiting time in the health facilities, difficulties in securing an appointment with physicians, frequent closures of health facilities, recurrent stock-outs of essential medicines, and delays in getting treatment during emergencies (Parulekar et al., 2016).
For healthcare workers, research has revealed that the circumstances and the environment in which they work predisposes them to accessing drugs during their routine work. Although majority of the healthcare workers may be knowledgeable about the dangers posed as a result of self-medication, most of them find solace in self-medication especially when faced with work-related stress, pressure, discomfort, and anxiety (Omolase et al., 2011, Rotenberg, 2009).
Currently, the world is struggling with COVID-19 pandemic (Lai et al., 2020, Weiss and Leibowitz, 2011, Zu et al., 2020), which has been declared a global public health emergency (WHO, 2020). Due to its fast spread, the disease has threatened lives and caused psychological distress and anxiety to both healthcare workers and the general public in many parts of the world (Holmes, 2003). This situation has complicated the already fragile healthcare systems in resource-limited settings, especially those offering maternal and child health services (Onchonga et al., 2020, Onchonga et al., 2020). The focus has shifted to combating the pandemic; thereby curtailing the strides made in other healthcare indicators.
The current situation has been exacerbated by inadequacies in healthcare infrastructure, essential medical equipment in health facilities and inadequate health workforce. As a result, the available workers are forced to work for long hours, sometimes under difficult circumstances (Bogren et al., 2019), which prompts them to self-medicate to relieve the discomfort and anxiety attributed to burnouts.
This cross-sectional study was designed to investigate the pattern of self-medication among healthcare workers before and during the 2019 COVID-19 pandemic. The objectives of the study included: (a) to evaluate the prevalence of self-medication reported by healthcare workers before and during the outbreak, (b) to identify the common conditions for self-medication among healthcare workers before and during the outbreak, and (c) to investigate the sociodemographic characteristics and health patterns associated with self-medication among different cadres of healthcare workers before and during the outbreak. It was envisaged that the results would inform healthcare policy makers on measures to put in place to improve the well-being of healthcare workers as they strive to save lives.
2. Methods
2.1. Study design
This was part of a larger study that was conducted in Kenya on the effect of COVID-19 pandemic. The study population consisted of 385 healthcare workers that were directly involved in the management and control of COVID-19 disease pandemic. The study employed stratified sampling. Various cadres of healthcare professionals were used as strata. An online questionnaire was developed, pretested, revised, and sent to different healthcare professionals' online groups and platforms such as WhatsApp, Messenger, and Facebook. From each stratum, data was collected through random sampling of the received questionnaires until the required sample was achieved. The shared questionnaire was made anonymous to ensure data confidentiality and reliability.
2.2. Data collection
A questionnaire was developed by the investigators, which contained respondents' sociodemographic characteristics such as age, marital status, gender, level of education, religion, and cadre. Moreover, it contained questions on the prevalence of self-medication before and during the outbreak, conditions treated for self-medication before and during the outbreak, reasons for preferring self-medication before and during the outbreak, respondent's attitude regarding self-medication, and knowledge and perceptions regarding self-medication before and during the outbreak. Adverse drug reaction experiences were also investigated.
2.3. Data analysis and presentation
Collected data was analysed using the Statistical Package Programme for Social Science (SPSS) version 23.0.0. by IBM. Data was analysed and summarized using descriptive and inferential statistics, and later presented in tables, graphs, percentages, and cross-tabulation. Multivariable logistic regression analyses were used to ascertain factors that influence an individual's desire to self-medicate, and associations were considered significant at p < 0.05.
2.4. Ethical approvals
The approval to conduct this research was obtained from the Jaramogi Oginga Odinga Teaching and Referral Hospital Ethical Review Committee (IERC/JOOTRH/209/20). All the respondents were well-versed on the study intentions and were required to consent before admission to the study.
3. Results
3.1. Sociodemographic characteristics of the respondents
Out of a targeted sample of 385 respondents, approximately 98.4% (n = 379) questionnaires were correctly filled and returned. A total of 14 cadres participated in the study where; 30.6% (n = 116) were nurses. Regarding the gender of participants, 51.5% (n = 195) were female and 91.3% (n = 346) were Christians. About 65.4% (n = 248) were married and 59.6% (n = 226) had a university degree as shown in Table 1.
Table 1.
Socio-demographic characteristics of respondents before and during COVID-19 Outbreak.
| Socio-demographic variable | N | (%) | |
|---|---|---|---|
| Gender | Female | 195 | 51.5 |
| Male | 184 | 48.5 | |
| Education | College diploma | 153 | 40.4 |
| University Degree | 226 | 59.6 | |
| Age | 18–30 | 128 | 33.8 |
| 31–40 | 159 | 42.0 | |
| 41–50 | 72 | 19.0 | |
| 51–60 | 20 | 5.3 | |
| Religion | Christian | 346 | 91.3 |
| Muslim | 17 | 4.5 | |
| Hindu | 4 | 1.1 | |
| Traditional | 2 | 0.5 | |
| No religion | 10 | 2.6 | |
| Marital status | Single | 131 | 34.6 |
| Married | 248 | 56.4 | |
| Geographical location | Rural | 99 | 21.6 |
| Peri-urban | 112 | 29.6 | |
| Urban | 168 | 44.3 | |
| Place of work | Public Health Facility | 260 | 68.6 |
| Private practice | 75 | 19.8 | |
| NGO | 36 | 9.5 | |
| Pharmaceutical company | 8 | 2.1 | |
| Cadre | Public Health Officers | 86 | 22.7 |
| Nursing Officer | 116 | 30.6 | |
| Clinical Officers | 13 | 3.4 | |
| Pharmacy/Technologists | 67 | 17.7 | |
| Medical Officers | 22 | 5.8 | |
| Community Health Assistants | 16 | 4.2 | |
| Nutritionists | 10 | 2.6 | |
| Laboratory Scientists/Technicians | 14 | 3.7 | |
| Physiotherapist | 5 | 1.3 | |
| Medical Consultants | 8 | 2.1 | |
| Medical Registrars | 9 | 2.4 | |
| Radiologists | 6 | 1.6 | |
| Health Records Information | 2 | 0.5 | |
| Dentist/ Dental Technologists | 5 | 1.3 | |
3.2. Prevalence and reported reasons for self-medication
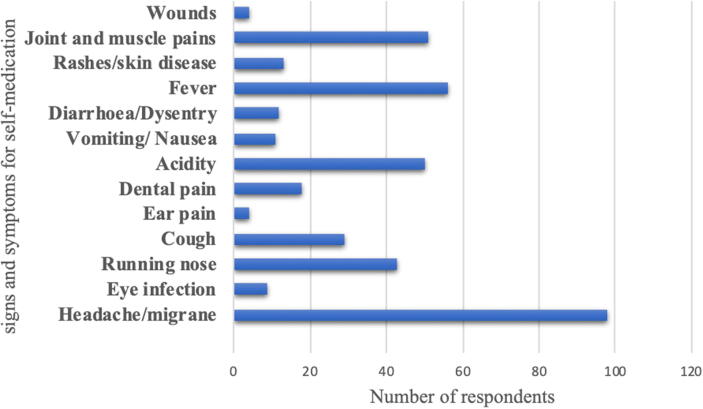
In this study, 50.9% (n = 193) reported having felt unwell in the last three weeks preceding the interview. Approximately 60.4% (n = 229) reported having taken medicines without a doctor's prescription in the last 21 days preceding the study. This was a 24.3% increase since those who had self-medicated before the COVID-19 outbreak were 36.1% (n = 137). The respondents were also asked about the conditions that necessitated self-medication. Approximately 42% (n = 139) mentioned headache and migraine, 15% (n = 51) indicated joint and muscle pains, and 13% (n = 43) mentioned running nose (Fig. 1). There were no differences on the conditions that necessitated self-medication before and during the outbreak.
Fig. 1.
Conditions for self-medication before and during COVID-19 Outbreak.
3.3. Perceptions of the respondents regarding their health status
About 19.8% (n = 75) of the respondents reported to be in perfect health, 74.7% (n = 238) had good health, and 5.5% (n = 21) had average or poor health status. Just about 90% (n = 341) of the respondents did not have any known psychiatric conditions, while 77.6% (n = 294) were actively participating in physical activities. Sleeping patterns were also investigated. About 14.8% (n = 56) of the respondents reported sleeping for more than eight hours a day, 79.9% (n = 303) had a sleeping pattern of between five and eight hours a day, and 5.3% (n = 20) had a sleeping pattern of below four hours a day. There were no differences in sleeping patterns before and during the outbreak.
3.4. Relationship between sociodemographic characteristics and self-medication
Chi-square test was conducted to compare self-medication before and during the outbreak with sociodemographic variables. The results showed statistically significant differences between self-medication and gender, physical activity, adverse drug reaction, work shift, marital status, level of education, and cadre.
There was no statistical significance between self-medication and residency of respondents, health status, psychiatric condition, place of work, and sleeping patterns (Table 2).
Table 2.
Relationship between Demographic Variables and Self-Medication before and during COVID-19 Outbreak.
| Socio-demographic | Self-medication Self-medication during COVID-19 before COVID-19 |
χ2 | p value | ||
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| 1. Gender | Female | 129(56.3) | 66(44.0) | 5.518 | 0.019 |
| Male | 100(43.7) | 84(56.0) | |||
| 2. Education | College Diploma | 83(36.2) | 70(46.7) | 4.090 | 0.043 |
| University | 146(63.8) | 80(53.3) | |||
| 3. Age | 18–30 | 69(30.1) | 59(39.3) | 10.592 | 0.014 |
| 31–40 | 111(48.5) | 48(32.0) | |||
| 41–50 | 37()16.2 | 35(23.3) | |||
| 51–60 | 12(5.2) | 8(5.4) | |||
| 4. Marital status | Single | 119(52.0) | 32(21.3) | 36.606 | 0.000 |
| Married | 110(48.0) | 118(78.7) | |||
| 5. Geographical location | Rural | 57(24.9) | 42(28.0) | 1.353 | 0.509 |
| Peri-urban | 65(28.4) | 47(31.3) | |||
| Urban | 107(46.7) | 61(40.7) | |||
| 6. Physical activity | Yes | 181(79.0) | 48(21.0) | 9.578 | 0.002 |
| No | 97(64.7) | 53(35.3) | |||
| 7. Drug reaction event | Yes | 135(59.0) | 94(41.0) | 14.759 | 0.000 |
| No | 117(78.0) | 33(22.0) | |||
| 8. Health status | Perfect health | 38(16.6) | 37(24.7) | 3.860 | 0.145 |
| Good health | 177(77.3) | 106(70.7) | |||
| Average health | 14(6.1) | 7(4.7) | |||
| 9. Psychiatric condition | Yes | 205(89.5) | 24(10.5) | 0.132 | 0.716 |
| No | 136(90.7) | 14(9.3) | |||
| 10. Sleeping pattern | More than 8 hrs | 28(12.2) | 28(18.7) | 3.523 | 0.172 |
| 5–8 hrs | 187(81.7) | 116(77.3) | |||
| 1–4 hrs | 14(6.1) | 6(4.0) | |||
3.5. Regression analysis of the factors prompting respondents to self-medication
The study applied multivariable logistic regression analyses to ascertain factors influencing an individual's desire to self-medicate. The respondents that undertook physical activity, worked on day shift and were healthy; were less likely to self-medicate (p < 0.01). Variables such as gender, drug reaction, reading drug instructions before use, level of education, having a known psychiatric condition, and perceived health status did not correlate with self-medication (Table 3).
Table 3.
Multivariable logistic regression analyses on influencing factors of self-medication during the COVID-19 outbreak.
| Independent variables (n = 379) | B | S.E. | Wald X2 | P | Exp(B) | (95% CI) |
|---|---|---|---|---|---|---|
| Physical activity (Yes/No) | −1.160 | 0.356 | 10.615 | 0.001 | 0.313 | (0.156,0.630) |
| Gender (Female/Male) | −0.081 | 0.308 | 0.069 | 0.793 | 0.922 | (0.504,1.687) |
| Drug reaction event (Yes/No) | −0.469 | 0.338 | 1.929 | 0.165 | 0.625 | (0.322,1.213) |
| Work shift (Night/Day) | −4.414 | 1.155 | 14.597 | 0.000 | 0.012 | (0.001,0.117) |
| Reading prescription (All the time/Sometimes/Not at all) | −0.105 | 0.626 | 0.028 | 0.866 | 0.900 | (0.264,3.070) |
| Level of education (Diploma/Degree) | 0.890 | 0.340 | 6.832 | 0.009 | 2.434 | (1.249,4.743) |
| Any known psychiatric condition (Yes/No) | 0.169 | 0.519 | 0.106 | 0.745 | 1.184 | (0.428,3.274) |
| Health status (Perfect /Good/Average) | 0.701 | 0.716 | 0.960 | 0.327 | 2.016 | (0.496,8.201) |
| Feeling unwell in the last 3 weeks (Yes/No) | −2.587 | 0.346 | 55.910 | 0.000 | 0.075 | (0.038,1.48) |
| Constant | −20.099 | 40193.683 | 0.000 | 1.000 | 0.000 |
3.6. Respondent's knowledge and practices regarding self-medication before and during the outbreak
The number of respondents who read the manufacturer's manual/leaflet all the time before purchasing medicines increased from 58.8% (n = 223) before the outbreak to 72% (n = 273) while those who did not read at all reduced from 5.1% (n = 19) before the outbreak to 1% (n = 4) during the outbreak. About 70.4% (n = 267) of the respondents noted that self-medication was not safe. Regarding the route of administration of the purchased medicine, dosage, and side effects, there was an increase in knowledge from 69.4% (n = 263) before the outbreak to 75% (n = 284) during the outbreak, an indication of an increase in knowledge regarding the route of administration of the purchased medicines.
3.7. Consideration for self-medication
About 31.1% (n = 118) considered the brand of the medicine, 18.5% (n = 70), the pharmaceutical company manufacturing the medicine, while 17.4% (n = 66) considered the cost. Access to self-medication changed significantly before and during the outbreak. About 16.9% (n = 64) obtained the medicines from the primary health facility, 56.5% (n = 214) from pharmacy stores while 26.6% (n = 101) from hospital pharmacies before the outbreak, while, 89.5% (n = 340) obtained medication from pharmacy stores and only10.5% (n = 39) from primary health facilities. None of the respondents obtained medication from hospital pharmacies during the outbreak.
3.8. Adverse drug reaction (ADR) following self-medication
Among the respondents who self-medicated, 22.4% (n = 85) had experienced perceived adverse drug reaction during the outbreak. There was a noteworthy association between self-medication and adverse drug reaction during the outbreak (X2 = 4.479, p = 0.034). Further, there was a significant association between taking drugs for chronic illness and experiencing adverse drug reactions during the outbreak (X2 = 4.897, p = 0.02), with results suggesting that those taking drugs for chronic illness during the outbreak were more likely to develop adverse drug reactions. Adverse drug effects prompted approximately 60.8%(n = 62) to stop self- medication (Table 4). The study did not find any significant association between self-medication and adverse drug reaction before the outbreak of COVID-19.
Table 4.
Action taken following adverse drug reaction event during COVID-19 outbreak.
| Action taken after adverse drug reaction event | N | (%) |
|---|---|---|
| Went to a private doctor | 12 | 11.8 |
| Went to primary health centre | 17 | 16.7 |
| Went to a pharmacist | 11 | 10.8 |
| Stopped taking the medicine | 62 | 60.8 |
3.9. The opinion of respondents regarding self-medication and COVID-19 disease
Of the 379 respondents, 214 (64.3%) believed that the COVID-19 pandemic had necessitated self-medication. About 55.9% (n = 212) reported that they would continue with self-medication post-COVID-19 pandemic. When asked about their opinion regarding self-medication and the outbreak, approximately 84.1% (n = 280) reported that the pandemic had increased the desire for self-medication for the general public. On a positive note, 91.3% (n = 304) would not advise other people to self-medicate.
4. Discussion
This study was conducted during the COVID-19 pandemic to investigate the prevalence of self-medication and associated factors among healthcare workers in Kenya before and during outbreak. The prevalence of self-medication had increased from 36.2% before the outbreak to 60.4%, during the outbreak. These results were close to the findings from a similar study undertaken in Nigeria (Bamgboye et al., 2006). In the current study, an analysis was done to determine the prevalence of self-medication across different cadres of healthcare workers, and the nursing officers reported a prevalence of 32.8% during the outbreak. This finding is similar to a study conducted in Brazil on the prevalence of self-medication among nurses (Rotenberg, 2009).
In the current study, several considerations for the preference of particular drugs for self-medication were evaluated. The brand of the medicine, cost, and the manufacturing company were the primary considerations. This, too, has been found in similar studies (Selvaraj and Ramalingam, 2014). The majority of the respondents took medicines for pain relief, more specifically headaches, migraine, fever, joint and muscle pains before and during the outbreak. Similar conditions have been documented as a common reason for self-medication (Auta et al., 2012).
Self-medication was significantly associated with the level of education as those with degrees were more likely to self-medicate both before and during the outbreak. These findings agree with similar studies (López and Dennis, 2009), and this has been attributed to the vast knowledge on the medication as most medical graduates do possess a higher level of understanding of the over-the-counter drugs, including their prescription and side effects. Of note was that some studies have given divergent results regarding this finding. A similar study (Sharma et al., 2005) reported that self-medication was higher among respondents who had secondary education and below compared to those with advanced education.
In the current study, gender was statistically significant. More female participants were likely to self- medicate before and during the outbreak. However, similar studies from other regions (Bennadi, 2014, Shankar et al., 2002) have shown that male healthcare workers are more likely to self-medicate than their female counterparts (Belachew Gutema et al., 2011, Sawalha, 2007). In this study, participants who engaged in physical activity were less likely to self-medicate both before and during the outbreak. This finding agrees with existing evidence on physical activity and self-medication (Wijesinghe et al., 2012).
The study participants were all working in healthcare institutions where access to medical care was guaranteed as all the respondents had a medical insurance cover. However, this did not deter them from preferring self-medication. This study agrees with similar studies that have shown that open access to healthcare does not significantly reduce self-medication (Osaboro et al., 2013).
In addition, it was noted that work shifts triggered self-medication; those working at night were more likely to self-medicate both before and during the outbreak. Similar studies have indicated that most healthcare workers on night shift tend to self-medicate as a result of unfavourable working conditions, and working for long hours with minimum rest, which may contribute to lassitude (Rotenberg, 2009).
The findings from multivariable logistic regression analyses showed that the respondents who undertook physical activity, worked during the day, and those who were healthy, correlated well with the prevalence of self-medication (p < 0.01). Similar studies conducted in other regions have shown similar results (Lei et al., 2018).
5. Study limitations
This study was restricted to healthcare workers who were currently actively involved in managing the COVID-19 pandemic and had self-medicated 21 days preceding the interview. Therefore, there is a possibility of recall bias. Also, cross-sectional studies do not permit an establishment of a clear cause and effect.
6. Conclusion
Self-medication is a significant health issue, especially during COVID-19 pandemic, and a refresher course in the form of continued medical education (CME) should be encouraged. Awareness creation is also needed, not only to the healthcare workers but also to the general public; especially on the risks involved since the potential danger of self-medication might be underestimated during emergencies. There is need to undertake a study on how ethnic differences, and religious beliefs would influence self- medication among healthcare workers.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors
CRediT authorship contribution statement
David Onchonga: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft, Supervision. Joshua Omwoyo: Visualization, Investigation, Software, Validation, Writing - original draft. Duke Nyamamba: Writing - review & editing, Formal analysis, Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
David Onchonga, Email: onchonga.david@etk.pte.hu.
Joshua Omwoyo, Email: joshu2064@gmail.com.
Duke Nyamamba, Email: nyamamba1@gmail.com.
References
- Adolfo F., Caamano F., Gestal-Otero J.J. Sociodemographic factors related to self-medication in Spain. Eur. J. Epidemiol. 2000;16:19–26. doi: 10.1023/A:1007608702063. [DOI] [PubMed] [Google Scholar]
- Auta A., Omale S., Folorunsho T.J., David S., Banwat S.B. Medicine vendors: Self-medication practices and medicine knowledge. N. Am. J. Med. Sci. 2012;4(1):24–28. doi: 10.4103/1947-2714.92899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamgboye E.A., Amoran O.E., Yusuf O.B. Self medication practices among workers in a tertiary hospital in Nigeria. Afr. J. Med. Med. Sci. 2006;35(4):411–415. 17722805. [PubMed] [Google Scholar]
- Belachew Gutema G., Alemayehu Gadisa D., Fikadu Berhe D., Hadgu Berhe A., Ghezu Hadera M., Solomon Hailu G., Gebresamuel Abrha N., Yarlagadda R., Wondimu Dagne A., Abebe Kidanemariam Z. Self-medication practices among health sciences students: The case of Mekelle University. J. Appl. Pharm. Sci. 2011;1(10):183–189. [Google Scholar]
- Bennadi D. Self-medication: A current challenge. J. Basic Clin. Pharm. 2014;5(1):19–23. doi: 10.4103/0976-0105.128253. 24808684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogren M.U., Erlandsson K., Byrskog U., Bogren M., Johansson A., Kalid M., Igal A.A., Mohamed J., Said F., Pedersen C., Osman F. Health workforce perspectives of barriers inhibiting the provision of quality care in Nepal and Somalia-A qualitative study. Sex. Reprod. Healthc. 2019;23 doi: 10.1016/j.srhc.2019.100481. [DOI] [PubMed] [Google Scholar]
- Holmes K.V. SARS coronavirus: a new challenge for prevention and therapy. J Clin Invest. 2003;111(11):1605–1609. doi: 10.1172/JCI18819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osaboro E., Clement C.A., Adebola O.E., Ejike B.E., Laura E., Ikechukwu U.M. Self-medication practices among dental, midwifery and nursing students. Eur. J. Gen. Dent. 2013;2(1):54–57. doi: 10.4103/2278-9626.106813. [DOI] [Google Scholar]
- Huffman M.A. Self-Medicative Behavior in the African Great Apes: An Evolutionary Perspective into the Origins of Human Traditional Medicine: In addition to giving us a deeper understanding of our closest living relatives, the study of great ape self-medication provides a window into the origins of herbal medicine use by humans and promises to provide new insights into ways of treating parasite infections and other serious diseases. BioScience. 2001;51(8):651–661. doi: 10.1641/0006-3568(2001)051[0651:SMBITA]2.0.CO;2. [DOI] [Google Scholar]
- Hughes C.M., McElnay J.C., Fleming G.F. Benefits and risks of self medication. Drug Safety. 2001;24:1027–1037. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei X., Jiang H., Liu C., Ferrier A., Mugavin J. Self-medication practice and associated factors among residents in Wuhan, China. Int. J. Environ. Res. Public Health. 2018;15(1) doi: 10.3390/ijerph15010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López, J.J., Dennis, R.M.S., 2009. A study of self-medication in a neighborhood in Bogotá. Rev. Salud Pública 11 (3) 432-442. URL: http://www.scielo.org.co/scielo.php?pid=S0124-00642009000300012&script=sci_arttext&tlng=en (accessed 5.20.20) [DOI] [PubMed]
- Mandal S. Can over-the-counter antibiotics coerce people for self-medication with antibiotics? Asian Pacific J. Trop. Dis. 2015;5(1):S184–S186. doi: 10.1016/S2222-1808(15)60886-6. [DOI] [Google Scholar]
- Menary K.R., Kushner M.G., Maurer E., Thuras P. The prevalence and clinical implications of self-medication among individuals with anxiety disorders. J. Anxiety Disord. 2011;25(3):335–339. doi: 10.1016/j.janxdis.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omolase C.O, Adeleke O.E, Afolabi A.O, Ofolabi O.T. Self medication amongst general outpatients in a Nigerian community hospital. Ann. Ibadan Postgrad. Med. 2011;5(2):64–67. doi: 10.4314/aipm.v5i2.64032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onchonga D. A Google Trends study on the interest in self-medication during the 2019 novel coronavirus (COVID-19) disease pandemic. Saudi Pharm. J. 2020;28(7):903–904. doi: 10.1016/j.jsps.2020.06.007. 32641903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onchonga D., MoghaddamHosseini V., Keraka M., Várnagy Á. Prevalence of fear of childbirth in a sample of gravida women in Kenya. Sex. Reprod. Healthc. 2020;24 doi: 10.1016/j.srhc.2020.100510. [DOI] [PubMed] [Google Scholar]
- Onchonga D., Várnagy Á., Keraka M., Wainaina P. Midwife-led integrated pre-birth training and its impact on the fear of childbirth. A qualitative interview study. Sex. Reprod. Healthc. 2020;25 doi: 10.1016/j.srhc.2020.100512. [DOI] [PubMed] [Google Scholar]
- Parulekar M., Mekoth N., Ramesh C.M., Parulekar A. Self-medication in developing countries a systematic review. J. Pharm. Technol. Res. Manage. 2016;4(2):103–127. doi: 10.15415/jptrm.2016.42007. [DOI] [Google Scholar]
- Rotenberg, A.R.R.B.R.H.G.L., 2009. Self-medication among nursing workers from public hospitals [WWW Document]. https://doi.org/https://doi.org/10.1590/S0104-11692009000600014 [DOI] [PubMed]
- Powis M.G., Rogers P.J., Wood SM. United Kingdom Community Pharmacists’ Views on Recent “POM-to-P” Switched Medicines. Soc. Admin. Pharm. 1996;13:188–197. [Google Scholar]
- Ruiz M. Risks of self-medication practices. Curr. Drug Saf. 2010;5:315–323. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
- Sawalha A.F. Assessment of Self-Medication Practice among University Students in Palestine: Therapeutic and Toxicity Implications. The Islamic University Journal. 2007;15(2) [Google Scholar]
- Selvaraj K., Ramalingam G.K.S.A. Prevalence of self‐medication practices and its associated factors in Urban Puducherry. India. 2014;5(1):32–36. doi: 10.4103/2229-3485.124569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar P.R., Partha P., Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: A questionnaire-based study. BMC Fam. Pract. 2002;3(17):1–7. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma R., Verma U., Sharma C.L, Kapoor B. Self-medication among urban population of Jammu city. Indian J. Pharmacol. 2005;37(1):40–43. doi: 10.4103/0253-7613.13856. [DOI] [Google Scholar]
- Smith S.K. Over the counter drugs. BMJ. 1996;312:593. doi: 10.1136/bmj.312.7031.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss S.R., Leibowitz J.L. Vol. 81. Academic Press Inc.; 2011. Coronavirus pathogenesis; pp. 85–164. (Advances in Virus Research). [DOI] [Google Scholar]
- WHO, 2020. Coronavirus disease 2019 (COVID-19) Situation Report – 81.
- Wijesinghe, P.R., Jayakody, R.L., Seneviratne, R.D.A., 2012. Prevalence and predictors of self-medication in a selected urban and rural district of Sri Lanka. J. Public Health 1 (1), 28–41. doi: https://apps.who.int/iris/handle/10665/329805. [DOI] [PubMed]
- Zu Z.Y., Jiang M.D., Xu P.P., Chen W., Ni Q.Q., Lu G.M., Zhang L.J. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;296(2) doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]