The primary challenge amid the COVID-19 crisis has been the hurdle of matching resources with demand. The predictive models for COVID-19 suggest several temporal phases to the time course of the disease. We describe them as (1) Early (initiation), (2) Surge (acceleration), (3) Peak/Plateau, and (4) Decline (deceleration). Anticipated shortfalls in personal protective equipment (PPE), mechanical ventilators, intensive care unit beds, and healthy hospital care providers have plagued the response in China, Italy, Spain, and most recently New York.
Collectively, these quantitative factors determine the health care system capacity. As COVID-19 represents a public health care crisis that taxes the capacity of geographic regions of health care delivery and therefore will require the pooling of scarce resources to meet clinical needs; system capacity should be viewed from a geographic regional health care delivery perspective not just practice group or hospital.1 The management of patients with end-stage renal disease (ESRD) presents unique challenges and opportunities given that it occurs across hospital-based, outpatient center, physician office-based, and “free standing” procedural facilities.
Herein, the Early phase is marked by the pre-pandemic period and the confirmation of the initial COVID-19 case. The Surge phase is marked by the rapid acceleration in COVID-19 cases, related hospitalizations, and intensive care unit admissions. Pandemic projection models vary depending on factors such as mitigation timing, application, and success. Therefore, Peak/Plateau refers to the cresting or sustained stabilization of pandemic metrics over 14 days. Finally, Decline refers to a consistent deceleration of pandemic metrics over 14 days.2
The 2018 United States Renal Dialysis System (USRDS) annual report, the most recently available report, documented over 725,000 prevalent and 124,000 incident patients.3 The placement and maintenance of functioning vascular access is essential for those patients receiving intermittent hemodialysis (IHD). To that end, The Centers for Medicaid/Medicare Services (CMS) released official guidance that conferred “essential surgery” status on dialysis vascular access procedures.4
Although the decision regarding “essential surgery” classification has been welcomed by all providers that render care to this vulnerable patient population, some conflict has arisen between disciplines that collaborate with regard to the interpretation and implementation of the guidance. These tensions are largely focused around the issue of the timing of permanent vascular access (VA) creation. The CMS guidance has been interpreted by many to mean “business as usual” toward the shared long-standing goal of meeting Kidney Dialysis Outcomes Quality Initiative (KDOQI) metrics, specifically, seeking appropriately timed early creation of VA in advanced chronic kidney disease (CKD) and prompt creation of VA in those patients initiated on IHD with a tunneled dialysis catheter (TDC).5
Informed members of the ESRD collaborative care team agree with the “non-crisis” approach to VA, that is, the “fistula first, catheter last” ideal. The characterization of VA as “essential surgery” is fully endorsed. The problem: a dogmatic interpretation of the guidelines without the context of the evolving COVID-19 crisis in various geographies of the United States. The reality of the crisis is that every part of the country finds itself in a different part of the pandemic curve. There is near uniform agreement that VA with prolonged bleeding, ulcerative skin lesion, or a clinically significant (preventing adequate hemodialysis) flow altering lesion associated with an autologous fistula should be addressed with haste to continue dialysis uninterrupted and to prevent an inpatient hospitalization.
However, the gray area emerges with the discussion of two groups: (1) the nondialyzed patient who is pre-ESRD and (2) the patient successfully dialyzing with a catheter who has yet to undergo permanent access. Unfortunately, USRDS data confirm that 80% of patients begin dialysis with a TDC (60%, TDC alone; 20%, TDC + fistula/bridge graft).3
The complete discussion of the decision-making process must not forget several important COVID-era considerations. First, entering a health care facility is not without hazard. Health care facilities pose relatively higher risks of COVID-19 infection (yet to be quantified) for patients with ESRD who have a disproportionately higher prevalence of comorbidities such as diabetes, cardiovascular disease, and overall immune suppression.6 Although procedures performed in a nonhospital setting such as an office-based procedural room or ambulatory surgical center might theoretically have a lower risk than a busy inpatient facility, no data exist to support this claim.
Second, for those health care facilities in the resource-conserving Surge and/or Peak phase of the COVID-19 pandemic, the operating room of a hospital or ambulatory surgical center is likely in an emergency only status. Stay-at-home orders have been issued in the form of executive orders or proclamations at the gubernatorial level. Executive orders, proclamations, and similar orders carry the same weight as legislature-passed laws, because they have been issued under the authority of existing legislature.7 , 8 In Texas, an executive order issued by Governor Abbott threatened penalties of $1000 or 180-day jail time for those providers found noncompliant by performing surgeries that are not immediately necessary.9
As proven by the New York pandemic experience, PPE conservation and maximizing availability of all mechanical ventilators is tantamount to saving the life of a patient or a provider during the Surge/Peak phase. The guiding principle is that the role of the proceduralist in what arguably is a wartime-like medical crisis is to conserve resources for the mass casualty scenario that may ensue with the Surge/Peak phase.
COVID-19 VA care model
Our practice setting is a clinically oriented academic employed physician model. Although this specific practice setting may facilitate some aspects of this model, we are confident that collaborative VA teams exist in all health care settings to varying degrees. Early engagement of this multidisciplinary team is necessary to ensure feedback from all participating parties and obtain the mutual agreement necessary to execute patient-centered and nuanced VA strategies.
Early on, we stratified vascular access “essential procedures” into those requiring immediate care, that is, within 24 to 48 hours, as Tier 1 and those deemed “important” but not requiring immediate treatment as Tier 2. Table I summarizes these two patient populations. Our primary goal was to continue delivery of these “essential procedures” by focusing on those procedures that are outpatient and thus require less collective resources including hospital bed, provider personnel, and PPE resources.
Table I.
Stratification of vascular access procedure timing
| Urgent—Tier 1: within 24 hours | Important—Tier 2: individual patient clinical circumstances dictate timing |
|---|---|
| Ulcerated overlying skin, bleeding | New access creation/functional TDC |
| Large aneurysm with skin compromise | New access creation/pre-ESRD |
| Thrombosed access | TDC removal |
| Threatened-prolonged bleeding/low flow | PD catheter placement |
ESRD, End-stage renal disease; PD, peritoneal dialysis; TDC, tunneled dialysis catheter.
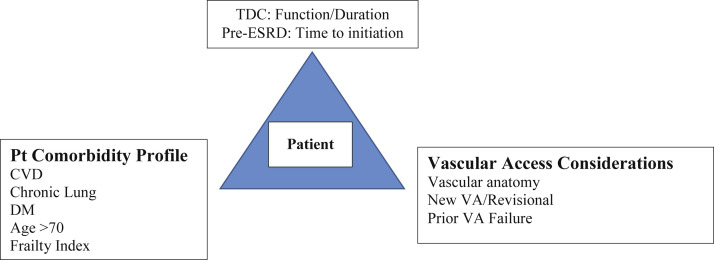
Lok et al have extensively described those patient vascular anatomic features and chronic disease comorbidities that are associated with increased rates of VA failure at early, mid-, and long-term interveals.10 The patient comorbidity profile associated with reduced life expectancy has been characterized in several published predictive models. Advanced age and the presence of chronic conditions such as diabetes mellitus, cardiovascular disease, peripheral vascular disease, and frailty impact life expectancy as well as VA durability outcomes.11, 12, 13, 14, 15 Our patient-centered vascular access risk model is depicted in the Fig .
Fig.
Patient-centered vascular access (VA) risk model. CVD, Cardiovascular disease; DM, diabetes mellitus; ESRD, end-stage renal disease; TDC, tunneled dialysis catheter.
We used this evidence-based rubric to identify those Tier 2 selective patients at higher risk for VA failure and those with high comorbidity profiles or reduced life expectancy profiles. Those “high risk” prevalent patients in whom a TDC has functioned well are considered for deferred VA creation following the Peak/Plateau phase. We use a triage team composed of a nephrologist or advanced practice nurse familiar with the patient, vascular surgeon, and interventional radiologist to stratify the patient as Tier 2 selective (Table II ).
Table II.
COVID-19 pandemic vascular access prioritization model
| Temporal phase of COVID era | Procedure Tier to be performed |
|---|---|
| Initiation | Tier 1, Tier 2 |
| Acceleration | Tier 1, Selective Tier 2 (low risk)a |
| Plateau | Tier 1, Selective Tier 2 (low risk)a |
| Deceleration | Tier 1, All Tier 2 |
Less than 90-120 minutes of surgical time, outpatient.
Early phase
In our northeastern Ohio footprint, we continued to perform Tier 1 and 2 procedures in the Early COVID-19 period. We have used virtual teleconferencing platforms to reduce the need to bring patients into the health care facility before the time of surgery. Telehealth is used in three distinct circumstances: (1) initial patient assessment to discuss VA options and immediacy of need in the pre-ESRD patient; (2) from the dialysis facility with the patient and the assistance of staff (nephrology advanced practice provider [APP], dialysis center nurse) to discuss and assess dysfunction; and (3) to assess and discuss new access creation and the risks and benefits in the patient currently on IHD with a TDC. Telehealth does not supplant the need to perform a careful physical examination to determine VA siting, but it initiates the process, sets patient and provider expectations, and allows one to set forth a pathway to establish a tailored VA creation strategy and timing.
We have engaged our multidisciplinary VA team of nephrology providers including physicians and APPs, interventional radiologists, and vascular surgeons to discuss the specific clinical circumstances of the patient that may influence timing of permanent access creation in two specific patient groups: (1) ESRD currently dialyzing with a TDC; (2) pre-ESRD patients with CKD. This patient-centric approach means that, now more than ever, our CKD outpatient clinic APPs must give careful consideration to the timing of consultation for creation of permanent VA.
For those patients dialyzing via a TDC, using the aforementioned rubric, we look to evaluate and to schedule surgery with a careful eye on our health care system resource capacity/demand status. We also recognize that some patients are unwilling to come to the hospital for care given what they have seen in the media surrounding COVID-19. To align our resource utilization with hospital capacity, our VA team participates in daily enterprise-wide A.M. and afternoon COVID-19 briefings that provide critical insight into the capacity of health providers, PPE, beds, and new COVID-19 patient surges or geographic outbreaks. Regionally within our geographic footprint, we have created a multidisciplinary cross health care system council to discuss institutional and regional capacity as well as regional best practice approaches to our shared COVID-19 management strategies for VA patients.
Peak/Plateau phase
Now, in what we find to be a “flattened” plateau phase of the pandemic due to effectively applied mitigation strategies in Ohio, we continue to function with this same model of strategic urgency for VA as an essential lifesaving therapy. Tier 1 and Selective Tier 2 patient surgery is performed after consideration of TDC-, patient-, and VA-associated features. We maintain our fistula first but “functioning access and catheter last” practice approach, which may be arguably more important in the pandemic era when we seek to avoid the need for revisional procedures that sometimes result from poor initial VA site selection. At the time of our institutionally required preoperative visit with anesthesia and the surgeon within 3 days of surgery, COVID-19 testing is performed. We maintain an “awaiting VA creation” queue within our VA program in coordination with our associated dialysis centers. This registry facilitates identifying if our health care facility side capacity limitations are “creating” a backlog secondary to VA procedure access. Concomitantly, our health care system is following CMS guidance for entering phase 1 of the “Restarting America” program, which will involve a strategic focus on broad COVID testing, contact tracing, and selective quarantine.16
Decline phase
Tier 1 and all Tier 2 procedures will be performed. Our goals will be severalfold. The first goal will be to identify and prioritize VA queue patients based on clinical needs. This will require our multidisciplinary team to have continuous dialogue to reduce TDC exposure. Health care facilities in our region may have a backlog of patients requiring VA. Collaboration in the offloading of patients may be necessary to meet patient demand and resource availability. Our regional cross health care system council will facilitate appraisal of this need. Next, we will need to identify the need and engage in an educational and information-providing effort within dialysis centers to allay patient and staff concerns regarding “re-entering” the physical health care setting.17 Last, health care systems and group practices performing VA procedures within nonhospital-associated settings may be able to leverage their capacity as dedicated VA creation facilities and compensate for increased service demand. For nonhospital-associated groups, constant dialogue with regional health care systems and public health authorities will be essential to understand health care system capacity and identify emerging COVID-19 threats to capacity.
The deceleration phase will be followed by a prolonged COVID-19 recovery that the Centers for Disease Control and Prevention (CDC) expects will be a long tail.18 A second and potentially third wave of the COVID-19 pandemic are also predicted in the fall and winter of 2020. Our COVID-19 VA model will remain active amid ebbs and flows of the pandemic may be applied as the local/regional health care VA population capacity/demand match dictates.
Discussion
Of course, nuanced scenarios will occur. A 25-year-old patient who presents with a second episode of TDC-associated blood stream infection and requires near term VA planning and creation. The risk of recurrent infection to life warrants the use of resources to create a permanent VA. An autologous fistula when anatomy is suitable vs an immediate use graft might be considered based on the interventionalist/surgeon's discretion. For those patients with suitable anatomy, percutaneous fistula may also be considered and may ultimately prove to mitigate risk and resources associated with surgical VA creation. Long-term procedural outcomes data and economic analysis are not yet available to verify this claim.19 , 20
By the same token, as we emerge from the pandemic and begin to enter the Decline phase, the risk to both patient and provider will begin to diminish. This will happen gradually and variably throughout the United States, and each region will need to grapple with similar discussions of appropriate care. There will be no single appropriate approach that fits all, and we will still need to design a VA strategy tailored to the specific patient circumstances—one that most importantly includes patient input.10
Socially disadvantage persons, low-income individuals, and racial and ethnic minorities are disproportionately affected by ESRD. In the best of times, the ESRD cohort represents a group at risk for poor outcomes due to health care system factors as well as social determinants.21 Now, in the COVID-19 pandemic, thoughtful strategies and a collective effort are necessary to optimize patient care, minimize morbidity, and control health care expenditure for this vulnerable patient group.
Conclusions
The need for shared responsibility, dialogue, and collaboration is essential between the care providers for this challenging patient population. We must continue to find a way to provide the highest level of care to this vulnerable patient population during this trying time. Open communication is even more important in the COVID pandemic as the availability of resources waxes and wanes and appropriate resource allocation remains critical. Care teams composed of nephrology, a vascular interventionalist/surgeon, and, in the case of COVID end-of-life decisions, a bioethicist may facilitate this goal.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Amid Ongoing COVID-19 Pandemic Governor Cuomo Announces Statewide Public-private Hospital Plan to Fight COVID-19. Governor Andrew M. Cuomo. https://www.governor.ny.gov/news/amid-ongoing-covid-19-pandemic-governor-cuomo-announces-statewide-public-private-hospital-plan Available at:
- 2.Qualls N., Levitt A., Kanade N., Wright-Jegede N., Dopson S., Biggerstaff M., et al. Community mitigation guidelines to prevent pandemic influenza—United States, 2017. MMWR Recomm Rep. 2017;66:1–34. doi: 10.15585/mmwr.rr6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United States Renal Dialysis Data System (USRDS) 2018 annual data report https://www.usrds.org/2018/view/Default.aspx Available at:
- 4.Centers for Disease Control and Prevention (CDC) 2020. Coronavirus Disease 2019 (COVID-19)https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html Available at: [Google Scholar]
- 5.Lok C.E., Huber T.S., Lee T., Shenoy S., Yevzlin A.S., Abreo K., et al. KDOQI clinical practice guideline for vascular access: 2019 update. Am J Kidney Dis. 2020;75(Suppl 2):S1–S164. doi: 10.1053/j.ajkd.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Basile C., Combe C., Pizzarelli F., Covic A., Davenport A., Kanbay M., et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol Dial Transplant. 2020;35:737–741. doi: 10.1093/ndt/gfaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Constitution Center Constitutional powers and issues during a quarantine situation. https://constitutioncenter.org/blog/constitutional-powers-and-issues-during-a-quarantine-situation Available at:
- 8.Justia Law Jacobson v. Massachusetts, 197 U.S. 11 (1905) https://supreme.justia.com/cases/federal/us/197/11/ Available at:
- 9.Texas Attorney General Health Care Professionals and Facilities, Including Abortion Providers, Must Immediately Stop All Medically Unnecessary Surgeries and Procedures to Preserve Resources to Fight COVID-19 Pandemic. https://www.texasattorneygeneral.gov/news/releases/health-care-professionals-and-facilities-including-abortion-providers-must-immediately-stop-all Available at:
- 10.Woo K., Lok C.E. New insights into dialysis vascular access: what is the optimal vascular access type and timing of access creation in CKD and dialysis patients? Clin J Am Soc Nephrol. 2016;11:1487–1494. doi: 10.2215/CJN.02190216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen L.M., Ruthazer R., Moss A.H., Germain M.J. Predicting six-month mortality for patients who are on maintenance hemodialysis. Clin J Am Soc Nephrol. 2010;5:72–79. doi: 10.2215/CJN.03860609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sy J., Johansen K.L. The impact of frailty on outcomes in dialysis. Curr Opin Nephrol Hypertens. 2017;26:537–542. doi: 10.1097/MNH.0000000000000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johansen K.L., Delgado C., Bao Y., Kurella Tamura M. Frailty and dialysis initiation. Semin Dial. 2013;26:690–696. doi: 10.1111/sdi.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Viecelli A.K., Lok C.E. Hemodialysis vascular access in the elderly-getting it right. Kidney Int. 2019;95:38–49. doi: 10.1016/j.kint.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Couchoud C., Labeeuw M., Moranne O., Allot V., Esnault V., Frimat L., et al. A clinical score to predict 6-month prognosis in elderly patients starting dialysis for end-stage renal disease. Nephrol Dial Transplant. 2009;24:1553–1561. doi: 10.1093/ndt/gfn698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CMS CMS Issues Recommendations to Re-Open Health Care Systems in Areas with Low Incidence of COVID-19. https://www.cms.gov/newsroom/press-releases/cms-issues-recommendations-re-open-health-care-systems-areas-low-incidence-covid-19 Available at:
- 17.The White House Opening Up America Again. https://www.whitehouse.gov/openingamerica/ Available at:
- 18.Institute for Health Metrics and Evaluation COVID-19 Projections. https://covid19.healthdata.org/ Available at:
- 19.Lok C.E., Rajan D.K., Clement J., Kiaii M., Sidhu R., Thomson K., et al. Endovascular proximal forearm arteriovenous fistula for hemodialysis access: results of the prospective, multicenter Novel Endovascular Access Trial (NEAT) Am J Kidney Dis. 2017;70:486–497. doi: 10.1053/j.ajkd.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 20.Yang S., Lok C., Arnold R., Rajan D., Glickman M. Comparison of post-creation procedures and costs between surgical and an endovascular approach to arteriovenous fistula creation. J Vasc Access. 2017;18(Suppl 2):8–14. doi: 10.5301/jva.5000723. [DOI] [PubMed] [Google Scholar]
- 21.Crews D.C., Novick T.K. Achieving equity in dialysis care and outcomes: the role of policies. Semin Dial. 2020;33:43–51. doi: 10.1111/sdi.12847. [DOI] [PubMed] [Google Scholar]