Abstract
This study analyzed the epidemiological and clinical features of dengue fever in Zhangshu, Jiangxi Province, in 2019 and provided evidence for the diagnosis, treatment, prevention, and control of dengue fever. A total of 718 dengue fever patients in Zhangshu in 2019 were involved. ELISA and qRT-PCR were used for pathogenic detection of dengue virus. Multiple adjuvant therapies were applied, and the condition of patients after treatment was examined. Patients were between the ages of 0.75 and 92 years old, and all of them had a fever. A total of 519 cases had fatigue, and 413 cases had generalized myalgia and bone ache; 356 cases had dry mouth, 289 cases had bitter taste, and 167 cases felt dry and bitter taste; 279 cases had rash, and 93 cases had pruritus; 587 cases had decreased leukocyte, among which, 7 cases had leukocyte lower than 1 × 10 [9]/L; 380 cases had a low platelet count, and the platelet count of 29 cases was lower than 50 × 10 [9]/L; 488 cases had increased aspartic transaminase, and 460 cases had increased alanine aminotransferase; 5 cases had a severe disease. It proved that the majority of dengue fever sufferers were adults, with the main clinical features being fever and rash and the chief injured organs being the blood system, liver, heart, and gastrointestinal tract. Besides, over 40% of patients had dry and bitter taste, and 12 cases had alopecia after discharge. It indicates that the incidence of dengue fever in Zhangshu is closely related to the sudden population flow and imported cases.
Keywords: Dengue fever, Clinical features, Epidemiology, Dry mouth and bitter taste
Introduction
Dengue fever (DF) is a kind of acute mosquito-borne infectious disease caused by dengue virus (DENV) through Aedes. With the development of tourism and more frequent international communications, dengue fever has become a global disease. In recent decades, the disease is prevalent in 128 countries and regions in tropical and sub-tropical regions of the world. Approximately, 0.39 billion people get infected with DENV every year globally, and about 25 thousand people died from dengue hemorrhagic fever, with the Southeast Asia and the Caribbean region in South America suffered most [1–4]. DENV, belonging to the genus Flavivirus of the family Flaviviridae, is a single-stranded positive-sense RNA virus and encodes 10 proteins, among which non-structural proteins are involved in RNA virus replication and the regulation of immune system function. Typical DF patients manifest sudden fever, frontal headache, orbital pain, back pain, and severe myalgia, while some patients have bleeding tendency, lymphadenopathy, thrombocytopenia, and so on [1, 5]. In DF endemic areas, people are generally susceptible to the disease, but the majority of the cases are adults, while in local endemic area, the majority of the cases are children. The prevention and control of DF is hard to be managed as it is highly different in the source of infection, transmission route, and susceptible population in different regions [6, 7]. Therefore, it is of utmost importance to see the incidence of DF in different regions.
As for the reason leading to the outbreak of DF, it is quite different in different regions. It is established that the main factors accounting for the rapid increase in DF incidence are climate change, virus evolution, and some social factors like rapid urbanization, population growth, the globalization of tourism, and trade [8]. As believed by many scientists, the global or local climate variables are the decisive factors contributing to the DF distribution in space and time [9]. Due to the fact that the variation of climate will significantly affect the prevalence of virus vectors to increase the transmission of DENV [10], greenhouse effect has been regarded as one of the main factors resulting in the outbreak of DF. For local areas, some region-specific factors are being focused. Struchiner et al. [8] found that in the past four decades in Singapore, the rapid urbanization and increased human waste might be the two major causes for intensified DF condition, while the two factors have been noted to be probably associated with the high prevalence of DF in China in recent years [9]. Therefore, understanding the onset of DF not only requires a comprehensive analysis for globalization consideration, but also allows for the investigation of region-specific etiology and relevant epidemiological statistical analysis.
With regard to the epidemiological features of DF, relevant statistical research has been done in many regions every year worldwide. From 1949 to 1977, there were no reported DF cases in China. In 1978, the fever broke out and was prevalent in Foshan, Guangdong Province; after which, the disease spreads every year in different degree mainly in coastal areas like Guangdong, Guangxi, Fujian, Hainan, and Taiwan [11, 12]. In mainland provinces and cities like Wuhan and Henan, the outbreak of DF is mainly driven by the arrival of travelers from the infected areas [13–15]. In 2018, the DF outbreaks in Southeast Asia were increased compared with previous years, and severely attacked the Philippines, Cambodia, Malaysia, Thailand, Vietnam, and so on. In Jiangxi Province of China, as the flight opened up between Nanchang and Cambodia in June 2019, population movements between the two regions remarkably increased, which contributed to the imported cases of DF in 10 districts and cities in Jiangxi in 2019 and local DF outbreaks in multiple county-level cities, with totally 1235 cases of DF reported throughout the year. Therefore, it is highly necessary to study the epidemiological features of DF in Jiangxi Province.
In this study, 718 DF cases were collected from Zhangshu People’s Hospital, Zhangshu Qingjiang Hospital, and The Ninth Hospital of Nanchang in Zhangshu City, Jiangxi Province. With the epidemiological data, clinical features, and laboratory examination results being retrospectively analyzed, this study aimed to explore the source and the possible drivers for DF in Zhangshu City in 2019, so as to provide evidence for further specification of DF diagnosis and treatment and strengthen of prevention and control.
Materials and methods
Research object
This study chose 718 confirmed cases of DF and clinically diagnosed cases from Zhangshu People’s Hospital, Zhangshu Qingjiang Hospital, and The Ninth Hospital of Nanchang in Zhangshu City, Jiangxi Province, from August to October 2019. The inclusion criteria for confirmed cases were in line with the Guidelines for Diagnosis and Treatment of Dengue in China: having a historical epidemiology of DF; presence of clinical manifestations like fever, rash, decreased counts of white blood cell (WBC), and platelet; positive for DENV-specific IgM antibody, NS1 antigen, or DENV nucleic acid. Diagnostic criteria for severe DF are as follows: accompanied with severe bleeding (including but not limited to subcutaneous hematoma, gross hematuria, hemoptysis, gastrointestinal hemorrhage, vaginal bleeding, intracranial hemorrhage and so on); shock; severe organ damage, including acute aspiratory distress syndrome (ARDS) or respiratory failure, acute myocarditis or acute heart failure, acute liver injury (alanine aminotransferase, ALT, and/or aspartic transaminase, AST > 1000 U/L), acute renal failure, encephalopathy, or encephalitis [16]. Clinically diagnosed cases recruited in this study met the health industry standard of the People’s Republic of China “Diagnosis for Dengue Fever” (WS216—2018) [17].
Epidemiological statistics and collection of patient’s clinical features
The epidemiological data in this study included patient’s age, gender, occupation, place of residence, travel history, contact history, mosquito bite history, and whether or not living in epidemic area. The clinical symptoms and signs of the patients contained fever, fatigue, chills, rash, dry mouth, bitter taste, headache, myalgia, and bone and joint pain.
DENV NS1 antigen detection
In this study, the serum of 15 DF patients from The Ninth Hospital of Nanchang was sent to Jiangxi Provincial Center for Disease Control and Prevention to detect dengue NS1 antigen by using colloidal gold immunochromatography assay (GICA) (01PF20, PANBIO, Australia). The serum of 245 patients were detected in Zhangshu People’s Hospital by using enzyme linked immunosorbent assay (ELISA) (48T/96T, WanDai, Beijing, China).
DENV typing by qRT-PCR
Twenty-one serum samples out of 718 patients (15 samples from The Ninth Hospital of Nanchang, 6 samples from Zhangshu People’s Hospital) were sent to Jiangxi Provincial Center for Disease Control and Prevention to identify DENV type by means of real-time fluorescence quantitative (qRT)-PCR assay. The detection reagent was purchased from Jiangsu Bioperfectus Technologies Company, Ltd.
Forty-six serum samples out of 718 patients (from Zhangshu People’s Hospital) were sent to Shanghai Huashan Hospital to identify DENV type. Serum virus RNA was extracted with MiniBEST virus abstraction kit (9767, Takara, Japan), and extracted RNA was reversely transcribed into cDNA by TaKaRa PrimeScript reverse transcription kit (RR055A, Takara, Japan). The detection reagent for DENV typing was purchased from Shanghai BioGerm Medical Biotechnology Co., Ltd. DENV1/2 and DENV3/4 qRT-PCR probes were used.
Patient’s physiological function detection
A series of physiological function tests were carried out on the patients, mainly including blood routine, hepatic and renal function, electrolyte, coagulation function, electrocardiogram, and abdominal Doppler ultrasound.
Statistical analysis
Data were input into the Microsoft Excel 2019 work sheets. All data of confirmed cases were statistically analyzed by the method of descriptive epidemiology. Part of data were processed using the SPSS 22.0.
Results
Epidemiological features of patients
First of all, the epidemiological features of patients were recorded and statistically analyzed (Fig. 1). The male to female ratio of DF cases was 0.82:1. In terms of age, the majority of patients were above 19 years old, and the number of female patients of all ages was more than that of male patients. Besides, most of the patients were farmers or the unemployed. Apart from the age and occupation, it was also found that 91% of the patients had a mosquito bite history prior to the onset of illness.
Fig. 1.
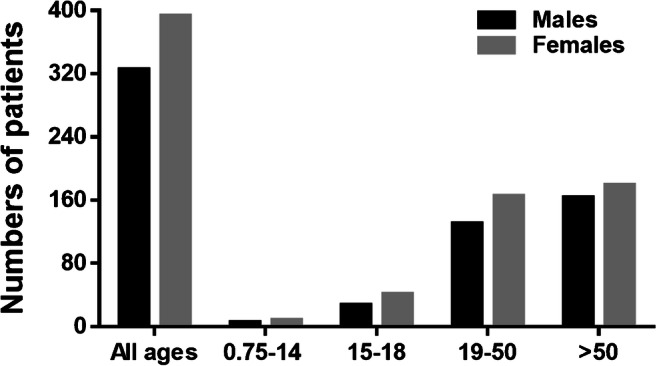
Ages and gender features of patients
Clinical features of patients
The clinical features of the 718 patients were sequentially statistically analyzed. As revealed in Table 1, the majority of the patients had common DF symptoms like fever, fatigue, headache, and arthralgia. Apart from that, we also found that over 40% of the local patients had dry mouth or bitter taste, which was not commonly seen in other reported features of DF. Therefore, the prevention and treatment for local DF are of great significance, and our finding has a certain reference value for the future judgment of the clinical features of DF.
Table 1.
Clinical features of 718 cases’ dengue fever
| Symptoms and signs | Number of cases | Incidence rate (%) |
|---|---|---|
| Fever | 718 | 100 |
| Double-phase fever | 57 | 7.93 |
| Hypodynamia | 519 | 72.28 |
| Headache | 492 | 68.52 |
| Muscle and bone joint pain | 431 | 60.03 |
| Poor appetite | 392 | 54.59 |
| Poor appetite and nausea | 287 | 39.97 |
| Poor appetite, nausea, and vomiting | 62 | 8.64 |
| Dry mouth | 356 | 49.58 |
| Bitter taste in the mouth | 289 | 40.25 |
| Dry mouth and bitter taste in the mouth | 167 | 26.26 |
| Rash | 279 | 38.86 |
| Pruritus | 93 | 12.95 |
| Abdominal pain | 126 | 17.55 |
| Diarrhea | 97 | 13.51 |
| Hemorrhage | 169 | 23.54 |
| Neurological symptoms | 8 | 1.11 |
| Superficial lymphadenopathy | 16 | 2.23 |
Physiological and biochemical characteristics of patients
After analyzing patient’s apparent characteristics, we also detected and analyzed their physiological and biochemical characteristics. The results indicated that decreased WBC and platelet were present in patients, while AST and ALT were increased compared with the reference value. Besides, there was a noticeable rise in lactate dehydrogenase (LDH) which is a myocardial enzyme index (Table 2). These results suggested that physiological and biochemical characteristics may be affected in part of the local patients after suffering from DF.
Table 2.
Physiological and biochemical characteristics of patients
| Biochemical index | Number of cases | Incidence rate (%) | Highest (lowest) value | |
|---|---|---|---|---|
| Leukocyte count | < 1.0*10^9/L | 7 | 0.97 | 0.8*10^9/L |
| 1.0–2.0*10^9/L | 87 | 12.12 | ||
| 2.0–3.0*10^9/L | 139 | 19.36 | ||
| 3.0–4.0*10^9/L | 350 | 48.75 | ||
| Platelet count | < 20*10^9/L | 29 | 4.04 | 1.0*10^9/L |
| 20–100*10^9/L | 351 | 48.89 | ||
| ALT | 40–80 U/L | 257 | 35.78 | 616 U/L |
| 80–200 U/L | 168 | 23.40 | ||
| 200–400 U/L | 26 | 3.62 | ||
| > 400 U/L | 9 | 1.25 | 616 U/L | |
| AST | 40–80 U/L | 261 | 36.35 | |
| 80–200 U/L | 179 | 24.93 | ||
| 200–400 U/L | 35 | 4.87 | ||
| > 400 U/L | 13 | 1.81 | 687 U/L | |
| Creatine kinase (CK) | 395 | 55.01 | 4327 U/L | |
| Creatine kinase isoenzyme CK-MB) | 230 | 32.03 | 776 U/L | |
| Lactate dehydrogenase (LDH) | 407 | 56.69 | 791 U/L | |
| Hematocrit (HCT) | 169 | 22.54 | 76% | |
| Hemodiastase | 38 | 5.29 | 470 U/L | |
| Total bilirubin | 17.10–34.2Umol/L | 32 | 4.46 | |
| > 34.2Umol/L | 11 | 1.53 | 56.3 Umol/L | |
| Blood urea nitrogen (BUN) | 17 | 2.37 | 22.93 umol/L | |
| Creatinine (Cr) | 26 | 3.62 | 583 mmol/L | |
Pathogenic detection
In regard to pathogenic detection, serum samples from 260 cases were subjected to NS1 antigen examination, with 256 positive cases, and the positive rate was 98.46%. Sixty-seven serum samples were used for nucleic acid testing with 62 positive cases, and the positive rate was 92.54%. The residual 5 negative cases underwent sampling inspection on and after the 6th day after the onset of the illness. The nucleic acid type of the 62 cases were all DENV1.
Features of patients with severe DF
Some patients in this study were noted to have a severe DF. In view of this, we paid close attention to the features of these cases and made an analysis. Overall, 5 cases (0.7%) in our study met the criteria of severe DF. Digestive tract bleeding is one of the severe complications of DF. Of the 5 cases, 2 cases suffered from digestive tract bleeding: one being male aged 62 years old and complicated with upper gastrointestinal bleeding; another being female aged 26 years old and complicated with non-menstrual vaginal bleeding. Moreover, it has been proven that DF could attack the central nervous system and cause severe complications such as encephalitis, meningitis, cerebral hemorrhage, and metabolic encephalopathy [18]. The other 3 cases developed neurological symptoms in the group: one was a 78-year-old female patient who suffered from unconsciousness, aphasia, and neck rigidity on the 8th day of the course of disease, and was transferred to The Ninth Hospital of Nanchang and confirmed to have viral encephalitis by lumbar puncture; one was a 35-year-old male patient with high fever, coma, unconsciousness, and neck rigidity on the 3rd day of the course of disease and was suspected for dengue encephalitis; one was a 17-year-old male patient accompanied by a fever for 9 days with the highest temperature reaching 40 °C, developed abnormal behavior and delusion of persecution on the 3rd day of the course of disease, and was considered as DF-induced schizophrenia.
Treatment and recovery of patients
After the patients were confirmed with DF, anti-mosquito precautions were done for all hospitalized patients. For patients with an acute DF, especially those with increased myocardial enzyme indexes, they were told to stay in bed, with their vital signs, spirit, gastrointestinal symptoms, urine volume, and hemorrhagic manifestations being closely observed. Symptomatic supportive treatment was the chief treatment method with fluid infusion appropriately applied. Patients who had underlying diseases were actively treated. Patients with elevated hematocrit (HCT) were treated with blood volume expansion and fluid infusion in time, and no shock cases were observed. Patients whose transaminase elevated by 2 times normal value and more were given glycyrrhizic acid preparations for the decrease in transaminase and hepatoprotection, and the level of liver enzymes in most of patients returned to normal before discharge. One DF patient complicated with digestive tract bleeding was told to fast, and treated with omeprazole, octreotide, hemostatic enzyme, and in time fluid infusion for 11 days; after which, he/she recovered and was discharged. One DF patient complicated with non-menstrual virginal bleeding recovered and was discharged after 1 week of treatment with hemostasis and fluid infusion. Two DF patients with viral encephalitis were treated with mannitol to reduce their intracranial pressure supplemented with albumin and other symptomatic supportive treatments. Their symptoms were relieved and they were discharged from the hospital on the 8th day and the 12th day of the course of disease, respectively. One DF patient who developed schizophrenia was transferred to the Zhangshu Mental Hospital after the fever disappeared, and had been discharged from hospital when follow up 2 months later. Among the patients whose blood amylase increased, 2 patients had nausea, vomiting, and abdominal pain. Pancreatitis was considered, and they were asked to fast and fluid infusion and octreotide were given for 7–10 days of treatment. Both of them recovered and were discharged from hospital. Overall, all the 718 patients recovered and were discharged from hospital with no death. A follow-up visit was scheduled 2 months after discharge and it was found that 12 patients had alopecia. These treatments and the post-treatment features are of certain value for the prevention and treatment of local DF in the future.
Discussion
DF is a seasonal and region-specific disease generally prevalent from May to November every year. At present, DF remains one of the tropical diseases that are most easily ignored. With the geographical expansion of DENV and the virus vectors Aedes over the recent decades, the incidence of DF has increased 30 times [5]. In Asia, monsoon is the major decisive factor leading to the variation of local climate, and the East Asian Summer Monsoon (EASN) is the main driver for climate change in East China, Korea, Japan, and other countries [19]. Jiangxi Province in the southeast of China is a typical sub-tropical zone with plentiful rainfall throughout the year. Zhangshu City locates in the center of Jiangxi with the Ganjiang River running through the city. With global warming intensifies, green plants are increased in the city, which creates conditions for the breeding of mosquitoes. As a consequence, it is easy to cause DF outbreak and prevalence once the DENV is imported. In the present study, our findings suggested that the age of the DF patients ranged from 0.75 to 92 years old, indicating that people of all age groups are susceptible to DENV. Of the 718 cases, 41% of patients were between the ages of 19 and 50 years old, 47.6% were over 50, and 14 cases were in the children. These results reveal that adults are the main sufferers in new endemic areas, which is different from the local endemic areas in Southeast Asia where children suffer the most.
Transmission by imported travelers with DF is one of the common ways contributing to the outbreak of DF in local areas. According to the epidemiological survey, the patients we enrolled earlier (in early August) were all the residents from Jingjiu Trade City in Zhangshu. The patients enrolled in late August were from the periphery areas of the trade city and the patients admitted in early September spread throughout the city. Further investigation found that there is a council house in Jingjiu Trade City where the same people live and they still get used to getting together to enjoy the cool air at night. In early July, some persons returned here from their tour in Southeast Asia. Some of them had a fever but only went to the community clinic, instead of going to the hospital, for infusion treatment and got well. During the treatment, they still got together to enjoy the cool air. Since then, some of them caught a fever and developed rash, and they still went to the community clinic. Until more and more people were infected, patients in the community began to go to the Zhangshu People’s Hospital, and the disease had been taken seriously. As epidemiological investigation suggested, the outbreak of DF in Zhangshu City was caused by the people with fever who returned from a tour in Southeast Asia. Furthermore, many investigations noted that the outbreak of DF in local areas is attributed to the local people who return from their tour in Africa or Latin America [20, 21]. Therefore, to manage the outbreak of DF in local areas, whether there are imported cases should be given priority so that specific quarantine measures and precautions can be effectively carried out.
DF is usually a self-limited disease with a generally good prognosis. The treatment for DF mainly focuses on symptomatic supportive treatment and clinical monitoring. Among the DF patients in Zhangshu City enrolled in this study, no death was found, and fever and rash were the typical manifestations. All patients had a fever in the course of disease with the highest temperature reaching 40.5 °C. Irregular fever was predominant and 57 cases (7.93%) had a double quotidian fever. A total of 279 cases (38.86%) had rash commonly seen in limbs and trunk, and congestive rash, erythematous rash, or local scarlatiniform rash was the majority. Approximately, half of the patients had dry mouth or bitter taste in the course of disease, which was rarely reported in previous research. Among the 718 cases, 167 (26.26%) cases had both dry mouth and bitter taste, 289 (40.25%) cases had dry mouth, and 356 (45.98%) cases had bitter taste. Dry mouth was considered to be related to the plasma leakage caused by the increased capillary permeability in DF patients, but only 169 (22.94%) cases had elevated HCT, which cannot fully explain this phenomenon. Bitter taste in the mouth belongs to the damp-heat category in Traditional Chinese medicine (TCM). Some patients who had bitter taste in the mouth were given aromatic damp-resolving drugs as suggested by TCM doctors, and their symptoms could be quickly relieved. Patients suffering from dry mouth were treated with hypotonic oral rehydration salts with water. Some patients who had dry mouth with elevated HCT were given blood volume expansion, fluid infusion, and correction of acid-base imbalance; after which, HCT soon returned to normal and no shock occurred.
As for the complications, leukopenia was the complication with the highest incidence rate in the patients in this study and occurred in 504 cases (70.19%). Thrombocytopenia happened in 380 cases (52.92%), elevated AST in 488 cases (67.97%) with the highest reaching 637 U/L and elevated ALT in 460 cases (64.07%) with the highest reaching 616 U/L, and the rise of AST was generally bigger than that of ALT. All above laboratory findings are similar to those reported by Cavailler [22]. The reason for the bigger rise in AST is that other than the AST in liver, more AST comes from the isoenzymes produced by myocardial cell injury. In DF patients, myocardial damage is easy to occur in early stage. In our study, the rise in myocardial enzyme indexes mainly seen in LDH in 407 cases (56.69%), followed by creatine kinase (CK) in 359 cases (55.01%) and creatine kinase-MB (CK-MB) in 230 cases (32.03%). These patients were told to stay in bed and given oxygen therapy and symptomatic treatments with favorable prognosis. In the meantime, there were 126 cases (17.55%) with abdominal pain, 97 cases (13.51%) with diarrhea, and 38 cases (5.29%) with increased blood amylase; among which, 2 patients had nausea, vomiting, and abdominal pain, and pancreatitis was suspected. The two patients both recovered and were discharged after 7–10 days of treatment with fasting, fluid infusion, and octreotide. Besides, 43 cases (5.98%) had raised total bilirubin with the highest reaching 56.3 Umol/L. In this group, there were 17 cases (2.37%) with elevated urea nitrogen (BUN) and 26 cases (3.62%) with increased creatinine (Cr), and most of them were elderly patients with underlying chronic kidney disease, which suggested that DF had a limited effect on renal functions. In this study, only 16 out of 718 (2.23%) cases had superficial lymph node enlargement, which is similar to the results studied by Daumas RP and other researchers in Brazil [23].
Conclusion
The outbreak of DF in 718 cases in this study was probably caused by the patients with a fever who returned from a travel in Southeast Asia. The disease had a high incidence from July to September, and the patients were mainly adults, most of whom were farmers and the unemployed. Typical clinical features were fever and rash, and the injured organs chiefly were the blood system, liver, heart, and gastrointestinal system. The incidence of severe type was low and there was no death. Over 40% of the patients had dry mouth and bitter taste in the mouth, and the follow-up visit found that 1.67% of the discharged patients had alopecia. With the increasing globalization and frequent international communications, the number of imported cases will rise. Clinicians at all levels (including community doctors) are supposed to identify early cases of mosquito-borne diseases, such as DF, malaria, Zika, yellow fever, and Chikungvnya fever, and report the cases in time. In the meantime, they should be skilled in the diagnosis of the common insect-borne infectious diseases and the identification and treatment of severe cases. The departments concerned should take comprehensive measures. For the people who go to the epidemic area for travel or work, it is important to strengthen propagation and education to raise their awareness of mosquito-borne diseases and take anti-mosquito precautions. By improving the screening of the people with a fever returning from a tour, the transmission route can be controlled in time and the spread of the pathogens of mosquito-borne infectious diseases like DENV in the local Aedes can be effectively prevented, and sequentially, the outbreak and prevalence of local infectious cases can be better prevented.
Availability of data and materials
The data used to support the findings of this study are included within the article. The data and materials in the current study are available from the corresponding author on reasonable request.
Authors’ contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Compliance with ethical standards
Ethics approval and consent to participate
This study was conducted in accordance with the Helsinki Declaration II and was approved by the Institutional Review Boards of The Ninth Hospital of Nanchang.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jingen Wang, Email: wangjinenen23@163.com.
Qiubo Chen, Email: chen892312567@163.com.
Zhongbao Jiang, Email: jzbpressure@163.com.
Xiaoju Li, Email: li_12347890@126.com.
Huiping Kuang, Email: kuangzonghp@163.com.
Ting Chen, Email: chenting9216@163.com.
Feng Liu, Email: liuwindyly@163.comm.
Wujuan Zhou, Email: zwjuan65238@126.com.
Yanxia Huang, Email: huangyellow9821@163.com.
Yong Luo, Email: luoyong65901@163.com.
Jianfeng Rao, Email: rao_1234342189@163.com.
Weihua Ju, Email: juweihua1976@163.com.
Li Wang, Email: li237619803@126.com.
Xuping Peng, Email: pengpeng_2_2@163.com.
Zhicheng Zhang, Email: zhang56762389@163.com.
Hongyi Chen, Email: chenhongredyi@163.com.
References
- 1.Bhatt S, et al. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brady OJ, et al. Refining the global spatial limits of dengue virus transmission by evidence-based consensus. PLoS Negl Trop Dis. 2012;6:e1760. doi: 10.1371/journal.pntd.0001760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duong V, et al. Asymptomatic humans transmit dengue virus to mosquitoes. Proc Natl Acad Sci U S A. 2015;112:14688–14693. doi: 10.1073/pnas.1508114112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khetarpal N, Khanna I. Dengue fever: causes, complications, and vaccine strategies. J Immunol Res. 2016;2016:6803098. doi: 10.1155/2016/6803098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guzman MG, Gubler DJ, Izquierdo A, Martinez E, Halstead SB. Dengue infection. Nat Rev Dis Primers. 2016;2:16055. doi: 10.1038/nrdp.2016.55. [DOI] [PubMed] [Google Scholar]
- 6.Racloz V, Ramsey R, Tong S, Hu W. Surveillance of dengue fever virus: a review of epidemiological models and early warning systems. PLoS Negl Trop Dis. 2012;6:e1648. doi: 10.1371/journal.pntd.0001648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lana-Peixoto MA, et al. Myelitis and cauda equina involvement following dengue fever. A case report and review of the literature. Mult Scler Relat Disord. 2018;20:48–50. doi: 10.1016/j.msard.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Struchiner CJ, Rocklov J, Wilder-Smith A, Massad E. Increasing dengue incidence in Singapore over the past 40 years: population growth, Climate and Mobility. PLoS One. 2015;10:e0136286. doi: 10.1371/journal.pone.0136286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu K, et al. Climate factors and the East Asian summer monsoon may drive large outbreaks of dengue in China. Environ Res. 2020;183:109190. doi: 10.1016/j.envres.2020.109190. [DOI] [PubMed] [Google Scholar]
- 10.Liu-Helmersson J, Stenlund H, Wilder-Smith A, Rocklov J. Vectorial capacity of Aedes aegypti: effects of temperature and implications for global dengue epidemic potential. PLoS One. 2014;9:e89783. doi: 10.1371/journal.pone.0089783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo C, et al. Global epidemiology of dengue outbreaks in 1990-2015: a systematic review and meta-analysis. Front Cell Infect Microbiol. 2017;7:317. doi: 10.3389/fcimb.2017.00317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiao JP, et al. Characterizing a large outbreak of dengue fever in Guangdong Province, China. Infect Dis Poverty. 2016;5:44. doi: 10.1186/s40249-016-0131-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang XY, et al. Outbreak of dengue fever in central China, 2013. Biomed Environ Sci. 2014;27:894–897. doi: 10.3967/bes2014.125. [DOI] [PubMed] [Google Scholar]
- 14.Du Y, et al. Discovery and whole genome sequences analysis of a dengue virus type 1 strain isolated in Henan province. Zhonghua Yu Fang Yi Xue Za Zhi. 2015;49:892–895. [PubMed] [Google Scholar]
- 15.Ma H, Du Y, Huang X, Li X, Xu B. Analysis of the genome sequences of dengue virus caused an outbreak of dengue fever in Henan province, 2013. Zhonghua Liu Xing Bing Xue Za Zhi. 2015;36:1185–1186. [PubMed] [Google Scholar]
- 16.Zhang FC, et al. Guidelines for diagnosis and treatment of dengue in China. Zhonghua Nei Ke Za Zhi. 2018;57:642–648. doi: 10.3760/cma.j.issn.0578-1426.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 17.NHFPC. (2018)
- 18.Misra UK, Kalita J, Syam UK, Dhole TN. Neurological manifestations of dengue virus infection. J Neurol Sci. 2006;244:117–122. doi: 10.1016/j.jns.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Li S, et al. Chemical evidence of inter-hemispheric air mass intrusion into the Northern Hemisphere mid-latitudes. Sci Rep. 2018;8:4669. doi: 10.1038/s41598-018-22266-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Redondo-Bravo L et al (2019) Imported dengue in Spain: a nationwide analysis with predictive time series analyses. J Travel Med 26. 10.1093/jtm/taz072 [DOI] [PMC free article] [PubMed]
- 21.Halstead S, Wilder-Smith A (2019) Severe dengue in travellers: pathogenesis, risk and clinical management. J Travel Med 26. 10.1093/jtm/taz062 [DOI] [PubMed]
- 22.Cavailler P, et al. Early diagnosis of dengue disease severity in a resource-limited Asian country. BMC Infect Dis. 2016;16:512. doi: 10.1186/s12879-016-1849-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daumas RP, et al. Clinical and laboratory features that discriminate dengue from other febrile illnesses: a diagnostic accuracy study in Rio de Janeiro, Brazil. BMC Infect Dis. 2013;13:77. doi: 10.1186/1471-2334-13-77. [DOI] [PMC free article] [PubMed] [Google Scholar]


